Abstract
Pituitary adenomas usually arise from the anterior lobe of the pituitary gland and are manifested with hormonal disorders or mass effect. Mass effect usually occurs in nonfunctional tumors. Pituitary adenomas may be manifested with visual field defects or rarely in the form of total oculomotor palsy. Visual field defect is most frequently in the form of bitemporal hemianopsia and superior temporal defect. Sudden loss of vision, papilledema and ophthalmoplegia may be observed. Pituitary apoplexy is defined as an acute clinical syndrome characterized with headache, vomiting, loss of vision, ophthalmoplegia and clouding of consciousness. The problem leading to pituitary apoplexy may be decreased blood supply in the adenoma and hemorrhage following this decrease or hemorrhage alone. In this article, we present a patient who presented with fever, vomiting and sudden loss of vision and limited outward gaze in the left eye following trauma and who was found to have pituitary macroadenoma causing compression of the optic chiasma and optic nerve on the left side on cranial and pituitary magnetic resonance imaging.
Keywords: Adenoma, pituitary apoplexy, sudden loss of vision
Introduction
Pituitary adenomas usually arise from the anterior lobe of the pituitary gland and are classified by their functions and light or elecron microscobe appearances (1). They are most frequently observed in the adult age group and occur rarely in children (2). These tumors are manifested with mass effect or hormonal disorders. Mass effect is observed especially in nonfunctional tumors (3). Some patients (especially the ones with microadenomas) may present with an acute clinical picture characterized with headache, vomiting, loss of vision, ophthalmoplegia and clouding of consciousness due to pituitary apoplexy which is a rare condition (4). In this article, a 9-year old boy who presented with mass compression and pituitary apoplexy possibly following trauma, who was thought to have adenoma with imaging methods and operated by neurosurgery and who was found to have pituitary macroadenoma is presented. The patient was in an age group in which pituitary adenomas occur rarely.
Case
A 9-year old male patient was referred to our clinic because of fever (up to 39°C) for the last 3 days, projectile vomiting, progressive loss of vision in the right eye and limited outward gaze in the left eye which occured on the day of presentation, with a prediagnosis of central nervous sytem infection. On physical examination, his general status was moderate and he had somnolance. His Glaskow coma score (GCS) was found to be 12 (E3 M5 V4). His both pupillae were isochoric and the movements of the right eye were found to be normal. Limited outward gaze due to involvement of the sixth cranial nerve was present in the left eye. Complete loss of vision due to involvement of the second cranial nerve was present in the right eye. Direct light reflex was absent and indirect light reflex was present in the right eye (Figure 1). Muscle strenght and sensory examination were found to be normal. No pathology was found on examination of the other systems. Laboratory test results were as follows: white blood cell count: 13 100/mm3, hematocrite: 34%, hemoglobin: 11.8 g/dL, platelet count: 445 000/mm3, blood glucose level: 95 mg/dL, urea: 9 mg/dL, creatinine: 0.7 mg/dL, sodium: (Na) 125 mEq/L, potassium (K): 4.6 mEq/L, calcium (Ca): 9.2 mg/dL, C reactive protein: 56.5 mg/dL and erythrocyte sedimentation rate: 57 mm/h. Cranial and pituitary magnetic resonance (MR) imaging revealed a mass with a size of approximately 3 × 3,5 × 3 cm which filled the base of the sella, obstructed the suprasellar cistern, formed crenation in the base of the third ventricle, compressed the left optic nevre and the optic chiasma on the left with regular borders having the same intensity as the heterogeneous gray matter in the T1A and T2A sequences and contrast enhancement following intravenous injection of contrast material (Figure 2). Patient was consulted with Neurosurgery clinic for operation. At the baseline, fluid restriction was initiated considering inappropriate antidiuretic hormone secretion because of presence of normovolemic hyponatremia, low urea values and normal blood glucose and serum potassium levels. However, the patient’s general status deteriorated in the follow-up and his blood pressure and blood glucose level decreased. In light of the presence of fever, vomiting, headache and visual findings, it was thought that pituitary apoplexy and related adrenal failure developed and corticosteroid treatment was added. The patient’s daily fluid intake and output and serum electrolyte levels were monitored closely. His vital signs improved, blood glucose and electrolyte values returned to the normal values. The mass was excised completely by right pterional craniotomy and compression on the optic chiasma and optic nevre was eliminated by operation. Pathological examination of the excised mass was compatible with pituitary macroadenoma with a Ki-67 proliferation index of 4% and diffuse necrosis and hemorrhage areas demonstrating growth hormone (GH) with a rate of 80%, thyroid stimulating hormone with a rate of 30% and prolactin cell reaction with a rate of 80% on immunohistochemical staining. In the postoperative period, desmopressin treatment was initiated because diabetes insipidus developed and hydrocortisone and L-thyroxine treatment was initiated because of pituitary failure in the patient whose general status was well. The patient was discharged to be followed up by pediatric endocrinology clinic. Informed consent was obtained from the parents to publish the patient’s clinical findings, laboratory test results and pictures.
Figure 1. a–c.
(a) Limited outward gaze related with involvement of the sixth cranial nerve in the left eye before surgery (b, c) Improvement in involvement of the sixth cranial nerve in the follow-up; the eye movements are free in all directions
Figure 2.
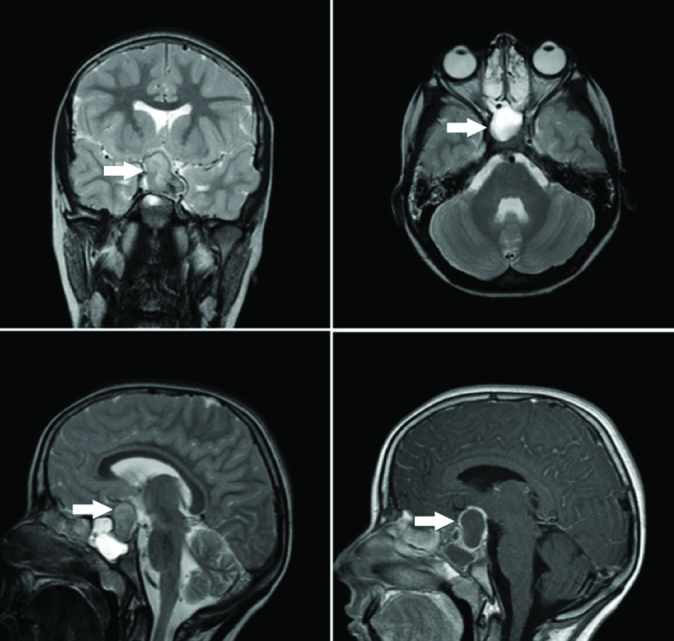
Mass lesion with a size of approximately 3×3,5×3 cm which filled the base of the sella, compressed the left optic nerve and the optic chiasma on the left with regular borders and contrast enhancement following intravenous injection of contrast material
Discussion
Pituitary adenomas are generally slowly growing, benign neoplasms of epithelial origin originating from the adenohypophysis. They constitute approximately 10–15% of all intracranial mass lesions (5, 6). Pituitary adenomas may be manifested with visual field defects and rarely with full opthalmoplegia. Bitemporal hemianopsia and superior temporal visual field defect are found most frequently. Sudden loss of vision, papilledema and opthalmoplegia may be observed (7, 8). Pituitary tumors may lead to symptoms in one or both eyes especially when their sizes exceed 1 cm. In the early phase, only diplopia or visual field defects may be observed. Involvement of the cavernous sinus is observed in 20% of macroadenomas and is usually unilateral (9). This patient presented with fever (up to 39 °C) for the last 3 days, projectile vomiting, headache, clouding of consciousness and progressive loss of vision in the right eye and limited outward gaze in the left eye which arised on the day of presentation. Visual field examination could not be performed initially, because the patient’s clinical status was not appropriate.
Brain tomography and especially MR imaging currently provide diagnosis of pituitary adenomas in the early stages. However, physical examination of the eye still maintains its importance in diagnosis and treatment of pituitary adenomas (6, 10). If pituitary adenomas are smaller than 10 mm, they are classified as microadenoma and they are generally functional. They most commonly secrete ACTH and prolactin. Adenomas larger than 10 mm are named macroadenoma and they are mostly nonfunctional. Symptoms generally arise with mass effect after the tumor reaches a certain size (5). The MR imaging of this patient revealed a macroadenoma with a size of 3×3.5×3 cm compressing the left optic nevre and the optic chiasm on the left side. Acromegaly or gigantism, Cushing disease, galactorrhea and signs and symptoms of secondary hyperthyroidism which are observed as a result of excessive secretion of pituitary hormones were not present a the time of the diagnosis. Although the patient’s signs and symptoms were compatible with a nonfunctional macroadenoma, it was thought that a definite diagnosis of nonfunctional macroadenoma was difficult to make, because the hormone values before development of hemorrhage into the adenoma were lacking, pathologic examination revealed cell reactions which could produce hormone and it was known that functional adenomas could remain asymptomatic for years. The term pituitary apoplexy is used to define hemorrhage within the pituitary gland related with any cause as well as acute infarction or hemorrhage within a pituitary adenoma (11). Although pituitary apoplexy generally occurs spontaneously, it has been associated with many conditions including head trauma, increased blood pressure, transient increase in the intracranial pressure, diabetes mellitus, dynamic tests directed to investigate pituitary function, radiotherapy and drugs. This patient also had a history of trauma in the right maxillary region just before onset of the complaints. Afterwards, the typical complaints began. Pituitary apoplexy is typically observed in pituitary adenomas, but the adenoma subtype with a higher risk of apoplexy has not been reported (1). The first step in treatment of patients presenting with pituitary apoplexy is close monitoring and corticosteroid treatment (2, 8). If loss of vision is present, urgent elimination of nerve compression is recommended (11, 12). Steroid treatment and appropriate fluid treatment was initiated in this patient and electrolyte levels and all vital signs were monitored closely. The mass was excised by way of craniotomy and compression to the optic nerve and optic chiasm was eliminated, because loss of vision was present.
Five percent of pituitary adenomas is presented with a more severe clinical picture. These adenomas lead to erosion in the scull base bones by extending to the sides (subtemporal or prepontine extension) in addition to cavernous sinus and suprasellar extension and may show sphenoid sinus involvement. These adenomas are generally associated with a poor prognosis. They are most frequently manifested with visual problems (4). Adenoma with a poor prognosis was also considered in this patient because of similar findings.
In patients with pituitary tumors, pituitary failure may develop with the effect of adenoma itself or following surgical excision. In pituitary failure, adrenocorticotropic hormone (ACTH), TSH, follicular stimulating hormone and luteinizing hormone are important (5). In one study, it was reported that hormone replacement treatment was administered in 83% of the patients and transient diabetes insipidus developed in 5% of the patients and persistent diabetes insipidus developed in 9% (11). Desmopressin, hydrocortisone and L-thyroxine treatment directed to hormone deficiencies which developed after surgery was inititated in this patient. He was started to be followed up by the division of endocrinology in terms of other (hormone deficiency) findings. Semple et al. (12) reported that visual acuity improved with a rate of 85%, visual field improved with a rate of 73% and cranial nerve involvement improved with a rate of 80% in the patients who were followed up. The results of the same series showed that 60% of the patients recovered completely, 5% were lost because of apoplexy and 10% were lost because of causes other than apoplexy. No motor loss was observed in this patient after surgery. In the follow-up, abducens palsy was improved and the eye movements were free in all directions. In the Visual Evoked Potential (VEP) test performed in the opthalmology clinic, it was observed that there was loss in P latance in the right eye and arcuate visual field defect was found in the right eye in the visual field test. Loss of vision related with involvement of the optic nerve in the right eye did not improve. The division of endocrinology reported that growth hormone treatment could be initiated in the patient whose somatomedin C and insulin like growth factor binding protein 3 levels were found to be low. In the follow-up visit performed in the third month, the parents reported that the patient had complaints of hyperactivity, lack of obedience and difficulty in holding back.
In conclusion, pituitary macroadenoma and apoplexy may be observed in children, though rarely. Rapid diagnosis of the disease is substantially important in terms of appropriate medical and surgical treatment and decreasing the morbidity and mortality risks.
Footnotes
Informed Consent: Written informed consent was obtained from patients’ parents who participated in this study.
Peer-review: Externally peer-reviewed.
Author Contributions: Concept - M.Ö., N.E.; Design - M.Ö., M.K.; Supervision - M.Ö., M.K.; Data Collection and/or Processing - E.T., M.K.; Analysis and/or Interpretation - M.Ö., M.K., N.E.; Literature Review - M.Ö., E.T.; Writing - M.Ö., M.K.; Critical Review - M.Ö., M.K.
Conflict of Interest: No conflict of interest was declared by the authors.
Financial Disclosure: The authors declared that this study has received no financial support.
References
- 1.Berkman ZM. Hipofiz adenomları. Türkiye Klinikleri J Surg Med Sci. 2007;3:152–64. [Google Scholar]
- 2.Yılmaz M, İzmirli M, Yuca K, Mumcu Ç, Ünal Ö. Nasal ve nasofarengeal kitle olarak bulgu veren bir dev pituiter adenom olgusu. Tıp Araştırmaları Dergisi. 2006;4:45–7. [Google Scholar]
- 3.Taylor M, Couto-Silva AC, Adan L, et al. Hypothalamic-pituitary lesions in pediatric patients: endocrine symptoms often precede neuro-ophthalmic presenting symptoms. J Pediatr. 2012;161:855–63. doi: 10.1016/j.jpeds.2012.05.014. http://dx.doi.org/10.1016/j.jpeds.2012.05.014. [DOI] [PubMed] [Google Scholar]
- 4.Erbaş T. Pituiter apopleksi. Turkiye Klinikleri J Surg Med Sci. 2006;2:28–30. [Google Scholar]
- 5.Uğraş S. Hipofiz adenomlarında transsfenoidal mikrocerrahi. Uzmanlık Tezi, İstanbul. 2005. pp. 1–109.
- 6.Cila A. Hipofiz Adenomlarında Radyoloji. Türk Nöroşirürji Dergisi. 2006;16:80–3. [Google Scholar]
- 7.Sashank P. Visuel problems due to pituitary tumors A Patient’s Guide. Harvard Medical School Brigham and Women’s Hospital Division of Neuro-Ophthalmology Brigham and Women’s Hospital Pituitary/Neuroendocrine Center. 2011. Available from: http://www.brighamandwomens.org/Departments_and_Services/neurosurgery/OurServices/Pituitary.aspx. (erişim tarihi:15.01.2014)
- 8.Aral F, Bayram F, Bolu E. Türkiye Endokrinoloji ve Metabolizma Derneği. Ankara: Tuna Matbaacılık; 2009. Hipofiz hastalıkları tanı, tedavi ve izlem kılavuzu; pp. 30–43. [Google Scholar]
- 9.Köşkderelioğlu A, Çelebisoy N. Pituitary macroadenoma manifesting as an isolated third nevre palcy. J Neurol Sci. 2009;26:102–5. [Google Scholar]
- 10.Cicik E, Başerer T, Gazioğlu N, Özdemir H, Topçuoğlu H. Hipofiz adenomu tanısı ile takip edilen olgularımızın oftalmolojik değerlendirilmeleri. T Oft Gaz. 2001:301–8. [Google Scholar]
- 11.Semple PL, De Villiers JC, Bowen RM, Lopes MB, Laws ER. Pituitary apoplexy: do histological features influence the clinical presentation and outcome? J Neurosurg. 2006;104:931–7. doi: 10.3171/jns.2006.104.6.931. http://dx.doi.org/10.3171/jns.2006.104.6.931. [DOI] [PubMed] [Google Scholar]
- 12.Semple PL, Webb MK, De Villiers JC, Laws ER. Pituitary apoplexy. Neurosurgery. 2005;56:65–72. doi: 10.1227/01.neu.0000144840.55247.38. http://dx.doi.org/10.1227/01.NEU.0000144840.55247.38. [DOI] [PubMed] [Google Scholar]



