Abstract
Background:
Population monitoring and surveillance of objectively measured child weight data in Canada is limited to national surveys with poor regional applicability, and no healthy weight data are available for children less than 2 years of age. We aimed to determine the prevalence of childhood overweight and obesity using objective measures derived from primary care electronic medical records.
Methods:
Observational data included all height and weight records for children less than 20 years of age, between 2004 and 2013, from 3 Ontario primary care research networks. We calculated body mass index (BMI)-for-age and weight-for-length using the World Health Organization Growth Standards and Reference to assign growth status indicator categories by age group. Descriptive data and prevalence estimates were generated for 2013. We also compared weight-for-length for children less than 2 years of age with a corresponding billing code for known well-child visits.
Results:
Our study included 8261 children with a corresponding growth status indicator, a sample close to 4 times larger than the national survey sample. In 2013, 28.4% of children aged 5-19 years, and 6% of children aged 0-5 years, were categorized as overweight or obese. Between 2008 and 2013, the total number of 18-month well baby visit billing codes was 1152; 6.9% of this group were categorized as overweight or obese; 19.2% were categorized as having risk of overweight.
Interpretation:
Primary care electronic medical records show good potential for ongoing population monitoring of overweight and obesity, particularly for very young children for whom early intervention is likely to show the greatest positive health impact.
According to national survey data, one-third of Canadian children and adolescents aged 5 to 17 years are overweight or obese.1 Children with obesity have higher risk for both short-term health consequences2-5 and long-term persistence of obesity into adulthood.6-8 Evidence shows that early childhood is a critical time for obesity prevention strategies and that early markers of obesity could be targeted for universal and individual intervention strategies to show positive, long-term, health benefits.9-11 In Canada, child and adolescent population health monitoring is limited. There are a few national surveys, such as the Canadian Community Health Survey (CCHS) (ages ≥ 12 yr), the Health Behaviour in School-Aged Children Survey (ages 11-15 yr) and the National Longitudinal Study of Children and Youth that provide population-level surveillance data.12-14 In 2004 and 2005 the CCHS included representative subsamples in which height and weight were measured. Measured heights and weights are also obtained as part of the Canadian Health Measures Survey (CHMS) (aged 3-79 yr).15 However, data on 3-5 year olds represents about 500 children from across Canada. The absence of data for children less than 3 years of age is a critical gap, given that early life trajectories in growth and development are of great importance in determining lifelong health and well-being. In addition, the lack of objectively measured data at regional levels severely limits design and evaluation efforts of a "whole system" public health approach to the prevention of childhood obesity.16
We conducted this study to determine the prevalence of overweight and obesity, using measured heights and weights for toddlers, children and adolescents aged less than 20 years, derived from a sample of primary care electronic medical records (EMRs) from the Canadian Primary Care Sentinel Surveillance Network (CPCSSN) chronic disease database.17,18 In particular, to fill the known data gap, we examined height and weight data for toddlers less than 2 years of age and assessed them in relation to a known well-child visit, the enhanced 18-month well-baby visit.
Methods
Setting and sources of data
The CPCSSN database contains standardized, deidentified EMR data, from multiple EMR platforms, from 10 primary care practice-based research networks across Canada. For this study, data were extracted from EMRs on all patients from 3 Ontario networks of the CPCSSN (the Eastern Ontario Network, the University of Toronto Practice Based Research Network and London's Deliver Primary Healthcare Information Project). Extracted data from EMRs included all patients who had an encounter with a CPCSSN primary care provider before Mar. 31, 2014. Duplicate patient records were removed, and remaining EMR data were standardized using established CPCSSN algorithmic coding processes. For example, each height and weight value was cleaned and converted into standard units (kilograms, centimetres). Following standardization, the EMR data were uploaded into the CPCSSN database. For this study, additional eligible patients were excluded if key measurement variables were missing: height (length), weight, date of height taken, date of weight taken, year of birth and month of birth.
Data for this observational study included all height and weight records for children under 20 years of age, between Jan. 1, 2004 and Dec. 31, 2013, to produce a sample for cross-sectional research. Data from 2013 were selected to report growth status indicators because this year provided the largest sample set. In addition, we obtained the encounter date (clinic visit date), the child's month and year of birth, and the child's sex. The A002 and A002A fee codes corresponding to the enhanced 18-month well-baby visit were also extracted.19 Because a toddler's primary care clinic encounter could be associated with either a wellness or illness visit, the fee code was used to assess weight classification against a known "well toddler" visit. To provide a larger data set for this comparison, toddler visits with length and height measurements collected on the same date were taken from Jan. 1, 2008, to Dec. 31, 2013. If a toddler had weight-for-length values available, the latest one was used.
Measures
The World Health Organization (WHO) Growth Standards (birth to age 5 yr) and Reference (ages 5-19 yr) were used to assign growth status indicators.20,21 Body mass index (BMI) was calculated from height and weight measurements that were collected on the same date for children and adolescents aged 5-19 years. If a child or adolescent had multiple BMI values available in 2013, the latest one was used. BMI-for-age was used as the growth status indicator, classified into 4 categories: "wasting," "normal weight," "overweight" and "obesity." The BMI-for-age cut-off point for "overweight" was greater than the 85th percentile and the cut-off point for "obesity" was greater than the 97th percentile for these age groups.
As per recommendations outlined in the Canadian collaborative statement, using the new WHO growth charts, weight-for-length was used as the growth status indicator for children from birth to 2 years of age (toddlers).21 Weight-for-length was calculated from length and weight measurements that were collected on the same date. If a toddler had multiple weight-for-length values available between 2008 and 2013, the latest one was used. Similarly, for preschool-aged children (2-5 yr), BMI-for-age was used as the growth status indicator. Toddler and preschool-aged children were classified into 5 growth status indicator categories as "wasting," "normal weight," "risk of overweight," "overweight" and "obesity." The cut-off point for these age groups differ from older children and adolescents: the cut-off point for "risk of overweight" was greater than the 85th percentile, the cut-off point for "overweight" was greater than the 97th percentile, and the cut-off point for "obesity" was greater than the 99th percentile.
Statistical analysis
We calculated prevalence estimates for growth indicator variables and expressed the results in terms of percentage and corresponding 95% confidence intervals (CIs) by sex and age (as of the date for height or length and weight measurement). In addition, we compared the proportion of toddlers with the 18-month enhanced well-baby visit fee code to those without a fee code. Significant differences between prevalence estimates within variable categories were assessed using χ2 tests. Alpha was set a priori at 0.05. Variable classifications and all statistical analyses were performed in 2015 using SAS, version 9.3 (SAS Institute, Cary, NC).
Ethics approval
This study was approved by the Health Sciences Research Ethics Board at Queen's University.
Results
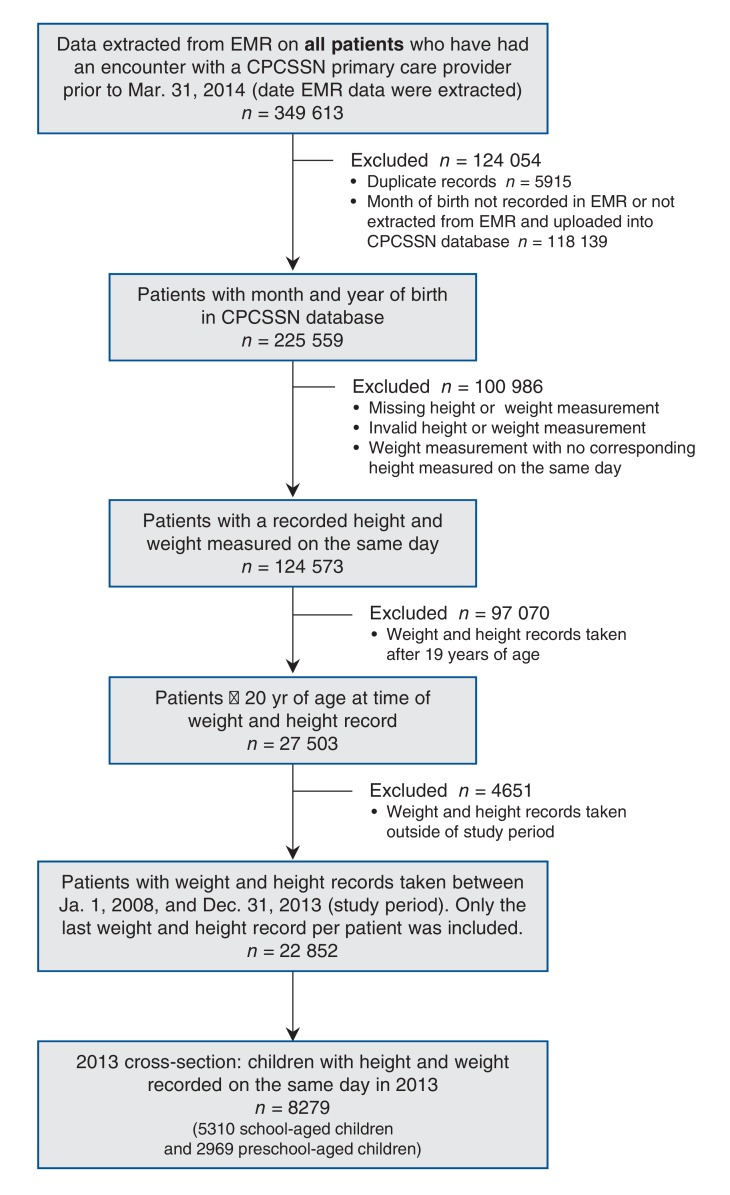
In total, 349 613 patient records were extracted from source EMRs. Duplicate records (5915) were identified and removed, and the remaining 343 698 records were uploaded to the CPCSSN database. Patient records with a missing month of birth (118 139), a missing or invalid height or weight measurement or weight measurement without a height measurement taken on the same date (100 986) were excluded. Records for patients aged 20 years and older were removed from the data set (97 070). A further 4651 weight and height records in the remaining data set were removed because the measurements were taken outside of the study period. The final child and adolescent sample of children with weight and height records (with the same measurement date) taken between Jan. 1, 2008, and Dec. 31, 2013, was 22 852. See Figure 1 for a flow diagram of the study sample inclusion process.
Figure 1.
Selection of study sample. CPCSSN = Canadian Primary Care Sentinel Surveillance Network, EMR = electronic medical record.
In 2013, there was a total of 5310 school-aged children, aged 5-19 years, with BMI-for-age calculated from height and weight measurements that were collected on the same date. There was a total of 1842 preschool-aged children, 2-5 years of age, with BMI-for-age and a total of 1127 toddlers (aged 0-2 yr) with a weight-for-length calculated from length and weight measurements that were collected on the same date in 2013. This represents a total of 8279 children, from birth to 19 years of age, with a growth status indicator derived from objectively measured height (length) and weight.
BMI-for-age for school-aged children (aged 5-19 yr) derived from the last height and weight measurements taken from encounters in 2013 are presented in Table 1. The overall prevalence of overweight and obesity was 28.4%. Boys and girls were equally represented (48.1% and 51.8%, respectively). Significantly more boys aged 12-19 years were classified as overweight and obese compared with girls in the same age group. For boys 5-11 years of age, significantly more were classified as obese compared with girls in the same age group. It follows that girls were significantly more likely to be classified as normal weight compared with boys. There were no significant differences across age groups within BMI-for-age categories for children and adolescents aged 5-19 years.
Table 1: Percentage distribution of school-aged children and adolescents, by BMI-for-age category in 2013.
|
Age group, yr |
No. of children | Percentage (95% CI) | |||
|---|---|---|---|---|---|
| Wasting | Normal weight | Overweight* | Obesity† | ||
| All children and adolescents | |||||
| 5-11 | 2649 | 2.6 (1.9 to 3.2) | 69.5 (67.7 to 71.2) | 18.1 (16.6 to 19.6) | 9.9 (8.7 to 11.0) |
| 12-19 | 2661 | 1.5 (1.1 to 2.0) | 69.6 (67.8 to 71.4) | 18.0 (16.5 to 19.5) | 10.9 (9.7 to 12.1) |
| 5-19 | 5310 | 2.1 (1.7 to 2.4) | 69.5 (68.3 to 70.8) | 18.0 (17.0 to 19.1) | 10.4 (9.5 to 11.2) |
| Boys | |||||
| 5-11 | 1356 | 3.3 (2.3 to 4.3) | 65.7 (63.1 to 68.3) | 19.4 (17.3 to 21.5) | 11.6 (9.8 to 13.3) |
| 12-19 | 1201 | 1.8 (1.0 to 2.6) | 64.2 (61.4 to 66.9) | 20.8 (18.5 to 23.2) | 13.2 (11.2 to 15.1) |
| 5-19 | 2557 | 2.6 (2.0 to 3.3) | 65.0 (63.1 to 66.9) | 20.1 (18.5 to 21.6) | 12.3 (11.0 to 13.6) |
| Girls | |||||
| 5-11 | 1293 | 1.8 (1.0 to 2.5) | 73.4‡ (70.9 to 75.8) | 16.7 (14.6 to 18.8) | 8.1‡ (6.6 to 9.6) |
| 12-19 | 1460 | 1.3 (0.7 to 1.9) | 74.0‡ (71.8 to 76.3) | 15.7‡ (13.8 to 17.6) | 9.0‡ (7.5 to 10.5) |
| 5-19 | 2753 | 1.5 (1.0 to 2.0) | 73.7‡ (72.1 to 75.4) | 16.2‡ (14.8 to 17.6) | 8.6‡ (7.5 to 9.6) |
Note: BMI = Body Mass Index, CI = confidence interval.
*Cut-off > 85th percentile.
†Cut-off > 97th percentile.
‡Significantly different from boys within the same age group (p < 0.05).
The percentage distribution of toddler (aged 0-2 yr) and preschool children (aged 2-5 yr) by growth status indicator, weight-for-length and BMI-for-age are presented in Table 2. Overall, 6.0% of toddlers and preschool-aged children were classified as overweight or obese in 2013; 18.1% were classified as having risk of overweight. Although we recognize that different growth indicators for these 2 age groups may prohibit comparison of growth between age groups, there appeared to be significantly more toddlers classified as wasting (6.8%) compared with preschool-aged children (2.7%) (and consequently, preschool-aged children were more likely to be classified as having normal weight). Both toddler and preschool-aged girls were significantly more likely to be classified as normal weight compared with boys in the same age groups.
Table 2: Percentage distribution of toddler and preschool-aged children, by growth status indicator* category in 2013.
| Age group, yr | No. of children | Percentage (95% CI) | ||||
|---|---|---|---|---|---|---|
| Wasting | Normal weight | Risk of overweight† | Overweight‡ | Obesity§ | ||
| All children | ||||||
| 0-2 | 1127 | 6.8 (5.3 to 8.3) | 68.5 (65.7 to 71.3) | 18.0 (15.7 to 20.3) | 5.5 (4.1 to 6.9) | 1.2 (0.5 to 1.8) |
| 2-5 | 1842 | 2.7 (1.9 to 3.4)¶ | 73.5 (71.4 to 75.5)¶ | 18.2 (16.4 to 20.0) | 4.0 (3.0 to 4.9) | 1.7 (1.1 to 2.4) |
| 0-5 | 2969 | 4.2 (3.5 to 5.0) | 71.6 (69.9 to 73.2) | 18.1 (16.7 to 19.5) | 4.5 (3.8 to 5.3) | 1.5 (1.1 to 2.0) |
| Boys | ||||||
| 0-2 | 566 | 8.1 (5.8 to 10.5) | 63.8 (59.7 to 67.8) | 20.1 (16.7 to 23.5) | 6.7 (4.6 to 8.9) | 1.2 (0.2 to 2.2) |
| 2-5 | 918 | 3.7 (2.4 to 5.0) | 70.2 (67.1 to 73.2) | 19.5 (16.9 to 22.1) | 4.4 (3.0 to 5.7) | 2.3 (1.3 to 3.3) |
| 0-5 | 1484 | 5.4 (4.2 to 6.6) | 67.7 (65.3 to 70.1) | 19.7 (17.7 to 21.8) | 5.3 (4.1 to 6.4) | 1.9 (1.2 to 2.6) |
| Girls | ||||||
| 0-2 | 561 | 5.5 (3.5 to 7.5) | 73.3 (69.5 to 77.0)** | 15.9 (12.8 to 19.0) | 4.3 (2.5 to 6.0) | 1.1 (0.1 to 2.0) |
| 2-5 | 924 | 1.6 (0.8 to 2.5) | 76.7 (74.0 to 79.5)** | 16.9 (14.4 to 19.4) | 3.6 (2.3 to 4.8) | 1.2 (0.4 to 1.9) |
| 0-5 | 1485 | 3.1 (2.2 to 4.0)** | 75.4 (73.2 to 77.6)** | 16.5 (14.6 to 18.4) | 3.8 (2.8 to 4.8) | 1.1 (0.6 to 1.7) |
Note: CI = confidence interval.
*For children birth to 2 years of age, weight-for-length was used as the growth status indicator; for children 2 to 5 years of age, BMI-for-age was used as the growth status indicator. Cut-off points are the same for each indicator.
†Cut-off > 85th percentile.
‡Cut-off > 97th percentile.
§Cut-off > 99.9th percentile.
¶Significantly different from toddlers (p < 0.05).
**Significantly different from boys within the same age group (p < 0.05).
Between 2008 and 2013, toddlers who had physician encounters without an 18-month enhanced well-baby visit fee code assigned were significantly more likely to be classified as wasting compared with toddlers with well-baby visits (9.1% v. 3.3%, respectively) (Table 3). Significantly more boys than girls in the wasting category (10.9% v. 7.1%, respectively) visited their physician for reasons other than a well-baby visit. The overall percentage of toddlers who were classified as overweight and obese between 2008 and 2013 was 6.7%; 17.5% were classified as having risk of overweight.
Table 3: Percentage distribution of toddlers less than 2 years of age, by weight-for-length category, with and without the 18-month enhanced well baby visit fee code (2008-2013).
| Group | No. of children | Percentage (95% CI) | ||||
|---|---|---|---|---|---|---|
| Wasting | Normal weight | Risk of overweight* | Overweight† | Obesity‡ | ||
| All toddlers | ||||||
| 18-month fee code | 1154 | 3.3 (2.2 to 4.4) | 70.6 (68.0 to 73.3) | 19.2 (16.9 to 21.6) | 6.1 (4.6 to 7.5) | 0.8 (0.2 to 1.3) |
| Without fee code | 2000 | 9.1 (7.8 to 10.3)§ | 68.1 (66.0 to 70.2) | 16.5 (14.8 to 18.2) | 5.3 (4.3 to 6.3) | 1.1 (0.6 to 1.5) |
| All aged < 2 yr | 3154 | 6.9 (6.0 to 7.8) | 69.0 (67.4 to 70.7) | 17.5 (16.2 to 18.8) | 5.6 (4.8 to 6.4) | 1.0 (0.6 to 1.3) |
| Boys | ||||||
| 18-month fee code | 560 | 3.8 (2.1 to 5.4) | 68.2 (64.3 to 72.2) | 20.9 (17.4 to 24.3) | 6.1 (4.0 to 8.1) | 1.1 (0.1 to 2.0) |
| Without fee code | 1032 | 10.9 (8.9 to 12.8) | 65.9 (63.0 to 68.8) | 16.7 (14.3 to 19.0) | 5.7 (4.3 to 7.2) | 0.9 (0.3 to 1.5) |
| All boys aged < 2 yr | 1592 | 8.4 (7.0 to 9.7) | 66.7 (64.4 to 69.1) | 18.2 (16.2 to 20.1) | 5.8 (4.7 to 7.0) | 0.9 (0.4 to 1.4) |
| Girls | ||||||
| 18-month fee code | 594 | 2.9 (1.4 to 4.3) | 72.9 (69.2 to 76.6) | 17.7 (14.5 to 20.8) | 6.1 (4.1 to 8.1) | 0.5 ( -0.1 to 1.2) |
| Without fee code | 968 | 7.1 (5.5 to 8.8)¶ | 70.5 (67.5 to 73.4) | 16.3 (13.9 to 18.7) | 4.9 (3.4 to 6.3) | 1.2 (0.5 to 2.0) |
| All girls aged < 2 yr | 1562 | 5.5 (4.3 to 6.7) | 71.4 (69.1 to 73.7) | 16.8 (14.9 to 18.7) | 5.3 (4.2 to 6.5) | 1.0 (0.4 to 1.5) |
Note: CI = confidence interval.
*Cut-off > 85th percentile.
†Cut-off > 97th percentile.
‡Cut-off > 99.9th percentile.
§Significantly different from toddlers with the 18-month enhanced well baby visit code (p < 0.05).
¶Significantly different from boys within the same fee code category (p < 0.05).
Interpretation
Our results suggest that 6.7% of toddlers aged less than 2 years are already overweight or obese and that 18.0% of toddlers are at risk of overweight. For school-aged children and adolescents (aged 5-19 yr), population estimates of overweight and obesity in our study are slightly lower than estimates derived from the CHMS (2009 to 2011) for children aged 5-17 years22 (28.4% v. 31.5%, respectively). This lower estimate is likely due to more "unwell" child visits with primary care providers in our study population compared with a general population. Similarities across weight-for-length classifications for normal, risk of overweight, overweight and obesity for toddlers less than 2 years of age with and without a "well-child visit" code suggest that weight-for-length measures derived from primary care EMRs can provide good proxy population risk of overweight, overweight and obesity estimates for this younger age group. The discrepancy between groups for the wasting category supports the inherent population bias in our study: it is likely that children with poor weight gain during infancy or who are unwell at a younger age visit primary care providers more often.
Our study includes height (length) and weight measurements for a large number of children and adolescents less than 20 years of age and population assessment measures for toddlers and preschool-aged children less than 3 years of age. Our study sample was almost 4 times larger than the national survey sample from the second cycle of the CHMS.22 Moreover, indicator variables were derived from objectively measured length, height and weight records in a clinical setting. Parent-reported measures of child heights and weights are consistently underestimated.23 It is commonly agreed that the best place for measuring length, height and weight is in primary care settings during routine wellness visits; this setting minimizes concerns about unintended negative consequences related to growth monitoring in other settings (e.g., schools) such as stigmatization; it ensures appropriate equipment is used; it provides ongoing staff training; and it follows measurement protocols.24-26
Limitations
Our results depend on the quality of data that we were able to extract. The recording of primary care EMR data continues to suffer entry error and can be absent or unavailable for use.27-29 Missing measurements for length, height and weight and data standardization are variable across clinics and EMRs, as well as within the same EMR.30,31
Our study population was limited to patients who visit their primary care providers. In a study investigating the representativeness of patients in CPCSSN, network patients were reasonably representative of patients in Canadian primary care practices and only somewhat representative of the Canadian general population.32 Ontario had the highest proportion of patients in CPCSSN; provincial-level comparison was reasonable.32
Our data were derived from records from physicians who participate as sentinels with the CPCSSN, limiting data extraction to include only providers who use EMRs. Although the number of primary care physicians using EMRs in Canada (77.6%) has more than doubled since 2006, there may be practice differences between providers who use or do not use EMRs.33,34 Because our study population comprised toddlers, children and adolescents who visit their primary care provider, the children may represent a population with shifting growth indicator measures due to medical reasons, biasing our prevalence estimates.35
For toddlers less than 2 years of age, length is most often measured lying down as opposed to standing. There are inherent practical challenges to providing accurate measurement of length for infants and toddlers, despite standardized techniques and equipment.21 For example, it is difficult for toddlers to lie still and to capture a measurement with full extension of the legs. Similarly, height measurements for older children may be biased by measurement variability. Despite measures taken by trained care providers in primary care settings, it is possible that growth indicator classifications may not be accurately derived given the measurement difficulty.
Finally, it is important to note that weight-for-length and BMI-for-age growth indicators represent only some of many risk factors,9,11,36 and that any prevention or treatment strategy, whether targeted or universal, must clearly account for the complexity of factors that influence healthy growth and development.
Conclusion
Evidence clearly indicates the need to assess weight status in children and adolescents, particularly for toddlers and preschoolers less than 3 years of age.25 Our study shows that EMR data are a valuable source for this information. These results provide a foundation upon which to build an ongoing, regionally specific, longitudinal monitoring system for population healthy weight status of Canadian toddlers, children and adolescents, especially toddlers, against which prevention measures may be designed, implemented and evaluated. Although primary care could become an improved source for healthy weight surveillance, a whole system population health approach to prevention is necessary.16,25,37 Our study shows the first steps toward improving our knowledge so that, collectively, clinical and community partners know how, when and where to focus and scale successful health promotion programming and policies.
Supplemental information
For reviewer comments and the original submission of this manuscript, please see www.cmajopen.ca/content/4/3/E538/suppl/DC1
Supplementary Material
Acknowledgements
The authors thank the Canadian Primary Care Sentinel Surveillance Network (CPCSSN) and following Ontario regional networks: the DELPHI (Deliver Primary Healthcare Information) Project; the University of Toronto Practice Based Research Network (UTOPIAN); the Eastern Ontario Network (EON); and their respective sentinel physicians, for providing the data for this study. This research was supported by the Centre for Studies in Primary Care at Queen's University and the EON, 1 of 10 research networks of the CPCSSN.
References
- 1.Roberts K, Shields M, de Groh M, et al. Overweight and obesity in children and adolescents: results from the 2009 to 2011 Canadian Health Measures Survey. Ottawa: Statistics Canada. 2012. [accessed 2013 Oct. 18]. Available www.statcan.gc.ca/pub/82-003-x/2012003/article/11706-eng.pdf. [PubMed]
- 2.Reilly JJ, Methven E, McDowell ZC, et al. Health consequences of obesity. Arch Dis Child. 2003;88:748–52. doi: 10.1136/adc.88.9.748. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Freedman DS, Mei Z, Srinivasan SR, et al. Cardiovascular risk factors and excess adiposity among overweight children and adolescents : trhe Bogalusa Heart Study. J Pediatr. 2007;150:12–17.e2. doi: 10.1016/j.jpeds.2006.08.042. [DOI] [PubMed] [Google Scholar]
- 4.Thompson DR, Obarzanek E, Franko DL, et al. Childhood overweight and cardiovascular disease risk factors : The national heart, lung, and blood institute growth and health study. J Pediatr. 2007;150:18–25. doi: 10.1016/j.jpeds.2006.09.039. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Skinner AC, Mayer ML, Flower K, et al. Using BMI to determine cardiovascular risk in childhood: how do the BMI cutoffs fare? Pediatrics. 2009;124:e905–12. doi: 10.1542/peds.2009-0179. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Park MH, Falconer C, Viner RM, et al. The impact of childhood obesity on morbidity and mortality in adulthood: a systematic review. Obes Rev. 2012;13:985–1000. doi: 10.1111/j.1467-789X.2012.01015.x. [DOI] [PubMed] [Google Scholar]
- 7.Singh AS, Mulder C, Twisk JW, et al. Tracking of childhood overweight into adulthood: a systematic review of the literature. Obes Rev. 2008;9:474–88. doi: 10.1111/j.1467-789X.2008.00475.x. [DOI] [PubMed] [Google Scholar]
- 8.Herman KM, Craig CL, Gauvin L, et al. Tracking of obesity and physical activity from childhood to adulthood: the Physical Activity Longitudinal Study. Int J Pediatr Obes. 2009;4:281–8. doi: 10.3109/17477160802596171. [DOI] [PubMed] [Google Scholar]
- 9.Brisbois TD, Farmer AP, McCargar LJ. Early markers of adult obesity: a review. Obes Rev. 2012;13:347–67. doi: 10.1111/j.1467-789X.2011.00965.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Matusik P, Malecka-Tendera E. Overweight prevention strategies in preschool children. Int J Pediatr Obes. 2011;6(Suppl 2):2–5. doi: 10.3109/17477166.2011.613651. [DOI] [PubMed] [Google Scholar]
- 11.Weng SF, Redsell SA, Swift JA, et al. Systematic review and meta-analyses of risk factors for childhood overweight identifiable during infancy. Arch Dis Child. 2012;97:1019–26. doi: 10.1136/archdischild-2012-302263. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Canadian Community Health Survey - Annual component (CCHS). Ottawa: Statistics Canada. [accessed 2015 Oct. 6]. Available www23.statcan.gc.ca/imdb/p2SV.pl?Function=getSurvey&SDDS=3226.
- 13.Roberts C, Freeman J, Samdal O, et al. The Health Behaviour in School-aged Children (HBSC) study: methodological developments and current tensions. Int J Public Health. 2009;54(Suppl 2):140–50. doi: 10.1007/s00038-009-5405-9. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.National Longitudinal Survey of Children and Youth (NLSCY). Ottawa: Statistics Canada. [accessed 2015 May 22]. Available www23.statcan.gc.ca/imdb/p2SV.pl?Function=getSurvey&SDDS=4450.
- 15.Canadian Health Measures Survey (CHMS). Ottawa: Statistics Canada. [accessed 2013 Oct. 21]. Available www23.statcan.gc.ca/imdb/p2SV.pl?Function=getSurvey&SDDS=5071&Item_Id=129548&lang=en.
- 16.Dietz WH, Baur LA, Hall K, et al. Management of obesity: improvement of health-care training and systems for prevention and care. Lancet. 2015;385:2521–33. doi: 10.1016/S0140-6736(14)61748-7. [DOI] [PubMed] [Google Scholar]
- 17.Birtwhistle R, Williamson T. Primary care electronic medical records: a new data source for research in Canada. CMAJ. 2015;187:239–40. doi: 10.1503/cmaj.140473. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.Birtwhistle R, Keshavjee K, Lambert-Lanning A, et al. Building a pan-Canadian primary care sentinel surveillance network: initial development and moving forward. J Am Board Fam Med. 2009;22:412–22. doi: 10.3122/jabfm.2009.04.090081. [DOI] [PubMed] [Google Scholar]
- 19.Enhanced 18-month well baby visit, and foot care services. The Education and Prevention Committee Bulletin, vol 8, no 5, p. 25-7. Toronto: Ontario Medical Association. 2010. Available https://www.oma.org/Resources/Documents/0805EPC_Bulletin.pdf (accessed 2015 May 15)
- 20.The WHO Child Growth Standards. Geneva: World Health Organization. 2006. [accessed 2014 Oct. 16]. Available www.who.int/childgrowth/en/
- 21.Promoting optimal monitoring of child growth in Canada: using the new WHO growth charts. Collaborative public policy statement. Toronto: Dietitians of Canada; Ottawa: Canadian Pediatric Society. 2010. Available www.dietitians.ca/downloadable-content/public/tcg-position-paper.aspx(accessed 2013 Oct. 6) [DOI] [PubMed]
- 22.Roberts KC, Shields M, de Groh M, et al. Overweight and obesity in children and adolescents: results from the 2009 to 2011 Canadian Health Measures Survey. Health Rep. 2012;23:37–41. [PubMed] [Google Scholar]
- 23.Shields M, Connor Gorber S, Janssen I, et al. Obesity estimates for children based on parent-reported versus direct measures. Health Rep. 2011;22:47–58. [PubMed] [Google Scholar]
- 24.Ontario Agency for Health Protection and Promotion (Public Health Ontario). Measuring the health of infants, children and youth for public health in Ontario: Indicators, gaps and recommendations for moving forward. Toronto: Queen's Printer for Ontario. 2013. [Google Scholar]
- 25.Canadian Task Force on Preventive Health Care. Recommendations for growth monitoring, and prevention and management of overweight and obesity in children and youth in primary care. CMAJ. 2015;187:411–21. doi: 10.1503/cmaj.141285. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 26.Himes JH. Challenges of accurately measuring and using BMI and other indicators of obesity in children. Pediatrics. 2009;124(Suppl 1):S3–22. doi: 10.1542/peds.2008-3586D. [DOI] [PubMed] [Google Scholar]
- 27.Shephard E, Stapley S, Hamilton W. The use of electronic databases in primary care research. Fam Pract. 2011;28:352–4. doi: 10.1093/fampra/cmr039. [DOI] [PubMed] [Google Scholar]
- 28.Greiver M, Barnsley J, Glazier RH, et al. Measuring data reliability for preventive services in electronic medical records. BMC Health Serv Res. 2012;12:116. doi: 10.1186/1472-6963-12-116. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 29.Coleman N, Halas G, Peeler W, et al. From patient care to research: a validation study examining the factors contributing to data quality in a primary care electronic medical record database. BMC Fam Pract. 2015;16:11. doi: 10.1186/s12875-015-0223-z. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 30.Rigobon AV, Birtwhistle R, Khan S, et al. Adult obesity prevalence in primary care users: An exploration using Canadian primary care sentinel surveillance network (CPCSSN) data. Can J Public Health. 2015;106:e283–9. doi: 10.17269/cjph.106.4508. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 31.Dean BB, Lam J, Natoli JL, et al. Use of electronic medical records for health outcomes research: a literature review. Med Care Res Rev. 2009;66:611–38. doi: 10.1177/1077558709332440. [DOI] [PubMed] [Google Scholar]
- 32.Queenan JA, Williamson T, Khan S, et al. Representativeness of patients and providers in the Canadian Primary Care Sentinel Surveillance Network: a cross-sectional study. CMAJ Open. 2016;4:E28–32. doi: 10.9778/cmajo.20140128. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 33.Zelmer J, Hagens S. Advancing primary care use of electronic medical records in Canada. Health Reform Observer, vol. 2, issue 3. Toronto: Canada Health Infoway. 2014. [accessed 2015 May 27]. Available www.infoway-inforoute.ca/en/component/edocman/2134-advancing-primary-care-use-of-electronic-medical-records-in-canada/view-document?Itemid=101.
- 34.2013 Survey results. Mississauga: National Physician Survey. 2013. [accessed 2014 Mar. 14]. Available http://nationalphysiciansurvey.ca/surveys/2013-survey/survey-results/
- 35.Maayan L, Correll CU. Weight gain and metabolic risks associated with antipsychotic medications in children and adolescents. J Child Adolesc Psychopharmacol. 2011;21:517–35. doi: 10.1089/cap.2011.0015. [DOI] [PubMed] [Google Scholar]
- 36.Wheeler JJ. Risk of obesity at 4 to 6 years of age among overweight or obese 18-month-olds: community-based cohort study. Can Fam Physician. 2013;59:e202–8. [PMC free article] [PubMed] [Google Scholar]
- 37.Lobstein T, Jackson-Leach R, Moodie ML, et al. Child and adolescent obesity: part of a bigger picture. Lancet. 2015;385:2510–20. doi: 10.1016/S0140-6736(14)61746-3. [DOI] [PMC free article] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.