Abstract
Objective
Peer support can be defined as the process of giving and receiving nonprofessional, nonclinical assistance from individuals with similar conditions or circumstances to achieve long-term recovery from psychiatric, alcohol, and/or other drug-related problems. Recently, there has been a dramatic rise in the adoption of alternative forms of peer support services to assist recovery from substance use disorders; however, often peer support has not been separated out as a formalized intervention component and rigorously empirically tested, making it difficult to determine its effects. This article reports the results of a literature review that was undertaken to assess the effects of peer support groups, one aspect of peer support services, in the treatment of addiction.
Methods
The authors of this article searched electronic databases of relevant peer-reviewed research literature including PubMed and MedLINE.
Results
Ten studies met our minimum inclusion criteria, including randomized controlled trials or pre-/post-data studies, adult participants, inclusion of group format, substance use-related, and US-conducted studies published in 1999 or later. Studies demonstrated associated benefits in the following areas: 1) substance use, 2) treatment engagement, 3) human immunodeficiency virus/hepatitis C virus risk behaviors, and 4) secondary substance-related behaviors such as craving and self-efficacy. Limitations were noted on the relative lack of rigorously tested empirical studies within the literature and inability to disentangle the effects of the group treatment that is often included as a component of other services.
Conclusion
Peer support groups included in addiction treatment shows much promise; however, the limited data relevant to this topic diminish the ability to draw definitive conclusions. More rigorous research is needed in this area to further expand on this important line of research.
Keywords: behavioral treatment, mentorship, substance use, alcohol, drugs, recovery
Introduction
Peer support can be defined as the process of giving and receiving nonprofessional, nonclinical assistance from individuals with similar conditions or circumstances to achieve long-term recovery from psychiatric, alcohol, and/or other drug-related problems. Historically, peer support has been shown to be a key component of many existing addiction treatment and recovery approaches such as the community reinforcement approach,1–11 therapeutic communities,12,13 and 12-step programs;14,15 the community reinforcement approach has demonstrated the importance of valued social roles in maintaining abstinence, which is the foundation of the peer support relationship.16–18
Varying approaches that include a mixture of services such as peer support groups, individual counseling, and case management have emerged as a highly effective and empowering method to manage the social context of health issues and are particularly popular in the substance abuse and mental health fields.19 As it relates to substance abuse recovery for individuals and families, addiction peer support services have emerged across time due to the shift from a biopsychosocial approach to a sustained recovery management approach to treat addictions.20 While in many cases, peer support groups do not replace the need for formal treatments or supervisory clinical guidance due to peers not having sufficient training to manage psychiatric conditions or high-risk situations, they still offer an augmentation to treatment that provides many benefits to individuals with substance use disorders.21
Terminology
Various terminologies are used interchangeably within the literature to describe peer-related support and contexts. For the purposes of this article, we attempted to utilize consistent language wherever possible. However, in certain instances, a term may be part of a broader term such as mentorship is a type of peer support, but mentorship is specific to an individual in later recovery providing peer support to someone in earlier recovery, which requires additional specification.21 We adapted and built upon White’s20 definition of peer support to include individuals with similar conditions or circumstances and inclusion of recovery from psychiatric problems in addition to substance use disorders. We also included this broadened scope in our definition of peer mentorship. Table 1 provides key peer support terms used throughout this review article and definitions.22–24
Table 1.
Key terms and definitions related to peer support
| Terms | Definitions |
|---|---|
| Peer support | The process of giving and receiving nonprofessional, nonclinical assistance from individuals with similar conditions or circumstances to achieve long-term recovery from psychiatric, alcohol, and/or other drug-related problems |
| Recovery | A process of change through which individuals improve their health and wellness, live self-directed lives, and strive to reach their full potential22 |
| Peer support group | Where people in recovery voluntarily gather together to receive support and provide support by sharing knowledge, experiences, coping strategies, and offering understanding23 |
| Peer provider (eg, certified peer specialist, peer support specialist, mentor, and recovery coach) | A person who uses his or her lived experience of recovery from mental illness and/or addiction, plus skills learned in formal training, to deliver services in behavioral health settings to promote mind–body recovery and resiliency24 |
| Peer mentorship | Where individuals in later recovery provide nonprofessional, nonclinical assistance to individuals in earlier recovery with similar conditions or circumstances to achieve long-term recovery from psychiatric, alcohol, and/or other drug-related problems |
Residential and sober living
Since the 1960s, a variety of residential options have emerged to help people with alcohol and drug addictions. These programs based on the social model of recovery provide support for people in recovery from alcohol addiction in a residential environment that focuses on Alcoholics Anonymous (AA) philosophy and practices.25 AA practice follows the 12-step guidelines based on spiritual principles and the assumption that addiction is a disease.26 Prior work utilizing social model programs can be found as early as the 1940s.27–29 The types of social model programs available include social setting detoxification, residential social model recovery programs, neighborhood recovery centers, and sober living houses.27
Sober living houses are alcohol- and drug-free living environments for a group of peers in recovery. Utilizing a peer-oriented social model modality, sober living houses rely on mutual sobriety support, self-efficacy, and resident participation. California Sober Living Houses and Oxford Houses are two variations of sober living houses.30–32 Previous studies have shown sober living houses to be beneficial33 and effective34,35 in assisting in the reduction of substance use. For example, Jason et al35 conducted a randomized study to test the efficacy of an Oxford House intervention compared to usual care (ie, outpatient treatment or self-help groups) following discharge from inpatient substance abuse treatment. Results demonstrated a significant increase in monthly income with a significant decrease in substance use and incarceration rates among those in the Oxford House condition compared with the usual-care condition.
12-step
Some of the most popular peer support groups held outside the formal treatment settings for addiction nationwide include 12-step programs such as AA, Narcotics Anonymous, and Cocaine Anonymous. Twelve-step is an intervention for drug abuse and addiction and can include dual recovery from substance abuse problems and co-occurring mental health disorders. Humphreys36 found 12-step groups to be the most referred adjunct support for professionally treated substance abuse patients. Other studies have demonstrated the effectiveness of 12-step groups for the treatment of substance abuse following treatment,37–39 and prior research of 12-step groups has shown reductions in alcohol and drug use.40–42
AA has been shown to be a highly utilized intervention for individuals with alcohol problems.43–45 Positive outcomes such as self-efficacy and healthy coping have been associated with AA affiliation, which has been linked to better outcomes.37,46 For those with drinking problems seen in treatment, certain AA activities such as having a sponsor and doing service might be key components of abstinence.47
In a focused review of the literature on AA effectiveness, six criteria were required for establishing causation: 1) magnitude of effect; 2) dose–response effect; 3) consistent effect; 4) temporally accurate effects; 5) specific effects, and 6) plausibility. The evidence for all criteria except specific effects was very strong. For magnitude, rates of abstinence within AA were approximately twice as high. For dose–response, higher rates of abstinence were related to higher levels of attendance. For consistency, the effects were found for different follow-up periods and different samples. For temporal, prior AA attendance is predictive of subsequent abstinence. For plausibility, mechanisms of action predicted by behavioral change theories were present in AA. However, for specificity of an effect for 12-step facilitation or AA, experimental evidence was mixed, with evidence for both positive and negative effects in addition to no effect.48
Although the peer support groups within 12-step approaches have provided benefits to select populations, some individuals with substance use disorders find the religious nature of 12-step approaches and often lack of integration in the treatment setting to be a deterrent.49–51 Alternatives to 12-step approaches are needed to more closely integrate peer support services within treatment and to provide more options to benefit from peer support groups.
Treatment and community settings
Recently, there has been a dramatic rise in the adoption of alternative forms of peer support services within treatment and community settings to assist recovery from substance use disorders, because of the potential benefits offered to patients.52 However, often peer support has not been separated out as a formalized intervention component and rigorously empirically tested, making it difficult to determine its effects.53
Peer support is delivered in a variety of modalities, including, but not limited to, in-person self-help groups, Internet support groups, peer run or operated services, peer partnerships, peers in health care settings who serve as peer advocates, peer specialists, and peer case managers.54 Among peer support services available today, peer support groups are considered an important aspect of the addiction recovery process.55–58
Previous studies have shown positive outcomes from participating in peer support groups. Active engagement in peer support groups has shown to be a key predictor of recovery,56,59,60 and sustaining recovery.61–63 In addition, evidence demonstrates that one’s belief in their own ability can increase and influence one’s behavior by watching other peoples’ behaviors (ie, performing activities).64 There is a mutual benefit between the members and facilitators of peer support groups. Oftentimes, peer support groups are facilitated by peer workers who themselves are in recovery and benefit positively from peer support groups.21 Benefits for the peer worker include increased self-esteem, confidence, positive feelings of accomplishment, and an increase in their own ability to cope with their challenges.
Existing systematic peer support reviews
Bassuk et al65 conducted a systematic review of the evidence on the effectiveness of peer support services for people in recovery from alcohol and drug addiction, which resulted in nine studies meeting the criteria for inclusion in the review. Despite methodological limitations found in the studies, the body of evidence suggested beneficial effects on participants. In another systematic review, Reif et al66 evaluated peer support services for individuals with substance use disorders resulting in ten studies. The studies demonstrated increased treatment retention, improved relationships with treatment providers and social supports, increased satisfaction, and reduced relapse rates. Similar to the other reviews, there were methodological limitations that included inability to distinguish the effects of peer recovery support from other recovery support activities, small sample sizes and heterogeneous populations, unclear or inconsistent outcomes, and lack of any or appropriate comparison groups. Both of these reviews included peer support services in general without a specific focus on peer support groups and excluded studies with substance-using populations with a primary focus on human immunodeficiency virus (HIV)/hepatitis C virus (HCV) risk behavior outcomes. In addition, 12-step peer support studies were excluded.
This article reports the results of a literature review that was undertaken to assess the use of peer support groups, one aspect of peer recovery support services, in the treatment of addiction. In reporting the outcomes related to this review, the authors intend to: 1) encourage the field to generate further research to more rigorously investigate the effectiveness of peer support groups and explore the multitude of other specific types of peer recovery support services and 2) provide greater awareness to the advantages of peer support integration within the substance use treatment continuum for adults with addiction problems.
Methods
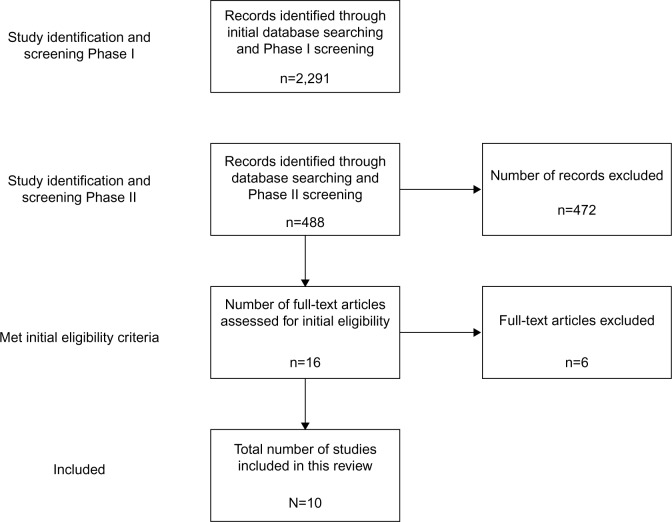
To effectively complete the review, the authors used a combination of searches on electronic scientific databases and screening results cross-checking the eligibility criteria to reduce the number of studies included in this article. At certain points, the authors independently cross-checked the results. If there was a discrepancy, further information was gathered to make an accurate determination of how to proceed. The process is described later and summarized in Figure 1.
Figure 1.
Flow diagram of study selection.
Study identification and screening: Phase I
The authors of this article searched the electronic databases of relevant peer-reviewed research literature including PubMed and MedLINE. Because addiction is a broad term that can be applied to varying types of addiction beyond alcohol- and nonalcohol-related substances (eg, gambling, Internet, sex, and eating) that are unrelated to the scope of this article, “substance use disorders” was the primary terminology used in searches to yield records pertaining to alcohol and drug problems. The initial database search used keywords “substance use disorders and peer support”. We also cross-checked our inclusion list by running similar searches containing specific substance names as keywords (eg, cocaine, alcohol, and heroin) to ensure comprehensiveness. This resulted in 2,291 records.
Study identification and screening: Phase II
The following keywords were used to identify all articles associated with several domains: substance use disorders, peer support or peer mentorship, and intervention. Including the keyword “intervention” allowed for higher yielding of treatment studies. While critiquing and critically reviewing results within an article that included a systematic review of studies,66 we found three additional studies that met our inclusion criteria, which were included.67–69 Using the keywords “substance use disorders and peer support and intervention”, 461 records were found. Using the keyword “substance use disorder and peer mentorship”, 24 records were found. Including three studies previously mentioned, a total of 488 articles were screened for eligibility.
Initial eligibility
By design, this discussion is limited to studies that included a peer support group component that: 1) had adult participants; 2) focused on addiction-related substance use (ie, alcohol, tobacco, legal/illicit drugs, and prescription drugs); 3) held in any group format; 4) included randomized controlled trials (RCTs) or studies with pre- and post-data results, and 5) US-conducted studies published in 1999 or later. Since certain groups (eg, HIV, HCV, and mental health) are at greater risk of having a substance use disorder, we did not exclude these populations.
As previously noted, the authors used keywords peer support or mentorship and substance use disorders to generate articles on the use of peer support groups within substance use disorder treatment to generate the initial pool of articles. We further narrowed our initial results in the current article to include only studies that focused on peer support group treatments. However, initially, we found that empirical studies assessing peer support groups solely were very limited and that our literature search would be much improved if we included not only peer support groups independently but also studies that integrated peer support groups as a component of a larger spectrum of peer services offered. We also included traditional forms of peer support services such as 12-step in addition to including any recent advancements within the field.
All study types that were not RCTs or quasi-experiments were excluded, including case reports, case series, cross-sectional surveys, and other qualitative studies. Adolescents-focused studies were excluded, because they focused generally on social support and social norms and peers may not have self-identified as having substance use problems. Cost-effectiveness studies were excluded. Article types such as books, editorials, guidelines, commentaries, dissertations, discussions, policy analyses, and newspaper or magazine articles were excluded. Of the 488 records that underwent review to meet the authors’ inclusion/exclusion criteria noted earlier, 16 articles met the initial eligibility.
Final selection
Of the 16 records, ten articles were selected to be included in the article. Of the six excluded, three studies had a primary focus of peer support groups to train the peer support staff, two studies did not have consistent or adequately structured peer support groups in the design, and one study’s substance use inclusion criteria were too minimal.
Results
The literature search revealed articles that support the use of peer support services that include peer support groups within addiction treatment to address: 1) substance use, 2) treatment engagement, 3) HIV/HCV risk behaviors, and 4) secondary substance-related behaviors. It should be noted, however, that data were limited in finding peer support groups that were a standalone treatment as these groups were largely incorporated into a full array of peer support services being delivered, thereby posing challenges in disentangling the effects. Table 2 provides summaries of each study selected.
Table 2.
Included studies utilizing peer support groups
| Authors | Design | N | Population | Findings |
|---|---|---|---|---|
| Armitage et al67 | Pre/posttest | 152 | Individuals in recovery from addiction and their families | 86% of participants indicated no use of alcohol or drugs in the past 30 days at the 6-month follow-up 95% of participants reported strong willingness to recommend the program to others, 89% found services helpful, and 92% found materials helpful |
| Boisvert et al70 | Pre-/posttest | 18 | Individuals in addiction recovery living in permanent supportive housing | Substance use relapse rate reduced (24%–7%) for participants in the peer support community Pretest relapse rate was 85%; posttest rate was 33% for tenants returning to homelessness No differences in pre- and post-QOLR The MOS–SSS subscales revealed significant differences and moderate-to-large effect sizes (r) on the MOS–SSS subscales: emotional/informational support (P=0.005; r=0.628), tangible support (P=0.028; r=0.493), and affectionate support (P=0.027; r=0.494) |
| Tracy et al21 | Pre-/posttest | 40 | Individuals with substance use disorders in an addiction treatment program | Feasibility and acceptance data in the domains of patient interest, safety, and satisfaction were promising In addition, mentees significantly reduced their alcohol use (P<0.01) and drug use (P<0.01) from baseline to termination The majority of mentors sustained abstinence Fidelity measures indicated that mentors adhered to the delivery of treatment |
| Tracy et al72 | RCT comparing TAU + MAP-engage vs TAU + DRT + MAP-engage vs TAU | 96 | High recidivism veterans (mostly males) with substance use disorders initially recruited from an inpatient clinic | TAU + MAP-engage alone and TAU + DRT + MAP-engage were associated with increased adherence to post-discharge outpatient appointments for substance use treatment (P<0.05) when compared with TAU only As well as for substance use treatment, general medical, and mental health services (P<0.05 for all appointments combined) when compared with TAU only |
| Mangrum68 | Quasi-experimental design comparing ATR and substance use treatment vs substance use treatment | 4,420 | Consumers with substance use disorders referred from drug courts, probation, or child protective services | Individuals who completed the program were significantly more likely to have received recovery support groups (t(1)=65.75, P<0.0001) |
| Purcell et al73 | RCT study of peer-mentoring intervention INSPIRE vs a video discussion control group | 966 | HIV-positive IDU participants | Adherence rates measured at 87%, 83%, and 85% at 3 months, 6 months, and 12 months, respectively Risk behaviors decreased among randomized participants although no significant differences in conditions |
| Latka et al74 | RCT study of peer-mentoring intervention vs a time-equivalent attention-control group | 418 | Individuals who are HCV-positive and IDUs | Compared with the controls, participants in the intervention group were less likely to report distributive risk behaviors at 3 months (OR =0.46; 95% CI =0.27, 0.79) and 6 months (OR =0.51; 95% CI =0.31, 0.83), a 26% relative risk reduction Peer mentoring and self-efficacy were significantly increased in the intervention group, and intervention effects were mediated through improved self-efficacy |
| Velasquez et al71 | RCT study of both individual counseling vs peer group education/support | 253 | HIV-positive men who have sex with men with alcohol use disorders | Treatment effect was demonstrated over each 30-day period with regard to number of drinks consumed (OR =1.38; 95% CI =1.02, 1.86) As well as the number of heavy drinking days (OR =1.5; 95% CI =1.08, 2.10) over each 30-day period Main effect was found in the number of days in which both heavy drinking and unprotected sex occurred over each 30-day period |
| Marlow et al79 | Pre-/posttest | 13 | Formerly incarcerated men on parole released from prison within the past 30 days | Findings from the assessment of psychosocial variables demonstrated significant improvement on two abstinence self-efficacy subscales, negative affect (P=0.01), and habitual craving (P=0.003) No significant differences in total scores for abstinence self-efficacy or the other measures from baseline to follow-up for the 13 participants who completed the study No significant differences in 12-step participation with regard to attendance, sponsor contact, or belief in 12-step framework |
| Andreas et al69 | Pre-/posttest | 509 | Men and women in recovery from addiction who had been incarcerated, and their families and significant others | Increased self-efficacy and increased family and friend support, quality of life, and feelings of guilt and shame were demonstrated at 12 months from baseline (no data were shown) Peer and staff accessibility were valued |
Abbreviations: ATR, access to recovery; CI, confidence interval; DRT, dual recovery treatment; HCV, hepatitis C virus; HIV, human immunodeficiency virus; IDU, injection drug user; INSPIRE, Intervention for Seropositive Injectors–Research and Evaluation; MAP, Mentorship for Alcohol Problem; MAP-engage, Mentorship for Addiction Problems to enhance engagement to treatment; MOS, Medical Outcomes Study; OR, odds ratio; QOLR, Quality of Life Rating; RCT, randomized controlled trial; SSS, Social Support Survey; TAU, treatment as usual.
Substance use
Armitage et al67 discussed and evaluated Recovery Association Project’s (RAP) Recovery Community Services Program, a funded peer recovery service from 2003 to 2007. Recovery Community Services Program provided a wide range of peer recovery services, which included numerous self-help meetings at the RAP center that became a popular location for self-help meetings (eg, AA, Narcotics Anonymous, Cocaine Anonymous, and Smart Recovery) with several scheduled meetings daily. The outcomes measured were substance use, consumer satisfaction, and progress toward RAP’s goals. RAP received participant feedback from the Government Performance Reporting Act survey and a satisfaction questionnaire. There were 152 survey participants included in this outcome evaluation. At 6-month follow-up, most (86%) participants receiving RAP services indicated on the Government Performance Reporting Act survey abstinence from using alcohol or drugs in the past 30 days, which is much higher than typically noted abstinence levels in this population. These results help to demonstrate that RAP services are associated with sustained recovery from substance use. Data from the satisfaction questions administered at 6 months were also high, indicating RAP’s services are effectively meeting the needs of participants.
Boisvert et al70 established and evaluated the effectiveness of a peer support community program. The primary purpose was to determine whether rates of relapse would decrease among addicts in recovery living in permanent supportive housing and increase their perceptions of community affiliation, supportive behaviors, self-determination (ie, proactive steps self-initiated to recovery), and quality of life. The peer support program was implemented by an occupational therapist and addiction professional following SAMHSA (Substance Abuse and Mental Health Services Administration) recovery community model. The staff person facilitated the first 10 weeks and then withdrew to a supportive background as the community became self-facilitating. Meetings involved discussions on principles of a peer support recovery or peer-driven community between the therapist and residents. Documents such as handouts and readings were provided to the community members who had interest in being a leader within the community, and supportive meetings were scheduled. The peer support group focused on training in leadership, group communication, and group facilitation with community-elected officers and conducted biweekly meetings and social events, all being organized by members.
Using previous year relapse data to provide a comparison rate, Boisvert et al70 found significant reductions in relapse rates among participants in the peer support community programs. In addition, return to homelessness was dramatically reduced by assisting participants in managing their recovery. These results imply that peer and community support groups are important in the process of relapse reduction, in particular, groups that focus on self-determination, as it can have a positive impact on recovery from substance abuse and homelessness. As for the main objectives, quantitative findings showed that three subscales (ie, emotional support, tangible support, and affectionate support) on the Medical Outcomes Study–Social Support Survey demonstrated significant differences, although there were no significant differences regarding quality of life from the Quality of Life Rating.70 In addition, qualitative findings showed that residents’ perceptions of community affiliation and supportive behaviors improved.
Another study conducted by Tracy et al21 investigated a new intervention, mentorship for alcohol problems (MAPs), that included peer support groups and one-to-one mentorship services for individuals with alcohol-use disorders in community-treatment programs. Mentors participated for 6 months until multiple mentees received MAP for 12 weeks. Behavioral and biological measures were conducted in addition to fidelity measures. Feasibility and acceptance data in the domains of patient interest, safety, and satisfaction were promising. In addition, mentees significantly reduced their alcohol and drug use from baseline to termination and the majority of mentors sustained abstinence. Fidelity measures indicated that mentors adhered to the delivery of treatment.
Velasquez et al71 evaluated the efficacy of a theory-based behavioral intervention that included both individual counseling and peer group education/support to reduce alcohol use among HIV-positive men who have sex with men when compared to a control condition where participants received resource materials. Reported treatment effects occurred in reduction in the number of drinks per 30-day period and number of days drank heavily per 30-day period.
Engagement to treatment
Beyond associated reductions in alcohol and drug use, services that have included peer support groups have been utilized to engage substance-using populations in treatment. Often high recidivism substance-using patients have difficulty connecting to outpatient treatment, contributing to greater functioning disturbances.72 Approaches to address this problem frequently are staff extensive. Tracy et al72 evaluated the impact of peer mentorship, which included, in addition to other peer support services, peer support groups and/or enhanced dual recovery treatment (DRT) on individuals who were inpatients, substance abusing, and had a history of high recidivism. The primary outcome was post-discharge treatment attendance. Within an inpatient Veterans Administration hospital setting, 96 patients with a history of high recidivism and current and/or past diagnosis of substance use disorders were randomized to either: 1) treatment as usual (TAU), 2) TAU + DRT + mentorship for addiction problems to enhance engagement to treatment (MAP-engage), or 3) TAU + MAP-engage. The investigators found that overall MAP-engage was comparable to the DRT + MAP-engage, and both of these conditions were significantly better than TAU alone at increasing adherence to post-discharge substance abuse, and medical and mental health outpatient appointments with participants in MAP-engage being three times as likely to attend their outpatient substance abuse treatment appointments than those in TAU 1 year post discharge. MAP-engage that included peer support groups offered an alternative approach to address lack of attendance to outpatient treatment appointments post discharge that is relatively low in staff reliance.
Similarly, in a large study, Mangrum68 compared access to recovery + substance use treatment to substance use treatment alone for consumers involved in the criminal justice system who had substance use disorders and were referred from drug courts, probation, or child protective services. Individuals who completed the program were significantly more likely to have received recovery support groups. However, it should be noted that only a relatively small portion of the sample within the completers group, 12%, utilized the support groups as there were multiple treatment options, but this was still over twice as much as in the non-completers group, 5%.
HIV/HCV risk behavior
Intervention for Seropositive Injectors–Research and Evaluation study, an RCT of a peer support intervention designed to assess the reduction in sexual and injecting-related risk behaviors, increased use of HIV care, and increased HIV medication adherence as primary outcomes, was discussed by Purcell et al.73 The peer support intervention was ten sessions over a 12-month time period, with seven sessions being specifically devoted to peer support groups. The control condition was eight sessions of a video intervention. One out of the ten sessions was a peer volunteer activity during which participants went to a local service organization for 2–4 hours to observe, participate, and practice peer support skills. The topics from the group sessions included setting group rules and the power of peer mentoring, utilization of HIV primary care and adherence, and sex and drug risk behaviors.
Of the participants randomized, 486 were assigned to the peer support condition and 480 were assigned to the video discussion condition, totaling a sample of 966 HIV injection drug users (IDUs). Purcell et al73 found that randomized participants in both conditions had retention rates of 87%, 83%, and 85% at 3 months, 6 months, and 12 months, respectively. Significant reductions were noted in both groups for reductions from baseline in injection and sexual transmission risk behaviors, but there were no significant differences between conditions. Participants in both conditions reported no change in medical care and adherence.73
An RCT with a time-equivalent attention-control group was conducted by Latka et al74 among 418 HCV IDUs to examine a peer-mentoring behavioral intervention to reduce the distribution of injection practices and equipment among HCV IDUs. Each intervention consisted of six sessions, 2 hours each twice a week. For the peer-mentoring group intervention, participants received information regarding HCV and learned risk reduction skills. By the fifth session, training participants were involved in outreach and delivered information about reducing HCV transmission risk. The control group watched a docudrama TV series about IDUs and participated in a facilitated group discussion focusing on family, education, self-respect, relationships, violence, parenting, and employment. Compared to the control group, participants in the peer support condition had significantly greater reductions in injection practices that could transmit HCV to other IDUs. Self-efficacy was significantly increased in the experimental condition, and post-intervention self-efficacy was a positive mediator between the intervention and distributive risk behaviors.
In the study previously discussed in the substance use section, Velasquez et al71 also found a reduction in the number of days on which both heavy drinking and unprotected sex occurred among HIV-positive men who have sex with men.
Secondary substance-related outcomes
Craving has been associated with use of substances.75–78 The authors’ search also revealed a recently published pilot study that evaluated a peer support program for formerly incarcerated adults who transitioned back into the community that included investigations of craving among other varriables.79 This population experiences high rates of substance use. One of the main objectives of this study was to assess program feasibility using a community-based participatory research approach. Participants were 20 men on parole who were released from prison within the past 30 days, with only 13 completing the 60-day peer mentor intervention. Marlow et al78 measured 12-step meeting participation using a 13-item questionnaire that assessed participation in 12-step programs, belief in the 12-step framework, and investigated relationships with craving and negative affect. Questions assessing belief in 12-step framework included: I am powerless over my drug and alcohol problem, I believe a higher power plays a role in my recovery, I am not alone with my drug and alcohol problem, I believe in the 12-step faith and spirituality, and I am member of 12-step. Twelve-step meetings were attended by participants on an average of 17 days out of 30 days and participants contacted their sponsor on average ten times. All participants’ belief in the 12-step framework was high. Pre- and posttest results on two abstinence subscales, negative affect and habitual craving, showed significant improvement, indicating an improved confidence level in the ability to abstain from substance use.
Andreas et al69 sought to examine Peers Reach Out Supporting Peers to Embrace Recovery (PROSPER), a peer-driven recovery community that provides a number of peer-driven supports for members to be able to recover from drug use and criminality as they transition back into the community and to provide support to their family members and loved ones. PROSPER provided a strategic mix of services, all planned, implemented, and delivered by peers including peer-run groups and group activities that take place in a light-hearted social environment away from traditional treatment settings. The aims of the program were to: 1) provide peer support environment, 2) build positive self-concept and achievement motivation, 3) reinforce family/significant others’ relationships and support, and 4) amplify the treatment continuum.77 The study outcome measures were self-efficacy, perceived social support, personal feeling, perceived stress, and quality of life. Program effects were evaluated and demonstrated at 12 months from baseline with significant and positive changes in participants’ self-efficacy, social support perceptions, quality of life, and feelings of guilt and shame over a 12-month period. The result of this study suggests the importance of peer support among people who are reentering the community, which can promote positive outcomes such as reduced substance use and recidivism.
Discussion
Despite the recent surge in the adoption of peer support services within addiction treatment systems, there are relatively limited data rigorously evaluating outcomes.21 These data become even more limited when considering one form of peer support services, such as peer support groups as in the case of this review, due to the nature of peer support services being delivered often in a multitude of combined modalities. Thus, we included studies of peer support groups that were delivered often in an array of other peer support treatments, which diminished our ability to disentangle the results. However, this review still provides a useful platform to begin to explore the inclusion of these peer support groups as a component of other peer services and associated benefits thus far to guide the field in the future researching of this area.
Although methodological limitations existed in studies that resulted from previous existing systematic reviews of peer support services, beneficial effects were noted.65,66 This article builds upon these reviews by the specificity on peer support groups, which is a common platform in treatment. To the authors’ knowledge, this is the first article to date to take such an approach reviewing controlled studies. The previous reviews examined a range of peer support services. Moreover, we expanded beyond existing reviews to include substance-related HIV/HCV risk behavior studies due to the high prevalence of substance use disorders in this population. Drug abuse is inextricably linked with HIV due to heightened risk both of contracting HIV and of worsening its consequences, and HCV is one of the most common viral hepatitis infections transmitted through drug-using high-risk behaviors, making reduction of risk behaviors one of the priorities in substance abuse treatment at the National Institute on Drug Abuse.80 Finally, we also expanded our review to include 12-step studies due to their focus on peer support groups and contributions to the peer support movement.
Our review revealed articles that demonstrated peer support services that include groups delivered to those with substance use problems showing associated benefits in the following areas: 1) substance use, 2) treatment engagement, 3) HIV/HCV risk behaviors, and 4) secondary substance-related behaviors such as craving and self-efficacy.
Those who participated in treatments, including peer support groups, showed higher rates of abstinence than common in substance-abusing populations while also being more satisfied with the treatment.67 Furthermore, significant reductions in relapse rates were shown in addition to significant reductions in return to homelessness in a challenging population to treat.70 Reported benefits extended beyond those being the recipient of the peer support groups to those also delivering the services, where significant reductions in alcohol and drug use were shown not only for mentees but also for sustained abstinence in the majority of mentors.21
Beyond substance use, peer support groups offer unique advantages to engaging our historically difficult-to-engage populations. Services that included peer support groups were found to be equally comparable to the additive of extensive DRT, and both were significantly better than standard treatment at increasing adherence to post-discharge substance abuse and medical and mental health outpatient appointments for high recidivism individuals with substance use disorders.72 Moreover, consumers involved in the criminal justice system who had substance use disorders and were referred from drug courts, probation, or child protective services, who completed the program, were significantly more likely to have received recovery support groups.68 However, it should be noted that only a relatively small sample completed, thus diminishing the impact of these results.
Peer support services that include groups have also been associated with reductions in HIV and HCV risk behaviors in IDUs. One study demonstrated a reduction in injection and sexually transmitted risk behaviors in both conditions, but there was no significant difference between the peer condition and the control condition, which was also an intervention.73 However, another study showed not just a reduction but significantly greater reductions in injection practices that could transmit HCV to other IDUs when comparing the peer support condition to the control group.74 Consistent with previous research, the study suggests that this enhanced behavioral intervention of education and counseling was associated with safer injection practices. Thus, providing implications that these components (ie, skill building and education) of peer mentoring provided to HCV-injecting drug users can lead to safer practices of injection drug use and may contribute to reducing the risk in IDUs and the transmission of HCV to other IDUs. Another study demonstrated significant reductions not only in risk behaviors but also in heavy drinking while accomplishing this.71
One of the key elements that peer support services significantly positively impact is improvement in participants’ self-efficacy, which was also found to be a positive mediator between interventions and distributive risk behaviors in one study.69 Associated positive changes have also been demonstrated such as improvements in negative affect, social support perceptions, reductions in habitual craving, and feelings of guilt or shame.69,79 All of these areas play important roles in one’s ability to achieve and sustain abstinence from substances. There were conflicting results from studies on whether or not quality-of-life improvements were associated with peer support groups being included in services.69,70
Peer support groups included in addiction treatment show much promise in potentially reducing substance use, improving engagement, reducing HIV/HCV risk behaviors, and improving substance-related outcomes. However, even given their widespread use, there are relatively limited empirical data relevant to this topic, which may diminish the ability to draw definitive conclusions, with resulting studies being ten. Although this is similar in number to other reviews in related peer support topics, it is relatively low. We included only US studies due to not having access to other non-English search engines in addition to ruling out language barriers, but this also limits the data. Finally, some investigators note that self-selection into peer support groups and residential recovery homes is important in the process in treatment,33,81 which then may confound outcomes and limit generalizability in RCTs for those select participants who may be solely interested in gains outside of participation such as participant payment. More rigorous research is needed, including meta-analytic studies as more data surface in this area, to substantiate the results of the studies included in this review and further expand on this important line of research.
Acknowledgments
This work was supported by the National Institute on Drug Abuse (R34DA034898) and the New York Harbor Healthcare System.
Footnotes
Disclosure
The authors report no conflicts of interest in this work.
References
- 1.Azrin NH. Improvements in the community-reinforcement approach to alcoholism. Behav Res Ther. 1976;14(5):339–348. doi: 10.1016/0005-7967(76)90021-8. [DOI] [PubMed] [Google Scholar]
- 2.Azrin NH, Sisson RW, Meyers R, Godley M. Alcoholism treatment by disulfiram and community reinforcement therapy. J Behav Ther Exp Psychiatry. 1982;13(2):105–112. doi: 10.1016/0005-7916(82)90050-7. [DOI] [PubMed] [Google Scholar]
- 3.Meyers RJ, Miller WR, editors. A Community Reinforcement Approach to Addiction Treatment. Cambridge: Cambridge University Press; 2001. [Google Scholar]
- 4.Silverman K, Svikis D, Robles E, Stitzer ML, Bigelow GE. A reinforcement-based therapeutic workplace for the treatment of drug abuse: six-month abstinence outcomes. Exp Clin Psychopharmacol. 2001;9(1):14–23. doi: 10.1037/1064-1297.9.1.14. [DOI] [PubMed] [Google Scholar]
- 5.Higgins ST, Wong CJ, Badger GJ, Ogden DE, Dantona RL. Contingent reinforcement increases cocaine abstinence during outpatient treatment and 1 year of follow-up. J Consult Clin Psychol. 2000;68(1):64–72. doi: 10.1037//0022-006x.68.1.64. [DOI] [PubMed] [Google Scholar]
- 6.Miller WR, Meyers RJ, Hiller-Sturmhofel S. The community-reinforcement approach. Alcohol Res Health. 1999;23(2):116–121. [PMC free article] [PubMed] [Google Scholar]
- 7.Stitzer ML, Bickel WK, Bigelow GE, Liebson IA. Effect of methadone dose contingencies on urinalysis test results of polydrug-abusing methadone-maintenance patients. Drug Alcohol Depend. 1986;18(4):341–348. doi: 10.1016/0376-8716(86)90097-9. [DOI] [PubMed] [Google Scholar]
- 8.Smith JE, Meyers RJ, Delaney HD. The community reinforcement approach with homeless alcohol-dependent individuals. J Consult Clin Psychol. 1998;66(3):541–548. doi: 10.1037//0022-006x.66.3.541. [DOI] [PubMed] [Google Scholar]
- 9.Meyers RJ, Miller WR, Smith JE, Tonigan JS. A randomized trial of two methods for engaging treatment-refusing drug users through concerned significant others. J Consult Clin Psychol. 2002;70(5):1182–1185. [PubMed] [Google Scholar]
- 10.Miller WR, Meyers RJ, Tonigan JS. Engaging the unmotivated in treatment for alcohol problems: a comparison of three strategies for intervention through family members. J Consult Clin Psychol. 1999;67(5):688–697. doi: 10.1037//0022-006x.67.5.688. [DOI] [PubMed] [Google Scholar]
- 11.Meyers RJ, Miller WR, Hill DE, Tonigan JS. Community reinforcement and family training (CRAFT): engaging unmotivated drug users in treatment. J Subst Abuse. 1998;10(3):291–308. doi: 10.1016/s0899-3289(99)00003-6. [DOI] [PubMed] [Google Scholar]
- 12.Guida F, De Leon G, Monahan K. Measuring Peer Interaction in the Therapeutic Community. Chicago, IL: American Psychological Association Convention; 2002. [Google Scholar]
- 13.Galanter M, Dermatis H, Egelko S, De Leon G. Homelessness and mental illness in a professional- and peer-led cocaine treatment clinic. Psychiatr Serv. 1998;49(4):533–535. doi: 10.1176/ps.49.4.533. [DOI] [PubMed] [Google Scholar]
- 14.Allen J, Anton RF, Babor TF, Carbonari J. Project MATCH secondary a priori hypotheses. Addiction. 1997;92(12):1671–1698. [PubMed] [Google Scholar]
- 15.Huselid RF, Self EA, Gutierres SE. Predictors of successful completion of a halfway-house program for chemically-dependent women. Am J Drug Alcohol Abuse. 1991;17(1):89–101. doi: 10.3109/00952999108992812. [DOI] [PubMed] [Google Scholar]
- 16.Smith JE, Meyers RJ, Miller WR. The community reinforcement approach to the treatment of substance use disorders. Am J Addict. 2001;10(suppl):s51–s59. doi: 10.1080/10550490150504137. [DOI] [PubMed] [Google Scholar]
- 17.Meyers RJ, Smith JE. Clinical Guide to Alcohol Treatment: The Community Reinforcement Approach. New York City: Guilford Press; 1995. [Google Scholar]
- 18.Hunt GM, Azrin NH. A community-reinforcement approach to alcoholism. Behav Res Ther. 1973;11(1):91–104. doi: 10.1016/0005-7967(73)90072-7. [DOI] [PubMed] [Google Scholar]
- 19.O’Hagan M. Peer Support in Mental Health and Addictions. A Background Paper. Wellington: Kites Trust; 2011. [Google Scholar]
- 20.White WL. Peer-Based Addiction Recovery Support. History, Theory, Practice, and Scientific Evaluation. Chicago, IL: Great Lakes Addiction Technology; 2009. [Google Scholar]
- 21.Tracy K, Burton M, Miescher A, et al. Mentorship for Alcohol Problems (MAP): a peer to peer modular intervention for outpatients. Alcohol Alcohol. 2012;47(1):42–47. doi: 10.1093/alcalc/agr136. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22.SAMHSA [webpage on the Internet] Recovery and Recovery Support. Rockville, MD: Substance Abuse and Mental Health Services Administration; [Accessed February 18, 2016]. [updated October 5, 2015; cited February 18, 2016]. Available from: http://www.samhsa.gov/recovery. [Google Scholar]
- 23.National Alliance on Mental Illness [homepage on the Internet] [Accessed August 2, 2015]. [cited August 2, 2015]. Available from: http://www.nami.org.
- 24.INTEGRATIONSAMHSA [webpage on the Internet] SAMHSA-HRSA Center for Integrated Health Solutions. Rockville, MD: Substance Abuse and Mental Health Services Administration; [Accessed March 5, 2016]. [cited March 5, 2016]. Available from: http://www.integration.samhsa.gov/workforce/team-members/peer-providers; http://www.samhsa.gov/recovery. [Google Scholar]
- 25.White WL. Recovery Monographs: Revolutionizing the Ways That Behavioral Health Leaders Think About People with Substance Use Disorders. Vol. 1. Bloomington: Author House; 2015. [Google Scholar]
- 26.Nowinski J, Baker S, Carroll KM. Twelve Step Facilitation Therapy Manual: A Clinical Research Guide for Therapists Treating Individuals with Alcohol Abuse and Dependence. Vol. 1. Rockville, MD: National Institute on Alcohol Abuse and Alcoholism; 1992. [Google Scholar]
- 27.Borkman TJ, Kaskutas LA, Room J, Bryan K, Barrows D. An historical and developmental analysis of social model programs. J Subst Abuse Treat. 1998;15(1):7–17. doi: 10.1016/s0740-5472(97)00244-4. [DOI] [PubMed] [Google Scholar]
- 28.Hayes B, Blacksher S, Dodd M, Fox T, Lewis K, Wittman FD. The Social Community Model for the Treatment of Alcohol and Other Drug Problems. A Report by the Social Model Consensus Panel Convened by the California. Los Angeles, CA: Department of Alcohol and Drug Programs; 1993. [Google Scholar]
- 29.Riessman F. The “helper” therapy principle. Soc Work. 1965;10(2):27–32. [Google Scholar]
- 30.Polcin DL, Borkman T. The Impact of AA on Non-Professional Substance Abuse Recovery Programs and Sober Living houses. Recent Developments in Alcoholism. New York: Springer; 2008. pp. 91–108. [DOI] [PubMed] [Google Scholar]
- 31.Wittman FD, Biderman F, Hughes L. Sober Living Guidebook for Alcohol and Drug Free Housing. Berkeley CA: University of California; 1993. [Google Scholar]
- 32.Wright A. Los Angeles county’s alcohol-free living centers: long-term, low-cost sober housing. In: Shaw S, Borkman T, editors. Social Model Recovery: An Environmental Approach. Burbank, CA: Bridge Focus Inc; 1990. pp. 119–128. [Google Scholar]
- 33.Polcin DL, Korcha R, Bond J, Galloway G. What did we learn from our study on sober living houses and where do we go from here? J Psychoactive Drugs. 2010;42:425–433. doi: 10.1080/02791072.2010.10400705. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 34.Jason LA, Davis MI, Ferrari JR. The need for substance abuse aftercare: longitudinal analysis of Oxford House. Addict Behav. 2007;32(4):803–818. doi: 10.1016/j.addbeh.2006.06.014. [DOI] [PubMed] [Google Scholar]
- 35.Jason LA, Olson BD, Ferrari JR, Lo Sasso AT. Communal housing settings enhance substance abuse recovery. Am J Public Health. 2006;96(10):1727–1729. doi: 10.2105/AJPH.2005.070839. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 36.Humphreys K. Clinicians’ referral and matching of substance abuse patients to self-help groups after treatment. Psychiatr Serv. 1997;48(11):1445–1449. doi: 10.1176/ps.48.11.1445. [DOI] [PubMed] [Google Scholar]
- 37.Humphreys K, Mankowski ES, Moos RH, Finney JW. Do enhanced friendship networks and active coping mediate the effect of self-help groups on substance abuse? Ann Behav Med. 1999;21(1):54–60. doi: 10.1007/BF02895034. [DOI] [PubMed] [Google Scholar]
- 38.McKay JR, McLellan AT, Alterman AI, Cacciola JS, Rutherford MJ, O’Brien CP. Predictors of participation in aftercare sessions and self-help groups following completion of intensive outpatient treatment for substance abuse. J Stud Alcohol. 1998;59(2):152–162. doi: 10.15288/jsa.1998.59.152. [DOI] [PubMed] [Google Scholar]
- 39.Ouimette PC, Moos RH, Finney JW. Influence of outpatient treatment and 12-step group involvement on one-year substance abuse treatment outcomes. J Stud Alcohol. 1998;59(5):513–522. doi: 10.15288/jsa.1998.59.513. [DOI] [PubMed] [Google Scholar]
- 40.McKellar J, Stewart E, Humphreys K. Alcoholics Anonymous involvement and positive alcohol-related outcomes: cause, consequence, or just a correlate? A prospective 2-year study of 2,319 alcohol-dependent men. J Consult Clin Psychol. 2003;71(2):302–308. doi: 10.1037/0022-006x.71.2.302. [DOI] [PubMed] [Google Scholar]
- 41.Ritsher JB, McKellar JD, Finney JW, Otilingam PG, Moos RH. Psychiatric comorbidity, continuing care and mutual help as predictors of five-year remission from substance use disorders. J Stud Alcohol. 2002;63(6):709–715. doi: 10.15288/jsa.2002.63.709. [DOI] [PubMed] [Google Scholar]
- 42.Moos RH, Moos BS. Protective resources and long-term recovery from alcohol use disorders. Drug Alcohol Depend. 2007;86(1):46–54. doi: 10.1016/j.drugalcdep.2006.04.015. [DOI] [PubMed] [Google Scholar]
- 43.Emrick CD, Tonigan JS, Montgomery H, Little L. Alcoholics anonymous: what is currently known? In: McCrady BS, Miller WR, editors. Research on Alcoholics Anonymous: Opportunities and Alternatives. New Brunswick, NJ: Rutgers University Press; 1993. pp. 41–76. [Google Scholar]
- 44.Ogborne AC. Assessing the effectiveness of alcoholics anonymous in the community: meeting the challenges. In: McCrady BS, Miller WR, editors. Research on Alcoholics Anonymous: Opportunities and Alternatives. New Brunswick, NJ: Rutgers University Press; 1993. pp. 339–356. [Google Scholar]
- 45.Weisner C, Greenfield T, Room R. Trends in the treatment of alcohol problems in the US general population, 1979 through 1990. Am J Public Health. 1995;85(1):55–60. doi: 10.2105/ajph.85.1.55. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 46.Morgenstern J, Labouvie E, McCrady BS, Kahler CW, Frey RM. Affiliation with Alcoholics Anonymous after treatment: a study of its therapeutic effects and mechanisms of action. J Consult Clin Psychol. 1997;65(5):768–777. doi: 10.1037//0022-006x.65.5.768. [DOI] [PubMed] [Google Scholar]
- 47.Witbrodt J, Kaskutas LA. Does diagnosis matter? Differential effects of 12-step participation and social networks on abstinence. Am J Drug Alcohol Abuse. 2005;31(4):685–707. doi: 10.1081/ada-68486. [DOI] [PubMed] [Google Scholar]
- 48.Kaskutas LA. Alcoholics Anonymous effectiveness: faith meets science. J Addict Dis. 2009;28(2):145–157. doi: 10.1080/10550880902772464. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 49.Harris J, Best D, Gossop M, et al. Prior Alcoholics Anonymous (AA) affiliation and the acceptability of the Twelve Steps to patients entering UK statutory addiction treatment. J Stud Alcohol. 2003;64(2):257–261. doi: 10.15288/jsa.2003.64.257. [DOI] [PubMed] [Google Scholar]
- 50.Tonigan JS, Miller WR, Schermer C. Atheists, agnostics and Alcoholics Anonymous. J Stud Alcohol. 2002;63(5):534–541. doi: 10.15288/jsa.2002.63.534. [DOI] [PubMed] [Google Scholar]
- 51.Walters GD. Lessons learned from project MATCH. Addict Disord Their Treat. 2002;1(4):135–139. [Google Scholar]
- 52.Galanter M. Network Therapy for Alcohol and Drug Abuse. New York City: Guilford Press; 1999. [Google Scholar]
- 53.Burden E, Hill T, Zastowny T. Developing an Accreditation System for Organizations and Programs Providing Peer Recovery Support Services. Washington, DC: Faces and Voices of Recovery; [Accessed April 28, 2016]. [cited 2012]. Available from: http://www.facesandvoicesofrecovery.org/resources/developing-accreditation-system-organizations-and-programs-providing-peer-recovery-support. [Google Scholar]
- 54.Solomon P. Peer support/peer provided services underlying processes, benefits, and critical ingredients. Psychiatr Rehabil J. 2004;27(4):392–401. doi: 10.2975/27.2004.392.401. [DOI] [PubMed] [Google Scholar]
- 55.Green CA, Yarborough MT, Polen MR, Janoff SL, Yarborough BJ. Dual recovery among people with serious mental illnesses and substance problems: a qualitative analysis. J Dual Diagn. 2015;11(1):33–41. doi: 10.1080/15504263.2014.975004. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 56.Best DW, Lubman DI. The recovery paradigm: a model of hope and change for alcohol and drug addiction. Aust Fam Physician. 2012;41(8):593–597. [PubMed] [Google Scholar]
- 57.Kelly JF, Julie DY. The role of mutual-help groups in extending the framework of treatment. Alcohol Res Health. 2011;33(4):350–355. [PMC free article] [PubMed] [Google Scholar]
- 58.Selby P, van Mierlo T, Voci SC, Parent D, Cunningham JA. Online social and professional support for smokers trying to quit: an exploration of first time posts from 2562 members. J Med Internet Res. 2010;12(3):e34. doi: 10.2196/jmir.1340. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 59.Donovan DM, Wells EA. ‘Tweaking 12-Step’: the potential role of 12-step self-help group involvement in methamphetamine recovery. Addiction. 2007;102(suppl 1):121–129. doi: 10.1111/j.1360-0443.2007.01773.x. [DOI] [PubMed] [Google Scholar]
- 60.Majer JM. Assessing the logotherapeutic value of 12-step therapy. Int Forum Logother. 1992;15:86–89. [Google Scholar]
- 61.Fiorentine R, Hillhouse MP. Drug treatment and 12-step program participation: the additive effects of integrated recovery activities. J Subst Abuse Treat. 2000;18(1):65–74. doi: 10.1016/s0740-5472(99)00020-3. [DOI] [PubMed] [Google Scholar]
- 62.Etheridge RM, Craddock SG, Hubbard RL, Rounds-Bryant JL. The relationship of counseling and self-help participation to patient outcomes in DATOS. Drug Alcohol Depend. 1999;57(2):99–112. doi: 10.1016/s0376-8716(99)00087-3. [DOI] [PubMed] [Google Scholar]
- 63.Vannicelli M. Impact of aftercare in the treatment of alcoholics: a cross-lagged panel analysis. J Stud Alcohol. 1978;39(11):1875–1886. doi: 10.15288/jsa.1978.39.1875. [DOI] [PubMed] [Google Scholar]
- 64.Bandura A. Editorial. Am J Health Promot. 1997;12(1):8–10. doi: 10.4278/0890-1171-12.1.8. [DOI] [PubMed] [Google Scholar]
- 65.Bassuk EL, Hanson J, Greene RN, Richard M, Laudet A. Peer-delivered recovery support services for addictions in the united states: a systematic review. J Subst Abuse Treat. 2016;63:1–9. doi: 10.1016/j.jsat.2016.01.003. [DOI] [PubMed] [Google Scholar]
- 66.Reif S, Braude L, Lyman DR, et al. Peer recovery support for individuals with substance use disorders: assessing the evidence. Psychiatr Serv. 2014;65(7):853–861. doi: 10.1176/appi.ps.201400047. [DOI] [PubMed] [Google Scholar]
- 67.Armitage EV, Lyons H, Moore TL. Recovery association project (RAP), Portland, Oregon. Alcohol Treat Q. 2010;28:339–357. [Google Scholar]
- 68.Mangrum L. Final Evaluation Report: Creating Access to Recovery through Drug Courts. Austin, Texas Department of State Health Services. Mental Health and Substance Abuse Services Division. Austin, TX: Gulf Coast Addiction Technology Transfer Center; 2008. [Google Scholar]
- 69.Andreas D, Ja DY, Wilson S. Peers reach out supporting peers to embrace recovery (PROSPER): a center for substance abuse treatment recovery community services program. Alcohol Treat Q. 2010;28(3):326–338. [Google Scholar]
- 70.Boisvert RA, Martin LM, Grosek M, Clarie AJ. Effectiveness of a peer-support community in addiction recovery: participation as intervention. Occup Ther Int. 2008;15(4):205–220. doi: 10.1002/oti.257. [DOI] [PubMed] [Google Scholar]
- 71.Velasquez MM, von Sternberg K, Johnson DH, Green C, Carbonari JP, Parsons JT. Reducing sexual risk behaviors and alcohol use among HIV-positive men who have sex with men: a randomized clinical trial. J Consult Clin Psychol. 2009;77(4):657–667. doi: 10.1037/a0015519. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 72.Tracy K, Burton M, Nich C, Rounsaville B. Utilizing peer mentorship to engage high recidivism substance-abusing patients in treatment. Am J Drug Alcohol Abuse. 2011;37(6):525–531. doi: 10.3109/00952990.2011.600385. [DOI] [PubMed] [Google Scholar]
- 73.Purcell DW, Latka MH, Metsch LR, et al. Results from a randomized controlled trial of a peer-mentoring intervention to reduce HIV transmission and increase access to care and adherence to HIV medications among HIV-seropositive injection drug users. J Acquir Immune Defic Syndr. 2007;46(suppl 2):S35–S47. doi: 10.1097/QAI.0b013e31815767c4. [DOI] [PubMed] [Google Scholar]
- 74.Latka MH, Hagan H, Kapadia F, et al. A randomized intervention trial to reduce the lending of used injection equipment among injection drug users infected with hepatitis C. Am J Public Health. 2008;98(5):853–861. doi: 10.2105/AJPH.2007.113415. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 75.Fatseas M, Serre F, Alexandre JM, Debrabant R, Auriacombe M, Swendsen J. Craving and substance use among patients with alcohol, tobacco, cannabis or heroin addiction: a comparison of substance- and person-specific cues. Addiction. 2015;110(6):1035–1042. doi: 10.1111/add.12882. [DOI] [PubMed] [Google Scholar]
- 76.Fox HC, Talih M, Malison R, Anderson GM, Kreek MJ, Sinha R. Frequency of recent cocaine and alcohol use affects drug craving and associated responses to stress and drug-related cues. Psychoneuroendocrinology. 2005;30(9):880–891. doi: 10.1016/j.psyneuen.2005.05.002. [DOI] [PubMed] [Google Scholar]
- 77.Hartz DT, Frederick-Osborne SL, Galloway GP. Craving predicts use during treatment for methamphetamine dependence: a prospective, repeated-measures, within-subject analysis. Drug Alcohol Depend. 2001;63(3):269–276. doi: 10.1016/s0376-8716(00)00217-9. [DOI] [PubMed] [Google Scholar]
- 78.Sinha R, O’Malley SS. Craving for alcohol: findings from the clinic and the laboratory. Alcohol Alcohol. 1999;34(2):223–230. doi: 10.1093/alcalc/34.2.223. [DOI] [PubMed] [Google Scholar]
- 79.Marlow E, Grajeda W, Lee Y, Young E, Williams M, Hill K. Peer mentoring for male parolees: a CBPR pilot study. Prog Community Health Partnersh. 2015;9(1):91–100. doi: 10.1353/cpr.2015.0013. [DOI] [PubMed] [Google Scholar]
- 80.ASAM [webpage on the Internet] HIV/AIDS & Hepatitis C. Chevy Chase, MD: National Institute on Drug Abuse; [Accessed February 28, 2016]. [cited February 28, 2016]. Available from: http://www.asam.org/public-resources/hiv-aids-hepatitis-c. [Google Scholar]
- 81.Polcin DL. How should we study residential recovery homes? Ther Communities. 2015;36(3):163–172. doi: 10.1108/TC-07-2014-0027. [DOI] [PMC free article] [PubMed] [Google Scholar]