Case
An eleven-year old male patient was referred to another hospital with complaints of alternation in consciousness and stupor which developed in one-two hours. Afterwards, bilious vomiting was observed for 5–6 times; fever, diarrhea or seizures were not observed. Laboratory tests revealed mild reduction in sodium (133 mmol/L) and complete blood count, serum biochemical values, blood gases, ammonia and lactate values were found to be normal. Electrocardiographic examination, echocardiographic examination and cranial magnetic resonance imaging (MRI) were found to be normal. The pediatric patient who had a picture of encephalopathy and whose consciousness deteriorated in 24 hours was internalized in our pediatric intensive care unit. It was learned that he had upper respiratory tract infection about two weeks ago and recovered without using medication. No drug usage or trauma was described before the complaints. No additional pathology was reported in his personal history and familial history. His vaccinations had been administered in accordance with the immunization schedule. It was stated that he had age-appropriate neuromotor development.
Physical examination revealed that the patient had a Glaskow coma score of 10, stupor and confusion. His respiratory rate was increased at the time of hospitalization (60/min). His body temperature, blood pressure and apical heart beat were found to be normal. He had no sign of dehydratation. Petechia or ecchymosis was not observed. Examination of the respiratory and cardiovascular system was found to be normal. On abdominal examination, the abdomen was easy, intestinal sounds were reduced, a sense of fullness was found below the liver and a mass extending from the right middle area to the left upper quadrant was palpable. Abdominal tenderness or rebound was not found. On neurological examination, withdrawal response to stimuli was present despite central hypotony. The pupillae were isocoric and light reflex was positive. His reflexes were found to be normal. Meningeal irritation sign or pathological reflex was not found. Pathological lymphadenomegaly was not found. Strawberry jam-like bloody, juicy feces was observed with rectal examination.
Laboratoy tests were as follows: blood glucose: normal, arterial blood gas analysis :compensated metabolic asidosis (pH: 7.47, pCO2: 22.7 mmHg, cHCO3: 16.6, lactate: 1%), hemoglobin: 10.3 gr/dL, WBC: 10 800/mm3, platalets: 193 000/mm3, serum biochemistry: sodium: 35 mmol/L, potassium: 3.4 mmol/L, chloride: 96 mmol/L, calcium: 9.4 mg/dL, phosphorus: 5.7 mg/dL, C-reactive protein: negative. Urinary organic acids, tandem mass spectroscopy, lactate and ammonia levels were ordered for differential diagnosis; no pathology was found. Abdominal X-ray revealed enlargement in the small intestines and gas transfer to the distal part was not observed. Air-fluid level or subdiaphragmatic air was not observed (Figure 1). Abdominal ultrasonography directed to the abdominal mass was performed and nested bowel loops were observed starting from the right lower quadrant and extending to the subhepatic region and splenic flexura (Figure 2). Abdominal ultrasonography was compatible with ileocolic invagination. Multiple lymphadenopathies were observed inside the target lesion. Surrenal areas were open. The other organs had normal size and appearance.
Figure 1.
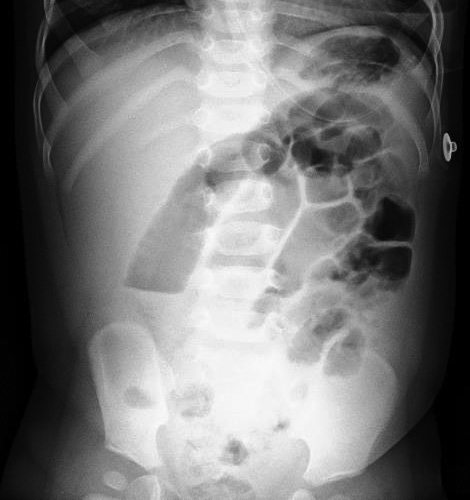
Standing abdominal X-ray
Figure 2.

Ultrasonographic appearance of the abdomen
Fluid therapy was initiated with a diagnosis of ileocolic invagination and the stomach was emptied by nasogastric intubation. Pneumotic reduction was attempted under fluoroscopy, but air passage from the cecum into the ileum was not observed and manual reduction was performed by right upper quadrant transverse incision. Signs of necrosis or perforation were not observed. Past upper respiratory tract infection and lymphoid hyperplasia were thought to be the cause which led to invagination. After surgery, the patient’s consciousness returned to normal completely. He was observed to be lively and active. His system examination findings were found to be natural. Follow-up laboratory tests were found to be normal and infectious markers were found to be negative. He was discharged four days after the operation. No problem was found in the follow-up visit one week later.
Diagnosis-Discussion Invagination Encephalopathy
The brain which is the most active organ of the human body has a fast metabolic rate. It requires a high blood supply and high level of oxygen to meet this high efficiency. On the other hand, its capacity of energy deposition is very low. Therefore, change in consciousness is added to the picture, because the brain is frequently affected in children whose states deteriorate suddenly. When the etiology leading to acute change in consciousness is treated, neurological improvement occurs and the prognosis is good. The most important point in patients who present with acute change in consciousness is to recognize the high-risk patient group in whom neurological sequela or mortality may occur. Therefore, history taking and physical examination should be performed carefully (1). At the time of admission, the airway, respiration and circulation should be evaluated rapidly and vital signs should be monitorized. The possibility of trauma should be kept in mind, immobilization should be ensured, airway stability should be provided and intubation should be performed, if necessary. For adequate brain perfusion, the blood pressure should be kept in the normal limits and fluid balance should be monitored. The blood glucose level should be measured, because hypoglycemia is one of the common causes. If convulsion is present, treatment should be administered immediately. The depth of coma should be assessed and recorded. Efficient fluid treatment should be administered and hypotonic fluids should be avoided. Previous morbidities of the patient, trauma, fever, intake of medication or toxic substance and history of seizure should be interrogated carefully. If the diagnosis cannot be made with primary care assessments, toxicologic and metabolic examination should be ordered and cranial imaging should be performed. Patients whose etiologies cannot be elucidated and whose changes in consciousness continue should preferably be monitored in intensive care units. It is important to evaluate and record the mental state of each patient in detail from the beginning using scaling systems in terms of monitoring the changes closely (2–5).
The patient whom we presented in this article was referred to us, because his neurological picture deteriorated and the etiology could not be elucidated. At the time of admission, the airway, respiration and circulation were assessed rapidly and the vital signs were monitorized. No prominent pathology was described in the history except for previous upper respiratory tract infection. His hemodynamic status was stable and body temperature was normal. He was followed up in another center before being internalized in intensive care unit and the laboratory tests and imaging methods performed there revealed no pathology. When a palpable mass was found on physical examination, urgent abdominal ultrasonography was performed to elucidate the etiology and ileocolic invagination was detected. After sugery, the patient’s consciousness returned to normal completely and additional investigation or treatment was not required.
Invagination is one of the most common causes of acute abdomen and surgical morbidities in the childhood age group. The classical clinical findings include colicky abdominal pain, vomiting and bloody stool. Bloody stool typically resembles strawberry jam (6, 7). Lethargy frequently accompanies. It may rarely lead to acute change in consciousness. When lethargy and change in consciousness occur, the typical signs may be masked. Therefore, invagination should be considered in the differential diagnosis in patients in the infancy and early childhood age groups who present with lethargy, hypotonia and change in consciousness (8). Invagination encephalopathy is a previously known picture which occurs rarely and predominantly involves neurological findings generally in the absence of classical findings. Few cases have been reported in the literature (9, 10).
In conclusion, acute change in consciousness is a difficult emergency situation which requires comprehensive approach. With this case report, we attempted to emphasize that significant clues could be obtained with history and physical examination in elucidating the etiology and invagination could present with encephalopathy alone.
Footnotes
Informed Consent: Written informed consent was obtained from the patient’s family.
Peer-review: Externally peer-reviewed.
Author Contributions: Concept - F.A., P.Ö.A.A., H.Ç.; Design - F.A., P.Ö.A.A.; Supervision - H.Ç., S.S.; Funding - H.Ç., S.S.; Materials - F.A., P.Ö.A.A., H.Ç.; Data Collection and/or Processing - F.A., P.Ö.A.A., H.Ç.; Analysis and/or Interpretation - F.A., P.Ö.A.A., H.Ç.; Literature Review - F.A., P.Ö.A.A., H.Ç.; Writing - F.A., P.Ö.A.A., H.Ç.; Critical Review - H.Ç., S.S.; Other - F.A., P.Ö.A.A., Ş.E., S.Ş.U., S.S., H.Ç.
Conflict of Interest: No conflict of interest was declared by the authors.
Financial Disclosure: The authors declared that this study has received no financial support.
References
- 1.Çıtak A. Akut bilinç değişikliği olan hastaya yaklaşım. İstanbul Üniversitesi Cerrahpaşa Tıp Fakültesi Sürekli Tıp Eğitimi Etkinlikleri. Pediatrik aciller. Sempozyum Dizisi; Nisan. 2007:s.9–15. [Google Scholar]
- 2.Karaböcüoğlu M, Yılmaz HL, Duman M. Akut bilinç değişikliği/koma. In: Demirkol D, Karapınar B, editors. Çocuk Acil Tıp Kapsamlı ve Kolay Yaklaşım. Vol. 1. Baskı; İstanbul: 2012. pp. s.197–203. [Google Scholar]
- 3.Gemke RJBJ, Tasker RC. Clinical assessment of acute coma in children. Lancet. 1998;351:926–7. doi: 10.1016/S0140-6736(05)60599-5. http://dx.doi.org/10.1016/S0140-6736(05)60599-5. [DOI] [PubMed] [Google Scholar]
- 4.Jones GD, Daly H, Murdoch IA. Coma in children. Lancet. 1998;351:1590–620. doi: 10.1016/S0140-6736(05)61164-6. http://dx.doi.org/10.1016/S0140-6736(05)61164-6. [DOI] [PubMed] [Google Scholar]
- 5.Kirkham FJ. Non-traumatic coma in children. Arch Dis Child. 2001;85:303–12. doi: 10.1136/adc.85.4.303. http://dx.doi.org/10.1136/adc.85.4.303. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Beasly SW, Hutson JM, Auldist AW. Essential paediatric surgery. 1st edition. London: Arnold; 1996. pp. 45–51. [Google Scholar]
- 7.Eliçevik M, Özcan R, Emre Ş. Çok iyi bilinen bir konunun hızlı tekrarı: invajinasyon. Cerrahpaşa Tıp Dergisi. 2006;37:41–4. [Google Scholar]
- 8.Domínguez-Carral J, Puertas-Martín V, Carreras-Sáez I, Maraña-Pérez AI, Escobar-Delgado T, García-Peñas JJ. Neurological symptoms in children with intussusception. An Pediatr. 2014;80:293–8. doi: 10.1016/j.anpedi.2013.06.034. http://dx.doi.org/10.1016/j.anpedi.2013.06.034. [DOI] [PubMed] [Google Scholar]
- 9.Goetting MG, Tiznado-Garcia E, Bakdash TF. Intussusception encephalopathy: an underrecognized cause of coma in children. Pediatr Neurol. 1990;6:419–21. doi: 10.1016/0887-8994(90)90012-p. http://dx.doi.org/10.1016/0887-8994(90)90012-P. [DOI] [PubMed] [Google Scholar]
- 10.Hoisington G, Bartlett W, Kelly T. Intussusception presenting as encephalopathy. Iowa Med. 1993;83:107–10. [PubMed] [Google Scholar]


