Abstract
Background
Appropriate assessment and interventions for breathing patterns prior to assessment of the patient's musculoskeletal complaint may be beneficial. Breathing pattern disorders (BPDs) are remediable and influenced by biochemical, biomechanical, psychological, and/or unknown factors. The purpose of this clinical commentary is to demonstrate the integratration of a BPD assessment into a standard clinical musculoskeletal orthopedic examination.
Clinical Assessment
The observation of a patient's breathing pattern begins when they enter the clinic, is followed by palpation and orthopedic tests, which allows for proper classification of BPDs.
Outcomes
Disease-oriented measures guide the assessment and classification of BPD, while patient-oriented measures describe clinically important differences among patient values.
Classification
There are many possible variations of classifications of BPD, however, six primary dysfunctions found in the literature have become the foundation of the BPD assessment.
Discussion and Conclusion
Restoring proper breathing mechanics and neuromuscular motor control patterns during breathing may result in a decrease in pain, improved patient outcomes, and overall patient well being associated with their primary musculoskeletal complaint. A comprehensive evaluation of breathing patterns, as a part of an orthopedic examination, may guide a clinician in providing effective and appropriate treatments to decrease pain and improve function.
Level of Evidence
5
Keywords: Dysfunctional movement patterns, startle reflex, musculoskeletal pain
INTRODUCTION AND BACKGROUND
The evaluation and treatment of breathing pattern disorders (BPDs) may be a missing component in the treatment of musculoskeletal pain.1-3 Breathing mediates neuromusculoskeletal responses through its influence on the autonomic nervous system (ANS) and the central nervous system (CNS).4-6 Breathing can be affected by biomechanical, biochemical, psychological, physiological, and/or unknown factors.2,3,7,8 Various examination and treatment paradigms such as, dynamic neuromuscular stabilization, selective functional movement assessment, Buteyko method, and the Janda approach support the concept that breathing is the foundation of allostasis and functional movement. In a typical rehabilitation clinic, assessing breathing patterns may seem like a foreign concept due to the lack of emphasis placed on breathing in the traditional patient examination. However, breathing assessment may be an overlooked and essential tool to address a patient's primary complaint of musculoskeletal pain. The purpose of this clinical commentary is to demonstrate the integratration of a breathing pattern disorder (BPD) assessment into a standard clinical musculoskeletal orthopedic examination. Part II of this commentary will describe the assessment and treatment of patients with BPDs and its effect on their primary complaint of musculoskeletal pain.
A BPD is a dysfunction, not a disease, which in most cases is remediable through rehabilitation and neuromuscular re-education.1,7,8 Symptoms of BPDs can mimic other diseases, often making diagnosis and treatment of BPDs challenging. Clinicians may not always be able to classify a patient into a specific BPD; therefore, must know the etiological features that can cause less than optimal breathing patterns.
Paradoxical breathing, where the abdomen draws in during inhalation and out on exhalation, is often considered the most severe BPD.3 The theoretical result of this BPD is inadequate tidal volume and over activation of the scalenes and other accessory breathing muscles of the upper chest.1,9 The subsequent insufficient exchange of gasses is thought to lead to respiratory distress and musculoskeletal imbalances.9 Similarly, BPDs known as hyperventilation syndrome and tachypnea alters the body's pH producing respiratory alkalosis; which results in an array of symptoms including headache, dizziness, chest pain, trouble sleeping, breathlessness, light sensitivities, exhaustion, and cramps.1,7,10,11 The cause of paradoxical breathing and hyperventilation syndrome is not always known, but can be associated with stress or an emotional response to a traumatic situation.9,12 The secondary symptoms of BPDs, such as frequent yawning, inability to take a deep breath, fatigue and panic attacks,8 may resolve with an appropriate intervention.
FUNCTIONAL BREATHING
The CNS is immature in infants, allowing muscular and breathing patterns to develop sequentially in a genetically pre-determined pattern.5 The diaphragm attains its position in the transverse plane between four to six months after birth, and costal breathing is fully established at six-months.5 Once the position of the diaphragm is established it contributes to the development of stability of the spine and core, allowing the baby to roll, crawl, sit, stand, and begin to walk.4,5 Breathing requires synchronized concentric activity of the diaphragm and pelvic floor, as well as eccentric activity of all muscles that insert into the thorax and abdominal wall muscles.13,14 Improper sequencing during an abdominal breath can alter motor control patterns of postural muscles and spinal stabilizers resulting in pain and/or dysfunction.5,6,15 Therefore, a functional breathing pattern can provide the clinician with a unique perspective into the coordination and maturation of the CNS.
Many muscles assist in the ability to take a breath. The primary and accessory muscles of inhalation and exhalation are listed in Table 1. The diaphragm is the primary muscle responsible for providing 70-80% of the inhalation force and is composed of the skeletal/costal and crural portions.9 The diaphragm is evaluated from the perspective of vital functions such as breathing and metabolism.16 Postural, visceral, and sphincter functions are important components that are often forgotten roles of the diaphragm.1
Table 1.
The Primary and Accessory Muscles in Inhalation and Exhalation
| Muscles of Inhalation | Muscles of Exhalation | |
|---|---|---|
| Primary | Diaphragm Parasternal internal intercostals Upper and lateral external intercostals Levatores costarum Scalenes (less active during normal breathing) |
Elastic recoil* Diaphragm Pleura and costal cartilage* |
| Accessory | Sternocleidomastoid Upper trapexius Serratus anterior Latissimus dorsi Iliocostalis thoracis Subclavius Omohyoid |
Interosseous internal intercostals Abdominal muscles Transversus thoracis Subcostales Iliocostalis lumborum Quadratus lumborum Serratus posterior inferior Latissimus dorsi |
Listed above is a comprehensive list of the primary and accessory muscles that are associated with proper breathing patterns. When there is a BPD the accessory muscles replace the primary movers.3
Primary non-muscular anatomic structures associated with breathing.
A normal breath at rest is referred to as a belly, diaphragmatic, or abdominal breath.3,6,8,15,17 Upon inhalation the diaphragm should move caudally toward the pelvic floor with symmetry, while flattening and compressing the internal organs; the lower ribcage should move proportionately and symmetrically in a lateral, ventral and dorsal direction.3 The abdominal walls should all expand equally in a cylindrical manner. The sternum moves ventrally while the intercostal spaces between the ribs expand minimally at the end of inhalation.3
ASSESSMENT OF BREATHING PATTERNS
The assessment of the patient's breathing pattern begins when the patient enters the clinic. During that time the patient is unaware that they are being observed, which reduces the possibility of conscious changes to breathing patterns.6 The patient's posture should also be observed, as a slumped or hunched posture can limit the ability of the diaphragm to fully expand.18 After the initial observational breathing pattern assessment and a full patient history, the clinician can start a comprehensive breathing examination.
Breathing is commonly assessed in a relaxed, supine position, but can also be observed in more challenging positions such as sitting, standing, or in positions that result in pain or discomfort.6 During the Hi Lo assessment the patient is directed to place one hand on their chest, while the other hand rests on their abdomen (Figure 1). Once in this position the patient is not given any further instructions but the clinician may ask him or her questions regarding their history. The patient should breathe normally, and not be cued to take a deep breath during the assessment, as typically a prompted breath will result in the movement of the chest unless the patient has had previous training in abdominal breathing.6
Figure 1.

The patient has been directed to place one hand on their chest and the other on their abdomen while in a supine position. As noted in the picture they are in a relaxed state and not focusing on their breathing. Placing the patient into a seated or standing position with the same handplacement can be challenging.
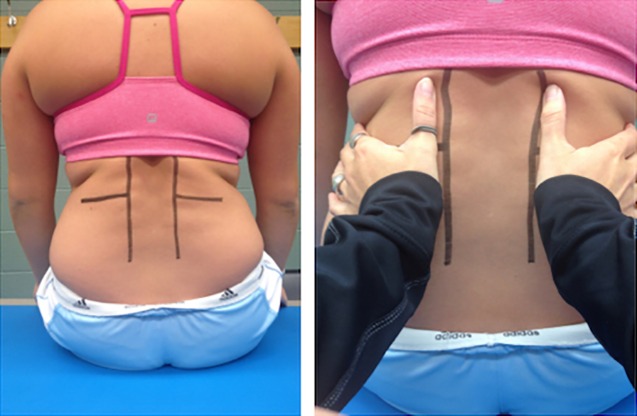
The assessment of breathing patterns is most often marked by the practitioner's observations, however standardized techniques are necessary to quantify a diagnosis. The Manual Assessment of Respiratory Motion (MARM) is a palpatory method that quantifies breathing patterns in a practical, inexpensive, and reliable manner.19 Clinicians have used the MARM to assess diaphragm function since the 1980s to determine thoracic, abdominal and lateral breath. The MARM has good inter-examiner reliability (ICC = 0.85, p=.0001, CI 0.78, 0.89) as compared to plethysmography.19 The MARM is performed by having the clinician positioned behind the seated patient and placing their hands on the posterior and lateral aspects of the 11th and 12th ribs.6,19 While the patient breathes, the clinician measures perceived displacement and functional movement of the upper and lower rib cage movement, as well as abdominal expansion using two lines drawn on the patient to form a half of a pie chart and pressure placed through the clinician's hands (Figure. 2).19 The MARM values are calculated by measuring angle differences between the highest point of the inhalation (upper rib cage) and the lowest point (lower rib cage).19 Each side of the body is considered its own entity and measurements should be between zero and 180 degrees. Positive values are indicative of chest breathing/vertical movement and negative values indicate abdominal/lateral movement.19
Patients are assessed for tender areas, jump signs, or withdrawal reflexes upon palpation at the 1st/2nd, 7th/8th, or 11th/12th ribs unilaterally or bilaterally, as this may be a sign of faulty breathing patterns.1,20,21 John Iams proposed that patients displaying increased sensitivity to normal palpation have an autonomic nervous system (ANS) that may be unable to balance the body's involuntary systems (i.e., parasympathetic and sympathetic nervous systems).20-22 Theoretically, if the patient's body is functioning mainly in a protective state through activity of the sympathetic nervous system (SNS), a state of “up-regulation” may exist that presents as a startle or withdrawal reflex upon palpation.21 If a patient presents with a startle reflex, or sensitivity to one or more of these locations, manual therapy could be used to “down-regulate” the area(s) or inhibit the pain cycle.21-23 Therefore, assessing these specific locations with palpation may be important in clinical practice, as an “up-regulated” ANS could be a source of BPDs and musculoskeletal pain.
CLASSIFICATION OF BREATHING PATTERN DISORDERS
There are many possible variations of classifications of BPDs, however, six primary dysfunctions found in the literature have become the foundation of the BPD assessment. A normal breathing pattern is classified as diaphragmatic or abdominal breathing.6 Although this is considered a normal breathing pattern, it should be noted that a “normal” breathing pattern found in patients should not be considered the ideal functional breathing pattern. A few dysfunctional variations of an abdominal breath exist, including: asymmetrical with limited motion on one side of the abdomen; anterior movement only, without lateral or posterior movement; and adequate anterior and lateral movement, without posterior.
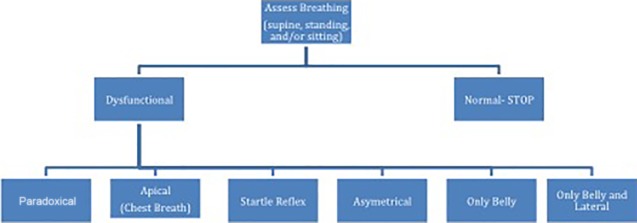
A chest or apical breather is characterized by excessive movement of the sternum and shoulder girdles toward the cranium, and minimal abdominal movement during inhalation.6-8 Paradoxical breathing is when the chest expands during inhalation and the abdomen is drawn inwards and then during exhalation the abdomen is pushed outwards.7,8 A new BPD classification, proposed by the authors of this commentary, is associated with a startle reflex. A startle reflex is when a patient elicits a withdrawal reflex upon palpation to the right or left 1st and 2nd ribs, anterior 7th and 8th ribs, and 11th and 12th ribs.24 In part 2 of this series, three patient cases will be presented that display the short-term effects of treating a startle reflex BPD. Figure 3 is a visual representation of the classification of BPD in a rehabilitation clinic.
Figure 3.
Breathing Pattern Assessment and Classification of Dysfunctions. The flow chart is the systematic approach designed by the clinicians to effectively and efficiently assess breathing in the Rehabilitation Clinic.
Figure 2.
The lines drawn on the patient depict the MARM angles the clinician is using to classify and quantify lower rib movement.
OUTCOME MEASURES
Breathing pattern assessments, patient reported outcome measures, and other examination findings help to build a complete picture of BPDs.6,7 Outcome measures identify minimal clinically important differences in patients with pain25 and dysfunction to determine the effectiveness of a clinician's assessment and treatment.19,26 A number of outcome measures can be used to quantify efficacy of evaluations and interventions in decreasing pain and correcting dysfunction in patients.1 Measurement tools to evaluate musculoskeletal pain and/or dysfunction include the Numerical Pain Rating Scale26 and the Disablement in the Physically Active scale.27,28 The Nijmegen Questionnaire is a patient-reported outcome measure used to identify the presence of signs and symptoms associated with general and respiratory distress and higher values represent distress and dysfunction of the respiratory system.1,11 These tools can easily be incorporated into an orthopedic examination without the addition of too much time.
Outcome measures should encompass both clinician and patient-reported evidence. Clinician-reported measures that may be useful in the collection of outcomes are the findings from the physical examination (functional impairments, range of motion, strength, asymmetry, MARM, Hi Lo, etc.). Patient-reported measures that may be useful in the collection of outcomes are the Numerical Pain Rating Scale,26 Disablement in the Physically Active scale,27,28 and Nijmegen Questionnaire,11 as well as specific patient-oriented evidence measures that can be used at the clinician's discretion.
All outcome measures can be used in conjunction with comprehensive examination and functional biomechanical assessment (e.g. Selective Functional Movement Assessment). The CNS allows for optimal positioning of posture and stability through functional movement patterns.5,13 Through the use of a functional assessment, the clinician may be able to locate pattern deficiencies contributing to the chief complaint(s) or less than optimal movement patterns. The correction of breathing patterns in low level postures should occur first and be followed by integration of proper breathing into complex movement patterns.
CLINICAL ADVANTAGES
Breathing is an involuntary process thought to be an essential aspect of posture and core stability. Restoring proper breathing mechanics and motor control can result in decreased pain, improved patient outcomes, and improved patient health.6,8 Evaluation of breathing patterns is an easy clinical technique to learn. Treating BPDs requires little to no equipment in the rehabilitation clinic and intervention techniques provided by the clinician can be structured as a home exercise program in approximately five minutes or less.
DISCUSSION
The purpose of this clinical commentary was to illustrate how to assess and classify BPDs prior to or in conjunction with the treatment of musculoskeletal pain or dysfunction. Since a BPD is not a disease, it is usually not recognized until an assessment is performed.6-8 The specific cause(s) of BPDs are unknown, and each patient may adapt individual neuromuscular patterns associated with faulty breathing patterns. Postural and structural adaptations could possibly result in pain and/or dysfunction of muscles, ligaments, or joints with no apparent organic source, possibly resulting in various BPD signs and symptoms. The three main contributing factors to BPDs are: biomechanical, biochemical, and psychological.3,8,9,29
The act of breathing is mechanical in nature as the diaphragm and primary muscles control most of the respiratory system.3,5 Restriction of muscle length, muscle imbalances, and diaphragm expansion can modify posture and core stability as a result of the body's inability to return to optimal resting position.3,5,8,15 The concept of regional interdependence suggests that if one part of the kinetic chain is unable to perform motor patterns sufficiently, another portion of the body compensates for the deficiency, resulting in dysfunction.30 Breathing patterns may change as a result of altered motor control patterns and postural changes and if the imbalances are not addressed can lead to suboptimal function of the CNS and chronic pain.5
While the biomechanical factors are visible to the clinician it is important to remember biochemical components of the respiratory system as well. Changes in the body's pH level, allergies, dietary factors, hormone levels, or internal organ dysfunction can potentially lead to premature fatigue, breathlessness, dyspnea, and resultant muscle pain.6,8 The mind and body work together to maintain homeostasis during times of stress and anxiety.31,32 While research is limited in understanding the emotional factors contributing to BPDs, researchers have suggested that memories, past experiences, and emotional states can have an effect on breathing patterns.33,34
“If breathing is not normalized, no other movement pattern can be.”35 Frank et al5 and Chaitow7 suggest that abnormal stabilization patterns are associated with BPDs and should be the starting point for all orthopedic evaluations. The authors believe that correction or re-education of BPDs can result in new neural connections and restoration of normal motor control patterns in the CNS. Roussel et al15 observed various dysfunctional breathing patterns and altered motor control patterns during functional testing in a group of patients with low back pain compared to a group of healthy individuals. Breathing patterns are established subcortically and often associated with an injury, pain, and/or movement dysfunction. The goal of restoring breathing patterns is to establish normal subcortical motor patterns.7 An athlete with an abnormal breathing pattern during physical activity may experience premature breathlessness or muscle fatigue, resulting in decreased performance.
CONCLUSIONS
The assessment and classification of BPDs is important, as normal and abnormal breathing patterns affect movement. Once a breathing dysfunction is classified, finding appropriate exercises for muscle relaxation, re-education of motor control patterns, and normal breathing patterns at rest and during activities may help restore normal and physiological balanced breathing.6 Breathing pattern assessments and interventions might improve patient quality of life, physical function, and decreased breathing signs and symptoms during activities of daily living and exercise.3,7,8,15,17,19 Part II of this clinical commentary will provide a case series related to BPDs in an athletic population, the interventions associated with BPDs, and the effects of BPDs interventions.
REFERENCES
- 1.Chaitow L Gilbert C Bradley D. Recognizing and Treating Breathing Disorders. Elsevier Health Sciences; 2013. [Google Scholar]
- 2.Courtney R Cohen M van Dixhoorn J. Relationship between dysfunctional breathing patterns and ability to achieve target heart rate variability with features of” coherence” during biofeedback. Altern Ther Health Med. 2010;17(3):38-44. [PubMed] [Google Scholar]
- 3.Perri MA Halford E. Pain and faulty breathing: a pilot study. J Bodyw Mov Ther. 2004;8(4):297-306. [Google Scholar]
- 4.Cook G. Movement: Functional movement systems: Screening, assessment, corrective strategies. On Target Publications; 2014. [Google Scholar]
- 5.Frank C Kobesova A Kolar P. Dynamic neuromuscular stabilization & sports rehabilitation. Int J Sports Phys Ther. 2013;8(1):62. [PMC free article] [PubMed] [Google Scholar]
- 6.Perri M. Rehabilitation of breathing pattern disorders. Liebenson C. Rehabilitation of the spine: a practitioner's manual, 2nd ed. Philadelphia: Lippincott Williams & Wilkins; 2007:93-109. [Google Scholar]
- 7.Chaitow L. Breathing pattern disorders, motor control, and low back pain. J Osteop Med. 2004;7(1):33-40. [Google Scholar]
- 8.Clifton-Smith T Rowley J. Breathing pattern disorders and physiotherapy: inspiration for our profession. Physl Ther Rev. 2011;16(1):75-86. [Google Scholar]
- 9.Simons DG Travell JG Simons LS. Travell & Simons’ myofascial pain and dysfunction: upper half of body. Vol 1: Lippincott Williams & Wilkins; 1999. [Google Scholar]
- 10.Folgering H. The pathophysiology of hyperventilation syndrome. Monaldi Arch Chest Dis. 1999;54(4):365-372. [PubMed] [Google Scholar]
- 11.Van Dixhoorn J. Hyperventilation and dysfunctional breathing. Paper presented at: Biological Psychology1997.
- 12.Lum L. Hyperventilation—a rose by any other name. Compl Ther Med. 1996;4(3):185-189. [Google Scholar]
- 13.Kolar P Kobesova A Valouchova P Bitnar P. Dynamic Neuromuscular Stabilization: developmental kinesiology: breathing stereotypes and postural-locomotion function. Recognizing and Treating Breathing Disorders. 2014:11. [Google Scholar]
- 14.Kolárˇ P Šulc J Kyncˇl M, et al. Postural function of the diaphragm in persons with and without chronic low back pain. J Orthop Sports Phys Ther. 2012;42(4):352-362. [DOI] [PubMed] [Google Scholar]
- 15.Roussel N Nijs J Truijen S Vervecken L Mottram S Stassijns G. Altered breathing patterns during lumbopelvic motor control tests in chronic low back pain: a case–control study. Eur Spine J. 2009;18(7):1066-1073. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Courtney R. The functions of breathing and its dysfunctions and their relationship to breathing therapy. Int J Osteop Med. 2009;12(3):78-85. [Google Scholar]
- 17.Hagman C Janson C Emtner M. Breathing retraining-A five-year follow-up of patients with dysfunctional breathing. Resp Med. 2011;105(8):1153-1159. [DOI] [PubMed] [Google Scholar]
- 18.White GM. Optimal Breathing Kit. Charlotte, NC 2014.
- 19.Courtney R Van Dixhoorn J Cohen M. Evaluation of breathing pattern: comparison of a Manual Assessment of Respiratory Motion (MARM) and respiratory induction plethysmography. Appl Psychophysiol Biofeedback. 2008;33(2):91-100. [DOI] [PubMed] [Google Scholar]
- 20.Iams J. When reflexes rule: A new paradigm in understanding why some patients don't get well. Adv Phy Ther Rehab Med. 2005;16(3):41. [Google Scholar]
- 21.Iams J. What is the primal reflex release technique for pain relief? 2012 http://www.theprrt.com/what-is-the-primal-reflex-release-technique-for-pain-relief.php. Accessed Accessed August 1 2013.
- 22.McKeon N. Use of Primal Reflex Technique in the Treatment of Chronic Pain: A Case Study [Campstone Project II] 2009.
- 23.Hansberger BL Baker RT May J Nasypany A. A Novel Approach To Treating Plantar Fasciitis–Effects of Primal Reflex Release Technique: A Case Series. Int J Sports Phys Ther. 2015;10(5):690. [PMC free article] [PubMed] [Google Scholar]
- 24.Iams J. Primal Reflex Release Technique Home Study Course. In: Inc. S, ed 2012.
- 25.Cook CE. Clinimetrics corner: the minimal clinically important change score (MCID): a necessary pretense. J Man Manip Ther. 2008;16(4):82E-83E. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 26.Farrar JT Young Jr JP LaMoreaux L Werth JL Poole RM. Clinical importance of changes in chronic pain intensity measured on an 11-point numerical pain rating scale. Pain. 2001;94(2):149-158. [DOI] [PubMed] [Google Scholar]
- 27.Vela LI Denegar CR. Transient disablement in the physically active with musculoskeletal injuries, part I: a descriptive model. J Athl Train. 2010;45(6):615. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 28.Vela LI Denegar CR. The disablement in the physically active scale, part II: the psychometric properties of an outcomes scale for musculoskeletal injuries. J Athl Train. 2010;45(6):630. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 29.Kox M van Eijk LT Zwaag J, et al. Voluntary activation of the sympathetic nervous system and attenuation of the innate immune response in humans. Proc Natl Acad Sci. 2014;111(20):7379-7384. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 30.Janda V Frank C Liebenson C. Evaluation of muscular imbalance. Rehab Spine. Baltimore: Lippincott Williams & Wilkins; 1996:97-112. [Google Scholar]
- 31.Balaban CD Thayer JF. Neurological bases for balance–anxiety links. J Anxiety Disorders. 2001;15(1):53-79. [DOI] [PubMed] [Google Scholar]
- 32.Bloch S Lemeignan M Aguilera-T N. Specific respiratory patterns distinguish among human basic emotions. Int J Psychophysiol. 1991;11(2):141-154. [DOI] [PubMed] [Google Scholar]
- 33.Gilbert C. Emotional sources of dysfunctional breathing. J Bodyw Mov Ther. 1998;2(4):224-230. [Google Scholar]
- 34.Grillon C Morgan III CA. Fear-potentiated startle conditioning to explicit and contextual cues in Gulf War veterans with posttraumatic stress disorder. J Abnorm Psychol. 1999;108(1):134. [DOI] [PubMed] [Google Scholar]
- 35.Lewit K. Relationship of faulty respiration to posture, with clinical implications. J Am Osteopath Assoc. 1980;79(8):525-528. [PubMed] [Google Scholar]