Abstract
We examined US nurse practitioner (NP) and physician assistant (PA) outpatient antibiotic prescribing. Antibiotics were more frequently prescribed during visits involving NP/PA visits compared with physician-only visits, including overall visits (17% vs 12%, P < .0001) and acute respiratory infection visits (61% vs 54%, P < .001). Antibiotic stewardship interventions should target NPs and PAs.
Keywords: antibiotic resistance, family practice, physician's practice patterns/trends, primary care, respiratory tract infections/drug therapy
Antibiotic overuse in ambulatory care settings is a major problem and contributes to antibiotic resistance and avoidable adverse drug events [1, 2]. The most common conditions for which antibiotics are prescribed in ambulatory care settings are acute respiratory tract infections (ARTIs). In many cases, these conditions do not warrant an antibiotic prescription, yet inappropriate antibiotic prescribing remains common [3]. Most research assessing outpatient antibiotic prescribing has focused on physicians [4]. Less is known about the prescribing practices of nurse practitioners (NPs) and physician assistants (PAs), who collectively represent more than one quarter of the US primary care workforce [5]. Studies from more than a decade ago suggested that antibiotic prescribing rates among NPs or PAs are similar to or higher than rates among physicians, but contemporary studies are needed due to a rapidly growing NP and PA workforce [5–8]. In order to guide public health initiatives and to better understand antibiotic prescribing practices across all provider types, we compared antibiotic prescribing during ambulatory care visits involving NPs and PAs with physician-only visits.
METHODS
Data Sources
Data from the National Ambulatory Medical Care Survey (NAMCS) and the National Hospital Ambulatory Medical Care Survey (NHAMCS) from 1998 to 2011 were used to examine trends in visits involving PAs/NPs; data from 2006 to 2011 were assessed for recent patterns in both overall antibiotic prescribing and antibiotic prescribing for ARTIs according to provider types involved (PA, NP, or physician), diagnosis, and antibiotic class. Details of NAMCS and NHAMCS methodology have been described previously [9]. In brief, NAMCS samples visits to office-based physicians whereas NHAMCS samples visits to nonfederal emergency departments (EDs) and outpatient offices of noninstitutional general and short-stay hospitals to create a nationally representative sample of ambulatory care visits in the United States. During randomly assigned 1-week reporting periods throughout the year, patient demographic information, International Classification of Diseases, Ninth Revision, Clinical Modification (ICD-9-CM) data for up to 3 diagnoses, and medication prescribing data were collected for individual visits.
Study Population and Analysis
All ambulatory visits from 1998 to 2011 in the United States were divided into 2 groups: visits that involved a NP or PA, and visits that involved physicians only. Both the frequency of NP/PA visit involvement and trends in antibiotic prescribing for all conditions over this time period were assessed to determine whether significant differences exist in the proportion of visits that result in an antibiotic prescription. To account for possible differences in case mix between NP/PA and physician-only visits, a subset of visits from 2006 to 2011 involving patients ≥18 years old who received a primary diagnosis of an ARTI and had no comorbid illness, as defined by the ICD-9-CM codes assigned to that visit, were analyzed (Appendix Table 1A). Details of visit selection have been described previously [2]. Visits with NPs and PAs were first combined to provide more statistical power and then separated to provide individual estimates. Visits to nursing midwives were included in the analysis as visits to NPs.
Statistical Analysis
Logistic regression with time period as a predictor variable was used to determine whether a significant time trend existed in the proportion of visits that involved PAs/NPs during the study period. To determine whether visits involving NPs or PAs were more likely to result in an antibiotic prescription compared with physician-only visits, we performed a multivariable logistic regression model that included antibiotic prescribing as the outcome variable. We chose initial variables a priori based upon factors known to be associated with antibiotic prescribing [4]. For example, age has been associated with higher rates of prescribing, especially the very young (ages 0 through 2) and the elderly (age 65 and older) [10]. Bivariate analyses were assessed using a χ2 test. Independent variables assessed included provider type; patient age, sex, and race; visit setting; US Census region; insurance status; Metropolitan Statistical Area; and whether a comorbid condition was diagnosed at the visit (Appendix Table 1A). Statistical analyses were performed using STATA 12 (StataCorp, College Station, TX). An alpha value <0.05 was considered statistically significant.
RESULTS
Between 1998 and 2011, there were an average of 1.13 billion (95% confidence interval [CI], 1.04–1.21 billion) ambulatory visits per year in the United States based on estimates from 1 301 474 sampled visits in the NAMCS/NHAMCS. Of these visits, 6.3% (95% CI, 5.7%–6.9%) involved NPs or PAs. The proportion of visits involving NPs/PAs between 1998 and 2011 more than doubled across all ambulatory care settings (3.9%–9.0%, Ptrend < .001) and more than tripled in EDs (5.1%–17.9%, Ptrend < .001) (Appendix Figure 1).
Ambulatory visits between 2006 and 2011 involving NPs and PAs more frequently resulted in an antibiotic prescription compared with physician-only visits (17% for visits involving NPs and PAs vs 12% for physician-only visits; P < .0001) (Table 1). This pattern persisted for ARTI visits (61% vs 54%, P < .001). Broad-spectrum antibiotic prescribing (defined in Table 1) was no different among visits involving NPs and PAs compared with physician-only visits (57% of visits in which antibiotics were prescribed vs 57%; P = .61). No significant differences in antibiotic prescribing were observed when PA visits were compared with NP visits.
Table 1.
Antibiotic Prescribing by Condition and Provider-Type for Adult Ambulatory Visits, 2006–2011a
| Diagnoses | Proportion of Visits in Which Antibiotics Were Prescribed |
Proportion of Antibiotics That Were Broad-Spectrum Antibioticsb |
||||
|---|---|---|---|---|---|---|
| Visit diagnosis | Physician-only | NP/PA | P(χ2) | Physician-only | NP/PA | P(χ2) |
| All ambulatory visits | 12% | 17% | <.0001 | 57% | 57% | .61 |
| ARTI | 54% | 61% | <.001 | 56% | 53% | .10 |
Abbreviations: ARTI, acute respiratory tract infection; ED, emergency department; NP, nurse practitioner; PA, physician’ assistant.
a Total sample of respiratory visits in which antibiotics were prescribed included 52, 438 physician-only visits, and 9284 NP/PA visits. The NP/PA data includes NPs, PAs, and midwives. Midwives were not present in ED settings. Visits in which a comorbid illness was diagnosed were excluded.
b Broad-spectrum antibiotic drug classes were defined as quinolones, macrolides, broad-spectrum cephalosporins (second, third, or fourth generation), broad-spectrum penicillins (amoxicillin/clavulanate), and lincomycin derivatives. Denominator includes only visits in which antibiotics were prescribed.
After controlling for patient- and practice-level characteristics, visits that involved NPs or PAs had independently higher odds of resulting in an antibiotic prescription (odds ratio = 1.31, 95% CI, 1.19–1.43) (Appendix Table 2A).
DISCUSSION
We observed (1) a substantial increase in the proportion of ambulatory care visits in which NPs or PAs were involved and (2) a higher frequency of antibiotic prescribing for visits involving NPs and PAs compared with physician-only visits. Previous studies using NAMCS and NHAMCS found higher rates of antibiotic prescribing during visits with NPs and PAs compared with physician-only visits [8]. Our study adds to this literature by examining the most recently available data and shows that despite both modest declines in the overall rate of antibiotic use nationwide and increased participation in ambulatory care by PAs/NPs, this difference by provider type has persisted.
Several factors may contribute to potential differences in antibiotic prescribing rates between NPs/PAs and physician visits. One important reason may be that antibiotic stewardship programs, including the Centers for Disease Control and Prevention's Get Smart: Know When Antibiotics Work Program, have focused more on physicians rather than NPs or PAs. Elements of antibiotic stewardship are often included in NP, PA, and physician education curricula, suggesting that potential differences in antibiotic prescribing are more likely due to practice environment, learned clinical behaviors, or differences in patient communication rather than medical education. There may be significant differences in case mix comparing visits involving NPs and PAs with physician-only visits. However, we found that higher rates of antibiotic prescribing persisted among visits involving NPs/Pas, even when our analysis was restricted to visits for patients with the same diagnosis (ARTI). Regardless of provider background or training, the widespread use of antibiotics for ARTIs raises concerns about avoidable increases in antibiotic-resistance and adverse drug events at both the individual and population levels.
There are important limitations to consider when using NAMCS and NHAMCS to analyze NP and PA prescribing. These surveys provide important estimates of healthcare delivery and patient care; however, the sampling methods were designed to produce estimates that are representative of visits to office-based and ED physicians and may not be representative of NP and PA practices in these settings [11]. Other limitations to our study include (1) a smaller number of visits to NPs and PAs compared with physicians and (2) potential unmeasured differences in case mix or illness severity seen by physicians compared with NPs or PAs. Finally, NPs and PAs frequently practice in nontraditional ambulatory care settings (eg, retail clinics or urgent care settings) that are not generally captured in NAMCS or NHAMCS and were not included in this study.
CONCLUSIONS
Future efforts should seek to understand the differences in antibiotic prescribing observed in the present study, including the assessment of workplace and patient communication dynamics that may contribute to excess antibiotic prescribing. As the proportion of outpatient visits involving NPs and PAs continues to increase, interventions to reduce inappropriate antibiotic use in ambulatory care should target these providers in addition to physicians. Finally, it is important to accurately characterize NP and PA practice. Therefore, US healthcare survey data should implement sampling strategies that capture nationally representative data for NP and PA practice. Regardless of provider type, antibiotic prescribing for ARTIs and use of broad-spectrum antibiotics in our study was much higher than desired and necessary, mandating ongoing evaluation and intervention to minimize antibiotic resistance, adverse drug events, and poor clinical outcomes that result from inappropriate antibiotic prescribing.
Acknowledgments
Financial support. Funding for this study was provided by the Centers for Disease Control and Prevention (Atlanta, GA).
Potential conflicts of interest. All authors: No reported conflicts. All authors have submitted the ICMJE Form for Disclosure of Potential Conflicts of Interest.
APPENDIX
Table A1.
Acute Respiratory Tract Infection ICD-9-CM Codes, Comorbid Conditions Used as Exclusion Criteria, and Patient Characteristics Included as Independent Variables in the Logistic Regression Model
| Description | ICD-9-CM Codes | |
|---|---|---|
| ARTIs | Sinusitis, pharyngitis, tonsillitis, otitis media, mastoiditis, streptococcal sore throat, peritonsillar abscess, nonviral pneumonia, nasopharyngitis, laryngitis/tracheitis, unspecified ARTI, bronchitis (acute and not otherwise specified, bronchiolitis, viral pneumonia, influenza, cough | 034, 381–383, 461–463, 475, 481–486, 460, 464–466, 480, 487–488, 490, 786.2 |
| Comorbid conditions |
Conditions: chronic obstructive pulmonary disease, asthma, congestive heart failure, ischemic or hypertensive heart disease, diabetes mellitus, malignant neoplasms and neoplasms of uncertain or unspecified behavior, cerebrovascular disease, acute or chronic renal disease, or human immunodeficiency virus infection Immunosuppressive medications: methotrexate, etanercept, infliximab, adalimumab, tacrolimus, cyclosporine, mycophenolate, prednisone, methylprednisolone, prednisolone, dexamethasone |
491–493, 496, 428, 410–414, 402, 404, 250, 140–208, 235–239, 430–438, 403, 580–588, 042, v08 |
| Patient characteristics included as independent variables in the logistic regression model | Patient age; patient sex and patient race; visit setting; US Census region; insurance status; Metropolitan Statistical Area; and presence of a comorbid condition diagnosis at the visit | Not applicable |
Abbreviations: ARTI, acute respiratory tract infection; ICD-9-CM, International Classification of Diseases 9th Revision Clinical Modification.
Table A2.
Characteristics Associated With Antibiotic Prescribing in Ambulatory Visits, 2006–2011
| Factor | Proportion of Visits in Which Antibiotics Were Prescribed | P(χ2) | Adjusted OR (95% CI) for Antibiotic Prescribing |
|---|---|---|---|
| (1) | |||
| Provider Type | <.0001 | ||
| NP or PA absent | 12% | 1.00 | |
| NP or PA present | 17% | 1.31 (1.19–1.43) | |
| Age | <.0001 | ||
| 0–17 | 20% | 1.00 | |
| 18–39 | 14% | 1.04 (.97–1.11) | |
| 40–59 | 11% | 0.84 (.79–.90) | |
| 60+ | 8% | 0.70 (.65–.76) | |
| Sex | <.01 | ||
| Male | 13% | 1.00 | |
| Female | 12% | 1.02 (.98–1.06) | |
| Race | <.001 | ||
| White | 12% | 1.00 | |
| Black | 13% | 0.93 (.87–1.00) | |
| Other | 11% | 0.78 (.70–.86) | |
| Setting | <.0001 | ||
| Office | 11% | 1.00 | |
| Outpatient department | 12% | 1.11 (1.00–1.23) | |
| Emergency department | 21% | 2.15 (2.02–2.28) | |
| United States Census region | <.0001 | ||
| Northeast | 11% | 1.00 | |
| Midwest | 13% | 1.20 (1.08–1.34) | |
| South | 14% | 1.28 (1.14–1.44) | |
| West | 11% | 1.10 (.96–1.26) | |
| Insurance status | <.0001 | ||
| Private | 13% | 1.00 | |
| Public | 11% | 0.86 (.82–0.91) | |
| Self-pay/other | 13% | 0.94 (.88–1.00) | |
| Metropolitan Statistical Area | 0.05 | ||
| Non-metropolitan | 14% | 1.00 | |
| Metropolitan | 12% | 0.89 (.76–1.03) | |
| Comorbiditya | <.02 | ||
| Comorbidity absent | 13% | 1.00 | |
| Comorbidity present | 12% | 1.24 (1.19–1.30) | |
| Diagnosis | <.0001 | ||
| ARTI | 56% | 12.81 | |
| Other diagnosis | 8% | 1.00 |
Abbreviations: ARTI, acute respiratory tract infection; CI, confidence intervals; NP, nurse practitioner; OR, odds ratio; PA, physician assistant.
a A comorbidity was defined as a chronic disease and/or immunosuppressive medication, see Appendix Table 1A.
Figure A1.
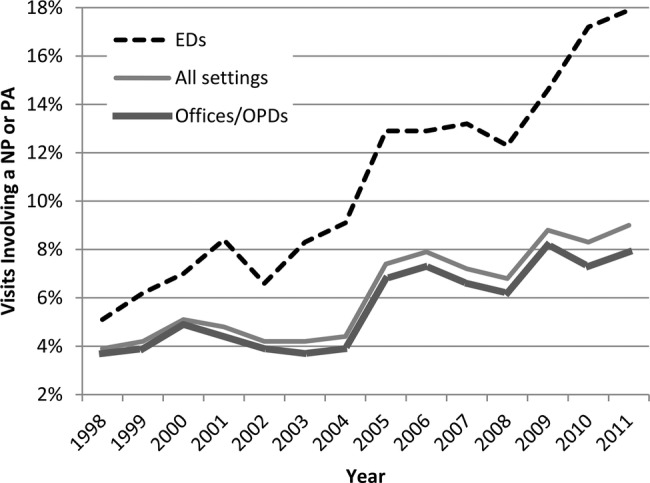
Proportion of outpatient visits involving a nurse practitioner (NP) or physician assistant (PA), 1998 to 2011.
References
- 1.Dantes R, Mu Y, Hicks LA et al. Association between outpatient antibiotic prescribing practices and community-associated Clostridium difficile infection. Open Forum Infect Dis 2015; 2:ofv113. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Bell BG, Schellevis F, Stobberingh E et al. A systematic review and meta-analysis of the effects of antibiotic consumption on antibiotic resistance. BMC Infect Dis 2014; 14:13. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Barnett ML, Linder JA. Antibiotic prescribing to adults with sore throat in the United States, 1997–2010. JAMA Intern Med 2014; 174:138–40. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Shapiro DJ, Hicks LA, Pavia AT, Hersh AL. Antibiotic prescribing for adults in ambulatory care in the USA, 2007–09. J Antimicrob Chem 2014; 69:234–40. [DOI] [PubMed] [Google Scholar]
- 5.Primary Care Workforce Facts and Stats: Overview. Agency for Healthcare Research and Quality. Rockville, MD: U.S. Department of Health & Human Services, 2012. [Google Scholar]
- 6.Brown DF, Sullivan AF, Espinola JA, Camargo CA Jr. Continued rise in the use of mid-level providers in US emergency departments, 1993–2009. Int J Emerg Med 2012; 5:21. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Goolsby MJ. Antibiotic-prescribing habits of nurse practitioners treating adult patients: antibiotic use and guidelines survey adult. J Am Acad Nurse Pract 2007; 19:212–4. [DOI] [PubMed] [Google Scholar]
- 8.Grijalva CG, Nuorti JP, Griffin MR. Antibiotic prescription rates for acute respiratory tract infections in US ambulatory settings. JAMA 2009; 302:758–66. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Centers for Disease Control and Prevention. Ambulatory Health Care Data. 2013. Available at: http://www.cdc.gov/nchs/ahcd.htm Accessed 14 November 2013.
- 10.Hicks LA, Bartoces MG, Roberts RM et al. US outpatient antibiotic prescribing variation according to geography, patient population, and provider specialty in 2011. Clin Infect Dis 2015; 60:1308–16. [DOI] [PubMed] [Google Scholar]
- 11.Morgan PA, Strand J, Ostbye T, Albanese MA. Missing in action: care by physician assistants and nurse practitioners in national health surveys. Health Serv Res 2007; 42:2022–37. [DOI] [PMC free article] [PubMed] [Google Scholar]


