Abstract
Green buildings are designed to have low environmental impacts and improved occupant health and well-being. Improvements to the built environment including ventilation, lighting, and materials have resulted in improved indoor environmental quality (IEQ) in green buildings, but the evidence around occupant health is currently centered around environmental perceptions and self-reported health. To investigate the objective impact of green buildings on health, we tracked IEQ, self-reported health, and heart rate in 30 participants from green and conventional buildings for two weeks. 24 participants were then selected to be relocated to the Syracuse Center of Excellence, a LEED platinum building, for six workdays. While they were there, ventilation, CO2, and volatile organic compound (VOC) levels were changed on different days to match the IEQ of conventional, green, and green+ (green with increased ventilation) buildings. Participants reported improved air quality, odors, thermal comfort, ergonomics, noise and lighting and fewer health symptoms in green buildings prior to relocation. After relocation, participants consistently reported fewer symptoms during the green building conditions compared to the conventional one, yet symptom counts were more closely associated with environmental perceptions than with measured IEQ. On average, participants had 4.7 times the odds of reporting a lack of air movement, 1.4 more symptoms (p-value = 0.019) and a 2 bpm higher heart rate (p-value < 0.001) for a 1000 ppm increase in indoor CO2 concentration. These findings suggest that occupant health in green and conventional buildings is driven by both environmental perceptions and physiological pathways.
Keywords: Green Buildings, Carbon Dioxide, Environmental Perceptions, Symptoms, Heartrate
Graphical Abstract
1.0 Introduction
Over the past century building design and operation has changed in response to social and economic stressors with unanticipated impacts to human health and well-being. For example, following World War II, buildings in Germany were rapidly reconstructed without allowing construction materials time to off-gas. The resulting health effects from exposures to these chemicals spurred the Building Biology field of study [1]. In the United States, two decades later, the oil crisis led to the construction of increasingly air-tight buildings, which require less energy to heat and cool [2]. The incidence of common heath symptoms ranging from viral infections to cognitive impairments were elevated in many of these buildings, and referred to generally as sick building syndrome (SBS) [3, 4]. The economic costs of SBS in poorly ventilated buildings are significant and far exceed the energy savings [5, 6]. In addition, research conducted by the Center for Indoor Environments and Energy at the Danish Technological University has demonstrated that increased symptoms and decreased performance are associated with a number of indoor design, operating, maintenance, and environmental exposure issues [7].
The indoor environment has been increasingly monitored since SBS was first identified. The Environmental Protection Agency (EPA) set out to characterize the Indoor Environmental Quality (IEQ) in typical office buildings in mid-90s through the Building Assessment Survey and Evaluation (BASE) study. They measured a wide array of environmental pollutants and building parameters in one hundred buildings in the U.S. [8]. 17% of the buildings had ventilation rates below the ASHRAE standard of 20 cfm per person and 40% were not operating the HVAC unit according to design specifications. Ventilation deficits contributed to elevated levels of other contaminants in the buildings investigated. An average total volatile organic compound (TVOC) concentration of 453 μg/m3 was measured.
The health problems that arose from conventional buildings with inadequate ventilation contributed to the advent of sustainable design or green building strategies, such as the US Green Building Council’s (USGBC) Leadership in Energy and Environmental Design (LEED) rating system. LEED aims to reduce the environmental footprint of buildings without compromising occupant health. They provide credits to new and existing buildings for adopting green design, operation, and maintenance. LEED then classifies buildings with a rating depending on the number of credits a building qualifies for. While many of the credits are aimed at energy efficiency and environmental performance, the LEED rating system also includes a section on Indoor Environmental Quality (IEQ), which details guidelines for improving ventilation and filtration, using low-emitting materials, controlling indoor chemical and pollutant sources, improving thermal and lighting conditions, offering daylight views to building occupants, and monitoring ventilation [9].
These IEQ credits translate to IEQ improvements in green buildings [10]. Exposure assessments comparing conventional buildings to green buildings show reductions in several key pollutants associated with symptom reports including particles, nitrogen dioxide, volatile organic compounds, and allergens [11–13]. However, the IEQ improvements did not extend to CO2 or air exchange rate, demonstrating the influence of energy efficiency on green building operation and design. Notably, the credit for increasing ventilation by 30% over the ASHRAE standard was obtained by only 40% of new constructions and 23% of existing buildings in LEED v2009 [6].
Several studies have found reductions in reported symptoms and improved health in home, school, and office settings in green buildings as a result of IEQ improvements [11, 14–17]. These studies, and others, indicate health benefits in green buildings, but lack objective measurements of health or sufficiently large cohorts of buildings. Considering that participants in these studies were not blinded to their exposure group (i.e. whether they were in green or conventional buildings), they may also be biased when self-reporting their health [10].
This paper builds on the the CogFx study, which found impacts on an objective measure of health – cognitive function – from exposure to different building conditions [18]. The IEQ, self-reported health, and heart rate of 30 participants in green and conventional buildings was tracked over the course of two weeks. 24 of the participants were then relocated to the Syracuse Center of Excellence (CoE), a LEED platinum green building, for six days. In addition to the naturally green environment, we simulated enhanced ventilation (green+) and typical VOC source (conventional) environments on different days of the study. This study design allowed us to test 1) the baseline difference in IEQ and health in a sample of green and conventional buildings, 2) how health is related to environmental perceptions and CO2 and 3) how subjective and objective measures of health change in response to blinded and unblinded built environment interventions.
2.0 Methods
In a previous publication [18], we described the methods for a study of workers and cognitive function in the CoE. This paper focuses on other aspects of that study including: monitoring participants for two weeks at their place of work prior to relocation to the CoE, physiological measurements, and daily questionnaires. For readers not familiar with the previous publication, we briefly describe the methods of both phases of the study (Phase I = prior to relocation; Phase II = after relocation to CoE), and describe in detail the methods for the physiological measurements and questionnaires.
Study Population
30 knowledge workers (professional grade employees like architects, designers, programmers, engineers, creative marketing professionals, middle management, etc.) in the Syracuse area were recruited to participate in a longitudinal study of the built environment and health during the fall of 2014. The study population was restricted to non-sensitive persons by excluding current smokers and people with asthma, claustrophobia or schizophrenia. The 24 participants with the best compliance through Phase I were selected to complete Phase II of the study, which required spending six workdays in the CoE. The demographic distributions did not change significantly from Phase I to Phase II (Table 1). All participants were administered informed consent and compensated for their participation in accordance with the Harvard T.H. Chan School of Public Health Institutional Review Board.
Table 1.
Demographic breakdown of participants in each phase of the study.
| Phase I | Phase II | |
|---|---|---|
| Gender | ||
| Male | 15 | 10 |
| Female | 15 | 14 |
| Age | ||
| 20–30 | 9 | 8 |
| 31–40 | 5 | 3 |
| 41–50 | 7 | 6 |
| 51–60 | 5 | 4 |
| 61–70 | 4 | 3 |
| Ethnicity | ||
| White/Caucasian | 26 | 22 |
| Black or African American | 1 | 1 |
| American Indian or Alaskan | 1 | 0 |
| Latino | 1 | 1 |
| No Response | 1 | 0 |
| Highest level of Schooling | ||
| High School Graduate | 1 | 1 |
| Some College | 2 | 2 |
| College Degree | 14 | 13 |
| Graduate Degree | 13 | 8 |
| Job Category | ||
| Managerial | 5 | 5 |
| Professional | 20 | 15 |
| Technical | 1 | 1 |
| Secretarial or Clerical | 1 | 1 |
| Other | 3 | 2 |
Phase I
Participants worked in their regular work environment for the first two weeks of the study. They received a sensor package including a Netatmo Weather Station and a Basis B1 watch. They were instructed to place the Netatmo on their desk and wear the Basis for the duration of the study. The Basis measured distal skin temperature, skin conductance, heart rate, and acceleration. The Netatmo measured temperature, humidity, CO2 concentrations in parts per million (ppm), and sound levels in decibels every 5 minutes. Instruments were calibrated before each phase of the study to 0 and 3000 ppm using an independently calibrated TSI Q-Trak model 7575. In addition, the Netatmo units were tested with 400 and 1000 ppm calibration gas after each phase of the study to determine if the sensors drifted during the two week period.
The participants also completed a series of surveys over the course of the study, derived from the BASE study [8]. At recruitment, they filled out a baseline survey, which obtained demographic information and information about their current work environment, and health. Each business day during the four weeks of the study they completed a daily survey on their time activity, potential exposures, and health. Lastly, they took a follow up survey at the end of each phase of the study, which asked questions about their work environment and health over the past two weeks.
Symptom counts were derived from the daily survey by asking whether participants had experience any of the following symptoms that day: respiratory (wheezing; chest tightness; sneezing; and shortness of breath), eyes and skin (tired or strained eyes; dry, itchy or irritated eyes; and dry or itchy skin), viral (headache; sore or dry throat; stuffy nose or congestion; wheezing; and cough), cognitive (feeling depressed, unusual tiredness; tension, irritability or nervousness; difficulty remembering things or concentrating; and dizziness or lightheadedness), and sensory (pain or arthritis and numbness in the hands or wrists). Total symptom counts were a summation of these 19 symptoms.
Phase II
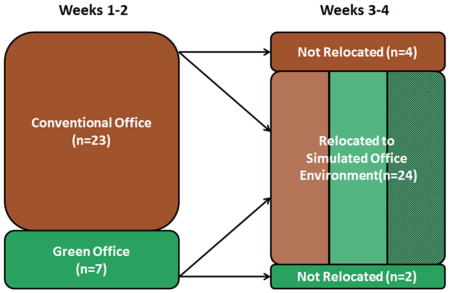
24 of the 30 participants were selected to relocate to the Willis H. Carrier Total Indoor Environmental Quality (TIEQ) labs in the CoE for six days during the next two weeks. The remaining six participants continued to complete surveys and wear the Basis watch in their regular work environment (Figure 1). The TIEQ lab consists of two rooms, each set up like a traditional office with 12 identical cubicles. While in the TIEQ lab, all 24 participants were exposed to conventional, green and green+ conditions by changing the indoor environment on different days. During the green and conventional conditions, the ventilation rate was equivalent to 20 cubic feet per minute (cfm) of outdoor air per person. This rate was doubled during the green+ conditions. On the conventional day, common sources of VOCs were placed to the supply air duct to reach a TVOC concentration of 550 μg/m3 in the chambers, which straddles the both the LEED credit guideline of 500 μg/m3 and the BASE study mean concentration of 453 μg/m3. Lastly, the independent effect of CO2 was tested in two conditions where pure CO2 was added to the chambers to reach 950 ppm and 1400 ppm. Detailed methods of building conditions can be found in our previous report investigating decision-making performance [18].
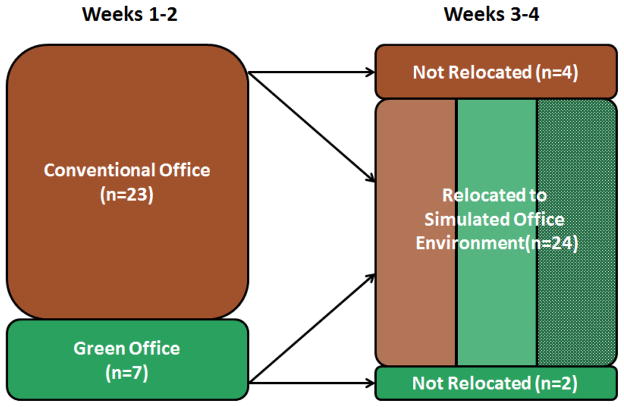
Figure 1.
Study design schematic. 30 participants were recruited from conventional and green office buildings in the Syracuse area. 24 were selected to spend 6 days in the Syracuse Center of Excellence, where they were exposed to simulated Conventional, Green and Green+ building conditions.
Statistical Methods
The CO2, temperature and RH data from the Netatmos was first limited to the hours of 9AM to 5PM on business days during the study period. As mentioned previously, the CO2 sensors in the Netatmos were tested with calibration gas after each phase of the study. An offset equal to the difference between 400 ppm and what the instrument read as 400 ppm using the calibration gas was calculated for all devices during each phase. The CO2 data was adjusted first by this offset and second by a scaling factor to match the 1000 ppm reading to 1000 ppm. This process corrected both the intercept and slope of the collected data to match experimentally derived values.
The Basis watch provided heart rate data with one second resolution for each participant. Minute averages were computed before compiling all participant data together. The real-time measurements by the Basis watch were merged with the in-office CO2 data. 5-minute averages were paired to CO2 data, which collects data with a 5 minute time resolution. Lags and moving averages of the IEQ data were calculated from the combined database. Lastly, the dataset was restricted to hours when the participant reported on the survey being in the office for more than 30 minutes to ensure that the physiological measurements occurred in same indoor environment as the IEQ measurements. The Netatmos were running for 66% of the study’s person-time, the Basis watches collected data for 36% of the person-time, and participants reported being in their office 76% of the time. The period of time when both sensors were collecting concurrently while participants reported being in the office amounted to 26% of person-time (i.e. 26% of the total time the participants were in the study); however, this still amounted to approximately 60,000 minutes of data total. The ratio of data collection by gender and age before and after relocation was constant: 1) 60% of data came from male participants prior relocation compared to 48% afterwards and 2) 90% of data came from participants over 40 years old prior to relocation compared to 87% afterwards. This indicates that the results are not confounded by differential use of the devices by participants during different phases of the study and that the data is missing at random. The data is not missing completely at random, as there were certain study days at the beginning and end of each phase when more data was missing while participants got set up with the devices.
During the green condition in the CoE, ozone concentrations in one chamber were over 11 times higher than the next highest concentration. The participants in this chamber reported 80% more symptoms on this day compared to those in the other chamber. Generalized additive mixed effect models (GAMMs) were used to account for variable ozone concentrations in the CoE. The fixed effects were ozone concentration in each room and building condition (Conventional, Green and Green+), treating participants as a random effect. Symptom counts fit a quasipoisson distribution. The estimates of this model were used to compute symptom counts at a median ozone concentration of 5.5 μg/m3.
GAMMs were also used to test the effect of CO2 on symptoms and heart rate after controlling for time in the CoE. Participant ID was treated as a random intercept to control for inter-personal confounders. The residuals were normally distributed and homoscedastic for all models. Linearity in the effect of environmental exposures on heart rate and symptoms were tested with penalized splines (4 knots, cubic regression). Temperature and actigraphy (more specifically, wrist accelerometry) were kept as penalized splines due to non-linear relationships. A distributed lag analysis was conducted on the association between CO2 and heart rate to determine the exposure window of interest. 5, 10, 30, 60 and 90 minutes lags were included. Of the lags tested, the significance of the effect was minimized at 60 minute prior exposure to CO2 (Table 2). The final heart rate model had the following specification:
Table 2.
Effect of CO2 on heart rate at different lags prior to the observed heart rate. The univariate model treats each lag independently with relevant confounders, while the multivariate model includes all lags concurrently.
| Lag (min) | Univariate Model | Multivariate Model | ||
|---|---|---|---|---|
| Estimate | p-value | Estimate | p-value | |
| 5 | 0.852 | 0.033 | 0.730 | 0.65 |
| 10 | 0.818 | 0.042 | −0.445 | 0.79 |
| 30 | 0.956 | 0.022 | −1.12 | 0.21 |
| 60 | 2.3 | <0.001 | 2.67 | 0.08 |
| 90 | 2.74 | <0.001 | 1.01 | 0.48 |
Where:
HRij= predicted beats per minute for subject i at minute j
i = 1,…,30 subjects
j =1,…,n minutes (n is participant specific)
β1= fixed intercept
β2= fixed effect of working in the CoE
β3= fixed effect of 60 minute prior CO2 concentration
β4= fixed effect of 5 minute prior relative humidity
s(Temp) = penalized spline of 5 minute prior average room temperature
s(Accel) = penalized spline of 5 minute prior average wrist actigraphy
b1i = random effect of intercept for subject i
Analyses were performed using the open-source statistical package R version 3.0.0 (R Project for Statistical Computing, Vienna, Austria).
3.0 Results
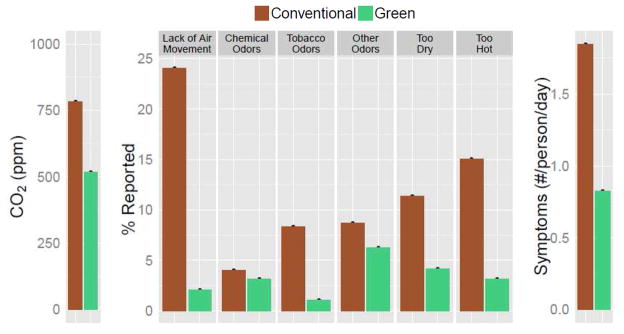
The IEQ and occupant comfort of the participants during the two weeks in their regular work environment is summarized in Figure 2. Participants in green buildings experienced significantly lower CO2 concentrations (518 ppm vs. 784 ppm) and reported improved IEQ compared to those in conventional buildings. Reports of too little air movement were reduced by 91%, chemical odors by 22%, tobacco smoke odors by 88%, other unpleasant odors by 28%, dryness by 63%, and high indoor temperatures by 79% among participants in green buildings. They were also more satisfied with lighting conditions; all participants in green buildings were satisfied or very satisfied with lighting conditions compared to 60% in the conventional buildings. This satisfaction was driven by improved daylighting as participants from green buildings reported only slightly better electric lighting. Despite that, they reported frequent flickering lights, electric light with undesirable color, insufficient desk lighting, and computer glare 13–30% less frequently, depending on the question. Participants from green buildings were generally more comfortable in their chair and at their desk and more satisfied with the noise in their office. Participants from green buildings were dissatisfied or very dissatisfied with their noise levels 14% of the time compared to 39% of the time for the rest of the participants. Improvements were primarily driven by reductions in noise from outside and from HVAC systems.
Figure 2.
CO2 concentration, environmental perceptions and symptom counts in green and conventional buildings prior to relocation.
Information on participants’ self-reported health was collected at the end of each workday. The participants in green buildings reported half as many symptoms per day as those in the conventional buildings (0.82 symptoms per person per day vs. 1.85 symptoms per person per day) (Figure 2). Respiratory, eyes and skin, viral, cognitive, and sensory symptoms were reduced by 67%, 70%, 50%, 28% and 65%, respectively, in green buildings compared to conventional buildings prior to relocation. Leaving the building for the weekend caused 38% of the symptoms to get better for participants in conventional buildings compared to 19% for participants in green buildings, suggesting that the greater number of symptoms experience by those in conventional buildings were likely caused by building-related factors rather than differences in the participants.
After relocating to the CoE, participants were exposed to three building conditions: conventional, green and green+. By design, CO2 concentrations were lower in the green building conditions than the conventional condition (Figure 3). The CO2 concentration during the conventional condition was 950 ppm, which exceeded the observed concentration in the conventional buildings prior to relocation. Similar trends in symptom counts were observed after relocation as before; symptom counts were reduced by 0.75 during the green conditions in the simulated environment after adjusting for ozone concentrations. The same building types prior to relocation had a 1 symptom difference.
Figure 3.
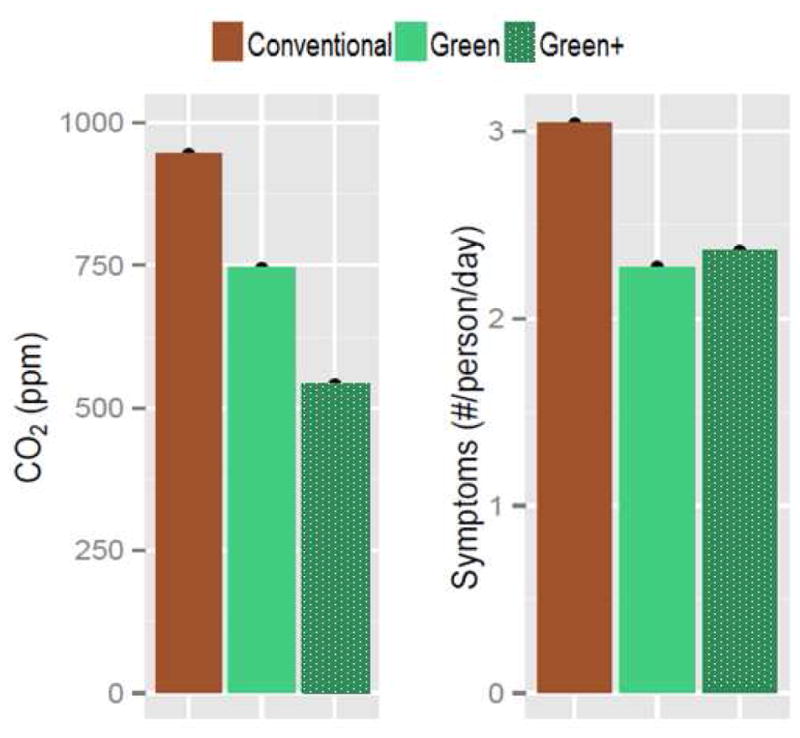
CO2 concentration and predicted symptom counts for the 24 participants in the Syracuse Center of Excellence during the conventional, green, and green+ conditions at the median ozone concentration of 5.5 μg/m3.
The relationship between CO2 and symptoms was modeled using data from both phases of the study, with environmental perceptions serving as an intermediary variable (Table 3). The odds of a participant perceiving a lack of air movement are 4.71 times higher for a 1000 ppm increase in CO2. Participants who perceive a lack of air movement report on average 1.67 more symptoms each day. Lastly, a 1000 ppm increase in CO2 is associated with a 1.43 increase in the number of symptoms per participant per day. All models were adjusted for time in CoE since participants were anticipating changes in IEQ, leading to placebo effects. Participants did report 1.43 more symptoms per person while in the CoE, despite the odds of reporting a lack of air movement decreasing by 37%.
Table 3.
Model results of the relationship between CO2, perceived lack of air movement, and reported symptoms adjusting for participant and time in the Center of Excellence.
| Estimate | Exp(β) | p-value | |
|---|---|---|---|
| Lack of Air Movement ~ CoE + CO2 | |||
| Intercept | −2.89 | <0.001 | |
| CoE | −0.464 | 0.629 | 0.115 |
| CO2 | 1.55 | 4.71 | <0.001 |
|
| |||
| Symptoms ~ CoE + Lack of Air Movement | |||
| Intercept | 0.102 | 0.521 | |
| CoE | 0.616 | 1.85 | <0.001 |
| Lack of Air Movement | 0.515 | 1.67 | <0.001 |
|
| |||
| Symptoms ~ CoE + CO2 | |||
| Intercept | 0.132 | 0.481 | |
| CoE | 0.425 | 1.53 | <0.001 |
| CO2 | 0.357 | 1.43 | 0.0191 |
Workstation CO2 concentrations were also compared to heart rate (Table 4). A 1000 ppm increase in CO2 was associated with a 2.3 bpm increase in heart rate after adjusting for potential confounders. Time in the CoE was associated with a nearly 5 bpm decrease in heart rate. Increases in humidity also resulted in slightly lowered heart rate. Based on the penalized spline, heart rate increased with temperature up to 24 °C before inverting; however, 80% of temperature data was below 24 °C. As expected, actigraphy had a strong positive relationship with heart rate.
Table 4.
Model results of the relationship between 60-minute prior CO2 and heart rate after adjusting for participant, time in the Center of Excellence, 5-minute prior relative humidity, 5-minute prior temperature, and 5-minute prior actigraphy.
| Parameter | Estimates | p-value |
|---|---|---|
| Intercept | 69.3 | <0.001 |
| CoE | −4.41 | <0.001 |
| CO2 | 2.31 | <0.001 |
| Relative Humidity | −0.204 | <0.001 |
| Temperature Spline | <0.001 | |
| Actigraphy Spline | <0.001 |
4.0 Discussion
The green buildings in this study had better IEQ: CO2 concentrations were lower and participants reported improved air quality, odors, noise, lighting, thermal comfort and ergonomics in green buildings. Participants also reported fewer symptoms in green buildings prior to relocation and in simulated green building conditions after relocation. These findings are consistent with the body of literature on green buildings, IEQ and health. In a review by Allen et al., the findings of 17 studies generally agree that all the IEQ parameters listed above are improved in green buildings with the exception of noise, which has mixed findings among the green buildings previously investigated. Individual studies have related indoor air quality, thermal comfort, ergonomics and lighting to increased symptoms [19–22]. However, these studies on green buildings are unable to attribute the increase in symptoms to physiological or psychological precursors. In other words, they are unable to answer whether it is more important to create a high-performing environment or simply the perception of a high-performing environment. By blinding participants to their environmental conditions and introducing physiological measurements, we are able to address this question.
Participants reported environmental perceptions and symptoms while being blinded to test conditions in the CoE. During the conventional condition when common sources of VOCs were added to the chambers, participants perceived a change in air quality and reported more symptoms. However, when ventilation rates were doubled for the green+ conditions, participants did not report better IEQ (lack of air movement reports were 6% higher for the green+ conditions than the green condition) and symptom counts were slightly higher (Figure 3). This finding suggests that environmental perceptions play an important role in self-reported health metrics, even when environmental perceptions are misaligned with actual IEQ conditions. While subjective measures of health may be biased due to environmental perceptions, environmental perceptions have been linked with objective health outcomes in many fields of study. Most prominent is the impact of natural environments on health through psychological pathways. For example, in a seminal study by Ulrich et al., patients with views of nature were prescribed less pain medication, had fewer complications and recovered faster than those with no views [23].
CO2 was found to influence both environmental perceptions and self-reported health. As a proxy for ventilation, the relationship between CO2 and lack of air movement shows that participants were able to perceive poor ventilation. In addition, CO2 concentration was associated with symptoms, which supports the literature on CO2, ventilation and health [24, 25]. This result combines the effect of ventilation and the direct effect of CO2 on symptoms as ventilation rate was not included in the model. It is still unclear to what degree symptoms can be attributed to each of these factors. However, we did observe elevated symptom counts during the conditions when ultrapure CO2 was added to the chambers while ventilation rate was held constant, controlling for ozone concentrations.
CO2 was also associated with objective, physiological indicators of health. Participants experienced a two bpm increase in heart rate with a 1000 ppm increase in CO2 levels. The physiological mechanism behind this association is the autonomic nervous system. The carotid body in the carotid artery is a chemoreceptor that monitors CO2 levels in the blood. When it senses hypercapnia, it signals the sympathetic component of the autonomic nervous system resulting in elevated blood pressure, respiration, and heart rate. Historically CO2 exposures below 5000 ppm were not anticipated to affect blood CO2 levels, but recent findings by Vehvilainen et al. show linear increases in the partial pressure of CO2 in blood (pCO2) as exposures to ambient CO2 were increased from 500 ppm to 4000 ppm through changes in ventilation rate. They also see other physiological responses consistent with increased sympathetic stimulation including changes to heart rate variability and increases to peripheral blood circulation [26]. Another study by Kajtar and Herczeg, which exposed participants to levels of CO2 ranging from 600 ppm to 5000 ppm, supports our findings and those by Vehvilainen. Participants showed larger reductions in blood pressure and decreased heart rate after spending several hours at 600 ppm compared to when those participants were exposed to 1500, 2500, and 5000 ppm of pure CO2 [27].
Autonomic dysfunction has a wide array of health impacts to cognitive, urinary, sexual, and digestive systems [28]. Activation of the autonomic system through stress decreases strategic ability and working memory [29], which supports finding by Allen et al and Satish et al. showing a decrease in decision making performance between 550 and 2500 ppm of CO2. The more strategic domains of cognitive function, such as crisis response, information usage, and strategy were the most significantly impacted [18, 30]. The hour-long exposure to CO2 prior to cognitive testing in Satish et al. aligns with the lag in heart rate response found in this study. In Kajtar and Herczeg (2012), participants found more typographic errors when reading through a document at 600 ppm of CO2 as compared to 3000 or 4000 ppm when their heart rate and blood pressure was elevated. Increased heart rate, or tachycardia, can have other acute effects including dizziness, lightheadedness, and shortness of breath. All of these symptoms were more frequently reported by participants in the CoE when CO2 levels were increased while holding all other exposures constant (Green+ days vs. Moderate/High CO2 days).
This study has several limitations. Many of the outcomes were self-reported and therefore can be biased by the participants’ perceptions. Although participants were blinded to test conditions, they were not blinded to the relocation and were aware that they may be exposed to VOCs or CO2. Direct comparisons of pre- and post-relocation data would be confounded by perceptions, so all models were controlled for time in the CoE. Due to the random recruitment process, the number of participants from green buildings is smaller than the number from conventional buildings, which limited the statistical significance of comparisons between the two groups. These seven participants also came from two buildings that may not be generalizable to all green buildings, and the environmental conditions simulated in the TIEQ lab may not be representative of conventional or green buildings as a whole. Lastly, a significant portion of Netatmo and Basis data was missing; however, the missingness appears to be at random.
5.0 Conclusion
Participants in green buildings experienced improved indoor environmental quality compared to those in conventional buildings, and as a result they also reported fewer symptoms. These symptoms were caused by two distinct mechanistic pathways. Psychologically, when participants perceived an environmental exposure they reported more symptoms, even if the exposure was not actually present. Physiologically, exposure to CO2 had direct effects on heart rate when controlling for the different physical environments participants were in. A green building must be both high performing and give the perception of high performance in order to address both these pathways and be a healthy building.
Highlights.
Participants in green buildings experience better indoor air quality and improved environmental perceptions
Participants in green buildings report fewer symptoms than those in conventional buildings
Participants report fewer symptoms in simulated green buildings conditions in controlled lab
A 1000 ppm increase in CO2 is associated with a 1.43 increase in symptoms and a 2.3 bpm increase in heart rate
Acknowledgments
This research was supported by a gift from United Technologies to the Center for Health and the Global Environment at the Harvard T.H. Chan School of Public Health. Dr. Allen’s time was primarily supported by faculty startup funds, Dr. Spengler’s time was primarily funded by his endowed chair, and Mr. MacNaughton’s time was supported by NIEHS environmental epidemiology training grant 5T32ES007069-35. United Technologies Research Center provided limited input during the study design phase (support for adding an additional Green+ day and a third CO2 test condition). United Technologies was not involved in the data collection, data analysis, data interpretation, data presentation, or drafting of the manuscript. We thank the study participants for volunteering, the Netatmo and Basis teams for their device support, and Building & Environment for their review of this manuscript.
Footnotes
Publisher's Disclaimer: This is a PDF file of an unedited manuscript that has been accepted for publication. As a service to our customers we are providing this early version of the manuscript. The manuscript will undergo copyediting, typesetting, and review of the resulting proof before it is published in its final citable form. Please note that during the production process errors may be discovered which could affect the content, and all legal disclaimers that apply to the journal pertain.
References
- 1.Gerber D. Baubiologie in Theorie und Praxis. Heimatshutz Patrimoine. 2000;95(3) [Google Scholar]
- 2.Persily A. Challenges in developing ventilation and indoor air quality standards: The story of ASHRAE Standard 62. Building and Environment. 2015;(91):61–67. doi: 10.1016/j.buildenv.2015.02.026. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Riesenberg DE, Arehart-Treichel J. “Sick building” syndrome plagues workers, dwellers. JAMA. 1986;255(22):3063–3063. [PubMed] [Google Scholar]
- 4.Redlich CA, Sparer J, Cullen MR. Sick-building syndrome. The Lancet. 1997;349(9057):1013–1016. doi: 10.1016/S0140-6736(96)07220-0. [DOI] [PubMed] [Google Scholar]
- 5.Fisk WJ, Rosenfeld AH. Estimates of Improved Productivity and Health from Better Indoor Environments. Indoor Air. 1997;7(3):158–172. [Google Scholar]
- 6.MacNaughton P, et al. Economic, Environmental and Health Implications of Enhanced Ventilation in Office Buildings. International Journal of Environmental Research and Public Health. 2015;12 doi: 10.3390/ijerph121114709. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Wargocki P, et al. The effects of outdoor air supply rate in an office on perceived air quality, Sick Building Syndrome (SBS) symptoms and productivity. Indoor Air-International Journal Of Indoor Air Quality And Climate. 2000;10(4):222–236. doi: 10.1034/j.1600-0668.2000.010004222.x. [DOI] [PubMed] [Google Scholar]
- 8.EPA. Building Assessment Survey and Evaluation. 1998 [cited 2015 1/22]; Available from: http://www.epa.gov/iaq/base/study_overview.html.
- 9.USGBC; U.S.G.B. Council, editor. LEED 2009 for New Construction and Major Renovations. Washington, D.C: 2009. [Google Scholar]
- 10.Allen J, et al. Green Buildings and Health. Current Environmental Health Reports. 2015;2(3):250–258. doi: 10.1007/s40572-015-0063-y. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Colton M, et al. Indoor Air Quality in Green Vs Conventional Multifamily Low-Income Housing. Environmental Science & Technology. 2014;48(14):7833–7833. doi: 10.1021/es501489u. [DOI] [PubMed] [Google Scholar]
- 12.Jacobs DE, et al. Moving Into Green Healthy Housing. Journal of Public Health Management and Practice. 2014:1. doi: 10.1097/PHH.0000000000000047. [DOI] [PubMed] [Google Scholar]
- 13.Noris F, et al. Indoor environmental quality benefits of apartment energy retrofits. Building and Environment. 2013;68:170–178. [Google Scholar]
- 14.Singh A, et al. Effects of green buildings on employee health and productivity. American journal of public health. 2010;100(9):1665. doi: 10.2105/AJPH.2009.180687. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.NRC; N.R. Council, editor. Green schools attributes for health and learning. Washington, DC: 2007. [Google Scholar]
- 16.Huizenga C, et al. Measuring indoor environmental quality: a web-based occupant satisfaction survey. 2003 [Google Scholar]
- 17.Corsi R, Sanders TVM, Kinney K. The Texas Elementary School Indoor Air Study. Indoor Air. 2002;1 [Google Scholar]
- 18.Allen J, et al. Associations of Cognitive Function Scores with Carbon Dioxide, Ventilation, and Volatile Organic Compound Exposures in Office Workers: A Controlled Exposure Study of Green and Conventional Office Environments. Environmental Health Perspectives. 2015;123(10) doi: 10.1289/ehp.1510037. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.Colton, et al. Health Benefits of Green Public Housing: Associations With Asthma Morbidity and Building-Related Symptoms. 2015 doi: 10.2105/AJPH.2015.302793. (1541-0048 (Electronic)) [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20.Fanger PO. Indoor air quality in the 21st century: search for excellence. 2000 doi: 10.1034/j.1600-0668.2000.010002068.x. (0905-6947 (Print)) [DOI] [PubMed] [Google Scholar]
- 21.Choobineh A, et al. The impact of ergonomics intervention on psychosocial factors and musculoskeletal symptoms among office workers. International Journal of Industrial Ergonomics. 2011;41(6):671–676. [Google Scholar]
- 22.Fostervold KI, Nersveen J. Proportions of direct and indirect indoor lighting - The effect on health, well-being and cognitive performance of office workers. Lighting Research & Technology. 2008;40(3):175–200. [Google Scholar]
- 23.Ulrich RS. View through a Window May Influence Recovery from Surgery. Science. 1984;224(4647):420–421. doi: 10.1126/science.6143402. [DOI] [PubMed] [Google Scholar]
- 24.Mendell MJ. Non-Specific Symptoms In Office Workers: A Review And Summary Of The Epidemiologic Literature. Indoor Air. 1993;3(4):227–236. [Google Scholar]
- 25.Erdmann C, Steiner K, Apte M. Indoor carbon dioxide concentrations and sick building syndrome in the base study revisited: analyses of the 100 building dataset. Indoor Air Proceedings. 2002 [Google Scholar]
- 26.Vehvilainen T, et al. High indoor CO concentrations in an Office Environment Increases the Transcutaneous CO Level and Sleepiness during Cognitive Work. 2015 doi: 10.1080/15459624.2015.1076160. (1545-9632 (Electronic)) [DOI] [PubMed] [Google Scholar]
- 27.Kajtar L, Herczeg L. Influence of carbon-dioxide concentration on human wellbeing and intensity of mental work. Idojaras. 2012;116(2):145–169. [Google Scholar]
- 28.Reichgott M. Clinical Methods: The History, Physical, and Laboratory Examinations. 3. Vol. 76. Boston: Butterworths; 1990. Clinical Evidence of Dysautonomia. [Google Scholar]
- 29.Starcke K, Brand M. Decision making under stress: A selective review. Neuroscience & Biobehavioral Reviews. 2012;36(4):1228–1248. doi: 10.1016/j.neubiorev.2012.02.003. [DOI] [PubMed] [Google Scholar]
- 30.Satish U, et al. Is CO2 an indoor pollutant? Direct effects of Low-to-moderate CO2 concentrations on human decision-making performance. Environmental Health Perspectives. 2012;120(12):1671. doi: 10.1289/ehp.1104789. [DOI] [PMC free article] [PubMed] [Google Scholar]