Abstract
Objectives:
More than a decade has passed since the last major workforce survey of child neurologists in the United States; thus, a reassessment of the child neurology workforce is needed, along with an inaugural assessment of a new related field, neurodevelopmental disabilities.
Methods:
The American Academy of Pediatrics and the Child Neurology Society conducted an electronic survey in 2015 of child neurologists and neurodevelopmental disabilities specialists.
Results:
The majority of respondents participate in maintenance of certification, practice in academic medical centers, and offer subspecialty care. EEG reading and epilepsy care are common subspecialty practice areas, although many child neurologists have not had formal training in this field. In keeping with broader trends, medical school debts are substantially higher than in the past and will often take many years to pay off. Although a broad majority would choose these fields again, there are widespread dissatisfactions with compensation and benefits given the length of training and the complexity of care provided, and frustrations with mounting regulatory and administrative stresses that interfere with clinical practice.
Conclusions:
Although not unique to child neurology and neurodevelopmental disabilities, such issues may present barriers for the recruitment of trainees into these fields. Creative approaches to enhance the recruitment of the next generation of child neurologists and neurodevelopmental disabilities specialists will benefit society, especially in light of all the exciting new treatments under development for an array of chronic childhood neurologic disorders.
In the past 2 decades, child neurology has undergone a remarkable transformation, and has been joined by an important companion field, neurodevelopmental disabilities. In the past, large academic child neurology groups were rarities in the United States. Now groups of a dozen or more child neurologists are becoming increasingly common in major metropolitan areas, as expectations regarding access to appointments and availability of specialty services have increased. More child neurologists now undergo subspecialty training in pediatric epilepsy/neurophysiology, behavioral neurology, neuromuscular diseases/neurophysiology, neuroimmunology, movement disorders, and other fields. The accurate diagnosis and treatment of childhood neurologic diseases has acquired a new urgency, as standards of care are advancing rapidly and novel molecular therapies for a range of these disorders are emerging. Thus, the need for a well-trained, highly motivated child neurology workforce is more important than ever.
Natural questions to ask are whether the workforce is equipped to handle this bounty and open new frontiers, and what challenges these specialists are currently encountering in their careers. The last child neurology workforce survey in the United States was conducted more than a decade ago by the Child Neurology Society (CNS).1 Because of the perceived changes in the size and focus of this workforce, the American Academy of Pediatrics (AAP) and the CNS concluded that a new survey was needed. The AAP and CNS therefore conducted a joint survey in 2015 to determine the current composition and clinical activities of the child neurology and neurodevelopmental disabilities workforce, and to identify future needs in these fields.
METHODS
The AAP Section on Neurology and the CNS convened a joint task force in 2014 to work with the AAP Division of Workforce and Medical Education Policy and conduct a child neurology workforce survey. This study was deemed exempt by the institutional review board of the AAP. The survey (available as supplemental data at Neurology.org) consisted of 112 questions that were approved by the joint task force, the AAP institutional review board, and the CNS. Forty-four of these questions were repeated from the AAP Future of Pediatric Education II survey in 1997 and were standardized across all pediatric subspecialty surveys. The survey was distributed by e-mail to the 145 members of the AAP Section on Neurology and the 1,175 members of the CNS, including 305 trainees. Those who appeared on both lists were removed from the CNS list to avoid duplication. Trainees received a shorter survey, containing a subset of 23 questions. The survey was open from March 18 to June 19, 2015, with 4 electronic reminders sent to nonresponders. The target population included child neurologists, neurodevelopmental disabilities specialists, and trainees in those fields. SPSS 18.0 (SPSS Inc., Chicago, IL) was used to generate frequency distributions of all variables. Those distributions as well as free text responses were made available to the task force members for further analysis.
RESULTS
Response rates and demographics.
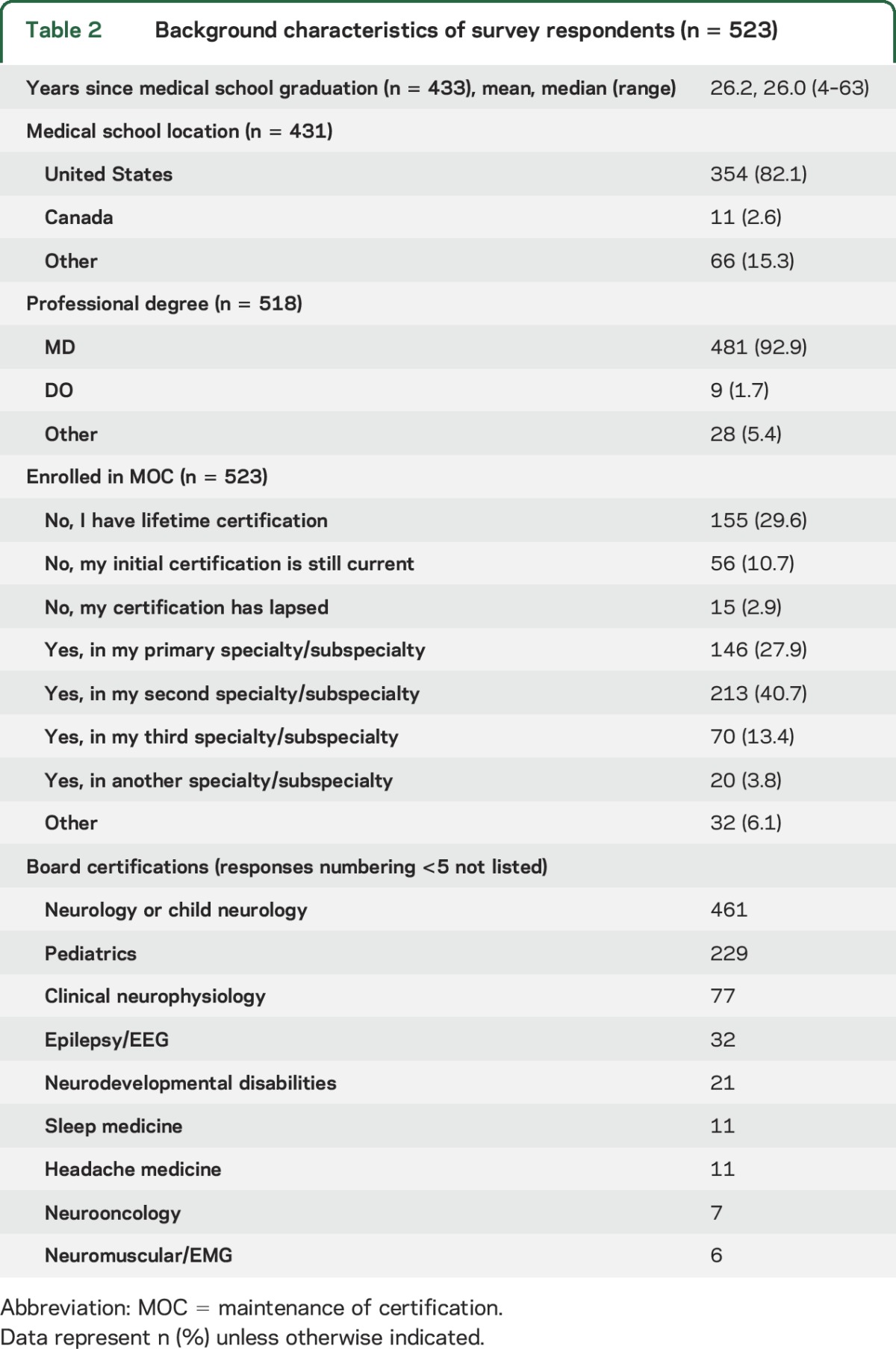
Response rates were 71/145 (49%) from the AAP Section on Neurology, 452/1,175 (38%) from the CNS, and 97/305 (32%) among trainees, for a total of 523 practicing physicians and 97 trainees. The primary or secondary subspecialty was reported to be child neurology, neurology, and/or neurodevelopmental disabilities in most cases, with 85.5% in active clinical practice. Table 1 lists demographic details. The overall sex distribution was more than 60% male, but was nearly equal between men and women for those who are 18 or fewer years from completion of training. Respondents were predominantly white, with some representation of Asian child neurologists and small numbers of black/African American, Hispanic, and other underrepresented minority groups. Table 2 lists educational background, maintenance of certification status, and board certifications. Among practicing child neurologists and neurodevelopmental specialists, 31 reported MD-PhD degrees, and 4 trainees reported these joint degrees. Subspecialty activities were reported by 65.2%, clinical research by 47.0%, translational research by 18.2%, and basic science research by 8.8%. A substantial minority (29.6%) reported that they do not participate in maintenance of certification because of lifetime certification, suggesting that they were certified prior to 1994. Table e-1 lists professional organization memberships.
Table 1.
Demographics
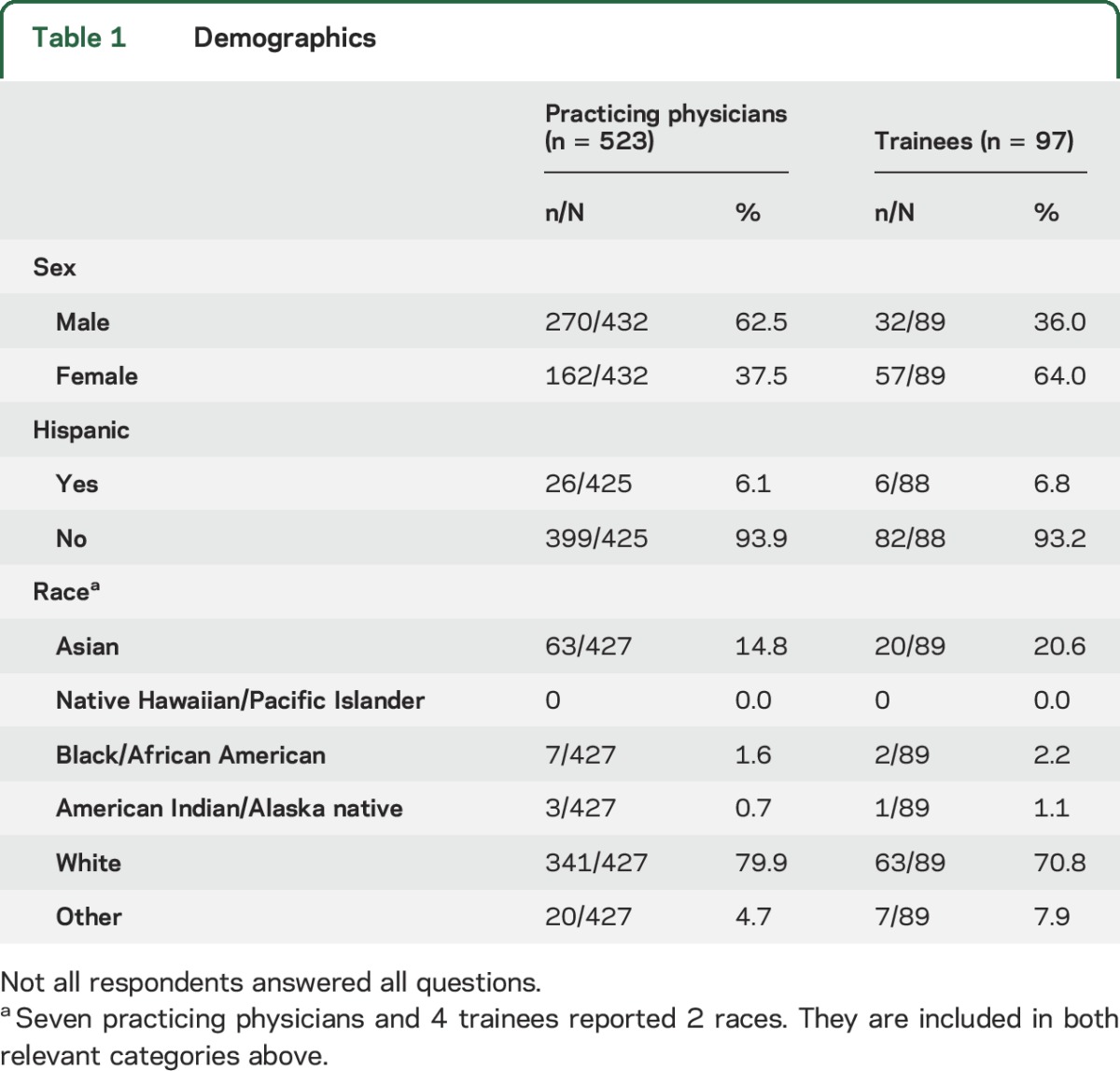
Table 2.
Background characteristics of survey respondents (n = 523)
Practice settings.
The majority of respondents practice in academic medical centers, with others practicing in multispecialty groups, specialty group practices, solo practices, and community hospitals (table e-2). Nearly all practice in urban or suburban areas, with only a small fraction working in rural settings. The mean hours worked per week was 54.6, with a median of 55. Nearly all respondents (97.4%) provide direct patient care. A small percentage work as hospitalists. The majority of child neurologists and neurodevelopmental disabilities specialists have yet to use telemedicine for formal consultation, but more than half were amenable to using telemedicine, especially for children with epilepsy. There was a broad spread of waiting times for new patient, non-emergency appointments, with the majority falling within 2 to 16 weeks (table e-2).
Diagnostic distributions.
For outpatient activities, the highest median patient proportions were 21% to 30% for seizures and epilepsy, and 11% to 20% for headaches. Median distributions were otherwise 0% to 10% for all other major disease categories: movement disorders, neurodevelopmental and intellectual disabilities, neuropsychiatric, behavioral, and learning disorders, neuromuscular, neuroimmunology, metabolic disorders, neurogenetic disorders, neuro-oncology, brain injury/concussion, fetal/neonatal neurology, and sleep disorders. For inpatient activities, the highest median patient proportions were 61% to 70% for seizures and epilepsy, but the distribution was scattered throughout the range, as the median only represented 8.6% of respondents. All other disease categories had median proportions of 0% to 10%: headaches, movement disorders, neurodevelopmental and intellectual disabilities, neuropsychiatric, behavioral, and learning disorders, neuromuscular, neuroimmunology, metabolic disorders, neurogenetic disorders, neuro-oncology, brain injury/concussion, fetal/neonatal neurology, and sleep disorders.
Epilepsy management.
Of the 402 respondents who reported managing patients with epilepsy, 65% (260) read EEGs. Of these, 42% (109) were formally trained in a neurophysiology or epilepsy fellowship, while more than 50% (142) reported receiving EEG training only during residency. Furthermore, 186 expressed an interest in virtual training in this field, and 63 work in groups that lack an epilepsy specialist; those physicians generally referred children with epilepsy to a specialty center. About 39% of these reported that the epilepsy specialists to whom they referred were more than 60 miles away. Details are listed in table e-3.
Referral patterns.
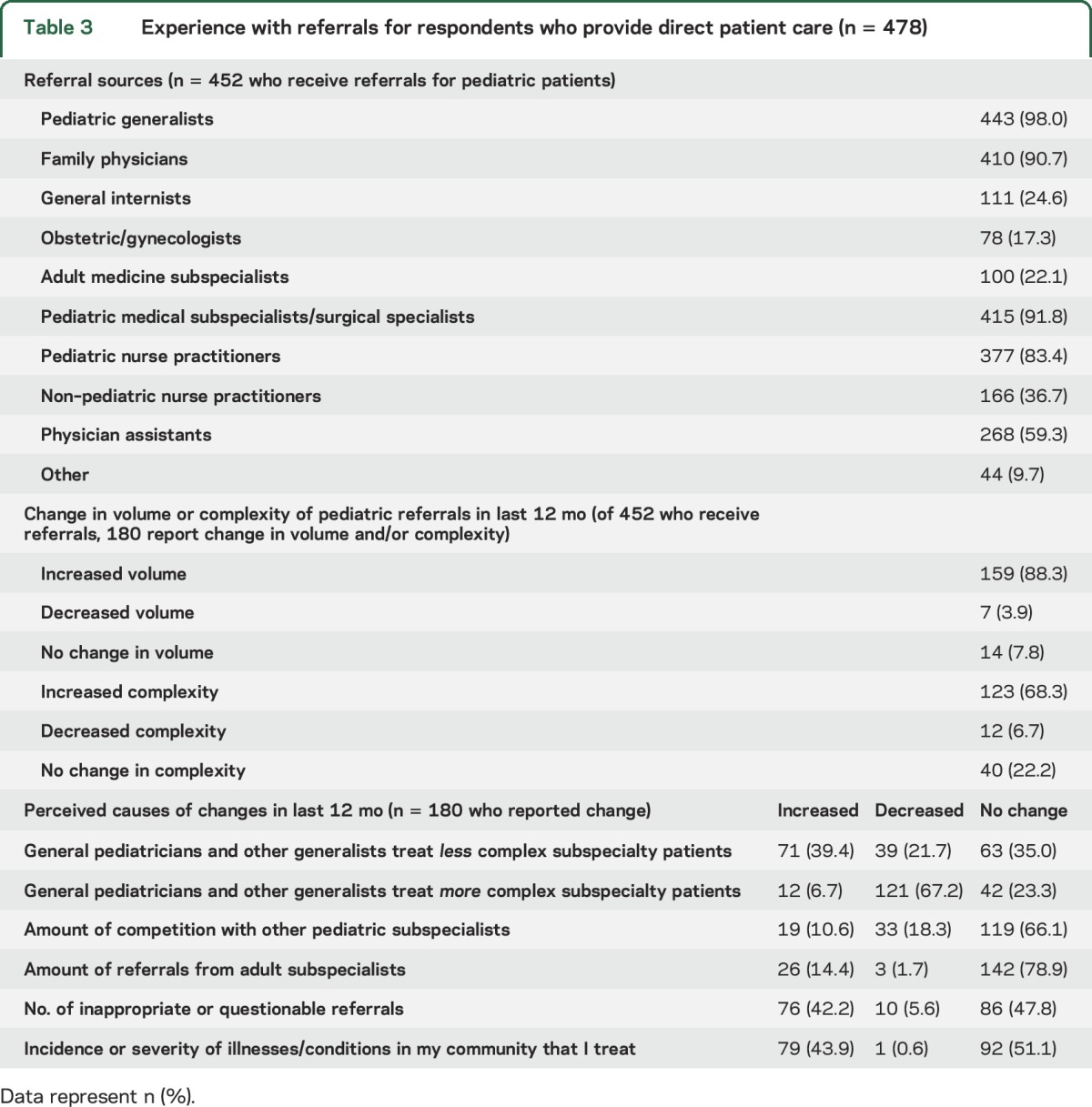
Details of referral patterns are found in table 3, including perceptions of changes in various factors that could influence the volume and complexity of referrals. Among the 39.8% of respondents who reported changes in referral volume or complexity in the past 12 months, 88.3% experienced an increase in volume, while 68.3% experienced an increase in complexity. The most common perceived reasons for these changes are a decrease in the complexity of patients whom general pediatricians treat, an increase in the number of inappropriate or questionable referrals, and local changes in the incidence or severity of certain diagnoses.
Table 3.
Experience with referrals for respondents who provide direct patient care (n = 478)
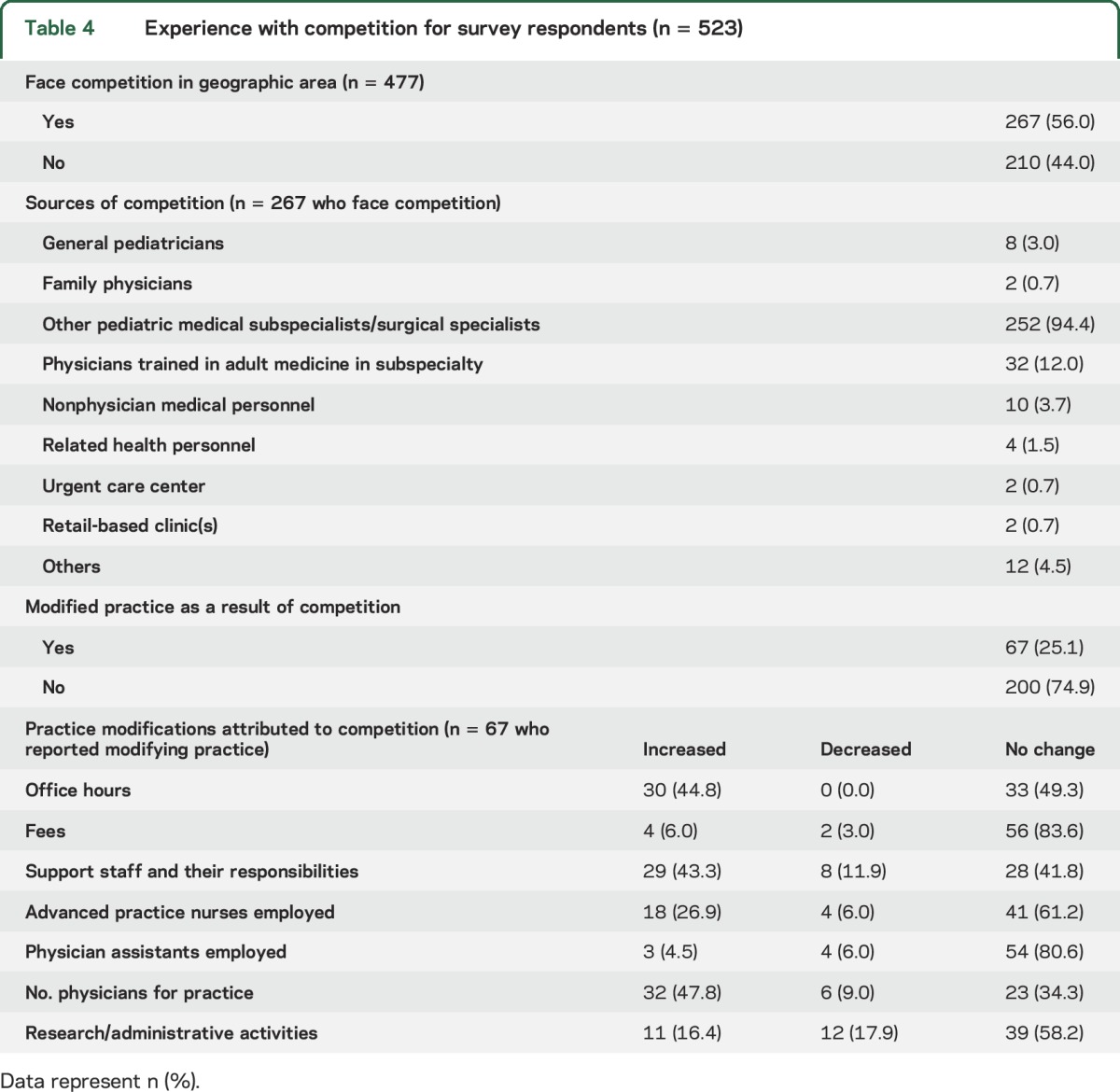
Competition.
Details of practice competition are described in table 4. A slim majority face competition in their immediate geographic area, primarily from other subspecialists. About a quarter of those respondents modified practice patterns as a result, including increased office hours, increased support staff/responsibilities, and increased physician staffing in the practice.
Table 4.
Experience with competition for survey respondents (n = 523)
Medical school financing.
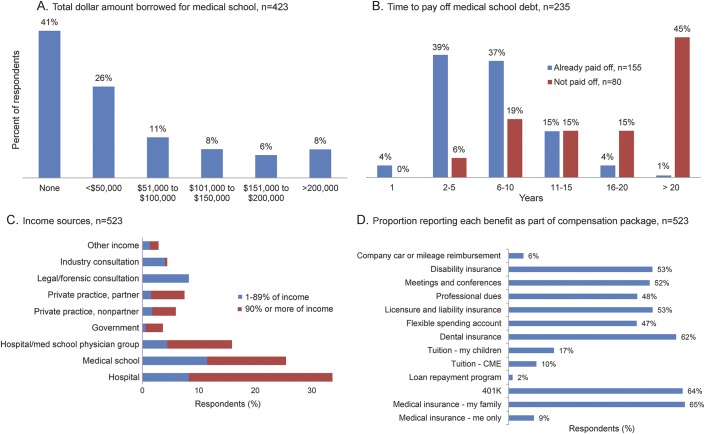
Like other physicians, most child neurologists and neurodevelopmental disabilities specialists incurred financial liabilities for medical education. Among the respondents who took out loans, the majority accumulated at least $50,000 in debt (figure, A). For those who have paid off their loans, fulfillment of these loans took 15 years or fewer in most cases (figure, B). However, 45% of those with outstanding loan obligations expect that it will take more than 20 years to pay them off (figure, B).
Figure. Financial data.
Graphical summaries of financial data, including (A) total medical school debt, (B) time taken/expected to pay off medical school debt, (C) income sources, and (D) fringe benefits as components of compensation packages. CME = continuing medical education.
Compensation.
A minority (26.5%) of respondents are positive or extremely positive about their total compensation, whereas a larger number are negative or extremely negative (42.4%), with the remainder neutral. This is corroborated by the 52% of our respondents who believe that the perceived lower income of child neurologists compared to other specialists explains at least in part the lower match rates for training programs. Less than half of respondents (48.7%) believe they are being fairly compensated with appropriate financial accountability, while 19.0% feel that they are fairly compensated but oppose the accountability methods applied to them, and 28.5% feel unfairly compensated. Furthermore, 68.2% believe that they receive inferior compensation, and 42.8% expect the future compensation of child neurologists to decrease. A higher percentage of child neurologists in private practice settings expect their future compensation to decrease compared to those in academic settings (51% vs 37%, p = 0.006). Common themes among open-ended comments include poor remuneration for the extensive training, long work hours, and stress accompanying the practice of child neurology and neurodevelopmental disabilities. Most feel that their contributions are not adequately recognized by large hospital systems and health care reimbursement structures. Details are listed in table e-4.
Compensation sources and structures.
Child neurologists and neurodevelopmental disabilities specialists derive the majority of their income from hospitals, hospital physician groups, or medical schools: approximately 78% receive all of their income from these sources (figure, C). Respondents are often held to accountability standards by these employers, including work relative value unit (53%) and cash collection (13%) methodologies. Only 18% report that they are not subject to such accountability methods. Base salaries comprise 71% to 100% of total compensation for 85.8% of respondents, but for 11% this base salary is not guaranteed. Bonuses account for 0% to 10% of total compensation for 76% of respondents, with another 22% reporting 11% to 30% of their income as bonus payments. Bonuses were not guaranteed for 94%. For 27%, the majority of their compensation was determined by individual productivity, compared to 22% who reported collective measures. Supplemental or alternative sources of revenue include medicolegal work (19%) and industry consultation (9.9%) (figure, C). Benefits varied as noted in figure, D. Although many receive core benefits such as medical insurance, dental insurance, disability insurance, and retirement plans, a substantial number do not. Tuition reimbursement and loan repayment programs are not commonly available. About half of respondents report support for professional expenses.
Workforce needs: Division director perspectives.
The vast majority of division directors, 67.8% (59), thought that the level of physician and nonphysician staffing in their groups is insufficient, and expect to hire additional physicians in the next 3 years to expand their groups, with a slimmer majority expecting to hire additional physicians in the next 3 years to replace departing colleagues, including retirees.
Career choices.
A broad majority, 70.7%, of child neurologists and specialists in neurodevelopmental disabilities would definitely or probably select the field again if given the choice, while 8.2% would definitely not or probably not select the field again. In a related free-text field, a number of respondents stated that they would not choose medicine again at all, indicating that the discontent may not be attributable primarily to factors specific to these fields.
Trainees: Division director perspectives.
Among division directors, 39 of 87 reported having child neurology and neurodevelopmental disabilities residents (postgraduate years 3–5, not including pediatric residents in 5-year categorical programs). Among these, 17 reported 1–3 total residents, 14 reported 4–6, and 8 reported 7 or more. Subspecialty fellows were reported by 25 of the 87 division directors: 18 with 1–3, 6 with 4–6, and 1 with 7 or more fellows.
Trainee responses.
Demographic characteristics are listed in table 1 and other details are listed in table e-5. Medical degrees held by trainees included 85.3% with MD degrees, 12.6% with DO degrees, and 2.1% with other medical degrees. Similar to their counterparts in practice, 93.7% are training in urban and suburban settings, with only 1.0% reporting a rural community. Regarding professional organizations, 37.1% report membership in the AAP, 3.1% in the AAP Section on Neurology, 82.5% in the American Academy of Neurology, 2.1% in the American Neurological Association, 91.8% in the CNS, 4.1% in the Society for Pediatric Research, and 11.3% in the International Child Neurology Association. A few respondents (6.2%) reported no residents at their own institutions (presumably these are institutions that only sponsor subspecialty fellowships), 14.4% reported 1–3, 37.1% reported 4–6, and 35.1% reported 7 or more. Almost a quarter (24.7%) of respondents reported no subspecialty fellows at their own institutions, 45.4% reported 1–3, 11.3% reported 4–6, and 10.3% reported 7 or more. Regarding career choices, 80.4% would definitely or probably select child neurology or neurodevelopmental disabilities again, while 3.1% would definitely not or probably not do so again.
DISCUSSION
The United States has a lower ratio of physicians per capita than other industrialized nations.2 The projection of future physician workforce needs is an inexact science, relying on numerous assumptions,2 and the fields of child neurology and neurodevelopmental disabilities are not exempt from these problems. A workforce survey of child and adolescent psychiatry estimated that 5% of the pediatric population would require psychiatry services, which helped calculate workforce deficits.3 Such calculations are difficult to replicate for child neurology and neurodevelopmental disabilities. For example, while as many as 91% of adolescents may experience headaches,4 an unknown fraction would seek specialty care. However, the current survey results provide valuable indications that the workforce remains understaffed, and that the rate of growth is not currently adequate to meet expected needs. The majority of division directors believe that their staffing levels are inadequate, and the volume and complexity of referrals is perceived to be rising. Work hours remain similar to the numbers from 2002,1 suggesting that child neurologists may be feeling pressure to increase productivity within limited time allowances. These specialists are seeing many referrals that they believe are more routine in nature. A 2006 survey of pediatricians focusing on their views of the child neurology workforce found that pediatricians had an increasing need to refer to child neurologists because of patient complexity and parental expectations, and that 90% of the pediatricians perceived a shortage of child neurologists in the United States.5 The typical wait for a new patient appointment ranged from 2 weeks to 4 months for the majority of respondents in the current survey, suggesting that the median wait of 45 days in 2002 has not changed dramatically.1
Sex ratios have evened out somewhat since 2002.1 The trainee cohort includes a much higher proportion of female physicians and a slightly higher proportion of Asian physicians compared to practicing physicians, but underrepresented minority groups remain at lower percentages compared to their proportions in the United States as a whole, as well as the proportions among current residents in all medical fields.6,7 This represents a significant problem given the burden of neurologic disease among children in minority populations.8 Growth in the minority physician workforce may contribute to increased access to health care for minority populations9 and better communications with minority patients.10 Practice settings remain predominantly urban and suburban, likely reflecting the location of academic medical centers and other large practices. The percentage working in academic medical centers has not changed significantly since 2002; however, the proportion of employed physicians has increased,1 raising the question of whether rural populations have adequate access. The proportion of child neurologists and neurodevelopmental disabilities specialists who read EEGs has decreased since 2002,1 likely reflecting the increasing expectation of subspecialty training to interpret such diagnostic procedures. Society memberships indicate a strong interest in subspecialty care for a substantial minority of these physicians.
Nearly half of respondents report clinical research activity, but less than 10% conduct basic research, suggesting that the physician-scientist workforce in child neurology and neurodevelopmental disabilities remains an endangered species, reflecting broader trends.11 The number of respondents with joint MD-PhD degrees is modest; however, these degrees were reported in a free-text field, thus the numbers may underestimate the true population. The goal of the NIH Neurological Sciences Academic Development Award (K12) has been to foster the growth and success of early career physician-scientists. This program is small, limiting its national footprint, but is being replaced by a new Child Neurologist Career Development Program (K12) that will fund a single national program to support this cohort. Concerns about workforce shortages for child neurology in the United States have been discussed since 2000.12 The number of training positions has increased from the average of 80 per year reported among 58 active programs in the 1997–2002 period13 to 154 positions offered by 73 active programs in 2014.6 Compared to the workforce in general pediatrics and other pediatric subspecialties, the supply of child neurologists is projected to grow slowly,14 especially compared to predicted needs,15 despite the perceived shortfall of child neurologists among pediatricians.5 Active members of the CNS in the United States have grown from 429 in 1981, 756 in 1991, 1,013 in 2001, 1,160 in 2011, to 1,322 in 2015 (Roger B. Larson, personal communication, 2015). The raw figures suggest impressive growth; however, the compound annual increase over this period is 3.37%. Junior membership, representing trainees, has grown from 84 in 1981 to 390 in 2015. Currently, the CNS membership is 43% female, but among junior members, 68% are female, mirroring our current survey results. The slow rate of growth raises concerns that an acute workforce shortage may develop as retirements accumulate. Concerns about workforce shortages are not universal across borders, however, as one study estimates an oversupply of child neurologists in Canada.16 The low proportion of physician-scientists in child neurology and neurodevelopmental disabilities is concerning, and shortfalls are developing across the range of pediatric physician-scientists.17
It is heartening that the majority of practicing child neurologists, neurodevelopmental disabilities specialists, and trainees would, given the choice, choose their fields again. However, that percentage has dropped from the 90% who reported similar sentiments in the previous survey in response to a similar but not identical question.1 As in many specialties, there are diminishing numbers of child neurologists and neurodevelopmental disabilities specialists practicing in independent practices, with only a small fraction of these functioning as owners, partners, or shareholders. A growing number are employed by hospitals or academic physician organizations, where they may be held to arduous accountability standards. This imbalance reduces practice options for child neurologists and neurodevelopmental disabilities specialists, and may limit physician leverage in negotiations to improve compensation or professional environments. Forces throughout the health care system are creating financial pressures and regulatory stresses on all physicians, but niche specialty areas such as child neurology and neurodevelopmental disabilities appear to bear a disproportionate burden.
The current study has certain limitations. The 38% overall response rate is substantially lower than the 65% rate in the landmark 2002 workforce study,1,14 suggesting that the current results could be influenced by an undefined selection bias. Four electronic reminders were e-mailed to eligible respondents in the current study, whereas 3 postal reminders were sent for the 2002 study.1 It is difficult to determine whether a postal survey would generate a higher response rate today, given the information overload from diverse sources. The response rate is within the accepted range for a web-based survey of clinicians, where response rates as low as 20% are not uncommon.18 A significant proportion of respondents trained before 1994, partially obscuring some of the demographic shifts that are apparent among younger specialists. The perspectives of referring providers and medical students were beyond the scope of this study, but those would have contributed an extra dimension to the data presented. The views of medical students would have been especially helpful for questions regarding the rationale behind career choices. The questions on competition in the current study did not specifically include competition from other child neurologists, a potential concern in large metropolitan areas with multiple academic medical centers. Finally, the current study did not address the nation's needs for clinician-scientists vs clinician-educators in child neurology and neurodevelopmental disabilities. This issue should be a focus of future workforce studies.
The fields of child neurology and neurodevelopmental disabilities continue to draw trainees who wish to devote their careers to the welfare of children and advance our knowledge of the developing nervous system, perhaps the most complex biological system in nature. However, pressures and threats to practice environments loom ever larger. Practicing specialists should help with recruitment and mentoring, and also advocate for better recognition of the value of their contributions. Child neurology and neurodevelopmental disabilities have lower visibility than some other specialties, and this may be especially pronounced among minority medical students. Academic child neurologists and neurodevelopmental disabilities specialists should make greater efforts to become involved in teaching activities at their medical schools, including first year courses when many strong impressions are made. Other issues to be addressed include overall workforce needs, medical education debt, compensation, support for independent medical practices, access to care in rural areas, and a strengthened pipeline of physician-scientists. Professional medical organizations can have a key role in these endeavors, including the CNS, AAP, and American Academy of Neurology, in collaboration with medical schools and the NIH. Professional organizations could draw more attention to the total value that child neurologists and neurodevelopmental disabilities specialists bring to health care systems, which is often not captured in traditional accountability calculations. Fostering the career development of young physician-scientists and child neurologists/neurodevelopmental disabilities specialists who actively collaborate with basic scientists will continue to be important, and new grant mechanisms and career development programs may help promote these goals. Formal programs to develop physician-scientists and future leaders will be a worthwhile investment for these fields.11,19,20
Supplementary Material
ACKNOWLEDGMENT
The taskforce members thank Lynn Colegrove, MBA, Manager of the AAP Section on Neurology, and Roger Larson, CAE, Executive Director of the CNS, for their assistance with organizing and distributing the survey and providing background information.
GLOSSARY
- AAP
American Academy of Pediatrics
- CNS
Child Neurology Society
Footnotes
Supplemental data at Neurology.org
Editorial, page 1318
AUTHOR CONTRIBUTIONS
Dr. Kang: study concept and design, analysis and interpretation, drafting and editing of the manuscript, study supervision. Dr. Bale: study concept and design, analysis and interpretation, drafting and editing of the manuscript. Dr. Mintz: study concept and design, analysis and interpretation, drafting and editing of the manuscript. Dr. Joshi: study concept and design, analysis and interpretation, critical revision of the manuscript for important intellectual content. Dr. Gilbert: study concept and design, analysis and interpretation, drafting and editing of the manuscript. Ms. Radabaugh: study concept and design, analysis and interpretation, critical revision of the manuscript for important intellectual content. Dr. Ruch-Ross: study concept and design, data acquisition, analysis and interpretation including statistical analysis, critical revision of the manuscript for important intellectual content.
STUDY FUNDING
This study was supported by the American Academy of Pediatrics and the Child Neurology Society.
DISCLOSURE
P. Kang served as an officer of the Massachusetts Medical Society and received honoraria from Genome British Columbia, the Muscular Dystrophy Association, the American Clinical Neurophysiology Society, the University of South Florida, C1 Consulting, HealthMatters CME, the American Academy of Pediatrics, and the University of Cambridge. He previously had grant funding from the Muscular Dystrophy Association and Catabasis Pharmaceuticals, and is currently funded by NIH R01 NS080929, Genzyme, and Pfizer. He is on the editorial boards of Pediatrics and Pediatric Neurology, has contracted with Springer to coedit a textbook, and receives royalties from UpToDate. He serves on an advisory board for Sarepta Therapeutics and on grant review panels for Fondazione Cariplo (Milan, Italy) and Fondazione Telethon (Milan, Italy). He performs EMG studies in his clinical practice (5% effort). J. Bale receives support from the Association of American Medical Colleges and Josiah Macy Jr. Foundation for studies of medical student education, a subcontract from Boston Children's Hospital for studies of family centered rounds, and book royalties from Taylor & Francis Group, UK. He has received honoraria for service on the MOC Assessment Task Force of the American Board of Pediatrics. M. Mintz serves on the editorial boards of the Journal of Child Neurology and Vision Development and Rehabilitation; has functioned as principal investigator for clinical trials research contracted through the Clinical Research Center of New Jersey, LLC (CRCNJ) sponsored by the following companies: Sunovion, Pfizer, Shire, Eisai Inc., and Allergan; is the principal investigator for research funded by the State of New Jersey through the Governor's Council for Medical Research and Treatment of Autism; is President, CEO, Founder, and sole proprietor of The Center for Neurological and Neurodevelopmental Health, LLC (CNNH) and CRCNJ; and is President of NeurAbilities, a 501(3)c public charity. S. Joshi is supported by HRSA MCHB Cooperative Agreement U23MC26252. D. Gilbert has received honoraria from the Tourette Syndrome Association, Centers for Disease Control and Prevention, and the American Academy of Pediatrics; has received book royalties from Elsevier, and one-time consulting fees for clinical trial design from Teva/Auspex Pharmaceuticals, and has received compensation for expert testimony for the US Department of Justice DVIC Program. He has received research support for the study of Tourette syndrome and attention-deficit/hyperactivity disorder from NIH R01MH092520, R01MH081854, R01MH104651, and R01NS085023, and for a clinical trial on Tourette syndrome from Ecopipam Pharmaceuticals. C. Radabaugh was a paid employee of the American Academy of Pediatrics, which funded the survey initiative, at the time of the study. H. Ruch-Ross reports no disclosures relevant to the manuscript. Go to Neurology.org for full disclosures.
REFERENCES
- 1.Polsky D, Weiner J, Bale JF Jr, Ashwal S, Painter MJ. Specialty care by child neurologists: a workforce analysis. Neurology 2005;64:942–948. [DOI] [PubMed] [Google Scholar]
- 2.Grover A, Orlowski JM, Erikson CE. The nations physician workforce and future challenges. Am J Med Sci 2016;351:11–19. [DOI] [PubMed] [Google Scholar]
- 3.Kim WJ; American Academy of Child and Adolescent Psychiatry Task Force on Workforce Needs. Child and Adolescent Psychiatry Workforce: a critical shortage and national challenge. Acad Psychiatry 2003;27:277–282. [DOI] [PubMed] [Google Scholar]
- 4.Oakley CB, Kossoff EH. Migraine and epilepsy in the pediatric population. Curr Pain Headache Rep 2014;18:402. [DOI] [PubMed] [Google Scholar]
- 5.Bale JF Jr, Currey M, Firth S, Larson R; Executive Committee of the Child Neurology Society. The Child Neurology Workforce Study: pediatrician access and satisfaction. J Pediatr 2009;154:602–606. e601. [DOI] [PubMed] [Google Scholar]
- 6.Brotherton SE, Etzel SI. Graduate medical education, 2014–2015. JAMA 2015;314:2436–2454. [DOI] [PubMed] [Google Scholar]
- 7.Deville C, Hwang WT, Burgos R, Chapman CH, Both S, Thomas CR Jr. Diversity in graduate medical education in the United States by race, ethnicity, and sex, 2012. JAMA Intern Med 2015;175:1706–1708. [DOI] [PubMed] [Google Scholar]
- 8.Wu YW, Xing G, Fuentes-Afflick E, Danielson B, Smith LH, Gilbert WM. Racial, ethnic, and socioeconomic disparities in the prevalence of cerebral palsy. Pediatrics 2011;127:e674–e681. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Marrast LM, Zallman L, Woolhandler S, Bor DH, McCormick D. Minority physicians' role in the care of underserved patients: diversifying the physician workforce may be key in addressing health disparities. JAMA Intern Med 2014;174:289–291. [DOI] [PubMed] [Google Scholar]
- 10.Cooper-Patrick L, Gallo JJ, Gonzales JJ, et al. Race, gender, and partnership in the patient-physician relationship. JAMA 1999;282:583–589. [DOI] [PubMed] [Google Scholar]
- 11.Milewicz DM, Lorenz RG, Dermody TS, Brass LF; National Association ofMD-PhD Programs Executive Committee. Rescuing the physician-scientist workforce: the time for action is now. J Clin Invest 2015;125:3742–3747. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Bradley WG. Neurology in the next two decades: report of the Workforce Task Force of the American Academy of Neurology. Neurology 2000;54:787–789. [DOI] [PubMed] [Google Scholar]
- 13.Laureta E, Moshe SL. State of training in child neurology 1997–2002. Neurology 2004;62:864–869. [DOI] [PubMed] [Google Scholar]
- 14.Werner RM, Polsky D. Comparing the supply of pediatric subspecialists and child neurologists. J Pediatr 2005;146:20–25. [DOI] [PubMed] [Google Scholar]
- 15.Dall TM, Storm MV, Chakrabarti R, et al. Supply and demand analysis of the current and future US neurology workforce. Neurology 2013;81:470–478. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Piedboeuf B, Jones S, Orrbine E, Filler G. Are the career choices of paediatric residents meeting the needs of academic centres in Canada? Paediatr Child Health 2012;17:17–20. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.Cornfield DN, Lane R, Abman SH. Creation and retention of the next generation of physician-scientists for child health research. JAMA 2013;309:1781–1782. [DOI] [PubMed] [Google Scholar]
- 18.Dykema J, Jones NR, Piche T, Stevenson J. Surveying clinicians by web: current issues in design and administration. Eval Health Prof 2013;36:352–381. [DOI] [PubMed] [Google Scholar]
- 19.Hromas R, Abkowitz JL, Keating A. Facing the NIH funding crisis: how professional societies can help. JAMA 2012;308:2343–2344. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20.Griffin JW, Griggs RC, Barchi R, Schneck SA, Moses H III. Opportunities and challenges in academic neurology: report of the Long Range Planning Committee of the American Neurological Association. Ann Neurol 1996;39:693–699. [DOI] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.