Abstract
Ten case reports of disseminated Mycobacterium chimaera infections associated with cardiovascular surgery were published from Europe. We report 3 cases of disseminated M chimaera infections with histories of aortic graft and/or valvular surgery within the United States. Two of 3 patients demonstrated ocular involvement, a potentially important clinical finding.
Keywords: cardiac surgery, infection, Mycobacterium chimaera
Mycobacterium chimaera was named in 2004 by Tortoli et al [1] after characterizing its nucleotide sequences in the 16S rDNA and 16–23S internal-transcribed spacer region as well as identifying its unique mycolic acid pattern derived from high-performance liquid chromatography. Since then, efforts have been made to determine its clinical relevance. Mycobacterium chimaera has been associated with pulmonary infections but appears to be less virulent than Mycobacterium avium and Mycobacterium intracellulare. However, within the past 2 years, outbreaks of M chimaera infections were reported among patients who underwent cardiothoracic surgery in 3 European countries, demonstrating evidence of pathogenicity in this setting [2–4]. In this article, we describe 3 cases of disseminated M chimaera infection in patients with prior histories of aortic graft and/or valvular surgery within the United States.
Case 1
A 66-year-old man presented with approximately 10 months of fatigue, weight loss, cough, and low-grade fevers. He underwent an ascending aortic aneurysm prosthetic graft repair 26 months prior. In view of a negative initial infectious disease workup and persistent laboratory abnormalities (including an elevated serum creatinine and hypercalcemia), a bone marrow biopsy was performed revealing non-caseating granulomas (Supplementary Figure 1). A presumptive diagnosis of sarcoidosis was made, and he was discharged on a course of oral prednisone.
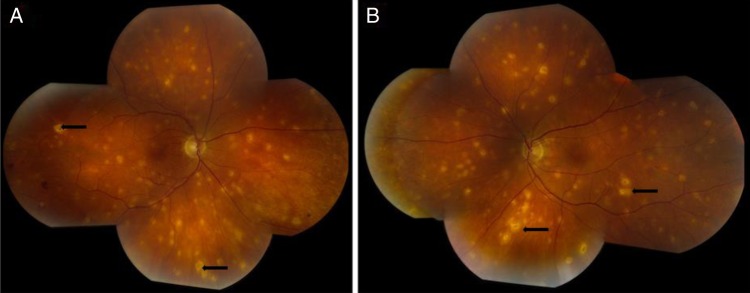
His bone marrow cultures and repeat blood cultures subsequently grew M chimaera, and he was readmitted for further workup. Ophthalmologic exam was remarkable for bilateral chorioretinitis (Figure 1); visual acuity was 20/20 in the right and 20/25 in the left. Positron emission tomography/computed tomography (PET/CT) demonstrated a fludeoxyglucose avid 1.5 cm fluid collection between the ascending aortic graft and the anterior mediastinum, raising concern for a possible graft infection (Supplementary Figure 2). The risk associated with graft explantation was felt to be prohibitively high, and the decision to proceed with conservative management was therefore made. He was started on a 4-antibiotic regimen of clarithromycin, ethambutol, rifabutin, and amikacin. Repeat blood cultures drawn 2 weeks postdischarge returned negative. Visual acuity 1 month later was 20/20 in both eyes; the chorioretinitis appeared to be inactive with scarring in prior areas of involvement and no new spots observed. Over the next 5 months, he had no recurrence of his fevers and he demonstrated significant improvement in energy levels while on the above antibiotic therapy. A repeat chest CT also demonstrated resolution of the fluid collection.
Figure 1.
Color fundus photos demonstrating diffuse bilateral chorioretinal lesions (black arrows) in the right and left eyes (A and B, respectively).
Case 2
A 74-year-old man presented with progressive confusion, urinary incontinence, and gait instability. His past medical history included severe aortic stenosis and ascending aortic aneurysm, for which he received concomitant aortic valve replacement and aortic root repair approximately 26 months ago. Magnetic resonance image of the head was negative for hydrocephalus, masses, or infarcts; cerebrospinal fluid (CSF) evaluation was within normal limits. A bone marrow biopsy demonstrated noncaseating granulomas; Gram, fungal, and acid-fast stains were negative.
A CT angiogram of the chest was performed due to the presence of sternal wound drainage noted on admission; this showed a 1.3 cm fluid collection in the anterior mediastinum at the level of the right pulmonary artery, with fluid and gas tracking towards the sternotomy. There was concern for an aortic valve and/or conduit infection, and he was started on intravenous vancomycin in view of a sternal wound swab growing coagulase-negative Staphylococcus in conjunction with 1 of 2 blood cultures being positive for the same organism on 2 occasions. Despite this, the patient clinically decompensated and required intensive care unit care with intubation and pressor support. He was not deemed a surgical candidate due to his frail physical condition and thus was transitioned to palliative care. No ophthalmologic evaluation was performed during his hospital admission.
His blood cultures returned positive for M chimaera 3 weeks after admission. However, the patient had expired by then. We retrospectively contacted the patient's outside institution for further information; mycobacterial cultures of the patient's blood, CSF, and bone marrow during his index admission did not demonstrate any growth. No autopsy study was performed.
Case 3
A 57-year-old man was admitted with fever, night sweats, and weight loss. He underwent bioprosthetic aortic valve replacement 16 months ago for aortic regurgitation. His initial workup was remarkable for splenomegaly and pancytopenia. A bone marrow biopsy showed noncaseating granulomas. A PET/CT revealed pulmonary infiltrates, prompting a bronchoscopy and bronchoalveolar lavage (BAL). His bone marrow and BAL cultures grew M chimaera, but these were believed to be contaminants. He was started on oral prednisone for presumed sarcoidosis at an outside institution.
The patient's symptoms initially improved, but he relapsed after approximately 5 months when his prednisone therapy was tapered. Blood cultures were obtained which grew M Chimaera. He was started on azithromycin, ethambutol, rifampin, and amikacin. Follow-up blood cultures 2 months after antibiotic initiation were negative. However, ethambutol and amikacin were discontinued after 3 months due to peripheral neuropathy and ototoxicity; moxifloxacin was added as a third agent. Unfortunately, monthly blood cultures after the discontinuation of ethambutol and amikacin were persistently positive for M chimaera for 12 months despite the addition of clofazimine and linezolid to his regimen. He then developed worsening thrombocytopenia and linezolid was discontinued. A transesophageal echocardiogram showed a 13 × 6 mm echodensity on the right cusp of the aortic bioprosthesis suspicious for endocarditis. Ophthalmologic examination revealed several bilateral chorioretinal lesions concerning for M chimaera involvement; visual acuity was 20/40 in the right and 20/30 in the left (without corrective lenses).
After being evaluated by the Cardiothoracic Surgery and Infectious Disease teams, plans were made for a repeat aortic valve replacement after 4 more weeks of antimicrobial therapy with azithromycin, rifampin, clofazimine, and moxifloxacin. However, the patient eventually decided to transition to hospice care without proceeding with surgery; he passed away 1 month later. No follow-up ophthalmologic examination was performed.
METHODS
Mycobacterium chimaera Identification and Sequencing
The first 500 base pairs of the 16S rRNA gene was sequenced using the Applied Biosystems MicroSeq kit as described in Hall et al [5] for Cases 1 and 2. In both cases, the sequence analysis yielded a 100% match for M chimaera using 2 libraries (a Mayo Clinic custom library and the NCBI GenBank library). No additional targets were sequenced. Matrix-assisted laser desorption ionization time-of-flight mass spectrometry (MALDI-TOF MS) profiling was not performed because MALDI is unable to differentiate M chimaera from several other members of the MAC complex [6]. Sequences for both cases were deposited in GenBank. The accession numbers for Cases 1 and 2 are KU867248 and KU878560, respectively. Case 3 was diagnosed outside and sequencing was not performed at our institution.
Environmental Analysis
The cardiac surgeries for the 3 cases took place in different outside institutions. No other known cases of disseminated M chimaera infections were identified in any of these facilities. One case triggered a 1500 patient review (http://haicontroversies.blogspot.com/2016/02/m-chimaera-infections-associated-with.html). We recommended an environmental analysis of the cardiothoracic operating theaters involved in the other 2 facilities, including an investigation of the heater-cooler units used. These studies are currently underway.
DISCUSSION
Ten case reports of disseminated M chimaera infections, described sequentially by Kohler et al [2], occurred in the setting of prior cardiothoracic surgery (for valvular heart disease and aortic aneurysm) across 3 European countries [3, 4]. Many cases were linked to airborne contamination of heater-cooler units used in cardiopulmonary bypass, prompting the European Center for Disease Prevention and Control and the Centers for Disease Control and Prevention in the United States to issue calls for increased vigilance regarding heater-cooler unit associated infections in 2015 [4, 7]. The salient demographics, clinical features, and diagnostic methods for the cases, including our own case reports, are highlighted in Supplementary Table 1. The time between the index surgery and diagnosis of infection ranged between 5 and 40 months (median, 21 months). There were few risk factors for immunosuppression among the cases: all patients were human immunodeficiency virus negative, and only 2 patients were on immunosuppressive therapy before their surgeries. Many patients presented with constitutional, nonspecific symptoms initially. It is interesting to note that 4 patients were misdiagnosed with sarcoidosis after the discovery of granulomatous involvement and initiated on steroid therapy.
Seven patients (including Cases 1 and 3; no ophthalmologic exam was performed on Case 2) were found to have positive ocular findings such as ocular emboli (n = 4), multifocal choroiditis (n = 2), and chorioretinitis (n = 1). The reason for this predilection is currently unclear; however, the high blood flow and circulation through the choroid may be an important contributing factor. Given that these are the first reported cases of M chimaera with eye findings, there is no established treatment protocol for ocular infection. However, treatment of Mycobacterium choroiditis or endophthalmitis of other species can include the use of intravitreal antibiotics, especially if there is inadequate response to systemic treatment, or if the ocular findings are severe and vision-threatening. It is therefore not unreasonable to obtain a baseline eye exam of patients diagnosed with M chimaera; further ocular treatment can then be tailored based on follow-up findings.
The M chimaera strains were generally susceptible to clarithromycin, whereas intermediate to resistant results were obtained for moxifloxacin and linezolid (Supplementary Table 2). Similar to infections caused by M avium and M intracellulare, M chimaera seems to be difficult to eradicate. Most patients had persistently positive blood or tissue cultures despite prolonged multidrug and surgical therapies, and 6 patients did not survive (Supplementary Table 3).
CONCLUSIONS
In conclusion, the 3 cases of disseminated M chimaera infection described in this manuscript are the first reported within the United States. All 3 cases took place in patients who underwent cardiovascular surgery months to years before symptom onset. Clinical manifestations were generally nonspecific, and sarcoidosis was a common misdiagnosis in a significant fraction of patients. Ocular involvement appears to be an important clinical finding. Patient outcomes are guarded despite aggressive medical and surgical therapy. The diagnosis of M chimaera infection in a postcardiovascular surgical patient should lead to a thorough investigation regarding the source of the infection.
Supplementary Data
Supplementary material is available online at Open Forum Infectious Diseases online (http://OpenForumInfectiousDiseases.oxfordjournals.org/).
Acknowledgments
Potential conflicts of interest. All authors: No reported conflicts. All authors have submitted the ICMJE Form for Disclosure of Potential Conflicts of Interest.
References
- 1.Tortoli E, Rindi L, Garcia MJ et al. . Proposal to elevate the genetic variant MAC-A, included in the Mycobacterium avium complex, to species rank as Mycobacterium chimaera sp. nov. Int J Syst Evol Microbiol 2004; 54(Pt 4):1277–85. [DOI] [PubMed] [Google Scholar]
- 2.Achermann Y, Rossle M, Hoffmann M et al. . Prosthetic valve endocarditis and bloodstream infection due to Mycobacterium chimaera. J Clin Microbiol 2013; 51:1769–73. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Kohler P, Kuster SP, Bloemberg G et al. . Healthcare-associated prosthetic heart valve, aortic vascular graft, and disseminated Mycobacterium chimaera infections subsequent to open heart surgery. Eur Heart J 2015; 36:2745–53. [DOI] [PubMed] [Google Scholar]
- 4.Sax H, Bloemberg G, Hasse B et al. . Prolonged outbreak of Mycobacterium chimaera infection after open-chest heart surgery. Clin Infect Dis 2015; 61:67–75. [DOI] [PubMed] [Google Scholar]
- 5.Hall L, Doerr KA, Wohlfiel SL, Roberts GD. Evaluation of the MicroSeq system for identification of mycobacteria by 16S ribosomal DNA sequencing and its integration into a routine clinical mycobacteriology laboratory. J Clin Microbiol 2003; 41:1447–53. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Buckwalter SP, Olson SL, Connelly BJ et al. . Evaluation of matrix-assisted laser desorption ionization-time of flight mass spectrometry for identification of Mycobacterium species, Nocardia species, and other aerobic actinomycetes. J Clin Microbiol 2016; 54:376–84. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Gotting T, Klassen S, Jonas D et al. . Heater-cooler units: contamination of crucial devices in cardiothoracic surgery. J Hosp Infect 2016; 93:223–8. [DOI] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.