Abstract
Objective
We sought to determine the prevalence of and factors associated with self-medication in patients with rheumatic diseases.
Material and Methods
An analytical cross-sectional study was conducted from February to July 2013 in the rheumatology department. We included all patients who consulted for a rheumatic disease during the study period and who gave their consent.
Results
In total, 203 patients were included; of these, 146 patients (71.92%) had practiced self-medication. Furthermore, 99 patients (48.8%) had practiced self-medication for rheumatologic problems. The mean age of the patients was 45.5 years (range: 18–75 years). State officials accounted for 44.4% of patients. Eighty-one patients were schooled. Low back pain (29.29%) was the main reason for consultation, followed by polyarthralgia (12.12%). Using a visual analogue scale, the level of pain for which patients had used self-medication was rated as >70 out of 100 in 57.6% of patients. Fifty-five patients often self-medicated and 28 patients rarely. Drugs were bought from the pharmacy in 97% of cases. The main channel of self-medication was word of mouth (43.4%). The drugs used were mainly anti-inflammatory drugs (diclofenac: 54.54% and ibuprofen: 57.57%). Ten patients were unaware of the risks of self-medication. In multivariate analysis, sex, education level, and occupation were statistically associated with self-medication.
Conclusion
Self-medication for a specific rheumatologic symptom appears less common than self-medication in general. The procedures for responsible self-medication should be defined in Burkina Faso in order to minimize the risks.
Keywords: Self-medication, rheumatology, risk factors
Introduction
The World Health Organization (WHO) defines self-medication as practices by which people deal with aches and health conditions with drugs that are approved and available without prescription and are safe and effective when used according to inscriptions (1). In addition, self-medication is called anarchic when treating a real or imagined pathological situation by drugs selected without medical advice or without consulting a health care professional in his area of competences (1). Rheumatic disease is a source of pain and disability that promotes responsible or anarchic self-medication. In France, 80% of the population uses self-medication and 20% of the population suffers from rheumatic diseases (2). In sub-Saharan Africa, the existing data mainly concern the overall self-medication rate, which varies from 11.9% to 75.7% (3, 4). Self-medication appears to be more common in women and is associated with a low socioeconomic level. To the best of our knowledge, no study has investigated self-medication in rheumatology in sub-Saharan Africa countries. The purpose of this study was to describe the prevalence of and factors associated with self-medication in rheumatology in a sub-Saharan African country.
Material and Methods
An analytical cross-sectional study was conducted from February to July 2013 in the rheumatology department. All patients aged over 15 years who presented during the study period for rheumatologic diseases and who gave their consent were included in the study. We did not include patients who forgot the medications taken. All patients were asked about their practice of self-medication. Data were collected using a questionnaire that included questions related to socio-demographic characteristics (age, sex, occupation), diagnosis, performance of patients on self-medication (definition, period, rhythm, and motivation), and role of health professionals according to self-medication (guide, application of pharmaceutical advice). The level of pain was assessed using a visual analogue scale. All patients underwent complete clinical examination by a rheumatologist and further investigations if necessary.
Statistical analysis
The data were entered using Epi Data software version 3.1 and analyzed with SPSS Version 21. The significance level of 0.05 was used.
Results
Patients characteristics
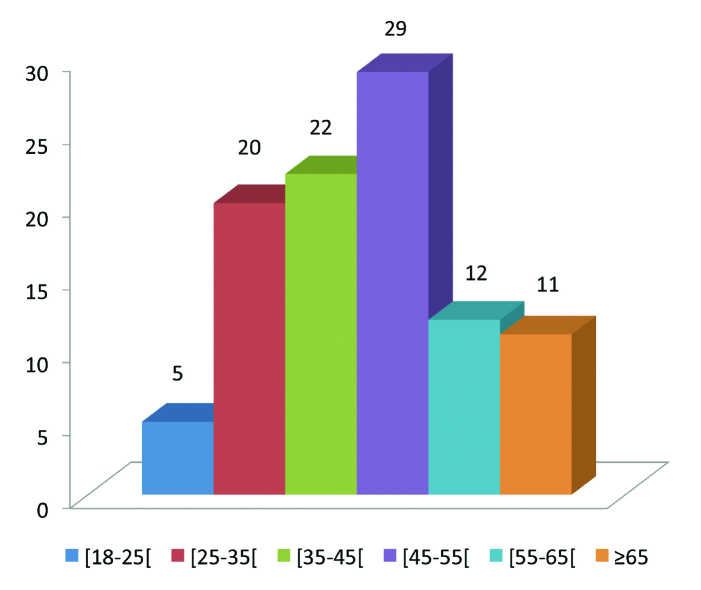
In total, 203 patients were included in the study during the study period. They were 156 women and 47 men, with a sex ratio of 0.32. Of these 203 patients, 146 (71.92%) had practiced self-medication in general, whereas 99 (48.80%) patients had used self-medication for a rheumatic disease. The mean age of these patients was 45.5±13.5 years (range: 18–75 years). The age group of 45–55 years was more represented. The distribution of patients by age group is shown in Figure 1. State officials (44 patients) accounted for 44.4% of patients, whereas housewives and traders accounted for 16.2% and 8.1% of patients, respectively.
Figure 1.
Distribution of patients number according age (years) groups
Eighty-one patients were schooled. Of these, 20.2%, 50.5%, and 11.1% had education up to the high school level, secondary school level, and primary school level (p<0.05), respectively. Comorbidities were represented by peptic ulcer in 7 patients (7.1%), kidney diseases in 5 patients (5.1%), and liver disease in 3 patients (3%). Reported diagnoses were dominated by low back pain (29.29%) and osteoarthritis of knee (12.12%). Table 1 shows the distribution of patients according to the final diagnosis. On the visual analog scale, the level of pain was >70 in 57.6% of patients, between 40 and 70 in 30.3% of patients, and <40 in 12.1% of patients.
Table 1.
Diagnosis of patients practicing self-medication
| Number | Percentage | |
|---|---|---|
| Low back pain | 29 | 29.29 |
| Osteoarthritis of the knee | 12 | 12.12 |
| Rheumatoid arthritis | 10 | 10.10 |
| Ankylosing spondylitis | 6 | 6 |
| Connectivitis | 5 | 5.05 |
| Undetermined spondyloarthropathy | 4 | 4 |
| Polyarthrosis | 3 | 3.03 |
| Gouty arthritis | 3 | 3.03 |
| Osteoarthritis of the hip | 2 | 2.02 |
| Infectious spondylitis | 2 | 2.02 |
| Carpal tunnel syndrome | 2 | 2.02 |
| Tendinopathy of the rotator cuff | 2 | 2.02 |
| Sickle cell crisis | 1 | 1.01 |
| Necrosis of the femoral head | 1 | 1.01 |
| Osteoarthritis of the glenohumeral joint | 1 | 1.01 |
| Polymyalgia rheumatica | 1 | 1.01 |
| de Quervain tenosynovitis | 1 | 1.01 |
| Kneck osteoarthritis | 1 | 1.01 |
| Diagnosis not established | 13 | 13.13 |
| Total | 99 | 100 |
Characteristics of self-medication
Definition
Fifty-six patients (56.6%) defined self-medication as the act of self-care without going to the doctor. Table 2 shows the distribution of patients according to their definition of self-medication.
Table 2.
Distribution of patients according to the definition of self-medication
| Number* | Percentage | |
|---|---|---|
| Heal yourself without going to the doctor | 56 | 56.6 |
| I do not know | 34 | 34.3 |
| Doctor’s prescriptions | 10 | 10.1 |
| Use an old prescription | 6 | 6.1 |
Multiple answers are possible
Period
Seventy-nine patients (79.8%) engaged in self-medication before rheumatology consultation. Two patients practiced self-medication after consultation and 18 (18.2%) practiced self-medication before and after consultation (p<0.05).
Frequency, source, motivation, and channel of self-medication
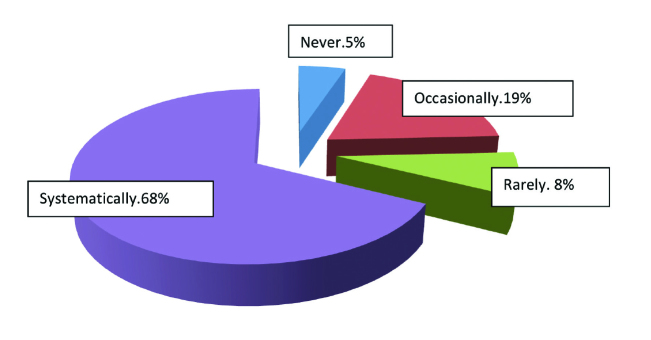
Fifty-five patients (55.5%) had often practiced self-medication, 28 (28.3%) had rarely practiced self-medication, and 16 (16.2%) had practiced casual self-medication. Drugs were bought from the pharmacy in 89% of cases and from the black market in 11% of cases. Thirty-nine patients (39.4%) said that they had used extra traditional medicines. Fifty-two patients (52.5%) were motivated by symptoms already known. Word of mouth (45.5%) was the most widely used channel. Table 3 lists the motivations and channels of self-medication. Drugs taken in self-medication were dominated by anti-inflammatory drugs. Table 4 shows the distribution of patients by the type of drugs. Ten patients (10.1%) were unaware of the risk associated with self-medication. Sixty-seven (67.7%) patients never asked for advice in pharmacies. Figure 2 illustrates the application of pharmaceutical advice through self-medication in rheumatology.
Table 3.
Guides for self-medication
| Number* | Percentage | |
|---|---|---|
| Word of mouth | 43 | 43.4 |
| Old prescriptions | 34 | 34.3 |
| Doctor’s advice | 22 | 22.2 |
| Drugs manual | 11 | 11.1 |
| Advice of pharmacist | 8 | 8.1 |
| Health articles | 2 | 2 |
| Media | 2 | 2 |
| Internet | 1 | 1 |
| Others | 7 | 7.1 |
Multiple answers are possible
Table 4.
List of drugs used for self-medication
| Number* | Percentage | |
|---|---|---|
| Paracetamol | 60 | 60.60 |
| Ibuprofen | 57 | 57.57 |
| Diclofenac | 54 | 54.54 |
| Tramadol | 6 | 6.06 |
| Topical ketoprofen | 5 | 5.05 |
| Niflumic acid | 3 | 3.03 |
| Paracetamol+codeine | 2 | 2.02 |
| Salicylic acid | 1 | 1.01 |
| Prednisone | 1 | 1.01 |
| Paracetamol+caffeine | 1 | 1.01 |
| Paracetamol+vitamin c | 1 | 1.01 |
| Paracetamol+tramadol | 1 | 1.01 |
Multiple answers are possible
Figure 2.
Pharmaceutical consulting request
Risk factors
In multivariate analysis, sex, education level, and occupation of the patients were statistically associated with self-medication. Table 5 shows the distribution of patients according to the factors associated with self-medication.
Table 5.
Factors associated with self-medication in rheumatologic diseases
| Number (n) | % AMAR* | OR (IC 95%) | p** | |
|---|---|---|---|---|
| Age (years) | ||||
| <45 | 62 | 45.2 | ||
| 45–55 | 96 | 51.0 | - | 0.770 |
| >55 | 45 | 48.9 | ||
|
| ||||
| Gender | ||||
| Male | 47 | 66.0 | 2.51 (1.27–4.95) | 0.007 |
| Female | 156 | 43.6 | 1 | |
|
| ||||
| Education level | ||||
| Not schooled | 47 | 38.3 | 1 | |
| Primary school | 31 | 35.5 | 0.53 (0.24–1.16) | 0.034 |
| Secondary school | 83 | 60.2 | 2.20 (1.24–3.89) | |
| High school | 42 | 47.6 | 0.94 (0.48–1.86) | |
|
| ||||
| Visual analogue scale | ||||
| Mild pain | 32 | 46.9 | ||
| Moderate pain | 94 | 47.9 | - | 0.912 |
| Intense pain | 77 | 50.6 | ||
|
| ||||
| Profession | ||||
| Official | 68 | 64.7 | 2.67 (1.46–4.88) | |
| Retired | 30 | 26.7 | 0.33 (0.14–0.78) | |
| Housewife | 27 | 59.3 | 1.63 (0.72–3.71) | |
| Trader | 22 | 36.4 | 0.57 (0.23–1.41) | |
| Informal sector | 17 | 35.3 | 0.55 (0.19–1.54) | 0.007 |
| Students | 17 | 29.4 | 1 | |
| Farmer | 13 | 53.8 | 1.24 (0.40–3.84) | |
| Unemployed | 9 | 55.6 | 1.33 (0.35–5.10) | |
Self-medication;
Probability
Discussion
The frequency of self-medication in general was 71.92%; it was higher than that for a specific rheumatologic symptom (48.80%). The frequency of self-medication for a rheumatic disease has been little studied; it was 65% in the studies conducted in France and Spain (2, 5). The frequency of self-medication in general ranges from 11.9% to 75.7% depending on the country (3, 4, 6–10). The mean age of patients who practiced self-medication for rheumatic diseases was 45.5 years, which is lower than that reported by a study conducted in France (65 years) (2). This mean age was similar to that of patients generally observed in the rheumatology department (11). Three factors appear to be statistically associated with self-medication for rheumatic diseases (gender, education level, and occupation) in our study. Female predominance has been reported in several studies (5). Although our sample was dominated by women (76.8%), self-medication for rheumatic diseases was significantly practiced by men (66%); this could be explained by the fact that men are better educated in our country. Furthermore, 60% of patients in our study with high school-level education had practiced self-medication; a study in the elderly in urban areas in Mexico reported that self-medication was statistically associated with illiteracy or low education level (8). This association is questionable because 92.50% of patients practicing self-medication in general in Congo were educated, with 12.92% having university-level education (4). Self-medication appears to be a complex phenomenon probably integrating socio-cultural habits of patients with a tendency to self-support for health problems they believe to be minor.
As most rheumatologic diseases are dominated by pain, the most commonly used drugs are anti-inflammatory (5, 12); however, the side effects and risks of this therapeutic class appear to be little or poorly understood by many rheumatologic patients (13). These risks are related to the lack of possible control of dosages, duration of treatment, drug interactions, allergic or iatrogenic effects, and comorbidities. The frequency of self-medication appears to decrease after consultation. It can be useful to temporarily alleviate a major disorder with short-term medication; on the contrary, it becomes dangerous if it takes long to see a doctor (14). Self-medication should be regulated by patient education, including relevant information about their disease and its treatment. Professionals in the health care field (doctors, pharmacists) have an important role to play.
Our study has limitations. We conducted this study in an urban setting and therefore the conclusions drawn here may not be applicable to rural areas. We relied on self-reported data collected using a questionnaire through an interview, which may underestimate the prevalence of self-medication.
Self-medication for rheumatologic symptoms appears to be less common than self-medication in general. Its definition is unclear and patients are guided by word of mouth. Self-medication appears to be associated with male gender and high level of education. The procedures for responsible self-medication should be defined in Africa in order to minimize the risks.
Footnotes
Ethics Committee Approval: Ethics committee approval was received for this study from the local Research Ethics Committee.
Informed Consent: Informed consent was obtained from patients who participated in this study.
Peer-review: Externally peer-reviewed.
Author Contributions: Concept - O.D.D., Z.T.W.J., Z.E.; Design - O.D.D., K.G.K.; Supervision - D.Y.J., G.P.I.; Materials - O.D.D., Z.T.W.J.; Data Collection and/or Processing - Z.E., K.F.; Analysis and/or Interpretation - O.D.D., Z.T.W.J.; Literature Review - K.G.K., K.F.; Writer - O.D.D., Z.T.W.J.; Critical Review - D.Y.J., G.P.I.
Conflict of Interest: No conflict of interest was declared by the authors.
Financial Disclosure: The authors declared that this study has received no financial support.
References
- 1.World Health Organiation. Guidelines for the regulatory assessment of medicinal products for use in self-medication. Geneva (CH): WHO; 2000. p. 31. Report No: WHO/EDM/QSM/001. [Google Scholar]
- 2.Hesbert A, Louis V, Curis E, Briot K, Gossec L, Poireaudeau S, et al. Automédication en rhumatologie. Le pharmacien hospitalier et clinicien. 2012;47:48. http://dx.doi.org/10.1016/j.phclin.2011.12.116. [Google Scholar]
- 3.Ocan M, Bwanga F, Blosa GS, Bagenda D, Waako P, Ogwal-Okeng J, et al. Patterns and predictors of self-medication in Northern Uganda. Plos One. 2014;9:e92323. doi: 10.1371/journal.pone.0092323. http://dx.doi.org/10.1371/journal.pone.0092323. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Mouankié JB, Mazonga B, Abena AA. L’automédication chez l’adulte à Brazzaville. Sci Med Afr. 2011;3:459–63. [Google Scholar]
- 5.Riedemann JP, Illesca M, Droghetti J. Self-medication among patients with musculoskeletal symptom in Araucania region. Rev Med Chil. 2001;129:647–52. [PubMed] [Google Scholar]
- 6.Yousef AM, Al-Bakri AG, Bustanji Y, Wazaify M. Self-medication patterns in Amman, Jordan. Pharm World Sci. 2008;30:24–30. doi: 10.1007/s11096-007-9135-x. http://dx.doi.org/10.1007/s11096-007-9135-x. [DOI] [PubMed] [Google Scholar]
- 7.Ylinen S, Hamen-anttila K, Seppomen K, Lindblad AK, Ahonen R. The use of prescription medicines and self-medication among children. A population-base study in Finland. Pharmaco Epidemiol Drug Saf. 2010;19:1000–8. doi: 10.1002/pds.1963. http://dx.doi.org/10.1002/pds.1963. [DOI] [PubMed] [Google Scholar]
- 8.Balbuena FR, Ananda AB, Figuaras A. Self-medication in older urban mexicans: an observational, descriptive, cross-sectional study. Drug Aging. 2009;26:51–60. doi: 10.2165/0002512-200926010-00004. http://dx.doi.org/10.2165/0002512-200926010-00004. [DOI] [PubMed] [Google Scholar]
- 9.Selvorraj K, Kumar SG, Ramalingam A. Prevalence of self-medication practices and its associated factors in urban puducherry, India. Perspect Clin Res. 2014;5:32–6. doi: 10.4103/2229-3485.124569. http://dx.doi.org/10.4103/2229-3485.124569. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Hounsa A, Kouadio L, De Mol Self-medication with antibiotics obstained from privates pharmacies in Abidjan, Ivory Coast. Med Mal Inf. 2010;40:333–40. doi: 10.1016/j.medmal.2009.10.002. http://dx.doi.org/10.1016/j.medmal.2009.10.002. [DOI] [PubMed] [Google Scholar]
- 11.Ouedraogo DD, Ntsiba H, Tiendrebeogo/Zabsonré J, Tieno H, Bokossa LIF, Kaboré F, et al. Clinical spectrum of rheumatologic diseases in a department of rheumatology in Ouagadougou (Burkina Faso) Clin Rheumatol. 2014;33:385–9. doi: 10.1007/s10067-013-2455-4. http://dx.doi.org/10.1007/s10067-013-2455-4. [DOI] [PubMed] [Google Scholar]
- 12.Ndol FM, Bompeka FL, Dramaix-Wilmet M, Meert P, Malengreau M, Mangani NN, et al. Self-medication among patients admitted to the emergency department of Kinshasa university Hospital. Sante Publique. 2013;25:233–40. [PubMed] [Google Scholar]
- 13.Ornbjerg LM, Andersen HB, Kryger P, Cleal B, Hetland ML. What do patients in rheumatologic care know about the risks of NSAIDs? J Clin Rheumatol. 2008;14:69–73. doi: 10.1097/RHU.0b013e31816b1e8e. http://dx.doi.org/10.1097/RHU.0b013e31816b1e8e. [DOI] [PubMed] [Google Scholar]
- 14.Pouillard J. Rapport adopté lors de la session du conseil national de l’ordre des medecins français. Paris: 2001. Automedication; p. 9. [Google Scholar]