Abstract
Tourette syndrome (TS) is a neuropsychiatric disorder that affects both children and adults. We searched for randomised controlled trials (RCTs) using acupuncture to treat TS written in English or Chinese without restrictions on publication status. Study selection, data extraction, and assessment of study quality were conducted independently by two reviewers. Meta-analyses were performed using Review Manager (RevMan) 5.3 software from the Cochrane Collaboration. Data were combined with the fixed-effect model based on a heterogeneity test. Results were presented as risk ratios for dichotomous data and mean differences (MDs) for continuous data. This review included 7 RCTs with a total of 564 participants. The combined results showed that acupuncture may have better short-term effect than Western medicine for TS and that acupuncture may be an effective adjuvant therapy in improving the effect of Western medicine on TS, but the evidence is limited because of existing biases. Rigorous high-quality RCTs are needed to verify these findings.
1. Background
Tourette syndrome (TS; also called Tourette's syndrome, Tourette's disorder, or Gilles de la Tourette syndrome) is an inherited neuropsychiatric disorder characterised by multiple physical (motor) tics and at least one vocal (phonic) tic present for more than 1 year [1]. These tics are characterised as sudden, rapid, recurrent, nonrhythmic motor movements or vocalisations usually appearing in bouts that can wax and wane in frequency, intensity, and diversity [2]. The population prevalence estimate of TS in children is 0.3–0.9% [3], and TS is 2–4 times more common in boys than girls [4]. Most cases are associated with other comorbidities such as obsessive compulsive disorder, attention deficit hyperactivity disorder, schizophrenia, and mental impairment. TS and these combined conditions cause impairment in people living with TS [5].
The European Society for the Study of Tourette Syndrome (ESSTS) guidelines developed in 2011 recommend that TS could be treated by medications including alpha-adrenergic agonists, typical neuroleptics, atypical neuroleptics, and benzamides [6, 7]. Medications cannot eradicate tics completely, and they can cause adverse reactions such as extrapyramidal symptoms and weight gain with atypical neuroleptics and drowsiness and extrapyramidal motoric adverse reactions with typical antipsychotics [7–10]. Therefore, there is a need for other effective and safe treatment methods for TS.
In recent years, complementary and alternative medicine (CAM) has been used to treat TS increasingly, including prayer, vitamins, massage, dietary supplements, chiropractic manipulations, meditation, diet alterations, yoga, hypnosis, homeopathy, EEG biofeedback, and acupuncture [11]. 73.6%–87.8% of TS patients selected CAM [11, 12], and 56% of patients reported improvement after CAM treatment [11].
Acupuncture is a branch of traditional Chinese medicine that dates back thousands of years [13]. It is defined as fine needles piercing into the acupoints based on traditional Chinese medicine theory. It has been reported that acupuncture can regulate the abnormal brain function of patients with tic disorders [14] and can alleviate tic symptoms [15–17]. To date, there is only one published Chinese systematic review on acupuncture for TS [18]; five RCTs and one quasi-RCT published between 2001 and 2009 were included and analysed, and all included studies were published in Chinese. This review indicated that acupuncture had a better effect than conventional Western medicine on response rate according to a Chinese criterion [19] but no difference in Yale Global Tic Severity Scale (YGTSS) evaluation; however, the studies included in the previous review were not all RCTs, and there was a high risk of bias in some studies. Nearly 20 RCTs regarding acupuncture and TS have been published since the last review [16, 20–35]. With a more comprehensive search strategy and more included databases, the present systematic review aims to update and evaluate whether acupuncture is effective and safe for alleviating the symptoms of TS.
2. Methods
2.1. Study Criteria
2.1.1. Types of Studies
RCTs written in English or Chinese were included, without restriction of publication status. We excluded quasi-randomised studies such as those with evidence of inadequate sequence generation, for example, alternate days or patient numbers.
2.1.2. Types of Participants
Studies including patients of any age who met the medically defined diagnostic criteria for TS were eligible for inclusion. Diagnostic criteria may have been from the Diagnostic and Statistical Manual, third edition (DSM-III), fourth edition (DSM-IV), or text revision of the fourth edition (DSM-IV-TR); the International Classification of Diseases, tenth version (ICD-10); the Chinese Classification of Mental Disorders, second revision version (CCMD-2R) and third version (CCMD-3); or other clearly defined diagnostic criteria. Studies including patients whose tics were transient tic disorders, chronic motor or vocal tic disorders, or tic disorders caused by medication were excluded.
2.1.3. Types of Interventions
Acceptable interventions included manual acupuncture, electroacupuncture, scalp acupuncture, auricular acupuncture, warm needling, plum-blossom needling, or intradermal needling. Acupoint injections, acupoint catgut embedding, and laser acupuncture were excluded.
Comparison interventions included no intervention/waiting list control, placebo/sham acupuncture, or active Western medicine. Studies evaluating acupuncture combined with Western medicine compared with the same Western medicine alone were included.
Studies that compared different acupoints, compared two different forms of acupuncture, compared acupuncture with a Chinese patent or decoction, or compared acupuncture plus Chinese medicine with Chinese medicine alone were excluded.
2.1.4. Types of Outcome Assessments
(i) Primary Outcomes. The most widely used checklists on tic characteristics and severity include the YGTSS, the Shapiro Tourette Syndrome Severity Scale (STSSS), and the Hopkins motor and vocal tic scale. Different scales focus on different aspects. The YGTSS includes 30 items including 18 categories of motor and vocal tics, self-injurious behaviour, and anger control problems and also a severity rating scale. The STSSS consists of five items including the noticeability to others and interference of daily life due to tics [2]. In this review, only the YGTSS was used in all included studies.
(ii) Secondary Outcomes
(1) Response Rate. Studies that reported the response rates as dichotomous measures (effective or ineffective) were considered. In some studies, patients with reduction rate of YGTSS less than 30% were regarded as “ineffective” and others as “effective.” These studies were included in this review. According to the criterion in China [19], some studies [30, 31, 39, 40] defined patients with no improvement in symptoms as “ineffective” and others as “effective,” but there was no quantified standard for improvement in this criteria, so we excluded these studies.
(2) Quality of Life (QOL). This was assessed by the health-related quality of life scale developed specifically for tic disorder patients [41], the Chinese Children and Adolescents' QOL Scale [42], and other QOL scales. None of the included studies used QOL as an outcome measure.
2.1.5. Adverse Reactions
All adverse reactions and acupuncture-related adverse reactions were analysed.
2.2. Search Methods for the Identification of Studies
We searched the Cochrane Movement Disorders Group Specialised Register of Controlled Trials, the Cochrane Central Register of Controlled Trials, MEDLINE, EMBASE, PsycINFO, and Cumulative Index to Nursing and Allied Health Literature. We also searched four Chinese electronic databases: Chinese BioMedical Literature Database, China National Knowledge Infrastructure, VIP Database for Chinese Technical Periodicals, and Wanfang Digital database.
Other electronic sources searched for relevant trials included
trial registers for ongoing and registered trials: http://www.clinicaltrials.gov/, http://www.who.int/trialsearch/Default.aspx;
reference lists from relevant reviews and trials: the Cochrane Library Database of Abstracts of Reviews of Effects (reference lists from non-Cochrane reviews on similar topics);
conference abstracts on the Web of Knowledge (http://wokinfo.com/);
OpenGrey for unpublished literature from Europe (http://www.opengrey.eu/).
The date of the last search was March 28, 2016. The search strategy used is detailed in Table 1.
Table 1.
Search strategy used in electronic databases.
| Number | Search items |
|---|---|
| 1 | Randomised controlled trial |
| 2 | Controlled clinical trial |
| 3 | Randomised |
| 4 | Randomized |
| 5 | Randomly |
| 6 | Placebo |
| 7 | Trial |
| 8 | 1 or 2–7 |
| 9 | Tourette Syndrome |
| 10 | Tourette Disorder |
| 11 | Gilles de la Tourette Syndrome |
| 12 | Tourette∗ |
| 13 | Tic |
| 14 | 9 or 10–13 |
| 15 | Acupuncture therapy |
| 16 | Acupuncture |
| 17 | Body acupuncture |
| 18 | Scalp acupuncture |
| 19 | Auricular acupuncture |
| 20 | Electroacupuncture |
| 21 | Intradermal needling |
| 22 | Plum-blossom needle |
| 23 | Acupoints |
| 24 | Acu∗ |
| 25 | 15 or 16–24 |
| 26 | 8 and 14 and 25 |
Tourette∗: any words or phrases starting with “tourette”. Acu∗: any words or phrases starting with “acu”.
2.3. Data Collection and Analysis
2.3.1. Selection of Studies
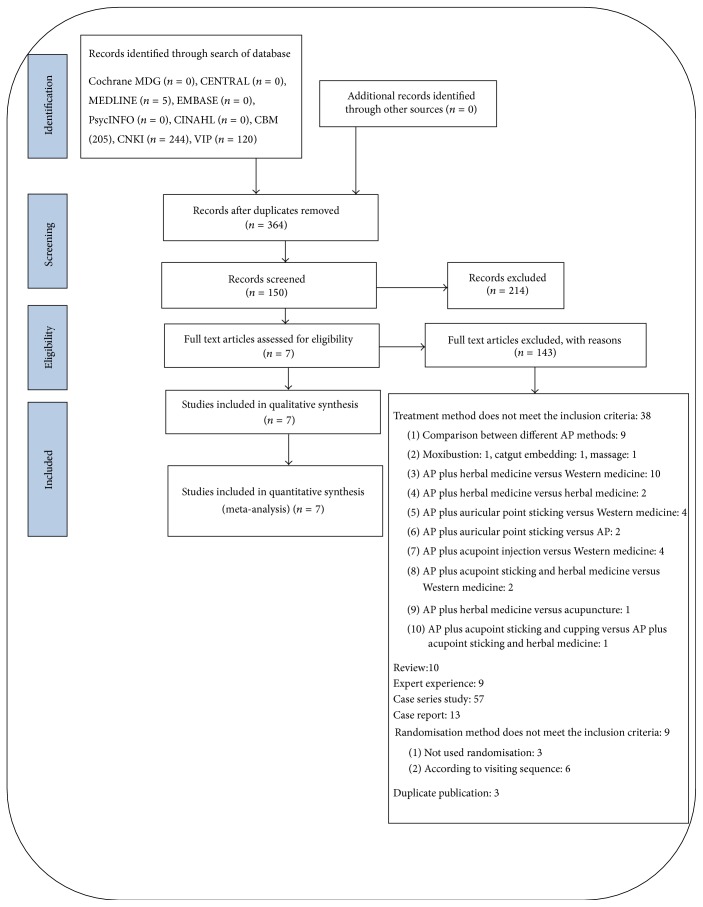
After an initial screening of titles and abstracts retrieved by the search, the full text of all potentially eligible studies was retrieved. Two review authors (YJ and LJ) independently examined these full text articles for compliance with the inclusion criteria and selected studies eligible for inclusion in the review. Disagreements about study eligibility were resolved by discussion or by a third review author (LZ). The selection process was documented in a “PRISMA” flow chart (Figure 1).
Figure 1.
PRISMA flow chart. CENTRAL: the Cochrane Central Register of Controlled Trials; CINAHL: Cumulative Index to Nursing and Allied Health Literature; CBM: Chinese Biomedical Literature Database; CNKI: China National Knowledge Infrastructure Database; VIP: a database for Chinese Technical Periodicals.
2.3.2. Data Extraction and Management
YJ and LJ independently extracted data from included studies using a data extraction form. Any disagreements were resolved by discussion or by a third review author (LZ). The extraction form included the following sections:
General study information.
Methods, including randomisation, blinding, and trial design.
Participants, including country, site, recruitment, inclusion, and exclusion.
Interventions, including methods of each group, duration, follow-up data, and withdrawals.
Outcomes, including primary and secondary outcomes.
Risk of bias, including the method of randomisation, allocation concealment, trial completion, and other bias.
We attempted to contact the original authors by telephone to obtain any incomplete data.
2.3.3. Assessment of the Risk of Bias in Included Studies
Two reviewers independently assessed the included studies for risk of bias using the Cochrane risk of bias assessment tool (Cochrane Handbook, version 5.1.0; March 2011). Reviewers assessed selection (random sequence generation and allocation concealment), performance (blinding of participants and personnel), detection (blinding of outcome assessors), attrition (incomplete outcome data), reporting (selective reporting), and other sources of bias. The assessments were categorised into three levels of bias: low risk, high risk, and unclear risk. Disagreements were resolved by discussion or by a third review author (LZ).
2.3.4. Data Synthesis and Analysis
RevMan 5.3 software was used to conduct the statistical analysis. Studies were classified and combined in the analysis according to different comparisons. To assess the heterogeneity across the studies, we searched for overlapping confidence intervals (CI) in forest plots and used the χ 2 test for statistical heterogeneity and the value of the I 2 statistic (I 2 > 50% showed the existence of heterogeneity). There was no significant heterogeneity in each group, so meta-analyses were all conducted with fixed-effect models in this review. For dichotomous data, we combined the risk ratios (RRs) of each study and calculated the 95% CI with the fixed-effect model. For continuous data, we combined the mean differences (MDs) of each study and calculated the 95% CI according to the outcome measurement. Publication bias was not explored via a funnel-plot analysis as the number of included studies in each group was less than 10.
3. Results
3.1. Characteristics of Included Studies and Literature Search Findings
The initial search identified 760 studies, of which 150 full text articles were screened, and a final total of 7 RCTs were included in this review [29, 32–34, 36–38]. All of the 7 RCTs were reported in Chinese and conducted in China.
Five studies compared acupuncture with Western medicine. Among them, two compared acupuncture with haloperidol [29, 36], one compared acupuncture with risperidone [32], and one compared acupuncture with tiapride [33]. Another one [34] compared acupuncture plus psychological behaviour therapy with haloperidol plus psychological behaviour therapy, which was regarded as comparison between acupuncture and haloperidol.
Two studies estimated the effect of acupuncture as an adjuvant therapy of Western medicine. One compared acupuncture plus haloperidol versus haloperidol alone [37], and the other one compared acupuncture plus haloperidol and psychological therapy versus haloperidol and psychological therapy [38]. The second study [38] was regarded as “comparing acupuncture plus haloperidol versus haloperidol alone” and was meta-analysed with the first study mentioned above [37].
The 7 RCTs included a total of 564 patients, with sample size ranging from 45 to 120. The age of the participants ranged from 2 to 21 years. All of the participants met the diagnostic criteria. The treatment duration ranged from 20 days to 3 months. In these studies, the acupoints that were commonly used were Baihui (GV20) (6/7), Fengchi (GB20) (5/7), Taiyang (EX-HN5) (5/7), Hegu (LI4) (4/7), Shenmen (HT7) (4/7), and Yintang (EX-HN3) (3/7). The most frequently used treatment methods were manual acupuncture (3/7) and electroacupuncture (3/7). The commonly used treatment frequency was once a day (6/7). The characteristics of included studies are listed in Table 2.
Table 2.
Summary of characteristics of included studies.
| Reference | Comparisons | Drug dose | Age (years) |
Duration of illness (years) |
YGTSS | Outcomes | Duration of intervention | Duration of follow-up |
|---|---|---|---|---|---|---|---|---|
| Guo et al., 2004 [36] | Electroacupuncture (n = 68) | 1.5–8 mg/d | NR | 1 to 8 in two groups | NR | Response rate | 30 days (30 sessions) |
No follow-up |
| Haloperidol (n = 34) | ||||||||
|
| ||||||||
| Liu et al., 2010 [30] | Electroacupuncture (n = 30) | 1.5–8 mg/d | NR | 1 to 5 | NR | Response rate | 20 days (20 sessions) |
No follow-up |
| Haloperidol (n = 30) | 1 to 5 | |||||||
|
| ||||||||
| Xu and Zhu, 2009 [33] | Scalp acupuncture (n = 30) | 0.25–1 mg/d | 6 to 18 | 1 to 7 | 30.07 ± 2.76 | YGTSS, response rate | 3 months (39 sessions) |
No follow-up |
| Risperidone (n = 30) | 4 to 17 | 1 to 8 | 35.03 ± 3.46 | |||||
|
| ||||||||
| Zhang et al., 2015 [34] | Manual acupuncture (n = 44) | 150–450 mg/d | 2 to 15 in two groups | 0.5 to 3.2 in two groups | NR | Response rate | 3 months (60 sessions) |
No follow-up |
| Tiapride (n = 43) | ||||||||
|
| ||||||||
| Mu et al., 2009 [35] | Electroacupuncture plus psychological behaviour therapy (n = 60) | From 1 mg/d | 10.24 ± 3.41 | 2.15 ± 1.07 | 33.61 ± 5.76 | YGTSS, response rate | 6 weeks (42 sessions) |
No follow-up |
| Haloperidol plus psychological behaviour therapy (n = 60) | 9.53 ± 2.75 | 2.48 ± 1.55 | 31.08 ± 6.54 | |||||
|
| ||||||||
| Chi and Sun, 2004 [37] | Manual acupuncture plus haloperidol (n = 24) | 1.5–8 mg | 2 to 21 | 1 to 9 | 39.875 ± 15.875 | YGTSS, response rate | 20 days (20 sessions) |
No follow-up |
| Haloperidol (n = 21) | 2 to 21 | 1 to 9 | 40.190 ± 15.863 | |||||
|
| ||||||||
| Yang et al., 2007 [38] | Manual acupuncture plus haloperidol and psychotherapy (n = 60 initially; final n = 56) | From 1 mg/d | 11.52 ± 2.96 | NR | 34.26 ± 5.88 | YGTSS, response rate | 40 days (40 sessions) |
No follow-up |
| Haloperidol and psychotherapy (n = 30) | 12.03 ± 3.37 | 36.01 ± 6.73 | ||||||
YGTSS: Yale Global Tic Severity Scale. NR: no reported.
3.2. Risks of Bias in Included Studies
All of the included RCTs mentioned randomisation; six RCTs used a random number table, the other RCT did not report the method of randomisation and we were unable to contact the authors [32]. The details of allocation concealment and blinding of outcome assessors were unclear in all studies. Blinding of participants was not done in any of the studies because of the characteristics of acupuncture. One RCT reported incomplete outcome data but did not conduct an intention to treat (ITT) analysis [38]. Neither RCT reported follow-up. The risks of bias assessments are presented in Table 3.
Table 3.
Risk of bias assessment of included studies.
| Bias | Guo et al., 2004 [36] | Liu et al., 2010 [30] | Xu and Zhu, 2009 [33] | Zhang et al., 2015 [34] | Mu et al., 2009 [35] | Chi and Sun, 2004 [37] | Yang et al., 2007 [38] |
|---|---|---|---|---|---|---|---|
| Random sequence generation (selection bias) |
Random number table (LR) |
Random number table (LR) |
NR (UR) |
Random number table (LR) |
Random number table (LR) |
Random number table (LR) |
Random number table (LR) |
|
| |||||||
| Allocation concealment (selection bias) |
UR | UR | UR | UR | UR | UR | UR |
|
| |||||||
| Blinding of participants and personnel (performance bias) | HR | HR | HR | HR | HR | HR | HR |
|
| |||||||
| Blinding of outcome assessment (detection bias) |
UR | UR | UR | UR | UR | UR | UR |
|
| |||||||
| Incomplete outcome data (attrition bias) |
LR | LR | LR | LR | LR | LR | LR |
|
| |||||||
| Selective reporting (reporting bias) | UR | UR | UR | UR | UR | UR | UR |
|
| |||||||
| Other bias | LR | LR | LR | LR | LR | LR | LR |
UR: unclear risk; LR: low risk; HR: high risk; NR: no reported.
3.3. Effects of Intervention
The 7 included RCTs were divided into two parts to conduct the meta-analysis according to different types of comparisons.
3.4. Acupuncture versus Western Medicine
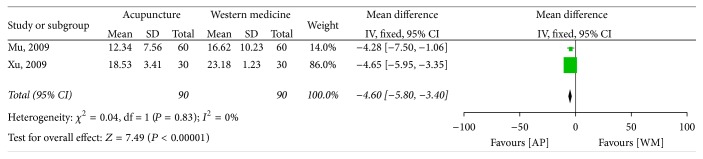
3.4.1. Yale Global Tic Severity Scale
In the five studies which compared acupuncture with Western medicine, only two RCTs used the YGTSS as an outcome measure, and they were pooled together [32, 34]. The MD was −4.60 (95% CI −5.80 to −3.40) using the fixed model, and there was a statistically significant difference between the effects of acupuncture and Western medicine (Figure 2).
Figure 2.
Forest plot of the effect of acupuncture versus Western medicine on the Yale Global Tic Severity Scale. AP: acupuncture; WM: Western medicine.
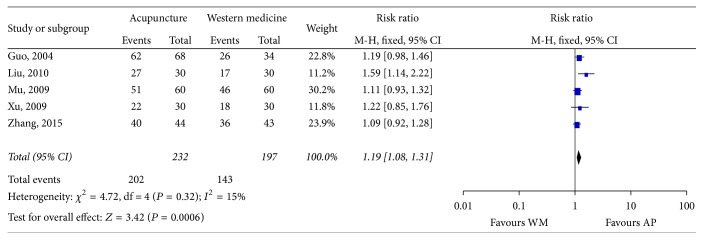
3.4.2. Response Rate
Five studies [29, 32–34, 36] reported response rate here with the RR as 1.19 (95% CI 1.08 to 1.31), which showed that there was a statistically significant difference between the effects of acupuncture and Western medicine (Figure 3).
Figure 3.
Forest plot of the effect of acupuncture versus Western medicine on response rate. AP: acupuncture; WM: Western medicine.
3.5. Acupuncture plus Western Medicine versus Western Medicine Alone
Two studies were included in this group. In one study [38], 60 participants were initially randomised into the acupuncture group, but only 56 finished the treatment. We did an ITT analysis on the “response rate” as a dichotomous outcome but not for the YGTSS because of a lack of original data for the missing four participants.
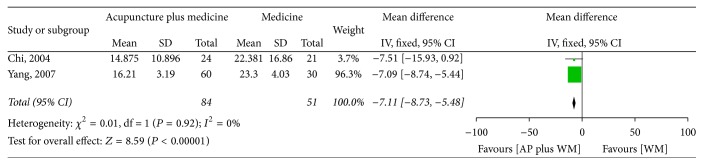
3.5.1. Yale Global Tic Severity Scale
Two RCTs were pooled together [37, 38]. The MD was −7.11 (95% CI −8.73 to −5.48) using the fixed model, and there was a statistically significant difference between the effects of acupuncture plus Western medicine and Western medicine alone (Figure 4).
Figure 4.
Forest plot of the effect of acupuncture plus Western medicine versus Western medicine alone on the Yale Global Tic Severity Scale. AP: acupuncture; WM: Western medicine.
3.5.2. Response Rate
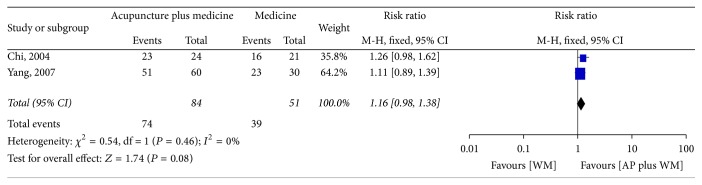
In this group, two studies were pooled together [37, 38]. The RR was 1.16 (95% CI 0.98 to 1.38) using the fixed model, from which we could not make a conclusion whether acupuncture plus Western medicine had better effect than Western medicine alone (Figure 5).
Figure 5.
Forest plot of the effect of acupuncture plus Western medicine versus Western medicine alone on response rate. AP: acupuncture; WM: Western medicine.
3.6. Follow-Up
No study reported follow-up after treatment.
3.7. Safety
One RCT reported no adverse reactions in the acupuncture group [29], and another RCT reported no adverse reactions in the 56 participants in the acupuncture plus haloperidol and psychotherapy group [38]. The other five included RCTs did not report whether there were adverse reactions in participants.
4. Discussion
4.1. Summary of Main Findings
Despite an extensive literature search, only 7 studies involving a total of 564 patients were eligible for our review. The result of meta-analysis indicated that, compared with Western medicine, acupuncture seemed to be more effective in improving the YGTSS (MD −4.60, 95% CI −5.80 to −3.40) and in response rate 1.19 (95% CI 1.08 to 1.31). Data from two studies showed that acupuncture as an adjuvant therapy enhanced the effect of Western medicine (MD −7.11, 95% CI −8.74 to −5.47) in improving the YGTSS, while it is inconclusive whether acupuncture could improve the response rate of Western medicine (RR 1.16, 95% CI 0.98 to 1.38). There was no report on follow-up of acupuncture on TS. Acupuncture seems to be associated with no adverse reactions, but the evidence is limited.
4.2. Applicability of Evidence
There were methodological limitations of included studies as no study reported the allocation concealment, which led to unclear selection bias. No study used participants and personnel blinding which led to high performance, and there was no report on assessment blinding which led to unclear detection bias. One study reported 4/90 (<5%) patients fell off and other studies reported that all patients finished the assessment. No protocol was published before outcome carried out, which led to unclear reporting bias in all studies. All studies were conducted in China, which made it unclear whether the conclusion of this review is fit for other races. Methodological weaknesses in the studies might have exaggerated the treatment effects of acupuncture.
Haloperidol and risperidone are both effective medicines recommended by the ESSTS. The effect of acupuncture may be better than these medicines, which may indicate that acupuncture may have clinical application value. However, we do not know clearly about the design of the included studies, such as superiority test and noninferiority test, and there is also a lack of sample size calculations in some studies. No study used placebo/sham acupuncture as a comparison, and therefore it is unclear whether acupuncture has a specific biological treatment effect.
4.3. Difference from Other Reviews
Six studies [36, 40, 43–46] published from 2001 to 2009 were included in the published Chinese review [18]. Among them, five [40, 43–46] were excluded and one [36] was included in our review. Of the excluded studies, one study was a quasi-randomised study that allocated treatment by patient number [43], two studies used false randomisation [44, 45], one study used incorrect outcome measure, and another study [46] was duplication of one study [39] that was included in our review. There are other differences between these two reviews explained as follows. First, one study included in the published Chinese review compared acupuncture plus point injection with medication [43], which makes it impossible to tell whether the treatment effect was produced by acupuncture or the injected medicine. In our review, acupuncture combined with other methods (e.g., acupressure, acupoint injection, and moxibustion) were all excluded. Second, the published Chinese review was published in Chinese; our review was written in English. Finally, the published Chinese review indicated that acupuncture had a better effect than conventional Western medicine on response rate but caused no difference in YGTSS evaluation. In our review, we found that acupuncture seemed to be more effective than Western medicine and seemed to be an effective method as an adjuvant therapy of Western medicine in YGTSS evaluation, and we also found that acupuncture may have a better effect than Western medicine in response rate, but the evidence is limited.
4.4. Mechanism and Limitations of Acupuncture on TS
Although acupuncture was widely used in TS treating in China, there is only one study [14] researched on the mechanism of acupuncture for TS by now. It reported acupuncture may regulate the abnormal brain function of patients with tic disorder using single photon emission computed tomography (SPECT). Acupuncture also has limitations in treating TS children. Maintaining a fixed position during conventional acupuncture is difficult for children, and the pain produced during conventional acupuncture treatment leads to poor compliance. Suitable acupuncture method is more feasible for TS children, such as plum-blossom needle therapy and acupoint embedding. Researches on mechanism of acupuncture for TS are also urgently needed.
4.5. Limitations of This Review
There are some limitations to this review. First, the size of included studies is small. Second, only Chinese and English databases were searched, so some relevant studies published in other languages might have been missed. Third, despite the difference among different acupuncture methods in this review (such as manual acupuncture, electroacupuncture, and scalp acupuncture), we still combined them together because of small number of studies of each acupuncture type. But this combination will make us unclear about the effect of each acupuncture type. Deeper subgroup analysis can be done when the number of studies is enough. Finally, some useful outcome measures have not been used in included studies. For example, “quality of life” is a good outcome measure that was not reported in any included study.
5. Conclusion
Based on the present findings, we cautiously suggest that acupuncture may have better short-term effect than Western medicine for TS in alleviating the symptoms and that acupuncture may be an effective adjuvant therapy in improving the effect of Western medicine on TS. However, the evidence is limited. There is a need for large-scale and well-designed RCTs of acupuncture for TS with rigorous methods of randomisation, blinding, and adequately concealed allocation, as well as validated outcome measures. All information including adverse effects should be reported in detail, according to both CONSORT [47] and CONSORT for acupuncture [48].
Acknowledgments
This systematic review was financially supported by a fund from the National TCM Clinical Research Demonstration Base of Guang'anmen Hospital, China Academy of Chinese Medical Sciences (no. 2014S298).
Abbreviations
- CI:
Confidence intervals
- ESSTS:
European Society for the Study of Tourette Syndrome
- ITT:
Intention to treat
- MD:
Mean difference
- RCT:
Randomised controlled trial
- STSSS:
Shapiro Tourette Syndrome Severity Scale
- TS:
Tourette syndrome
- YGTSS:
Yale Global Tic Severity Scale.
Ethical Approval
Ethical approval was not necessary as the data used in this systematic review did not include individual patient data.
Disclosure
The findings of this study will be disseminated through peer-reviewed publications and national and international conferences.
Competing Interests
There was no funding from any commercial agency, so the authors declare they have no competing interests.
Authors' Contributions
Jinna Yu contributed to the conception, design, and writing of the review. Yongming Ye contributed to data collection and data analysis. Jun Liu contributed to data collection and data analysis. Yang Wang contributed to amending the review. Weina Peng contributed to amending the review. Zhishun Liu contributed to the conception, design, and amendment of this review. All authors read and approved the final manuscript.
References
- 1.Diagnostic and Statistical Manual of Mental Disorders: DSM-IV-TR. Washington, DC, USA: American Psychiatric Association; 2000. [Google Scholar]
- 2.Cath D. C., Hedderly T., Ludolph A. G., et al. European clinical guidelines for Tourette syndrome and other tic disorders. Part I: assessment. European Child & Adolescent Psychiatry. 2011;20(4):155–171. doi: 10.1007/s00787-011-0164-6. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Scharf J. M., Miller L. L., Gauvin C. A., Alabiso J., Mathews C. A., Ben-Shlomo Y. Population prevalence of Tourette syndrome: a systematic review and meta-analysis. Movement Disorders. 2015;30(2):221–228. doi: 10.1002/mds.26089. [DOI] [PubMed] [Google Scholar]
- 4.Stern J. Tourette syndrome. Paediatrics and Child Health. 2014;24(10):447–451. doi: 10.1016/j.paed.2014.03.003. [DOI] [Google Scholar]
- 5.Bloch M. H., Leckman J. F. Clinical course of Tourette syndrome. Journal of Psychosomatic Research. 2009;67(6):497–501. doi: 10.1016/j.jpsychores.2009.09.002. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Roessner V., Plessen K. J., Rothenberger A., et al. European clinical guidelines for Tourette syndrome and other tic disorders. Part II: pharmacological treatment. European Child & Adolescent Psychiatry. 2011;20(4):173–196. doi: 10.1007/s00787-011-0163-7. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Verdellen C., van de Griendt J., Hartmann A., Murphy T. European clinical guidelines for Tourette Syndrome and other tic disorders. Part III: behavioural and psychosocial interventions. European Child & Adolescent Psychiatry. 2011;20(4):197–207. doi: 10.1007/s00787-011-0167-3. [DOI] [PubMed] [Google Scholar]
- 8.Müller-Vahl K. R. The benzamides tiapride, sulpiride, and amisulpride in treatment for Tourette's syndrome. Der Nervenarzt. 2007;78(3):264–271. doi: 10.1007/s00115-006-2131-x. [DOI] [PubMed] [Google Scholar]
- 9.Waldon K., Hill J., Termine C., Balottin U., Cavanna A. E. Trials of pharmacological interventions for Tourette Syndrome: a systematic review. Behavioural Neurology. 2013;26(4):265–273. doi: 10.3233/ben-2012-120269. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Huys D., Hardenacke K., Poppe P., Bartsch C., Baskin B., Kuhn J. Update on the role of antipsychotics in the treatment of Tourette syndrome. Neuropsychiatric Disease and Treatment. 2012;8:95–104. doi: 10.2147/ndt.s12990. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Kompoliti K., Fan W., Leurgans S. Complementary and alternative medicine use in Gilles de la Tourette syndrome. Movement Disorders. 2009;24(13):2015–2019. doi: 10.1002/mds.22724. [DOI] [PubMed] [Google Scholar]
- 12.Mantel B. J., Meyers A., Tran Q. Y., Rogers S., Jacobson J. S. Nutritional supplements and complementary/alternative medicine in Tourette syndrome. Journal of Child and Adolescent Psychopharmacology. 2004;14(4):582–589. doi: 10.1089/cap.2004.14.582. [DOI] [PubMed] [Google Scholar]
- 13.Fields A. Ancient Chinese surgery: acupuncture. California Medicine. 1947;67(1, article 39) [PMC free article] [PubMed] [Google Scholar]
- 14.Jia S., Xu W., Gao Z., Shi J., Ou Y., Xie X. SPECT research on acupuncture for 36 cases with tic disorders. Proceedings of the National Symposium on Nuclear Medicine and Neuroscience; 2007; Chinese Society of Nuclear Medicine; pp. 75–76. [Google Scholar]
- 15.Zhu B., Shan Y. Clinical observation on treatment of Tourette Syndrome by different acupuncture methods. Journal of Acupuncture and Moxibustion. 2008;27(12):17–18. [Google Scholar]
- 16.Xiang S.-J., Cai Y.-H., Zhang Z.-D. Observation on therapeutic effect of tic disorders treated with local acupuncture. Chinese Acupuncture & Moxibustion. 2010;30(6):469–472. [PubMed] [Google Scholar]
- 17.Shi X., Wang Z., Jiang L., Ge Z. Therapeutic observation on acupuncture plus medication for tic disorders in children. Shanghai Journal of Acupuncture and Moxibustion. 2012;32(7):512–514. [Google Scholar]
- 18.Xiao L., Chen Y., Du Y., Gao X., Lin X., Sun P. Evaluation of clinical randomized control trials of acupuncture for treatment of multiple tics-coprolalia syndrome. Lishizhen Medicine and Medical Research. 2010;21(5):1199–1200. [Google Scholar]
- 19.Sun C. H. X. Standard on Curative Effect of Clinical Diseases. Beijing, China: People's Military Medical Press; 2002. [Google Scholar]
- 20.Zhu Y., Xu S.-f., Zhu B.-c. Observations on the efficacies of different needle retention modes of scalp acupuncture in treating multiple tics. Shanghai Journal of Acupuncture and Moxibustion. 2011;30(5):286–288. [Google Scholar]
- 21.Shang Y., Li B. Clinical study of scalp point penetration needling in treatment of children with tic disorder. Asia-Pacific Traditional Medicine. 2015;11(17):113–114. [Google Scholar]
- 22.Zhu Q., Xu N. Clinical research of Tourette's syndrome treatment by Jin's three needles therapy plus Chinese herba medicine [Ph.D. thesis] 2011. [Google Scholar]
- 23.Jiang L., Chen W. Clinical observation on treating tourrette syndrome by acupuncture plus auricular pressure. Clinical Journal of Chinese Medicine. 2015;7(26):1–3. [Google Scholar]
- 24.Shi X.-c., Wang Z.-x., Jiang L.-p., Ge Z.-z. Therapeutic observation on acupuncture plus medication for tic disorders in children. Shanghai Journal of Acupuncture and Moxibustion. 2012;31(7):512–514. [Google Scholar]
- 25.Sun Q., Zhenf Z.-Y. Clinical observation of tourette's syndrome qi depression transforming into fire type treated with acupuncture [M.S. thesis] 2015. [Google Scholar]
- 26.Zou W.-Q. Observation on efficacy of acupuncture combined with traditional Chinese medicine in treating children with Tourette syndrome. China Journal of Chinese Medicine. 2011;26(159):1018–1019. [Google Scholar]
- 27.Tang Y., Shang Q., Li W., Xu S. Clinical controlled trial on infantile Tourette syndrome treated with integrated therapy of acupuncture and medicine. Chinese Acupuncture & Moxibustion. 2015;35(2):141–144. [PubMed] [Google Scholar]
- 28.Wei X.-W., Li L., Pu X., Li Z., Yang M. Clinical study on acupuncture for children with tic disorder. Collection of Papers of the 30th Academic Conference of Pediatric Branch of the Chinese Society of Traditional Chinese Medicine, pp. 304-305, 2013.
- 29.Huang N., Yuan Q. The clinical research on treatment of tourette syndrome in children by acupuncture added chinese herbs [M.S. thesis] 2015. [Google Scholar]
- 30.Liu L., Yu X., Li X., Xu Y., Wang F., Qu B. Clinical observation on head electro-acupuncture for patients with Tourette Syndrome. Journal of Clinical Acupuncture and Moxibustion. 2010;26(10):21–22. [Google Scholar]
- 31.Sun Y., Nie X. Acupuncture on Baihui and points of distal extremities for Tourette Syndrome. Journal of Clinical Acupuncture and Moxibustion. 2014;30(3):29–30. [Google Scholar]
- 32.Zhang Z. Clinical efficacy of acupuncture with plum needle acupuncture in treating Tourette Syndrome. Chinese Journal of General Practice. 2009;7(12):1331–1332. [Google Scholar]
- 33.Xu S., Zhu B. Observation on the effect of dynamic needle retention mode of scalp acupuncture in treating Tourette Syndrome. Guiding Journal of Traditional Chinese Medicine and Pharmacy. 2009;15(6):58–59. [Google Scholar]
- 34.Zhang X., Wang X., Wei Y., Wu Y. Clinical research on acupuncture in dynamic needle rentention mode for multiple tics. Shandong Journal of Traditional Chinese Medicine. 2015;34(4):266–267. [Google Scholar]
- 35.Mu J., Cheng J., Ao J., Zhou L., Wang J., Fang W. Clinical observation on acupuncture combined with psychological therapy for 60 cases with Tourette's Syndrome. Jiangsu Journal of Traditional Chinese Medicine. 2009;41(2):49–51. [Google Scholar]
- 36.Guo W., Chi X., Sun Y. Clinical observation on head electro-acupuncture for 102 cases with Tourette Syndrome. Chinese Journal of Traditional Medical Science and Technology. 2004;11(6):p. 345. [Google Scholar]
- 37.Chi X., Sun Y. Clinical study on treatment of Tourette's Syndrome by combination of acupuncture and medicine [M.S. thesis] 2004. [Google Scholar]
- 38.Yang L., Wu J., Zhou X. Clinical observation on comprehensive rehabilitation therapy focus on acupuncture for Tourette's Syndrome. Chinese Journal of Rehabilitation Medicine. 2007;22(5):457–459. [Google Scholar]
- 39.Du G.-S. Observation on the curative effect of acupuncture on child Tourette's syndrome. Journal of Acupuncture and Tuina Science. 2007;5(5):294–296. doi: 10.1007/s11726-007-0294-z. [DOI] [Google Scholar]
- 40.Ma S., Liu X.-Y., Yu R.-L., Chen L.-J. Clinical observation on acupuncture for treatment of Tourette's syndrome. Chinese Acupuncture & Moxibustion. 2006;26(6):392–394. [PubMed] [Google Scholar]
- 41.Cavanna A. E., Schrag A., Morley D., et al. The Gilles de la Tourette syndrome-quality of life scale (GTS-QOL): development and validation. Neurology. 2008;71(18):1410–1416. doi: 10.1212/01.wnl.0000327890.02893.61. [DOI] [PubMed] [Google Scholar]
- 42.Wu H., Liu P., Meng H. Norm, reliability and validity of children and adolescents' QOL scale. Chinese Journal School Health. 2006;27(1):18–21. [Google Scholar]
- 43.Zhang H., Deng H. Observations on efficacy of acupuncture plus point injection for treatment of child twitch. Shanghai Journal of Acupuncture and Moxibustion. 2005;124(5):15–16. [Google Scholar]
- 44.Zhang Y. Acupuncture for Tourette syndrome. Chinese Acupuncture & Moxibustion. 2002;22(4):p. 222. [Google Scholar]
- 45.Shan Y., Yao W. Clinical observation on treatment of multiple Tourette's syndrome with scalp acupuncture. Chinese Acupuncture & Moxibustion. 2001;21(6):331–332. [Google Scholar]
- 46.Du G. Observations on the curative effect of acupuncture on child Tourette's syndrome. Shanghai Journal of Acupuncture and Moxibustion. 2007;26(3):5–6. [Google Scholar]
- 47.Moher D., Schulz K. F., Altman D. G. The CONSORT statement: revised recommendations for improving the quality of reports of parallel-group randomised trials. The Lancet. 2001;357(9263):1191–1194. doi: 10.1016/s0140-6736(00)04337-3. [DOI] [PubMed] [Google Scholar]
- 48.Hugh M., Altman D. G., Hammerschlag R., et al. Revised standards for reporting interventions in clinical trials of acupuncture (STRICTA): extending the CONSORT statement. Zhong Xi Yi Jie He Xue Bao. 2010;8(9):804–818. doi: 10.3736/jcim20100902. [DOI] [PubMed] [Google Scholar]