Abstract
This paper presents a description and pilot data for a new adjunctive intervention designed to reduce suicidal behavior among high-risk individuals. The Coping Long Term with Active Suicide Program (CLASP) has three major components: 1) three individual, in-person meetings, 2) one significant other/family meeting and 3) 11 brief (15-30 min) phone contacts with the patient and his/her significant other. Open trial and pilot randomized trial data provide preliminary evidence that CLASP is a feasible, acceptable and efficacious intervention to reduce suicidal behavior.
Introduction
Suicidal behavior is a significant public health issue. In 2013, there were 41,149 deaths attributed to suicide in the United States. Although completed suicide rates are high, attempted suicide is unfortunately an even more common event with approximately 18 people attempting suicide for every one person who completes suicide.
Despite the public health significance of suicidal behavior, relatively few controlled trials have evaluated interventions to reduce suicidal behavior, especially in the U.S. Overall, the results of available studies have been mixed. Virtually all reviews (Comtois & Linehan, 2006; Hepp, Wittmann, Schnyder, & Michel, 2004; Institute of Medicine, 2002; Linehan, 2008; HHS, 2012) have commented on the paucity of studies, small sample sizes, small effects and inconsistent results.
Thus, there is a compelling need for development and evaluation of new interventions for suicide prevention. Similarly, development and evaluation of suicide interventions is one of the objectives of the “National Strategy for Suicide Prevention” (HHS, 2012) “Evaluate the Effectiveness of Suicide Prevention Programs (Objective 13.1)”.
Consistent with this agenda, we have developed a new intervention called Coping Long Term with Active Suicide Program (CLASP) that targets multiple risk factors for suicide using a unique combination of formats (in-person and telephone) and therapeutic strategies (values-goals clarification, problem solving, significant other support).
Coping Long Term with Active Suicide Program (CLASP)
The CLASP intervention is an adjunctive intervention specifically designed to reduce subsequent suicidal behavior in high risk populations during times of acute risk or transition. CLASP has three major components: 1) three individual, in-person meetings, 2) one significant other/family meeting and 3) and 11 brief (15-30 min) phone contacts with the patient and his/her significant other.
Treatment Rationale and Targets
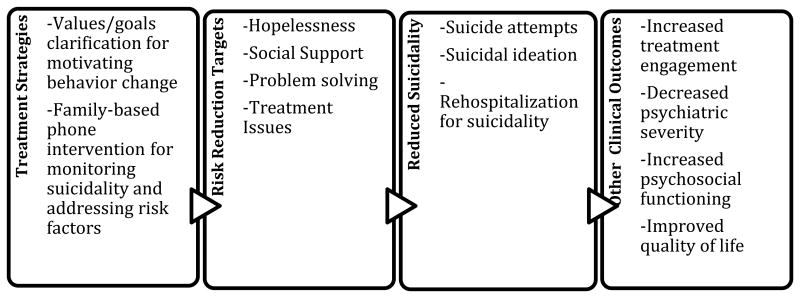
Suicide risk is multi-determined. We chose to employ a “risk reduction” model similar to those utilized in heart disease and diabetes (Cockcroft, Wilkinson, & Yki-Jarvinen, 2001; Kuller, Neaton, Caggiula, & Falvo-Gerard, 1980). Modifying risk factors is hypothesized to decrease the incidence of unwanted outcomes. The more risk factors modified the lower the risk of the unwanted outcome is assumed to be. Some known predictors of suicidality are relatively static and difficult or impossible to change (e.g. history of attempts). Thus, we selected intervention targets that were: a) malleable, b) related to suicide risk, c) could be successfully modified by our intervention strategies, and d) were generalizable across diagnostic groups. These criteria led us to focus on: a) hopelessness, b) family and social support, c) problem solving skills and d) treatment adherence. In addition, the CLASP provider also can identify “patient-specific” risk factors in addition to our general factors for a given patient (See Figure 1).
Figure 1. Outline of Treatment Strategies and Targets.
Theoretical Basis
The strategies used in CLASP are adapted from two main therapeutic approaches: Acceptance and Commitment Therapy (ACT) (Hayes, Strosahl, & Wilson, 1999) and Family Intervention-Telephone Tracking (FITT) (Bishop et al., 2014; Miller, Weiner, Bishop, Johnson, & Albro, 1998).
Clarification of Values and Goals
ACT proposes that a discussion and clarification of the patient's personal values can facilitate behavior change (Wilson & Murrell, 2004). Values are defined as broad, personally defined verbal constructs that provide the context for more specific behaviorally consistent goals. Values provide a personal rationale that can help motivate individuals to remain committed to desired actions. In contrast, goals represent more narrowly defined desired consequences that can be impeded by various internal and external factors. Values are intentionally broader in conceptualization to promote more flexible and adaptive responses from individuals, who otherwise may feel “stuck” in narrowly-defined goals that are thwarted or unattainable. Values clarification can help patients identify new goals that are still consistent with the person's deeply held beliefs but yet more “workable” to pursue in a given context. The ACT values strategies inform the initial, in-person sessions between the patient and significant other (SO) and culminate in an individualized “Life Plan” document that represents the treatment plan to be followed during subsequent telephone contacts (see description below).
Family-based Telephone Intervention
FITT (Bishop, et al., 2014; Davis, Tremont, Bishop, & Fortinsky, 2011; Miller, et al., 1998) is designed to improve problem-solving in chronic illness. FITT consists of a single family meeting followed by telephone contacts between a provider and the patient and his/her significant other (separately). Telephone contacts are used to: a) identify and address problems in key areas relevant to the patient's illness and b) provide additional support. The phone calls with both patient and significant other focus on improving their communication and problem solving. Further, the regular phone calls allow routine monitoring of patients' levels of suicide risk. Also, the problem-solving stance of FITT increases patient and significant other coping skills and reduces treatment barriers.
Therapeutic Stance
CLASP differs from typical psychotherapy in that it involves a relatively unique combination of case management, individual and family-based therapeutic strategies. The CLASP provider's primary role is to monitor suicide risk areas, and if problems occur in these areas, to help facilitate the patient and significant other in resolving these difficulties. Thus, the CLASP provider's role is more of a treatment “advisor” than traditional “therapist.” For example, the CLASP provider would not attempt to provide direct psychotherapy to address increased depression, but would instead function more as an advisor, by exploring potential treatment options for depression with the patient and significant other. While the CLASP provider does provide some family and individual strategies, these are: a) used sparingly, b) not the major focus of the CLASP telephone calls, and c) done in the context of a more “facilitator or case manager” type relationship. For these reasons and in order to emphasize the difference between the CLASP provider and the patient's community providers, the CLASP provider identifies him/herself to the patient as a “CLASP Treatment Advisor.” Furthermore, the CLASP Advisor is more proactive than a typical clinician. The CLASP Advisor initiates the telephone calls to the patient and significant other, and will continue to contact each as necessary. Furthermore, unlike most outpatient treatments, CLASP involves both patient and significant other, providing consultation to both. Finally, if necessary, the CLASP Advisor will also contact the patient's community clinicians to facilitate/optimize treatment for the patient.
Session-by-Session Outline (See Table 1)
Table 1. CLASP Session Content Summary.
| Timing | Contact | Goals |
|---|---|---|
| In-Person Session 1 | Patient |
|
| In-Person Session 2 | Patient |
|
| In-Person Session 3 | Patient |
|
| In-Person Session 4 | Patient and Significant Other |
|
| Phone Sessions 1-11 | Patient |
|
| Phone Sessions 1-11 | Significant Other |
|
Individual In-Person Meetings
Meeting 1 focuses on rapport building, history taking and psychoeducation. Values clarification is introduced to motivate change and instill hopefulness. In Meeting 2, the Advisor reviews and finishes the values clarification discussion as needed and helps the patient define a list of short-term, values-consistent goals. The majority of Meeting 3 is spent formulating an individualized “Life Plan.” The Life Plan document provides dedicated space to record the patient's previously specified values and accompanying goals, with corresponding space to document specific actions to help the patient achieve greater consistency between values and behaviors, as well as a specific safety plan to address any future suicidality.
SO In-Person Meeting
Meeting 4 includes the Advisor, patient, and a significant other (SO) following the FITT format. The Advisor reviews psychoeducational information regarding suicide and asks the SO to discuss his/her perspective on the patient's recent hospitalization. The majority of the session is spent reviewing and discussing the patient's Life Plan. The Advisor facilitates a discussion between the SO and patient about the role the SO can play in the treatment plan to support the patient's goals. If severe patient-SO conflict is identified, referrals for family therapy are provided. If the patient cannot or is unwilling to identify a SO, he/she will continue to receive the intervention and Meeting 4 will be an additional individual meeting or skipped, based on clinical need.
Telephone contacts
Following the in-person meetings, the Advisor conducts Telephone Contacts 1-11 with the patient and their SO individually. Each session is 15-30 min in length based on the number and severity of clinical issues identified. Sessions are conducted on a schedule of decreasing frequency for a target of 11 sessions over 6 months. At the start of each contact, the Advisor conducts a brief assessment of risk factors since last contact. If suicidality is identified, this is discussed first and a safety plan is developed. Consistent with the FITT model, the Advisor facilitates problem-solving and communication between the patient and SO. The Advisor discusses problems in terms of values strategies and in reference to the previously developed Life Plan document. If a problem develops that cannot be solved in this manner, the Advisor may obtain permission to contact the patient's primary treatment provider directly or temporarily increase the frequency of the phone contacts during times of crisis. The SO phone contact proceeds in a similar manner. If an SO cannot be identified, only the patient calls will occur. The specific content and timing of calls can be seen in Table 1.
Pilot Testing
In order to begin empirical testing the CLASP intervention, we initiated an open trial, administering CLASP to a sample of inpatients with suicide risk, followed by a pilot randomized trial comparing CLASP to a control condition. Consistent with recommendations for early pilot work (Leon, Davis, & Kraemer, 2010), the major goals of this pilot work were to explore the feasibility and acceptability of the intervention and associated procedures. While we collected outcome data, these studies were not designed to be sufficiently powered to detect statistically significant effects. Instead, we were looking for “signal” that the intervention might be efficacious.
Open Pilot Trial
Subjects
Subjects consisted of 25 patients who met the following inclusion criteria: a) recent admission to a private psychiatric hospital due to previous suicide attempt or suicidal ideation with intent, b) have a diagnosis of major depressive disorder, c) be age 18 years or older, d) have a working telephone, and e) speak English sufficiently to complete study procedures. Exclusion criteria included: a) current psychotic symptoms or substance dependence, b) borderline or antisocial personality disorder with therapy-interfering behaviors, c) participation in a treatment program with established efficacy in preventing suicidal behavior, d) significant cognitive impairment, e) current homelessness; or f) discharge to long-term residential treatment. Whenever possible, subjects identified a significant other (SO; spouse/partner, sibling, child, parent, or close friend), who also participated in the study. SOs were: 1) 18 years or older; 2) able to speak and read English; and 3) in regular (weekly) contact with the participant.
Advisors and training
The CLASP intervention was provided by 6 Ph.D. clinical psychology post-doctoral fellows. These “Advisors” received training based on the CLASP Manual consisting of readings regarding suicide and the interventions utilized in the intervention, discussion and review of the CLASP intervention manual, didactic/one-to-one presentation of the CLASP model, and close supervision by the developers (IM, BG, LW) for at least two patients. Advisors go through an initial “certification” process in which they must demonstrate acceptable levels of adherence and competency prior to treating study patients with ongoing supervision and monitoring thereafter to prevent “drift.”
Procedures
The Butler Hospital Institutional Review Board approved all study procedures. Newly-admitted patients' hospital charts were screened based on inclusion and exclusion criteria after obtaining a PHI Waiver. Patients who appeared to meet study criteria were approached, given a brief verbal overview of the study, including the nature, purpose, risks, and benefits, and invited to participate. Informed consent was obtained from those who expressed interest.
CLASP
CLASP individual sessions were initiated in the hospital after consent and eligibility assessments were completed. If the in-person sessions were not completed prior to hospital discharge, they were completed on an outpatient basis as soon as possible after discharge. Following the completion of the individual and significant other sessions, the telephone calls to the patient and the significant other were initiated. The 11 CLASP calls were scheduled in decreasing frequency over the subsequent 6 month period.
Follow-up
Subsequent suicide attempts and hospitalizations due to suicide risk for six months following hospital discharge were tracked by chart review and brief follow-up contacts at 3 and 6 months post-discharge.
Results
Subject characteristics
Subject characteristics can be seen in Table 2. Briefly, subjects were both men and women and largely Caucasian, middle-aged and with some high school education. Two-thirds of the sample had a history of a prior suicide attempt, with 44% making an attempt immediately prior to admission.
Table 2. Baseline and Follow-up Data.
| Variable | Open Trial (n=25) | Randomized Trial N=55 | |
|---|---|---|---|
| CLASP (n=24) | SAFE (n=31) | ||
| Patient | |||
| Sex | Female – 10 | Female – 15 | Female – 23 |
| Male 13 | Male – 9 | Male -8 | |
| Age | 44.3 (13.7) | 42.0 (10.7) | 43.5 (10.8) |
| Race | Caucasian - 21 | Caucasian – 24 | Caucasian - 31 |
| Ethnicity | Hispanic - 1 | Hispanic – 0 | Hispanic - 2 |
| Education (years) | 14.6 (2.9) | 13.9 (3.7) | 12.5 (5.0) |
| Suicide Attempt prior to admission ( | 11 (44%) | 15 (62.5%) | 9 (29%) |
| Suicide attempt – Lifetime | 17 (68%) | 20 (83%) | 21 (69%) |
| Multiple suicide attempts – lifetime | 5 (20%) | 9 (38%) | 15 (48%) |
| Significant Other | N= 16 | N=15 | N= 23 |
| Relationship to patient | Spouse/partner – 9 | Spouse/partner 7 | Spouse/partner – 10 |
| Parent – 4 | Parent – 3 | Parent – 4 | |
| Child – 3 | Child – 1 | Child – 1 | |
| Other Relative - 1 | Other Relative-2 | Other Relative-5 | |
| Friend - 6 | Friend - 2 | Friend - 3 | |
| Follow -up | |||
| Suicide Attempt | 3 (12%) | 3 (13%) | 7 (23%) |
| Hospitalization due suicide risk | 7 (28%) | 6 (25%) | 10 (32%) |
| Suicide Attempt or Hospitalization | 7 (28%) | 6 (25%) | 12 (39%) |
Treatment adherence
A majority of patients completed all in-person sessions (n = 15; 60%), with an overall mean of 3.3 of 4 sessions completed. Six (24%) patients did not complete any subsequent telephone calls. Among those who were able to be contacted, a mean of 8.0 (of 11 scheduled) telephone calls were completed. Sixteen (64%) patients identified a significant other who participated in the intervention with a mean of 8.7 SO calls completed.
Satisfaction
Satisfaction was also quite high among patients receiving CLASP, with scores on the Client Satisfaction Questionnaire (Attkisson & Zwick, 1982) almost uniformly high (CSQ total = 26.6; SD = 2.0). On ratings of overall satisfaction, the mean was 3.7 (SD = .63) on a scale of 1 (“quite dissatisfied”) to 4 (“very satisfied.”). Although we did not formally assess significant others' satisfaction, our clinical sense is that significant others were also extremely pleased with their participation.
Outcomes
During the six month follow-up period, 3 (12%) of the sample made a suicide attempt and 7 (28%) were re-hospitalized due to suicide risk. No patient died by suicide.
Summary
The results of this preliminary open trial were very encouraging. CLASP was acceptable to roughly 75% of eligible patients. Similarly, a majority of patients were able to identify a significant other who participated actively in the program. Patient satisfaction was high. Finally, the proportion of patients with a subsequent suicide attempt (12%) was markedly below previously published re-attempt rates for suicidal psychiatric inpatients (Brown et al., 2005; Hawton & van Heeringen, 2000; Owens, Horrocks, & House, 2002). However, in order to provide a better approximation of the utility of CLASP, we initiated a pilot randomized control trial, comparing CLASP to an enhanced treatment as usual comparison.
Pilot Randomized Controlled Trial
Subjects and Procedures
Inclusion and exclusion criteria and study procedures were identical to those of the open pilot trial.
Advisors and training
As in the open pilot trial, the “advisors” for this trial consisted of 5 clinical psychologist post-doctoral fellows who received training and supervision from the CLASP developers as described above.
Comparison condition
The choice of a comparison or control condition for suicide prevention research has been the subject of much debate (Pearson, Stanley, King, & Fisher, 2001). Our control condition was an enhanced treatment as usual condition, labeled “Safety Assessment and Follow-up Evaluation” (SAFE). In addition to treatment as usual, patients participating in SAFE receive enhanced assessment and monitoring services. The enhanced monitoring consisted of regular monitoring of suicidal ideation and risk factors. We obtain releases to share information with the patient's nonstudy clinician(s). At 3 and 6 months, we provide the patient's clinician(s) with a standardized report that summarizes the patient's level of suicidal ideation and identified risk factors.
Procedure
Recruitment procedures were similar to the Open Pilot trial. Following completion of eligibility, subjects were randomly assigned using an urn randomization procedure (Stout, Wirtz, Carbonari, & Del Boca, 1994) balanced on number of previous suicide attempts and gender to receive either CLASP or SAFE as described for the 6 months post-discharge.
Follow-up
As in the Open Pilot study, subsequent suicide attempts and hospitalizations due to suicide risk for six months following hospital discharge were tracked by chart review and brief follow-up contacts at 3 and 6 months post-discharge.
Results
Subject characteristics
Subject characteristics can be seen in Table 2. Subjects included both sexes (69% female) and were mostly Caucasian and middle aged. A large proportion (75%) had made a previous suicide attempt in their lifetime and 44% had made multiple attempts. A total of 44% of the sample had made a suicide attempt immediately prior to admission to the hospital.
Treatment adherence
A total of 73% of patients completed the interventions. Similar to the Open Pilot, a proportion of patients never engaged in their assigned treatment and were unable to be contacted after discharge from the hospital (15/55; 27%). Similar proportions of these “non-engagers” were found in CLASP (6/24; 25%) and SAFE (9/31; 29%). Among those patients who did engage in the CLASP intervention, adherence was quite high with approximately 75% of the CLASP contacts (in-person and phone calls) completed to both patient and significant other.
Outcomes
During the six month follow-up period, no subject died by suicide. When compared to subjects who were assigned to SAFE, subjects assigned to CLASP had lower rates of suicide attempts (13% vs. 23%: absolute risk reduction = 10%; relative risk reduction = .45; number needed to treat = 9.9) and hospitalizations due to suicide risk (25% vs. 32%; absolute risk reduction = 7%; relative risk reduction = .23; number needed to treat = 13.8).
Discussion
In this paper, we have presented the rationale, description and preliminary pilot data for a new intervention designed to reduce suicidal behavior among high risk individuals during times of crisis or transition. The Coping Long Term with Active Suicide Program (CLASP) is an adjunctive intervention of moderate intensity that focuses on multiple risk factors using an integration of therapeutic strategies from Acceptance and Commitment Therapy and Family Intervention-Telephone Tracking in a unique combination of in-person and telephone contacts.
While preliminary, our open trial and pilot randomized trial data suggest that CLASP is a feasible and acceptable intervention and may be effective in reducing suicidal behavior. Other pilot studies have investigated the utility of CLASP for bipolar patients (Weinstock, Gaudiano, Melvin, & Miller, 2013) as well as adolescents (Yen, Spirito, Weinstock, Tezanos, Melvin & Miller, 2014) and found evidence for the feasibility and acceptability of CLASP as well as promising pilot efficacy data.
CLASP has a number of potential advantages as a suicide prevention intervention. First, CLASP is an adjunctive intervention, which allows (and encourages) patients to develop and maintain their own treatment providers. Second, both the adjunctive nature and the focus on multiple potential risk factors suggest that CLASP will be applicable to a broad selection of individuals at risk for suicide. Third, while some instruction is necessary, particularly to adopt the somewhat different “therapeutic stance” of an “advisor,” CLASP does not require intensive interventionist training. We have found that with a moderate amount of training and supervision, even less experienced therapists were able to conduct the CLASP intervention competently. Fourth, due to the limited number of in-person sessions and the brief nature of the telephone contacts, CLASP has the potential to be a cost-effective intervention.
In order to examine if these potential advantages and pilot results hold true, CLASP is currently being evaluated in larger clinical trials (Boudreaux et al., 2013; Miller, 2014; Primack, 2014). We also are testing similar interventions based on the CLASP model but applied to other clinical targets (e.g., treatment adherence) (Wenze, Gaudiano, Weinstock, Tezanos, & Miller, 2015). While these trials will ultimately determine the utility of CLASP, currently CLASP appears to offer a new, alternative intervention to reduce suicidal behavior that has substantial advantages and promise.
Acknowledgments
Funding: This project was supported by Award Number R34 MH073625 from the National Institute of Mental Health. The content is solely the responsibility of the authors and does not necessarily represent the official views of the National Institute of Mental Health or the National Institutes of Health.
Footnotes
Conflict of interest: The authors have no conflicts of interest to report.
Contributor Information
Ivan W. Miller, Director of the Psychosocial Research Program at Butler Hospital and Professor in the Department of Psychiatry and Human Behavior at the Warren Alpert Medical School of Brown University
Brandon A. Gaudiano, Research Psychologist in the Psychosocial Research Program at Butler Hospital and Associate Professor in the Department of Psychiatry and Human Behavior at the Warren Alpert Medical School of Brown University
Lauren M. Weinstock, Associate Professor in the Department of Psychiatry and Human Behavior at the Warren Alpert Medical School of Brown University
References
- Attkisson CC, Zwick R. The client satisfaction questionnaire. Psychometric properties and correlations with service utilization and psychotherapy outcome. Evaluation and Program Planning. 1982;5(3):233–237. doi: 10.1016/0149-7189(82)90074-x. [DOI] [PubMed] [Google Scholar]
- Bishop D, Miller I, Weiner D, Guilmette R, Mukand J, Feldman & Springate B. Family Intervention: Telephone Tracking (FITT): A pilot stroke outcome study. Topics in Stroke Rehabilitation. 2014;21 doi: 10.1310/tsr21S1-S63. [DOI] [PubMed] [Google Scholar]
- Boudreaux E, Miller I, Goldstein A, Sullivan A, Allen M, Manton A, Arias S, Camargo C. The Emergency Department Safety Assessment and Follow-up Evaluation (ED-SAFE): methods and design considerations. Contemporary Clinical Trials. 2013;36:14–24. doi: 10.1016/j.cct.2013.05.008. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Brown GK, Ten Have T, Henriques GR, Xie SX, Hollander JE, Beck AT. Cognitive therapy for the prevention of suicide attempts: a randomized controlled trial. JAMA Journal of the American Medical Association. 2005;294(5):563–570. doi: 10.1001/jama.294.5.563. [DOI] [PubMed] [Google Scholar]
- Cockcroft JR, Wilkinson IB, Yki-Jarvinen H. Multiple risk factor intervention in type 2 diabetes. Diabetes Obesity and Metabolics. 2001;3(1):1–8. doi: 10.1046/j.1463-1326.2001.00083.x. [DOI] [PubMed] [Google Scholar]
- Comtois KA, Linehan MM. Psychosocial treatments of suicidal behaviors: a practice-friendly review. Journal of Clinical Psychology. 2006;62(2):161–170. doi: 10.1002/jclp.20220. [DOI] [PubMed] [Google Scholar]
- Davis JD, Tremont G, Bishop DS, Fortinsky RH. A telephone-delivered psychosocial intervention improves dementia caregiver adjustment following nursing home placement. International Journal of Geriatric Psychiatry. 2011;26(4):380–387. doi: 10.1002/gps.2537. [DOI] [PubMed] [Google Scholar]
- Hayes S, Luoma J, Bond F, Masuda A, Lillis J. Acceptance and Commitment Therapy: Model, processes and outcomes. Behaviour Research and Therapy. 2006;44:1–25. doi: 10.1016/j.brat.2005.06.006. [DOI] [PubMed] [Google Scholar]
- Hayes S, Strosahl K, Wilson K. Acceptance and Commitment Therapy. New York: Guilford Press; 1999. [Google Scholar]
- Hepp U, Wittmann L, Schnyder U, Michel K. Psychological and psychosocial interventions after attempted suicide. Crisis. 2004;25:108–117. doi: 10.1027/0227-5910.25.3.108. [DOI] [PubMed] [Google Scholar]
- Reducing suicide: A national imperative. Institute of Medicine; Washington, DC: National Academies Press; 2002. [PubMed] [Google Scholar]
- Kuller L, Neaton J, Caggiula A, Falvo-Gerard L. Primary prevention of heart attacks: the multiple risk factor intervention trial. American Journal of Epidemiology. 1980;112(2):185–199. doi: 10.1093/oxfordjournals.aje.a112984. [DOI] [PubMed] [Google Scholar]
- Leon A, Davis L, Kraemer H. The role and interpretation of pilot studies in clincial research. Journal of Psychiatric Research. 2010;45(5):626–629. doi: 10.1016/j.jpsychires.2010.10.008. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Linehan MM. Suicide intervention research: a field in desperate need of development. Suicide and Life Threatening Behavior. 2008;38(5):483–485. doi: 10.1521/suli.2008.38.5.483. [DOI] [PubMed] [Google Scholar]
- Miller I. Evaluation of the Coping Long Term with Active Suicide Program. Providence, RI: NIMH RO1 MH101129 2014 [Google Scholar]
- Miller I, Weiner D, Bishop D, Johnson B, Albro J. Telephone administered family intervention following stroke. Rehabilitation Psychology. 1998;43:181. [Google Scholar]
- Owens D, Horrocks J, House A. Fatal and non-fatal repetition of self-harm: Systematic review. British Journal of Psychiatry. 2002;181(3):193–199. doi: 10.1192/bjp.181.3.193. [DOI] [PubMed] [Google Scholar]
- Pearson J, Stanley B, King C, Fisher C. Intervention, research with persons at high risk for suicidality: Safety and ethical considerations. Journal of Clinical Psychiatry. 2001;62:17–26. [PubMed] [Google Scholar]
- Primack J. Veterans Coping Long Term with Active Suicide Program. Providence, RI: VA Merit Award 2014 [Google Scholar]
- Stout R, Wirtz P, Carbonari J, Del Boca F. Ensuirng balanced distribution of prognostic factors in treatment outcome research. Journal of Studies on Alcohol, supplement. 1994;12:70–75. doi: 10.15288/jsas.1994.s12.70. [DOI] [PubMed] [Google Scholar]
- U.S. Department of Health and Human Services (HHS) Office of the Surgeon General and National Action Alliance for Suicide Prevention. 2012 National Strategy for Suicide Prevention: Goals and Objectives for Action. Washington, DC; HHS: Sep, 2012. [PubMed] [Google Scholar]
- Weinstock L, Gaudiano B, Melvin C, Miller I. The Coping Long Term with Active Suicide Program for bipolar Disorder: a pilot randomized controlled trial. Paper presented at the International Conference on Bipolar Disorder; Miami, FL. 2013. [Google Scholar]
- Wenze S, Gaudiano B, Weinstock L, Tezanos K, Miller I. Adjunctive psychosocial intervention following hospital discharge for patients with bipolar disorder and comorbid substance use: a pilot randomized controlled trial. Psychiatry Research. 2015;228(3):516–525. doi: 10.1016/j.psychres.2015.06.005. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Wilson K, Murrell A. Values Centered Interventions: Setting the course for behavioral interventions. In: Hayes S, Follett V, Linehan M, editors. The New Beahvior Therapies:Expanding the Cognitive-Behavioral Tradition. New York: Guilford Press; 2004. [Google Scholar]
- Yen S, Spirito A, Weinstock L, Tezanos K, Melvin C, Miller I. Coping Long Term with Active Suicide Program - Adolescents: Results from the pilot randomized control trial phase. Paper presented at the Associaton for the Advance of Cognitive and Behavioral Therapies; Philadelphia, PA. 2014. [Google Scholar]