Abstract
Aim
The aim of the retrospective study was to develop a planning class solution for prostate intensity-modulated radiotherapy (IMRT) that achieved target and organs-at-risk (OAR) doses within acceptable departmental protocol criteria using the Monaco treatment planning system (Elekta-CMS Software, MO, USA).
Background
Advances in radiation therapy technology have led to a re-evaluation of work practices. Class solutions have the potential to produce highly conformal plans in a time-efficient manner.
Materials and Methods
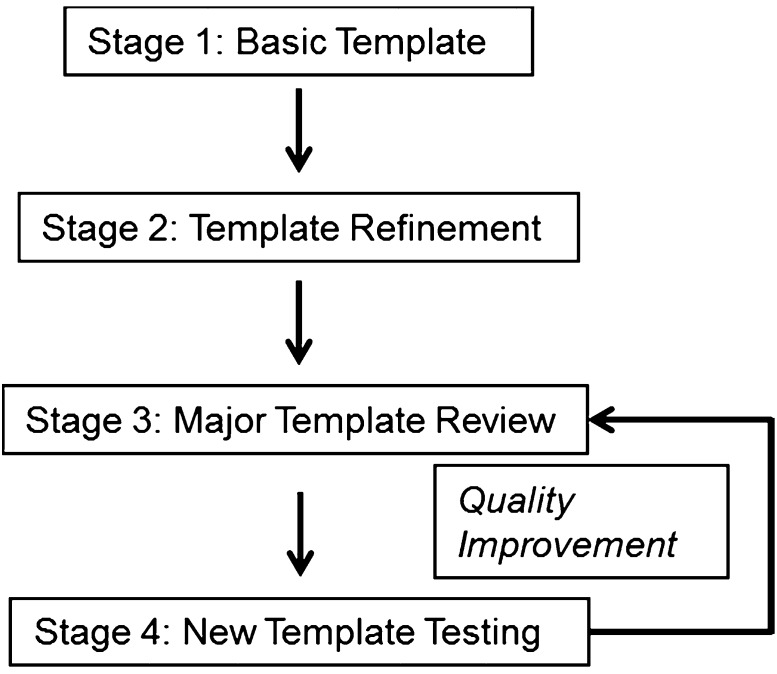
Using data from intermediate and high risk prostate cancer patients, a stepwise quality improvement model was employed. Stage 1 involved the development of a broadly based treatment template developed across 10 patients. Stage 2 involved template refinement and clinical audit (n = 20); Stage 3, template review (n = 50) and Stage 4 an assessment of a revised template against the actual treatment plan involving 72 patients.
Results
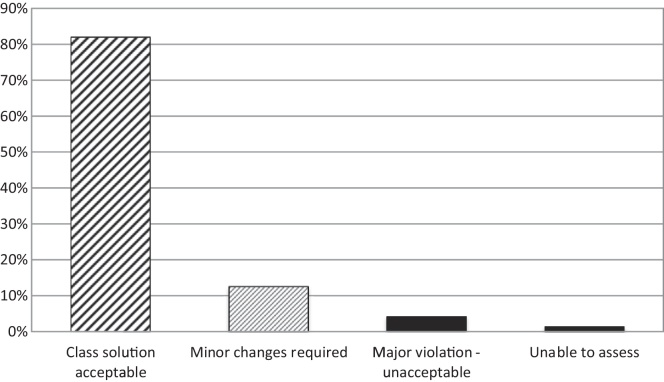
The computer algorithm that comprised the Stage 4 template met clinical treatment criteria for 82% of patients. Minor template changes were required for a further 13% of patients. Major changes were required in 4%; one patient could not be assessed. The average calculation time was 13 min and involved seven mouse clicks by the planner. Thus, the new template met treatment criteria or required only minor changes in 95% of prostate patients; this is an encouraging result suggesting improvements in planning efficiency and consistency.
Conclusion
It is feasible to develop a class solution for prostate IMRT using a stepwise quality improvement model which delivers clinically acceptable plans in the great majority of prostate cases.
Keywords: Computer assisted, Diagnostic imaging, Prostate, Radiotherapy planning
1. Introduction
Radiotherapy treatment protocols are widely used to streamline the planning process while promoting safety and consistency.1 Advances such as the introduction of intensity-modulated radiation therapy (IMRT) and better software tools have led to a re-evaluation of planning procedures and work practices. There is interest for example in protocols which are applicable to a wide range of cases – a class solution – while meeting local, national and international guidelines and treatment criteria. A class solution is often defined as a set of IMRT objective and penalty parameters and beam arrangements that are robust enough to produce a clinically acceptable dose distribution regardless of patient size, anatomy, target volumes and organs at risk (OAR).1 Class solutions have the potential to simplify the planning process and allow clinicians of all levels of experience to produce highly conformal plans in a time efficient manner.2
In the present report, we describe the development of a class solution for prostate cancer using IMRT and the Monaco planning system (Elekta-CMS Software, MO, USA). Prostate cancer is the most commonly diagnosed cancer in males in New South Wales, Australia (34%),3 with our institute treating around 250 patients a year with prostate IMRT. Development of a class solution for this common cancer, therefore, has the potential to significantly impact efficiencies in radiotherapy planning procedures and work practices, and also has the potential to achieve improvements in consistency and quality of planning.
2. Materials and methods
All patients in this retrospective study were planned with the Monaco planning system (Elekta-CMS Software, MO, USA) at our cancer Institute. The patient cohort comprised intermediate and high risk prostate cancer patients. These patients were volumed using magnetic resonance imaging (MRI) and computed tomography (CT) fusion4 and treated to 81 Gy as previously described.5, 6 Planning criteria and OAR constraints are summarised in Table 1, Table 2 and were based on evidence-based guidelines (EviQ recommendations).7
Table 1.
Acceptable plan criteria for prostate IMRT.
| PTV | CTV | |
|---|---|---|
| Ideal | D95 > 81 Gy D99 > 76.95 Gy |
D100 = 81 Gy |
| Mean Dose 81–84.24 Gy |
||
| Minor violation (acceptable) | D90 > 81 Gy or D98 > 76.95 Gy |
D99.0 > 81 Gy |
| Mean Dose 84.24–85.46 Gy |
Minor violation: allowable when organs at risk constraint cannot be met. Dx refers to the dose that covers X percent of the structure. The prescribed dose was 81 Gy. Gy: Grey.
Table 2.
Organ at risk constraints for prostate IMRT.
| Organ at risk | Ideal constraint | Minor violation |
|---|---|---|
| Rectum, sigmoid | V40Gy < 35% V65Gy < 17% V75Gy < 10% Max Dose 2cc < 102.5% |
V40Gy < 45% V65Gy < 21% V75Gy < 15% |
| Small bowel | Single phase max dose 70 Gy 100cc < 45 Gy |
Refer to RO |
| Bladder | V40Gy < 60% V50Gy < 50% V60Gy < 40% |
V50 Gy between 50–60% |
| Femoral heads | V35Gy < 100% V45Gy < 60% V60Gy < 30% |
|
| Penile bulb | V50Gy < 95% |
Minor violations were acceptable when all reasonable efforts to achieve ideal constraints had been made. PD: prescribed dose. Gy: Grey. Vx refers to the percentage volume of a structure receiving XGy.
The study employed a stepwise quality improvement model to develop a class solution template for prostate IMRT (Fig. 1). Our aim was to develop a class solution that worked for the majority of cases and which did not require the planner to make edits. We also ensured that the processes involved were consistent with our conformity to the planning procedures of the national radiation oncology practice standards.8 In brief, Stage 1 involved the development of a broadly based template based on a number of templates developed across 10 patients. The Stage 1 template offered a significant improvement in quality and also planning efficiency as compared to the earlier XiO planning system. Plans were tested by physicists to ensure they would pass quality assurance and delivery was timed to ensure no additional time was added to treatment. This template was rolled out across the three sites of our institute.
Fig. 1.
Stepwise quality improvement model for the development of a class solution for prostate IMRT.
Stage 2 involved a phase of template refinement. Information was gathered from the Monaco team members who were planning the cases and their feedback was used to develop a series of templates which were compared across 10 patients. The best-performing template was adopted and rolled out for use across the three sites. It was requested that radiotherapy staff log the cases where the template failed to meet protocol criteria and the steps taken to address the issue(s).
An audit of the Stage 2 template was undertaken on 20 patients at two centres using sensitivity analysis (Table 3). In this analysis, minor changes comprised changes to the values in the cost functions; major changes added new cost functions. The Stage 2 template met protocol criteria (no changes or only minor changes required) in 70% of cases.
Table 3.
Stage 2 Template audit (n = 20).
| Changes required to meet protocol criteria | [Site 1] (n = 12) | [Site 2] (n = 8) | Combined (%) |
|---|---|---|---|
| None | 2 | 0 | 10% |
| Minor | 6 | 6 | 60% |
| Major | 4 | 2 | 30% |
These results, while encouraging, suggested that further refinement would be necessary to meet the requirements of a class solution for prostate cancer. Therefore, Stage 3 involved a major review of treated plans across a larger number of cases (n = 50) and across the three sites. Data including dose constraints achieved as per protocol, all cost functions, sequencing parameters used, resultant monitor units (MU) and segments (for treatment time analysis) were collected from the treated plans and entered into a spreadsheet for analysis. The information was used to inform the development of a new template via careful analysis of which cost functions and their values resulted in the best dosimetric outcome. A trend became evident and these cost functions and values were used for the new class solution template.
The final stage, Stage 4, involved the application of the new template (computer algorithm) in 72 consecutive patients across three sites. For each plan the template was run as a batch optimisation and then reviewed to see if the template met treatment criteria. Plans that met all constraints (ideal) or with only minor violations were considered acceptable for treatment. Those with major violations were considered unacceptable.
3. Results
The stepwise quality improvement process for a class solution resulted in the development of a ‘new template’ for prostate IMRT. As summarised in Fig. 2, treatment criteria were satisfied for 82% of patients; of these, three patients required a minor rescale and were counted as meeting the criteria. Minor template changes were required for a further 13% of patients (e.g. changing the control points to 120 and/or increasing the root mean square {RMS} in the PTV quadratic overdose {QOD} to 0.25). Major changes were required in 4% of patients; these were often patients where PTV was significantly wrapping around the rectum and rectum was small. One patient could not be reached for assessment (1%).
Fig. 2.
Stage 4: Application of new template for a class solution for prostate cancer (n = 72).
The time taken to run the new class solution (computer algorithm) was calculated. An average of 13 min calculation time was needed for planning, and applying the class solution involved a total of seven clicks of the computer mouse by the treatment planner.
4. Discussion
In general terms, the benefits of a class solution include consistency in quality of plans, improvements in efficiency in planning and improvements in efficiency in treatment delivery times. In this study, the new template met treatment criteria or required only minor changes in 95% of prostate patients; this is an encouraging result suggesting improvements in planning efficiency and consistency. This is particularly important for smaller rural and regional centres that may have more limited resources than larger metropolitan centres, yet are attempting to achieve equivalent quality.9
The suitability of class solutions for prostate radiotherapy protocols has been considered by others.5, 10, 11, 12, 13, 14 Neill14 investigated the implementation of a modified class solution for intact prostate IMRT in 10 patients and concluded that a modified class solution provided a good starting point for planning radiotherapy. Coburn et al.1 differentiated between flexible protocols – where the radiation therapist could adapt or tailor the treatment plan using a wide range of beam and dose parameters – and rigid protocols (class solution) – where the radiation beam and dose parameters are set – and found that while flexible protocols took longer than rigid protocols (142 min vs. 83 min), more of the flexible plans were acceptable without modification (58% vs. 40%). It is worth pointing out that we have used a strategy similar to that suggested by these authors, namely, that we sought to develop a class solution for prostate IMRT which allowed some flexibility to make minor modifications should the template not meet the treatment criteria. The allowed modifications were listed in a set of guidelines. We feel that that is a pragmatic solution with benefits for both radiotherapy planners and patients.
During the course of this study a number of hurdles were encountered. Ongoing developments in radiotherapy planning (such as moving from step-and-shoot to multi-leaf collimator (dMLC) and upgrades to the Monaco planning system) have necessitated re-evaluations of the template to assess the impact of unintentional changes to standard procedures. In addition, radiation oncologists – who could see potential benefits of a class solution – were pressing for further tightening of treatment criteria, for example, to reduce dose to OAR. These retrospective planning and trialling evaluations were necessary but time-consuming and have contributed to another hurdle: getting planning staff on board to use the templates. In the midst of this, radiation oncologists, radiation therapists and medical physicists were applying their own pressure to develop class solutions for additional anatomical sites. Sites in the planning stage include anal, post-prostatectomy, gynaecological and brain.
Additional improvements in the class solution have been made recently and an independent group has provided dosimetric evaluation of the results using a quality metrix programme. This final stage of the class solution demonstrated that 89% of prostate patients met treatment criteria outright (S. Greenham, personal communication). Further research is required to determine whether prostate class solutions can maintain or improve upon the clinical and patient-reported outcomes5, 6, 15 of dose-escalated image-guided IMRT.
5. Conclusion
This study has demonstrated that it is feasible to develop a class solution for prostate IMRT using a stepwise quality improvement model. Planning was achieved with seven clicks of the computer mouse and an average of 13 min calculation time. Moreover, the class solution met treatment criteria outright in 82% of prostate patients and required only minor changes in a further 13% – a satisfactory result. A dosimetric study using specialist evaluation software and involving a larger group of patients is necessary to further evaluate the template on a prospective basis.
Conflict of interest
None declared.
Financial disclosure
None declared.
Acknowledgements
We acknowledge the contributions of the Prostate IMRT Workgroup, the Monaco Workgroup and the Plan IQ™ Workgroup during the development of the class solution.
References
- 1.Coburn N., Beldham-Collins R., Westling J., Trovato J., Gebski V. Evaluation of flexible and rigid (class solution) radiation therapy conformal prostate planning protocols. Med Dosim. 2012;37:5–8. doi: 10.1016/j.meddos.2010.12.004. [DOI] [PubMed] [Google Scholar]
- 2.Likhacheva A., Palmer M., Du W., Brown P.D., Mahajan A. Intensity modulated radiation therapy class solutions in Philips Pinnacle treatment planning for central nervous system malignancies: standardized, efficient, and effective. Pract Radiat Oncol. 2012;2:e145–e153. doi: 10.1016/j.prro.2012.03.010. [DOI] [PubMed] [Google Scholar]
- 3.Currow D., Thomson W. Cancer Institute NSW; Sydney: 2014. Cancer in NSW: incidence report 2009. February. [Google Scholar]
- 4.Horsley P.J., Aherne N.J., Edwards G.V. Planning magnetic resonance imaging for intensity-modulated radiotherapy: impact on target volumes, radiotherapy dose, and androgen deprivation administration. Asia Pac J Clin Oncol. 2015;11:15–21. doi: 10.1111/ajco.12266. [DOI] [PubMed] [Google Scholar]
- 5.Wilcox S.W., Aherne N.J., Benjamin L.C. Long-term outcomes from dose-escalated, image-guided IMRT with androgen deprivation: encouraging results for intermediate- and high-risk prostate cancer. Onco Targets Ther. 2014;7:1519–1523. doi: 10.2147/OTT.S65238. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Wilcox S.W., Aherne N.J., Benjamin L.C. Is modern external beam radiotherapy with androgen deprivation therapy still a viable alternative in an era of robotic surgery and brachytherapy: a comparison of Australian Series. J Med Imag Radiat Oncol. 2015;59:125–133. doi: 10.1111/1754-9485.12275. [DOI] [PubMed] [Google Scholar]
- 7.EviQ Cancer Treatments Online . 2011. Radiation oncology, prostate, intermediate risk, EBRT, definitive. March. [Google Scholar]
- 8.Manley S., Last A.J., Fu K., Shakespeare T.P. Regional cancer centres demonstrate voluntary conformity with the national radiation oncology practice standards. J Med Radiat Sci. 2015;62:152–159. doi: 10.1002/jmrs.102. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Shakespeare T.P., Turner M., Chapman A. Is rural radiation oncology practice quality as good as the big smoke? Results of the Australian Radiotherapy Single Machine Unit Trial. Austral Radiol. 2007;51:381–385. doi: 10.1111/j.1440-1673.2007.01754.x. [DOI] [PubMed] [Google Scholar]
- 10.Khoo V.S., Bedford J.L., Webb S., Dearnaley D.P. Class solutions for conformal external beam prostate radiotherapy. Int J Radiat Oncol Biol Phys. 2003;55:1109–1120. doi: 10.1016/s0360-3016(02)04393-6. [DOI] [PubMed] [Google Scholar]
- 11.Schreibmann E., Xing L. Feasibility study of beam orientation class-solutions for prostate IMRT. Med Phys. 2004;31:2863–2870. doi: 10.1118/1.1797571. [DOI] [PubMed] [Google Scholar]
- 12.Rodrigues G., Yartsev S., Chen J. A comparison of prostate IMRT and helical tomotherapy class solutions. Radiother Oncol. 2006;80:374–377. doi: 10.1016/j.radonc.2006.07.005. [DOI] [PubMed] [Google Scholar]
- 13.Xhaferllari I., Wong E., Bzdusek K., Lock M., Chen J. Automated IMRT planning with regional optimization using planning scripts. J Appl Clin Med Phys. 2013;14:4052. doi: 10.1120/jacmp.v14i1.4052. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Neill C.J. Dosimetric comparison of intensity-modulated solutions for intact prostate cancer. Med Dosim. 2014;39:366–372. doi: 10.1016/j.meddos.2014.06.006. [DOI] [PubMed] [Google Scholar]
- 15.Steer A., Aherne N., Shakespeare T.P. Decision regret in men undergoing dose escalated radiotherapy for prostate cancer. Int J Radiat Oncol Biol Phys. 2013;86:16–20. doi: 10.1016/j.ijrobp.2013.03.006. [DOI] [PubMed] [Google Scholar]