Abstract
Objective
In the case of high erythrocyte sedimentation rate (ESR) and C-reactive protein (CRP) levels, the diagnosis of the underlying disease can be challenging especially in serologically unrevealing patients who have nonspecific clinical findings. We aimed to investigate the final distribution of definitive diagnoses in patients who initially presented with nonspecific clinical findings and sustained elevations in serum ESR/CRP levels.
Material and Methods
The medical records of patients hospitalized in a rheumatology clinic between January 2010 and January 2011 were retrospectively analyzed. The patients were classified into two main groups: those with previously diagnosed underlying rheumatic disease (RD) and those without. The groups were analyzed for the final distribution of definitive diagnoses.
Results
Out of 112 patients in the general study population, 47 had a previous RD and 65 had no previous history of RD. In these 65 patients, the most common etiology of nonspecific elevations in ESR/CRP levels was new onset RD (52.3%). Polymyalgia rheumatica (PMR) was the most common new onset RD (38% of all new onset RD) followed by seronegative rheumatoid arthritis. The incidences of infections and malignancies were 24.6% and 9.2%, respectively. CRP levels were significantly higher in infections when compared with new onset RD or malignancies (p<0.05). In patients with previous RD, the flare of the underlying disease was the most common etiology of nonspecific elevations in ESR/CRP levels (n=39, 83%, 20 female/19 male).
Conclusion
Extraordinarily high levels of serum CRP in a patient with nonspecific clinical findings should raise suspicion for non-rheumatic diagnoses, such as infection and malignancy, even in the presence of a previously diagnosed RD. Advanced radiological investigation is justified in these cases to rule out malignancy.
Keywords: Blood sedimentation, C-reactive protein, rheumatology
Introduction
Erythrocyte sedimentation rate (ESR) and C-reactive protein (CRP) levels are among the most commonly used acute phase reactants in the detection and follow-up of disease activity in rheumatology clinics. Although they are called acute phase reactants, they accompany both acute and chronic inflammatory conditions (1).
In our university-based, tertiary-referral rheumatology clinic, we observed that a substantial number of our patients initially presented with a combination of nonspecific clinical findings and sustained elevations of serum ESR/CRP levels. This vague presentation can become a diagnostic challenge especially if the rheumatologic serologies are unrevealing. These patients often require extensive investigations to rule out other major causes of elevated serum ESR/CRP levels such as infection and malignancy. Although no patient is left undiagnosed, the pathway to definitive diagnosis significantly varies from one patient to another. In the current era of evidence-based medicine, a physician can be held accountable for every decision that he/she makes, and clinical guidelines are more important than ever. There is no widely accepted guideline for the management of this presentation type in rheumatology clinics. Although it is not our intention to come up with a clinical guideline at this point, we believe that the outcome data presented in this study will serve as a cornerstone in the construction of one. Our study investigates the final distribution of definitive diagnoses in patients who initially presented with nonspecific clinical findings and sustained elevations in serum ESR/CRP levels. To our knowledge, there is no prior study that investigated this relationship from a rheumatologist’s perspective.
Material and Methods
Between January 2010 and January 2011, a total of 124 patients were hospitalized in our university-based, tertiary-referral rheumatology clinic for further diagnostic investigation after their initial presentation with nonspecific clinical findings and elevated serum CRP/ESR levels. All patients had sustained elevations in serum ESR/CRP levels at the time of hospitalization. Usually, patients who have arthralgia, fatigue, or flare of their rheumatic disease (RD) such as rheumatoid arthritis do not require admission to hospital; however, in our center, we prefer to hospitalize these patients when their symptoms are severe or when it is not easy to perform the diagnostic work-up in the outpatient clinic. Checking serum ESR and CRP levels in all patients is a routine test in our rheumatology outpatient clinic. The reference ranges for normal CRP and ESR levels in our institution were 0–6 mg/L and 0–20 mm/h, respectively.
Only the first “diagnostic” hospitalizations were included in our study. Patients with insufficient data in their medical records were excluded (8 patients). Four patients with chronic kidney disease were also excluded because of the different dynamics of the acute phase reactants in this group.
The electronic medical records of the remaining 112 patients were retrospectively reviewed for patient demographics, ESR and CRP levels at the time of hospitalization and discharge, radiology reports, laboratory tests, microbiological cultures, and reports of histopathological samples.
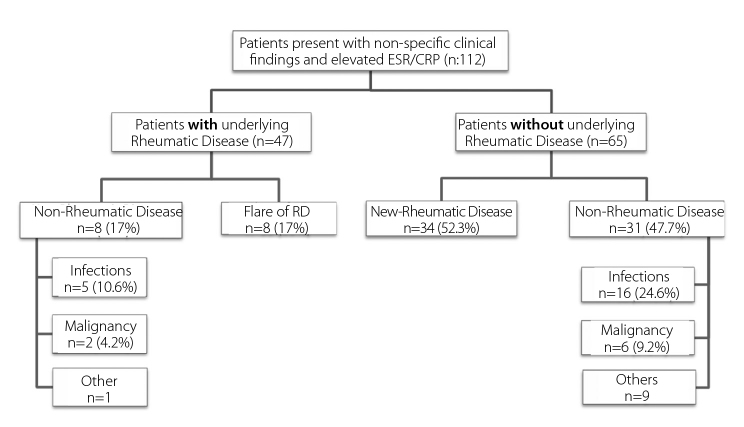
The patients were classified into two main groups: those with previously diagnosed underlying RD and those without (Figure 1). The groups were analyzed for the final distribution of definitive diagnoses. Within each group, differences in patient age and ESR and CRP levels were compared between RD, infections, and malignancies. Approval from the ethics committee was not required for this retrospective study.
Figure 1.
Distribution of definitive diagnoses in patients with nonspecific clinical findings and elevated serum ESR & CRP levels
SPSS for windows version 15.0 (SPSS Inc; Chicago, IL, USA) was used for statistical analyses. Median ESR/CRP levels in infection, malignancy, and new RD/flare groups were compared with Kruskal-Wallis test. For post-hoc comparisons of medians and percentages, Mann-Whitney U test was used. A p<0.05 was accepted to be statistically significant.
Results
Of the 112 patients, 83 were female and 29 were male. The mean (±SD) duration of hospitalization was 13 (±7) days. The chief complaint at the time of presentation was fatigue/arthralgia in 45 patients, back pain in 20, and arthritis in 25. Other chief complaints included fever of unknown origin, skin lesions, and blindness.
Patients with Previously Diagnosed Underlying RD Group
Out of the 112 patients in the general study population, 47 had a previous rheumatologic diagnosis. In these patients, the most common etiology of nonspecific elevations in ESR/CRP levels was the flare of underlying disease (n=39, 83%, 20 female/19 male). The previous diagnoses were rheumatoid arthritis [26], ankylosing spondylarthritis [4], systemic lupus erythematosus (SLE) [2], granulomatosis with polyangiitis [2], Behçet’s disease [2], giant cell arteritis [2], and mixed connective tissue disorder [1]. The average age in this group was 56 years (range 32–81). The most common RD to flare was rheumatoid arthritis (66% of all flares). The incidences of infections and malignancies were 10.6% and 4.2%, respectively. In this group, infections presented at a significantly older age when compared with the flare of RD (p=0.02). In this group, ESR and CRP levels were significantly higher in malignancies when compared with the flare of RD (p<0.05) (Table 1).
Table 1.
Characteristics of patients with underlying rheumatic disease
| Flare n=39 | Infections n=5 | Malignancy n=2 | Significance p | |
|---|---|---|---|---|
| Age (median; min-max) | 48.5 (18–83) | 70 (45–75) | 59.5 (59–60) | 0.051* |
| ESR (median; min-max) | 66 (20–108) | 72 (32–77) | 130 (120–140) | 0.060** |
| CRP (median; min-max) | 32.5 (3–192) | 63 (9–119) | 235 (153–317) | 0.071*** |
In post-hoc analyses,
p=0.026 flare vs. infections.
p=0.018 flare vs. malignancy,
p=0.025 flare vs. malignancy.
ESR: erythrocyte sedimentation rate; CRP: C-reactive protein
Patients without Previously Diagnosed Underlying RD Group
Out of the 112 patients in the general study population, 65 had no previous history of rheumatologic diagnosis. In these 65 patients, the most common etiology of nonspecific elevations in ESR/CRP levels was new onset RD (n=34, 52.3%, 25 female/9 male). The average age in this group was 56 years (range 21–83). Polymyalgia rheumatica/giant cell arteritis was the most common new onset RD [38% of all new onset RD followed by seronegative rheumatoid arthritis (Table 2)]. Although new onset RD (52.3%) was the most common etiology of nonspecific elevations in ESR/CRP levels in this group, non-rheumatic diagnoses were almost as prevalent (47.7%). The incidences of infections and malignancies were 24.6% and 9.2%, respectively. CRP levels were significantly higher in infections when compared with new onset RD or malignancies (p<0.05) (Table 3).
Table 2.
Distribution of new rheumatic diagnoses (n=34)
Table 3.
Characteristics of patients without underlying rheumatic disease
| New rheumatic n=34 | Infections n=16 | Malignancy n=6 | p | |
|---|---|---|---|---|
| Age (median; min-max) | 58 (21–83) | 57 (25–84) | 48 (32–72) | ns |
| ESR (median; min-max) | 67.5 (8–120) | 78.5 (30–109) | 71 (40–100) | ns |
| CRP (median; min-max) | 29.5 (10–109) | 75 (12–394) | 35.5 (9–75) | 0.01* |
In post-hoc tests, newly diagnosed rheumatic disease vs. infection p=0.003
ESR: erythrocyte sedimentation rate; CRP: C-reactive protein
Distribution of Non-Rheumatic Diagnoses in General Study Population
In the general study population (n=112), a total of 39 patients (23 female, 16 male) received non-rheumatic diagnoses. The average age in this group was 52 years (range 20–75). Non-rheumatic diagnoses were infections [21], malignancies [8], sarcoidosis [4], gastrointestinal diseases [3], and other causes [3] (Table 4). The mean ESR level was 75 (30–109) for infections and 85.7 (40–140) for malignancies. The mean CRP level was 72 (9–394) for infections and 85 (9–317) for malignancies.
Table 4.
Distribution of non-rheumatic diagnoses
| Diagnoses | Description (n) |
|---|---|
| Infections | Urinary [5], Pneumonia [5], Osteomyelitis [2], Fasciola hepatica [1], Acute rheumatic fever [2], Infective endocarditis [3], Neurobrucellosis [1], Prosthetic joint infection [1], PID *[1] |
| Malignancy | Ovarian cancer, Lymphoma [3], Multiple myeloma, Fibrosarcoma, Extramedullary myeloid tumor, small cell lung cancer |
| Gastrointestinal | Celiac disease, Crohn’s disease, Non-alcoholic steatohepatitis |
| Sarcoidosis | Sarcoidosis |
| Others | Gitelman syndrome, Madelung’s syndrome, Sneddon’s syndrome |
PID: pelvic inflammatory disease
Cultures were obtained from 111 patients (98.2%), including blood cultures in 50 (44.2%). In 16 of the 21 patients with infection (76%), a causative pathogen could be identified. The identified pathogens in this group were Staphylococcus aureus (n=4), Escherichia coli (n=7), Fasciola hepatica (n=1), Streptococcus pneumoniae (n=2), Brucella (n=1), and Cytomegalovirus (n=1). In 5 patients, although a specific pathogen could not be identified by cultures or serology, there was a strong clinical suspicion in favor of an infectious etiology. The criteria in those patients were good clinical and acute phase reactant response to empirical antibiotic therapy. No mortality was seen in any patient during hospitalization in the rheumatology clinic.
In total, 8 out of 112 patients (7.1%) who were hospitalized for nonspecific symptoms and high ESR and CRP levels had been diagnosed with malignancy. Of these 8 patients, 2 had a previous history of RD (SLE and rheumatoid arthritis). The symptoms in the malignancy group were nonspecific. Acute onset inflammatory low back pain was the major complaint in 3 out of 8 patients with malignancy. Peripheral blood smears were not helpful for the diagnosis in lymphoma patients. Radiology was the mainstay of diagnosis for patients with malignancy (Table 5).
Table 5.
Characteristics of patients with malignancy and tests performed
| Age/gender | Medical History | Clinical presentation | ESR* | CRP* | Test** | Diagnosis |
|---|---|---|---|---|---|---|
| 72, M | Unremarkable | Arthralgia, skin rash | 72 | 49 | Thorax CT | Small cell lung cancer |
| 32, F | Unremarkable | Back pain*** | 40 | 75 | Sacroiliac MRI | Burkitt’s lymphoma |
| 60, F | SLE | Polyarthritis | 120 | 153 | Thorax CT | B-cell lymphoma |
| 44, M | Unremarkable | Fatigue, Numbness in legs | 81 | 16 | Radiography, Bone marrow biopsy | Multiple myeloma |
| 58, F | Unremarkable | Fever, Arthralgia | 83 | 30 | Thorax CT Abdomen CT |
Non-Hodgkin lymphoma |
| 59, F | Rheumatoid arthritis | Fatigue | 140 | 317 | Pelvic USG | Ovarian cancer |
| 44, F | Myelofibrosis | Back pain*** | 100 | 68 | Abdomen CT | Extramedullary myeloid tumor |
| 52, F | Unremarkable | Back pain*** | 61 | 41 | Abdomen CT | Retrorectal solitary fibrosarcoma |
Levels on the first day of hospitalization
Test that resulted in the diagnosis
Inflammatory low back pain occurring within one month.
M: male; F: female
CT: computed tomography; MRI: Magnetic resonance imaging; ESR: erythrocyte sedimentation rate; CRP: C-reactive protein; SLE: systemic lupus erythematosus; USG: ultrasonography
Discussion
RDs often present with nonspecific clinical findings that may be confused or overlapped with those of non-rheumatologic diseases such as infections and malignancies. In patients with nonspecific clinical presentations, serology can be helpful; however, it does not necessarily lead to a definitive diagnosis. ESR and CRP are among the most widely used inflammatory markers for the detection and follow-up of disease activity in current rheumatology practice (2). In our practice, we observed that a steady subset of our initial presentations were characterized by nonspecific clinical findings and elevated serum acute phase reactants. This type of initial presentation was considered worthy of further investigation because of the variety and severity of eventual non-rheumatologic diagnoses associated with it.
In the study population, the most common causes of elevated ESR and CRP levels were flare of RD, newly diagnosed RD, infection, and malignancy. Although ESR and CRP levels have a very low specificity in differentiating between these conditions, in cases of unusually high levels of CRP (especially above 200), more consideration should be given to infections or malignancies. It is generally accepted that a CRP level between 10 and 100 mg/L indicates a moderate increase and a level greater than 100 mg/L reflects a marked increase (3, 4). Levels exceeding 500 mg/L are found to be associated with bacterial infections in 88% of the patients in a study (5).
In our study population, PMR was the most common new onset RD. The differential diagnosis between PMR and rheumatoid arthritis can be difficult because these conditions may have a similar clinical presentation, especially in the elderly (6). Normal ESR and CRP levels virtually rule out PMR or giant cell arteritis (7). PMR is classically known as a diagnosis of exclusion. Therefore, a rheumatologist should also have a sound knowledge of non-rheumatic differential diagnoses. Our study will guide daily rheumatology practice by defining “what else to expect.”
The threshold for advanced radiological investigation should be kept low for any patient who presents with nonspecific clinical findings and elevated acute phase reactants. In our study, computed tomography and magnetic resonance imaging had a high diagnostic accuracy in the detection of malignancies. Two of our patients who had previous rheumatic diagnoses were diagnosed with malignancies. ESR and CRP levels were significantly higher in those patients when compared with patients in the flare group. Our study underlines the fact that malignancy can coexist with previously diagnosed RDs and that it can easily be overlooked in this rare occurrence. Therefore, we suggest that in patients with previous rheumatic diagnoses, unexpectedly high levels of serum inflammatory markers should warn the physician to rule out non-rheumatic conditions such as infection or malignancy before concluding with rheumatic etiologies such as disease reactivation or resistance to therapy.
Acute onset low back pain should be a warning sign because 3 out of 8 patients in the malignancy group presented with this chief complaint. In rheumatology clinics, inflammatory back pain was generally associated with ankylosing spondylarthritis. However, we should keep in mind that the duration of back pain should be more than 3 months for the diagnosis of ankylosing spondylarthritis (8). The diagnostic evaluation of back pain requires a systematic approach. Blood tests usually help rule out a systemic inflammatory condition from mechanic causes such as disc hernias or spinal stenosis (9).
Our study has some limitations. This study was designed as a retrospective cross-sectional analysis that aimed to correlate ESR and CRP levels at the time of initial rheumatology consultation with the final definitive diagnosis. Because this is not an outcome study, the long term follow-up of patients and longitudinal assessments of ESR and CRP levels were not included. The distribution of initial presentations and definitive diagnoses were closely influenced by the characteristics of the study population. If a similar study was conducted in a primary care setting, the distribution of definitive diagnoses may have been largely different, probably inclined to infectious etiologies.
Extraordinarily high levels of serum CRP in a patient with nonspecific clinical findings should raise a suspicion for non-rheumatic diagnoses, such as infection and malignancy, even in the presence of a previously diagnosed RD. Advanced radiological investigation is justified in these cases to rule out malignancy. Future studies are needed for the development of clinical algorithms and diagnostic guidelines in this group of patients.
Footnotes
Ethics Committee Approval: N/A.
Informed Consent: N/A.
Peer-review: Externally peer-reviewed.
Author Contributions: Concept - B.B.; Design - B.B.; Supervision - B.G., A.T.; Materials - B.B., R.M.; Data Collection and/or Processing - B.B.; Analysis and/or Interpretation - B.B., M.E.T., M.N.İ.; Literature Review - B.B.; Writer - B.B.; Critical Review - Ş.H., M.A.Ö.
Conflict of Interest: No conflict of interest was declared by the authors.
Financial Disclosure: The author declared that this study has received no financial support.
References
- 1.Firestein Gary S, Budd Ralph C, Gabriel Sherine E, Mcınnes Iain B, O’Dell James R. Kelley’s Textbook of Rheumatology. Saunders; 2012. Acute Phase Reactants and the Concept of Inflammation; pp. 818–29. [Google Scholar]
- 2.Amezcua-Guerra LM, Castillo-Martinez D, Bojalil R. The story behind the acute-phase reactants. J Rheumatol. 2010;37:469. doi: 10.3899/jrheum.090991. http://dx.doi.org/10.3899/jrheum.090991. [DOI] [PubMed] [Google Scholar]
- 3.Morley JJ, Kushner I. Serum C-reactive protein levels in disease. Ann N Y Acad Sci. 1982;389:406–18. doi: 10.1111/j.1749-6632.1982.tb22153.x. http://dx.doi.org/10.1111/j.1749-6632.1982.tb22153.x. [DOI] [PubMed] [Google Scholar]
- 4.Macy EM, Hayes TE, Tracy RP. Variability in the measurement of C-reactive protein in healthy subjects: implications for reference intervals and epidemiological applications. Clin Chem. 1997;43:52–8. [PubMed] [Google Scholar]
- 5.Vanderschueren S, Deeren D, Knockaert DC, Bobbaers H, Bossuyt X, Peetermans W. Extremely elevated C-reactive protein. Eur J Intern Med. 2006;17:430–3. doi: 10.1016/j.ejim.2006.02.025. http://dx.doi.org/10.1016/j.ejim.2006.02.025. [DOI] [PubMed] [Google Scholar]
- 6.Kermani TA, Warrington KJ. Polymyalgia rheumatica. Lancet. 2013;381:63–72. doi: 10.1016/S0140-6736(12)60680-1. http://dx.doi.org/10.1016/S0140-6736(12)60680-1. [DOI] [PubMed] [Google Scholar]
- 7.Martinez-Taboada VM, Blanco R, Rodriguez-Valverde V. Polymyalgia rheumatica with normal erythrocyte sedimentation rate: clinical aspects. Clin Exp Rheumatol. 2000;18( 4 Suppl 20):34–7. [PubMed] [Google Scholar]
- 8.Zeidler H, Amor B. The Assessment in Spondyloarthritis International Society (ASAS) classification criteria for peripheral spondyloarthritis and for spondyloarthritis in general: the spondyloarthritis concept in progress. Ann Rheum Dis. 2011;70:1–3. doi: 10.1136/ard.2010.135889. http://dx.doi.org/10.1136/ard.2010.135889. [DOI] [PubMed] [Google Scholar]
- 9.Deyo RA, Weinstein JR. Low back pain. N Engl J Med. 2001;344:363–70. doi: 10.1056/NEJM200102013440508. http://dx.doi.org/10.1056/NEJM200102013440508. [DOI] [PubMed] [Google Scholar]