Abstract
Importance
Absolute and relative risks of violence are increased in patients with psychotic disorders, but the contribution of triggers for violent acts to these risks is uncertain.
Objective
To examine whether a range of triggers for violent acts are associated with risks of violence in patients diagnosed with psychotic disorders and in individuals without a psychiatric diagnosis.
Design, Setting, and Participants
Using a sample of all individuals born in Sweden between 1958 and 1988 (N = 3 123 724), we identified patients in the National Patient Register who were diagnosed with schizophrenia spectrum disorders (n = 34 903) and bipolar disorder (n = 29 692), as well as unaffected controls (n = 2 763 012). We then identified, within each subsample, persons who had experienced any of the following triggers for violent acts between January 1, 2001, and December 15, 2013: exposure to violence, parental bereavement, self-harm, traumatic brain injury, unintentional injuries, and substance intoxication. By using within-individual models, we conducted conditional logistic regression to compare the risk of the individual engaging in violent acts in the week following the exposure to a trigger with the risk during earlier periods of equivalent length. All time-invariant confounders (eg, genetic and early environmental influences) were controlled for by this research design and we further adjusted for time-varying sociodemographic factors.
Main outcomes and Measures
Adjusted odds ratios (aORs) of violent crime occurring in the week following the exposure to a trigger event compared with earlier periods.
Results
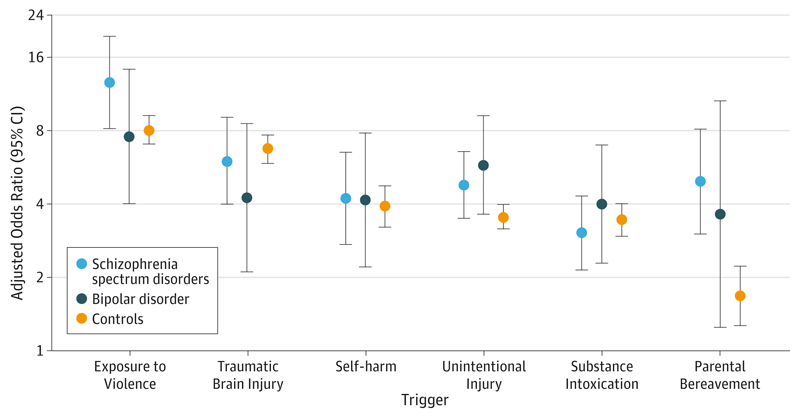
Among the sample of 2 827 607 individuals (1 492 186 male and 1 335 421 female), all of the examined trigger events were associated with increased risk of violent crime in the week following exposure. The largest 1-week absolute risk of violent crime was observed following exposure to violence (70-177 violent crimes per 10 000 persons). For most triggers, the relative risks did not vary significantly by diagnosis, including unintentional injuries (aOR range, 3.5-4.8), self-harm (aOR range, 3.9-4.2), and substance intoxication (aOR range, 3.0-4.0). Differences by diagnosis included parental bereavement, which was significantly higher in patients with schizophrenia spectrum disorders (aOR, 5.0; 95% CI, 3.0-8.1) compared with controls (aOR, 1.7; 95% CI, 1.3-2.2).
Conclusions and Relevance
In addition to identifying risk factors for violence, clarifying the timing of the triggers may provide opportunities to improve risk assessment and management in individuals with psychotic disorders.
Patients diagnosed with schizophrenia spectrum and bipolar disorders have higher rates of violent criminal convictions than do the general population,1,2 particularly if they have comorbid substance use disorders.3,4 A recent systematic review5 has further identified elevated rates of impulsivity and hostility, as well as nonadherence to treatment, as key modifiable risk factors for violence in individuals with psychotic disorders. An important limitation of the literature is the relative neglect of temporal effects; little is known about triggers that occur within days of the incident violent event. In other noncommunicable disorders, particularly cardiovascular diseases, triggers have been shown to have important effects on serious outcomes. For example, modifiable psychological factors (eg, anger, anxiety, and depression), elevated work stress, and unintentional work injuries can act as triggers of myocardial infarction and stroke.6
Three pilot studies7–9 conducted within Swedish correctional and forensic settings on 327 individuals have suggested that certain symptoms and, particularly, alcohol intoxication and high doses of benzodiazepines may trigger violence within 24 hours. However, the generalizability of these findings remains limited owing to their small and highly selected samples. More important, it is not known how such triggers act in individuals with psychosis; less than 20% of those included in previous work had a psychotic disorder,7–9 and whether patients with psychosis act differently from the general population needs clarification. The identification of triggers for violence is potentially clinically important for risk assessment, which is recommended in patients with schizophrenia by systematic reviews10,11 but currently relies mostly on historical factors and is moderately accurate at best.12 In addition, delineating the role of triggers may assist in developing new treatments by, for example, identifying targets for cognitive behavioral therapy. This possibility aligns with recent theoretical work in criminology that emphasizes the ways in which situation-specific factors moderate individual risks of offending.13 Both prediction of aggression and violent behaviors14 and psychological treatments reducing risk15 have limited real-world effects and providing more evidence on risk factors, such as triggers, could suggest novel interventions that could mitigate their effect.
To address the lack of evidence on triggers for violence in patients with psychosis, we used nationwide Swedish data for approximately 3.1 million individuals born between 1958 and 1988, including 64 595 patients diagnosed with psychotic disorders. This cohort represents a substantial increase in sample size compared with all previous work on risk factors for violence in patients with psychosis; a 2013 systematic review of 110 studies was based on 45 533 patients.5 That review identified substance use, impulsivity, positive symptoms, treatment nonadherence, exposure to violence, and self-harm as key risk factors. Two important limitations were further highlighted by the review; little is known about the causal and temporal mechanisms linking the risk factors with violence.
By triggers, we mean proximal risk factors, including stressful life events, occurring in the week before the incident violent offense. We only considered triggers that had either been considered as risk factors or consequences of violence in previous studies.16–19 We adopted a within-individual design,20 where each individual acted as his or her own control across time. This design is important because this approach accounts for all constant factors within each individual (eg, genetic and childhood environmental influences). We also addressed time-varying confounding by adjusting for a comprehensive set of sociodemographic factors that were reliably collected on each individual. In addition, we were able to explore whether our findings were moderated by individual diagnosis, as research suggests that the etiologic determinants of the risk of violence differ between patients with schizophrenia and those with bipolar disorder.21
Methods
Swedish Nationwide Registers
Statistics Sweden, an independent governmental agency, maintains several nationwide longitudinal registries with routinely gathered data derived from many governmental agencies linked by a personal identification number. Following institutional review board approval from the Regional Research Ethics Committee in Stockholm, we were given access to anonymized data.
The National Patient Register provided data on all inpatient hospitalization episodes (based on International Classification of Diseases eighth and ninth editions [ICD-8 and ICD-9] and International Classification of Diseases and Related Health Problems [ICD-10] codes) and specialist outpatient care visits (based on ICD-10 codes).22 The Multi-Generation Register, which encompasses all Swedish residents, enabled us to link the participants with their biological parents. Emigration and mortality dates came from specific registers. Dates of violent crime were taken from the National Crime Register, which includes all criminal convictions. We chose dates that crimes occurred rather than conviction dates. The Integrated Database for Labour Market Research and the Small Area Marketing Statistics Register provided annual data on sociodemographic factors between 1990 and 2012, measured at the end of each year.
Sample
Our sample consisted of all 3 435 357 residents born in Sweden between 1958 and 1988 who could be linked with both biological parents. We excluded 56 721 individuals who died before the start of the study (January 1, 2001) and 254 912 with incomplete data on sociodemographics, leaving 90.9% of the original sample (n = 3 123 724).
Measures
In keeping with previous work,23,24 we defined violent crime as conviction for homicide, assault, robbery, threats and violence against an officer, unlawful threats, unlawful coercion, kidnapping, illegal confinement, arson, intimidation, or sexual offenses (rape, indecent assault, indecent exposure, or child molestation, but excluding prostitution, hiring of prostitutes, or possession of child pornography).
Trigger Events
We examined 2 stressful life events: exposure to violence and parental bereavement. In addition, we examined 3 injury-related triggers (self-harm, traumatic brain injury, and unintended injuries) and substance intoxication (eTable 1 in the Supplement). Diagnoses of exposure to violence,25 traumatic brain injury,26 and unintended injuries27 have been validated. We excluded trigger events that occurred within 14 days of each other to avoid duplication of the same episode.
Psychotic Disorders
To explore moderation effects, we identified individuals with lifetime diagnoses of schizophrenia spectrum disorders (here-after referred to as schizophrenia) and bipolar disorder. The National Patient Register diagnoses of schizophrenia28 or bipolar disorder29 have been validated. We defined healthy controls as individuals who had never been diagnosed with any psychiatric disorder (excluding substance use disorder).
Sociodemographic Factors
Single status was defined as not being married or registered in a same-sex partnership. Low educational level referred to not achieving secondary school qualifications.30 Frequent residential relocations indicated an individual changing his or her residential address at least 4 times in a given year. Residence in a deprived neighborhood indicated that the individual’s standardized neighborhood deprivation score31 ranked in the top decile. Low family income indicated that the individual’s disposable family income fell below the bottom decile. We also measured whether the individuals had been recipients of unemployment benefits, means-tested welfare benefits, and/or disability pension.
Research Design
To test the effects of triggers on violent crime, we adopted a within-individual design in which the included individuals were their own controls, allowing us to control for time-constant confounders (eg, genetic and early childhood environmental factors). The rationale is to examine the risk of the individual committing a violent crime in the 7 days following exposure to a trigger and comparing this risk with earlier control periods when they were unexposed to any trigger. The control periods had an equivalent follow-up period of 7 days and were measured every 30 days before the exposure to the trigger, up to a maximum of 1080 days (36 months). We allowed individuals to be exposed to multiple triggers throughout the entire follow-up period. We defined control periods for subsequent trigger exposures using the same criteria as above, with 1 exception: we only retained control periods that had occurred after the preceding trigger event.
Statistical Analysis
We selected individuals who had been exposed to any of the 6 triggers between January 1, 2001, and December 15, 2013. From the index date of the trigger, we identified all of the available retrospective control periods for each individual. Data on sociodemographic factors measured at the end of the previous year were recorded to adjust for potential bias.
We estimated odds ratios and corresponding 95% CIs for the associations between each trigger and violent crime while adjusting for all individual-specific factors by fitting conditional logistic regression models with individuals as strata. Because the comparisons of the risk of violence across exposures to triggers were made within each individual rather than between individuals, the research design controls for all constant factors within an individual (eg, sex and race/ethnicity). In the crude model, we adjusted for age and calendar month. In the adjusted model, we further adjusted for time-varying sociodemographic factors, including single status, low educational level, frequent residential relocations, low family income, residence in deprived neighborhoods, and being the recipient of unemployment benefits, social assistance, or disability pension benefits. In complementary analyses, we tested whether narrower definitions of psychotic disorders (eTable 2 in the Supplement), longer follow-up periods (eTable 3 in the Supplement), and effect moderation by sociodemographic factors altered our findings (eTable 4 through eTable 9 in the Supplement).
Results
Table 1 presents descriptive statistics for the distribution of sociodemographic characteristics within each group of individuals in the population (n = 3 123 724) that had ever met criteria for schizophrenia (34 903 [1.1%]) or bipolar disorder (29 692 [1.0%]), as well as the unaffected control group (2 763 012 [88.5%]). All indicators of poor psychosocial functioning were more common in patients with psychotic disorders, particularly schizophrenia, when compared with the controls (Table 1).
Table 1. Sociodemographic Characteristics.
| Characteristic | No. (%) | ||
|---|---|---|---|
| Schizophrenia Spectrum Disorders (n = 34 903) |
Bipolar Disorder (n = 29 692) |
Controls (n = 2 763 012) |
|
| Male sex | 20 069 (57.5) | 11 149 (37.5) | 1 460 968 (52.9) |
| Age distribution, y | |||
| <20 | 2657 (7.6) | 3675 (12.4) | 362 320 (13.1) |
| 20-29 | 8296 (23.8) | 9102 (30.7) | 831 634 (30.1) |
| 30-39 | 12 498 (35.8) | 9906 (33.4) | 947 352 (34.3) |
| ≥40 | 11 452 (32.8) | 7009 (23.6) | 621 706 (22.5) |
| Not married | 31 143 (89.2) | 23 807 (80.2) | 2 042 609 (73.9) |
| Low educational level | 11 198 (32.1) | 7999 (26.9) | 529 586 (19.2) |
| Frequent residential relocations | 1224 (3.5) | 1483 (5.0) | 69 470 (2.5) |
| Low family income | 9010 (25.8) | 4877 (16.4) | 251 404 (9.1) |
| Residence in deprived neighborhood | 6130 (17.6) | 3895 (13.1) | 262 887 (9.5) |
| Recipient of benefits | |||
| Unemployment | 4180 (12.0) | 5084 (17.1) | 358 046 (13.0) |
| Social assistance | 6494 (18.6) | 4702 (15.8) | 120 453 (4.4) |
| Disability pension | 14 899 (42.7) | 4860 (16.4) | 62 190 (2.3) |
Absolute risks for violent crime were typically highest among individuals diagnosed with schizophrenia, followed by those diagnosed with bipolar disorder and, last, the unaffected controls (Table 2). Furthermore, we observed that the rates of a violent crime occurring in the week following exposure to a trigger were considerably elevated when compared with their respective control periods (Table 2). This finding was consistent for patients with both psychotic disorders and the controls. Exposure to violence contributed to the largest absolute risks of violent offending, with rates ranging between 70 and 177 violent crimes per 10 000 persons in the week following the violent exposure event compared with 9 to 22 violent crimes per 10 000 persons during the control periods in the same individuals.
Table 2. Rates of Violent Crime in the Week Following Exposure to Triggers vs Control Periodsa.
| Characteristic | Schizophrenia Spectrum Disorders |
Bipolar Disorder |
Unaffected Controls |
|||
|---|---|---|---|---|---|---|
| Observations, No. | Violent Crime Rate (95% CI) | Observations, No. | Violent Crime Rate (95% CI) | Observations, No. | Violent Crime Rate (95% CI) | |
| Exposure to violence | ||||||
| Following trigger | 2995 | 177.0 (132.8-230.8) | 2527 | 83.1 (51.5-126.8) | 65 174 | 70.4 (64.2-77.1) |
| Control periods | 86 508 | 22.0 (19.0-25.3) | 73 130 | 13.1 (10.6-16.0) | 1 842 886 | 9.0 (8.6-9.5) |
| Parental bereavement | ||||||
| Following trigger | 11 628 | 17.2 (10.5-26.6) | 7934 | 5.0 (1.4-12.9) | 654 701 | 0.8 (0.6-1.1) |
| Control periods | 405 146 | 4.6 (3.9-5.3) | 277 330 | 2.4 (1.8-3.0) | 22 903 823 | 0.6 (0.6-0.6) |
| Self-harm | ||||||
| Following trigger | 9944 | 41.2 (29.6-55.9) | 9614 | 22.9 (14.4-34.6) | 71 282 | 25.8 (22.2-29.8) |
| Control periods | 205 370 | 11.7 (10.3-13.3) | 216 397 | 3.9 (3.1-4.8) | 1 930 674 | 6.4 (6.0-6.7) |
| Unintentional injury | ||||||
| Following trigger | 21 425 | 39.2 (31.3-48.5) | 20 285 | 20.2 (14.5-27.4) | 1 256 192 | 4.6 (4.3-5.0) |
| Control periods | 480 937 | 8.9 (8.0-9.7) | 467 158 | 3.6 (3.2-4.3) | 31 260 699 | 1.3 (1.3-1.4) |
| Traumatic brain injury | ||||||
| Following trigger | 5066 | 92.8 (68.3-123.2) | 4109 | 31.6 (16.9-54.0) | 182 147 | 23.9 (21.7-26.2) |
| Control periods | 144 110 | 15.8 (13.8-18.0) | 122 342 | 8.1 (6.6-9.9) | 5 492 908 | 3.6 (3.5-3.8) |
| Substance intoxication | ||||||
| Following trigger | 6157 | 65.0 (46.5-88.4) | 4711 | 34.0 (19.4-55.1) | 60 671 | 33.1 (28.7-38.0) |
| Control periods | 219 840 | 23.0 (21.1-25.1) | 167 279 | 9.3 (7.9-10.9) | 2 089 078 | 10.4 (10.0-10.8) |
Rates are per 10 000 individuals.
We further found that there remained an increased relative risk of violent crime occurring immediately following the occurrence of all the examined triggers, even after accounting for all constant confounders (eg, genetic and childhood family environmental influences) and a wide range of time-varying sociodemographic factors (Figure). The adjusted odds ratios (aORs) ranged between 7.6 and 12.7 for exposure to violence, 4.2 and 6.7 for traumatic brain injuries, 3.5 and 4.8 for unintentional injuries, 3.9 and 4.2 for self-harm, 3.0 and 4.0 for substance intoxication, and 1.7 and 5.0 for parental bereavement. These findings were not materially different from those of the unadjusted models (eTable 10 in the Supplement) or models using narrower definitions of the psychotic disorders (eTable 2 in the Supplement). Moreover, we did not find strong evidence of effect modification by psychosis across the triggers, with 1 exception: parental bereavement was associated with a 5-fold increase in the odds of schizophrenia, which was significantly elevated compared with the controls (aOR, 1.7; 95% CI, 1.3-2.2).
Figure. Relative Risks of Violent Crime.
Violent crime occurring in the week following exposure to a trigger compared with control periods across patients with psychotic disorders and controls. Within-individual estimates adjusted for age, calendar month, single status, low educational level, frequent residential relocations, low family income, residence in deprived neighborhoods, and being the recipient of unemployment benefits, social assistance, or disability pension benefits.
The effects of the triggers weakened across time (eTable 3 in the Supplement), thus providing additional support for their transient effect on violence. This effect was most noticeable in the case of exposure to violence. Among patients diagnosed with schizophrenia, the risk of violent offending following exposure to violence dropped from a nearly 13-fold increase (aOR, 12.7; 95% CI, 8.2-19.6) in the first week to a fully attenuated association in the second week (aOR, 0.8; 95% CI, 0.4-2.0), which persisted into the third week (aOR, 1.1; 95% CI, 0.5-2.3). Similar results were found in patients with bipolar disorder and in the controls.
We found little evidence for the presence of moderation effects by sociodemographic factors (eTable 4 through eTable 9 in the Supplement). Following Bonferroni correction, we found that only 4 of 180 tests (2.2%) were statistically significant. Consistent with interpretation of a ceiling effect, we found that individuals in the control group who were recipients of welfare benefits and those who had only achieved a low educational level had lower relative risks of violent offending following exposure to violence and traumatic brain injury.
Discussion
We conducted a nationwide within-individual study examining the role of triggers for violent criminality in 64 595 patients diagnosed with psychotic disorders and in 2 763 012 controls. The triggers included 2 stressful life events (parental bereavement and exposure to violence), 3 injury-related triggers (self-harm, traumatic brain injury, and unintentional injuries), and substance intoxication.
First, we found statistically significant associations between all triggers and the rate of violent criminality in the week following the exposure compared with the rate of violent criminality in earlier control periods. Findings of complementary sensitivity analyses using different diagnostic criteria were consistent with our overall findings. More important, we also observed that the triggers had less effect as follow-up time increased. These findings support the hypothesis that recent exposure to a stressful life event, an intentional or unintentional injury, or having been diagnosed with substance intoxication increases the short-term risk of interpersonal violence in individuals with psychotic disorders and in controls.
Second, we found that the absolute risks of violence occurring in the week following exposure to the triggers differed by individual diagnosis, with the strongest effects being observed in patients with schizophrenia, followed by those with bipolar disorder and controls. However, relative risks across the 3 groups were similar. The only exception to this rule was parental bereavement, where we found stronger relative risks in the patients with schizophrenia (aOR, 5.0; 95% CI, 3.0-8.1) than in the controls (aOR, 1.7; 95% CI, 1.3-2.2). An explanation for this finding is that elevated levels of social support from family members and close friends in the controls32 may be protective against violence. More generally, these findings suggest that interventions to minimize the risk of violence in individuals who have experienced injuries and substance intoxication should target not only psychiatric patients but also the general population. Current clinical guidelines for alcohol use disorders33 recommend that trained professionals in the health and social care sectors should routinely screen patients for harmful drinking and offer affected individuals structured brief advice to reduce their alcohol consumption. The efficacy of such brief interventions has been recently confirmed in a systematic review.34 Nonexperimental data have further suggested more comprehensive interventions aimed at reducing violence rates among individuals admitted to emergency departments for injury due to exposure to violence by closely following up high-risk patients with a multidisciplinary team that includes physicians, nurses, and social workers.35 If such efforts prove to be effective in large-scale randomized trials, our findings suggest that expanding them to include a wider range of injury and substance-related triggers may reduce rates of violence in patient groups and the general population.
Third, our findings demonstrating that self-harm increases the risk of interpersonal violence are, to our knowledge, novel. Prior studies36,37 have generally viewed selfharm as a consequence of interpersonal violence38,39 and research examining the direction of the association between self-inflicted and interpersonal violence is inconclusive.19,40 Our findings suggest that self-harming patients, particularly those with psychoses, are an important group to be assessed for interpersonal violence in addition to the routinely examined risk of suicide.
Previous studies have considered all of these triggers as risk factors or consequences of violence,16–19 but only 3 studies have considered triggers for violence using within-individual designs in small and highly selected clinical samples with a combined total of 70 patients with psychosis using short follow-up periods and no population controls.7–9
Four methodological limitations to our study should be considered. First, despite our efforts to minimize confounding, we cannot exclude the possibility that other timevarying confounders simultaneously explain the cooccurrences of the examined triggers and violent criminality. In the case of the psychotic disorders, for instance, exposure to a specific trigger and the resulting violent outcome may be simultaneously caused by an acute phase of a psychotic or manic episode. The effect of such confounding factors are, however, likely to be marginal, as our findings suggest that the relative risks of violence following most triggers are either similar or stronger in the unaffected controls compared with the patients diagnosed with psychotic disorders. Future work should therefore focus on replicating these findings across different contexts and designs. More clinically rich cohorts could, in addition, examine the underlying causal mechanisms linking the triggers to each other as well as to later adverse outcomes, including acts of violence. By adopting life-course approaches, such studies could concurrently investigate a wide range of distal and proximal risk factors for violence in adulthood. These factors include impulsivity and positive symptoms that our data sets did not have reliable data to examine. Furthermore, the combination of such approaches with longer follow-up data could address whether recurrent exposures to a given trigger confer higher risks of violence than the first episode.
Second, our violent crime measure was derived from nationwide conviction data, which constitute a comprehensive measure of severe offenses but less comprehensiveness for minor offenses. The extent to which our results would have differed if we had access to data on nonreported violent acts and triggering events remains therefore an empirical question that should be addressed in future research. Alternative approaches, such as gathering self-reported data, tend to be subject to other methodological limitations, including increased measurement error,41 which artificially deflates estimates down to the null.42 Third, the data on sociodemographic factors were measured at the end of each year. Any changes that had occurred between the end of the previous year up until the measurement of the trigger and control periods were consequently subject to misclassification bias. However, given that the combined effects of all sociodemographic factors did not affect the crude associations, we expect such bias to be minimal. Fourth, it is possible for an individual to engage in interpersonal violence and consequently require treatment for being injured during exposure to violence. We attempted to separate these effects by considering only violent offenses that occurred after hospital discharge.
The generalizability of the presented findings is an important consideration. Comparative studies on police-recorded rates of common types of serious violent offenses have been shown to be fairly similar across high-income countries.43 Violence prevalence estimates for psychotic disorders vary minimally across European countries and the United States.44–46 Age and disability-adjusted life years attributed to unintentional injuries are similar across Sweden, the United Kingdom, and the United States.47 Sweden’s estimated alcohol sales per capita are comparable to those of the United States48 and nationally representative data from Sweden and the United Kingdom on self-reported exposure to violence rates indicate marginal differences.49,50 Thus, for key exposures and our outcome, Sweden is not clearly different from Western Europe and the United States.
Conclusions
Using a novel approach and large sample size, we have shown the importance of triggers for the risk of violence in patients with psychotic disorders. By including controls, we were able to examine possible mechanisms by which they could act. To our knowledge, identifying triggers for violence has not been incorporated into many risk assessment approaches, but our findings suggest that it may provide opportunities to improve the monitoring and management of violence risk.
Supplementary Material
Key Points.
Question What are important triggers for violent crime in patients diagnosed with psychotic disorders and do these associations with violence differ from those in population controls?
Findings In this population-based time-stratified case-crossover study, all of the triggers, which included exposure to violence, traumatic brain injuries, unintentional injuries, self-harm, substance intoxication, and parental bereavement, contributed to elevated relative risks of violent crime among patients with psychotic disorders in the week after their occurrence compared with earlier periods within the same individuals.
Meaning Triggers contribute to the risk of violent crime in patients with psychotic disorders as well as controls. These findings may offer opportunities to improve the monitoring and management of the risk of violence.
Acknowledgments
Funding/Support: This study was supported by grant 095806 from the Wellcome Trust; the Swedish Council for Working Life and Social Research; grants 2010-3184, 2011-2492, and 2013-5867 from the Swedish Research Council; and grant HD061817 from the National Institute of Child Health and Human Development.
Role of the Funder/Sponsor: The funding sources were not involved in the design and conduct of the study; collection, management, analysis, and interpretation of the data; preparation, review, or approval of the manuscript; and decision to submit the manuscript for publication.
Footnotes
Author Contributions: Dr Sariaslan had full access to all the data in the study and takes responsibility for the integrity of the data and the accuracy of the data analysis.
Study concept and design: Sariaslan, Larsson, Fazel.
Acquisition, analysis, or interpretation of data: Sariaslan, Lichtenstein, Fazel.
Drafting of the manuscript: Sariaslan, Fazel.
Critical revision of the manuscript for important intellectual content: Sariaslan, Lichtenstein, Larsson, Fazel.
Statistical analysis: Sariaslan.
Obtained funding: Lichtenstein, Larsson, Fazel.
Administrative, technical, or material support: Lichtenstein.
Study supervision: Lichtenstein, Larsson, Fazel.
Conflict of Interest Disclosures: None reported.
Contributor Information
Amir Sariaslan, Department of Psychiatry, University of Oxford, Warneford Hospital, Oxford, United Kingdom.
Paul Lichtenstein, Department of Medical Epidemiology and Biostatistics, Karolinska Institutet, Stockholm, Sweden.
Henrik Larsson, Department of Medical Epidemiology and Biostatistics, Karolinska Institutet, Stockholm, Sweden; Department of Medical Sciences, Örebro University, Örebro, Sweden.
Seena Fazel, Department of Psychiatry, University of Oxford, Warneford Hospital, Oxford, United Kingdom.
References
- 1.Fazel S, Gulati G, Linsell L, Geddes JR, Grann M. Schizophrenia and violence: systematic review and meta-analysis. PLoS Med. 2009;6(8):e1000120. doi: 10.1371/journal.pmed.1000120. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Fazel S, Lichtenstein P, Grann M, Goodwin GM, Långström N. Bipolar disorder and violent crime: new evidence from population-based longitudinal studies and systematic review. Arch Gen Psychiatry. 2010;67(9):931–938. doi: 10.1001/archgenpsychiatry.2010.97. [DOI] [PubMed] [Google Scholar]
- 3.Steadman HJ, Mulvey EP, Monahan J, et al. Violence by people discharged from acute psychiatric inpatient facilities and by others in the same neighborhoods. Arch Gen Psychiatry. 1998;55(5):393–401. doi: 10.1001/archpsyc.55.5.393. [DOI] [PubMed] [Google Scholar]
- 4.Elbogen EB, Johnson SC. The intricate link between violence and mental disorder: results from the National Epidemiologic Survey on Alcohol and Related Conditions. Arch Gen Psychiatry. 2009;66(2):152–161. doi: 10.1001/archgenpsychiatry.2008.537. [DOI] [PubMed] [Google Scholar]
- 5.Witt K, van Dorn R, Fazel S. Risk factors for violence in psychosis: systematic review and meta-regression analysis of 110 studies. PLoS One. 2013;8(2):e55942. doi: 10.1371/journal.pone.0055942. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Mittleman MA, Mostofsky E. Physical, psychological and chemical triggers of acute cardiovascular events: preventive strategies. Circulation. 2011;124(3):346–354. doi: 10.1161/CIRCULATIONAHA.110.968776. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Haggård-Grann U, Hallqvist J, Långström N, Möller J. The role of alcohol and drugs in triggering criminal violence: a case-crossover study. Addiction. 2006;101(1):100–108. doi: 10.1111/j.1360-0443.2005.01293.x. [DOI] [PubMed] [Google Scholar]
- 8.Haggård-Grann U, Hallqvist J, Långström N, Möller J. Short-term effects of psychiatric symptoms and interpersonal stressors on criminal violence—a case-crossover study. Soc Psychiatry Psychiatr Epidemiol. 2006;41(7):532–540. doi: 10.1007/s00127-006-0056-0. [DOI] [PubMed] [Google Scholar]
- 9.Lundholm L, Haggård U, Möller J, Hallqvist J, Thiblin I. The triggering effect of alcohol and illicit drugs on violent crime in a remand prison population: a case crossover study. Drug Alcohol Depend. 2013;129(1-2):110–115. doi: 10.1016/j.drugalcdep.2012.09.019. [DOI] [PubMed] [Google Scholar]
- 10.Douglas KS, Skeem JL. Violence risk assessment: getting specific about being dynamic. Psychol Public Policy Law. 2005;11(3):347–383. doi: 10.1037/1076-8971.11.3.347. [DOI] [Google Scholar]
- 11.Large MM, Nielssen O. Violence in first-episode psychosis: a systematic review and meta-analysis. Schizophr Res. 2011;125(2-3):209–220. doi: 10.1016/j.schres.2010.11.026. [DOI] [PubMed] [Google Scholar]
- 12.Singh JP, Serper M, Reinharth J, Fazel S. Structured assessment of violence risk in schizophrenia and other psychiatric disorders: a systematic review of the validity, reliability, and item content of 10 available instruments. Schizophr Bull. 2011;37(5):899–912. doi: 10.1093/schbul/sbr093. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Wikström P-OH. Individuals, settings, and acts of crime: situational mechanisms and the explanation of crime. In: Wikström P-OH, Sampson RJ, editors. The Explanation of Crime: Context, Mechanisms and Development. Cambridge, UK: Cambridge University Press; 2006. pp. 61–107. [Google Scholar]
- 14.Troquete NA, van den Brink RH, Beintema H, et al. Risk assessment and shared care planning in out-patient forensic psychiatry: cluster randomised controlled trial. Br J Psychiatry. 2013;202(5):365–371. doi: 10.1192/bjp.bp.112.113043. [DOI] [PubMed] [Google Scholar]
- 15.McGuire J. A review of effective interventions for reducing aggression and violence. Philos Trans R Soc Lond B Biol Sci. 2008;363(1503):2577–2597. doi: 10.1098/rstb.2008.0035. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Wilcox HC, Kuramoto SJ, Lichtenstein P, Långström N, Brent DA, Runeson B. Psychiatric morbidity, violent crime, and suicide among children and adolescents exposed to parental death. J Am Acad Child Adolesc Psychiatry. 2010;49(5):514–523. doi: 10.1097/00004583-201005000-00012. [DOI] [PubMed] [Google Scholar]
- 17.Fazel S, Lichtenstein P, Grann M, Långström N. Risk of violent crime in individuals with epilepsy and traumatic brain injury: a 35-year Swedish population study. PLoS Med. 2011;8(12):e1001150. doi: 10.1371/journal.pmed.1001150. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.Jennings WG, Piquero AR, Reingle JM. On-the overlap between victimization and offending: a review of the literature. Aggress Violent Behav. 2012;17(1):16–26. doi: 10.1016/j.avb.2011.09.003. [DOI] [Google Scholar]
- 19.O’Donnell O, House A, Waterman M. The co-occurrence of aggression and self-harm: systematic literature review. J Affect Disord. 2015;175:325–350. doi: 10.1016/j.jad.2014.12.051. [DOI] [PubMed] [Google Scholar]
- 20.Mittleman MA, Mostofsky E. Exchangeability in the case-crossover design. Int J Epidemiol. 2014;43(5):1645–1655. doi: 10.1093/ije/dyu081. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21.Sariaslan A, Larsson H, Fazel S. Genetic and environmental determinants of violence risk in psychotic disorders: a multivariate quantitative genetic study of 1.8million Swedish twins and siblings [published online December 15, 2015] Mol Psychiatry. doi: 10.1038/mp.2015.184. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22.Ludvigsson JF, Otterblad-Olausson P, Pettersson BU, Ekbom AL. The Swedish personal identity number: possibilities and pitfalls in healthcare and medical research. Eur J Epidemiol. 2009;24(11):659–667. doi: 10.1007/s10654-009-9350-y. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23.Fazel S, Grann M. The population impact of severe mental illness on violent crime. Am J Psychiatry. 2006;163(8):1397–1403. doi: 10.1176/ajp.2006.163.8.1397. [DOI] [PubMed] [Google Scholar]
- 24.Sariaslan A, Larsson H, D’Onofrio B, Långström N, Lichtenstein P. Childhood family income, adolescent violent criminality and substance misuse: quasi-experimental total population study. Br J Psychiatry. 2014;205(4):286–290. doi: 10.1192/bjp.bp.113.136200. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25.Kühlhorn E, Grevholm E. The Serious Violence in Hospital Data: A Methodological Study: Report 2007:13. Stockholm, Sweden: The National Council for Crime Prevention; 2007. [Google Scholar]
- 26.Nilsson AC, Spetz CL, Carsjö K, Nightingale R, Smedby B. Reliability of the hospital registry: the diagnostic data are better than their reputation [in Swedish] Lakartidningen. 1994;91(7):598, 603–605. [PubMed] [Google Scholar]
- 27.Gedeborg R, Engquist H, Berglund L, Michaëlsson K. Identification of incident injuries in hospital discharge registers. Epidemiology. 2008;19(6):860–867. doi: 10.1097/ede.0b013e318181319e. [DOI] [PubMed] [Google Scholar]
- 28.Dalman C, Broms J, Cullberg J, Allebeck P. Young cases of schizophrenia identified in a national inpatient register. Soc Psychiatry Psychiatr Epidemiol. 2002;37(11):527–531. doi: 10.1007/00127-002-0582-3. [DOI] [PubMed] [Google Scholar]
- 29.Sellgren C, Landén M, Lichtenstein P, Hultman CM, Långström N. Validity of bipolar disorder hospital discharge diagnoses: file review and multiple register linkage in Sweden. Acta Psychiatr Scand. 2011;124(6):447–453. doi: 10.1111/j.1600-0447.2011.01747.x. [DOI] [PubMed] [Google Scholar]
- 30.Halldén K. The Swedish Educational System and Classifying Education Using the Isced-97. In: Schneider SL, editor. The International Standard Classification of Education (Isced-97): An Evaluation of Content and Criterion Validity in 15 European. Mannheim, Germany: MZES; 2008. [Google Scholar]
- 31.Sariaslan A, Larsson H, D’Onofrio B, Långström N, Fazel S, Lichtenstein P. Does population density and neighborhood deprivation predict schizophrenia? a nationwide Swedish family-based study of 2.4million individuals. Schizophr Bull. 2015;41(2):494–502. doi: 10.1093/schbul/sbu105. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 32.Gayer-Anderson C, Morgan C. Social networks, support and early psychosis: a systematic review. Epidemiol Psychiatr Sci. 2013;22(2):131–146. doi: 10.1017/S2045796012000406. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 33.The National Institute for Health and Care Excellence (NICE) Alcohol-Use Disorders: Diagnosis, Assessment and Management of Harmful Drinking and Alcohol Dependence. London, UK: NICE; 2011. [Google Scholar]
- 34.Elzerbi C, Donoghue K, Drummond C. A comparison of the efficacy of brief interventions to reduce hazardous and harmful alcohol consumption between European and non-European countries: a systematic review and meta-analysis of randomized controlled trials. Addiction. 2015;110(7):1082–1091. doi: 10.1111/add.12960. [DOI] [PubMed] [Google Scholar]
- 35.Purtle J, Rich JA, Fein JA, James T, Corbin TJ. Hospital-based violence prevention: progress and opportunities. Ann Intern Med. 2015;163(9):715–717. doi: 10.7326/M15-0586. [DOI] [PubMed] [Google Scholar]
- 36.Penn JV, Esposito CL, Schaeffer LE, Fritz GK, Spirito A. Suicide attempts and self-mutilative behavior in a juvenile correctional facility. J Am Acad Child Adolesc Psychiatry. 2003;42(7):762–769. doi: 10.1097/01.CHI.0000046869.56865.46. [DOI] [PubMed] [Google Scholar]
- 37.Hawton K, Linsell L, Adeniji T, Sariaslan A, Fazel S. Self-harm in prisons in England and Wales: an epidemiological study of prevalence, risk factors, clustering, and subsequent suicide. Lancet. 2014;383(9923):1147–1154. doi: 10.1016/S0140-6736(13)62118-2. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 38.Caine ED, Knox KL, Conwell Y. Public Health and Population Approaches for Suicide Prevention. London, UK: Routledge; 2011. [Google Scholar]
- 39.Caine ED. Forging an agenda for suicide prevention in the United States. Am J Public Health. 2013;103(5):822–829. doi: 10.2105/AJPH.2012.301078. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 40.Gvion Y, Apter A. Aggression, impulsivity, and suicide behavior: a review of the literature. Arch Suicide Res. 2011;15(2):93–112. doi: 10.1080/13811118.2011.565265. [DOI] [PubMed] [Google Scholar]
- 41.Edmondson D, Newman JD, Whang W, Davidson KW. Emotional triggers in myocardial infarction: do they matter? Eur Heart J. 2013;34(4):300–306. doi: 10.1093/eurheartj/ehs398. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 42.Frisell T, Öberg S, Kuja-Halkola R, Sjölander A. Sibling comparison designs: bias from non-shared confounders and measurement error. Epidemiology. 2012;23(5):713–720. doi: 10.1097/EDE.0b013e31825fa230. [DOI] [PubMed] [Google Scholar]
- 43.Heiskanen M. Trends in police recorded crime. In: Harrendorf S, Heiskanen M, Malby S, editors. International Statistics on Crime And Justice. Helsinki, Finland: United Nations European Institute for Crime Prevention and Control; 2010. pp. 21–47. [Google Scholar]
- 44.Saha S, Chant D, Welham J, McGrath J. A systematic review of the prevalence of schizophrenia. PLoS Med. 2005;2(5):e141. doi: 10.1371/journal.pmed.0020141. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 45.Wittchen H-U, Jacobi F, Rehm J, et al. The size and burden of mental disorders and other disorders of the brain in Europe 2010. Eur Neuropsychopharmacol. 2011;21(9):655–679. doi: 10.1016/j.euroneuro.2011.07.018. [DOI] [PubMed] [Google Scholar]
- 46.Merikangas KR, Jin R, He J-P, et al. Prevalence and correlates of bipolar spectrum disorder in the world mental health survey initiative. Arch Gen Psychiatry. 2011;68(3):241–251. doi: 10.1001/archgenpsychiatry.2011.12. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 47.World Health Organization. Global Health Observatory data repository: estimates by country: age-standardized DALY rates. [Accessed November 26, 2015]; http://apps.who.int/gho/data/node.main.DALYCTRY?lang=en.
- 48.National Institute of Public Health. Alcohol Statistics 2007. Österund, Sweden: National Institute of Public Health; 2007. [Google Scholar]
- 49.The Swedish National Council for Crime Prevention. Exposure to Crime 2014: Results From the National Safety Survey 2015 [in Swedish] Stockholm, Sweden: The Swedish National Council for Crime Prevention; 2015. [Google Scholar]
- 50.Office for National Statistics. Crime in England and Wales, Year Ending March 2015. London, UK: Office for National Statistics; 2015. [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.