Abstract
Aim
The aim of this clinical paper is to introduce a technique to plan for functional maxillofacial reconstructions.
Materials and Methods
Preoperative dental casts were made of the patient and mock surgery performed on the casts. A fibula analogue was then placed in an ideal functional reconstruction position. New dentures were fabricated on the fibula analogue and drill holes for the placement of implants were placed through the denture. This denture formed as a guide to position the fibula transplant during surgery.
Results
This technique was useful in producing functional and rehabilitative outcomes in cases of both maxillary and mandibular reconstructive surgeries.
Conclusion
The Jugaad technique—denture based inverse planning—is a cost effective method for planning and executing maxillofacial reconstructions using mock surgery on casts and interim dentures.
Keywords: Mandibular reconstruction, Free fibula flap, Oral rehabilitation, Oral Implantology, Quality of Life
Introduction
In patients who undergo large ablative surgeries of the jaws, reconstruction is done using vascularized bone containing free flaps. The ultimate goal of maxillofacial reconstructive surgery is to improve functional, esthetic and quality of life outcomes. Implant supported dental rehabilitation improves the oral health related quality of life in patients with reconstructed jaws [1]. Among various donor-site options, the free fibula flap is the method of choice for mandibular reconstructions. However, the fibula bone is a relatively straight bone, the anatomy of which differs considerably from the native mandible.
It is clinically challenging and time consuming to osteotomize the straight fibula flap into the shape of the mandible. Additionally, the alveolus of the mandible (responsible for the functioning of housing the teeth) is in a different sagittal/transverse position as compared to the basal bone of the mandible (that is responsible for esthetic outcomes) [2]. In these complex cases, failure to incorporate this aspect while performing the reconstructive surgery often produces postoperative results that would make oral rehabilitation extremely difficult or impossible.
At present, to solve this issue and obtain predictable outcomes, image guided planning software as well as the use of STL models have been proposed to achieve excellent functional outcomes [3]. However, due to the cost involved, it becomes impractical to apply these techniques in all situations, especially in developing countries like India, where there is no insurance that will cover planning for reconstructive surgery [4]. Hence, it is of importance to innovate cost effective methods to plan for reconstruction.
The aim of this technical note is to introduce the “Jugaad technique”, a cost effective method for planning and executing maxillofacial reconstructions using mock surgery on casts and interim dentures.
Description of the Technique
Preoperative Planning
Upper and lower impressions are taken and two sets of casts are poured. Jaw relations are recorded and transferred. Mock surgical resection is carried out on the cast corresponding as much as possible to the surgical plan. A preformed triangular bar with width of approximately 1.2 cm is made that acts as an analogue to the fibula. This bone is then placed in relation to the cast that would provide a good base for the support of dental rehabilitation. The fibula analog is attached onto the altered cast in the desired position using multiple layers of sticky wax or putty. A wax-up of the denture is created with the fibula analogue as the base and teeth arrangement done (Figs. 1, 2).
Fig. 1.
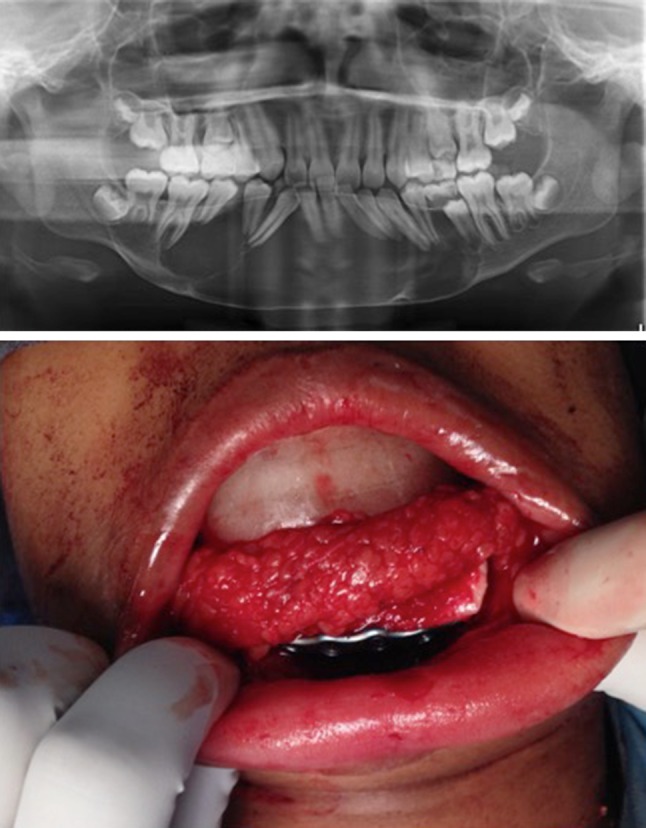
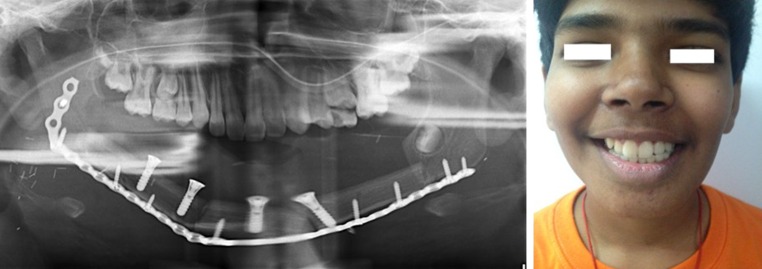
Top Preoperative panoramic radiograph showing a patient with an osteolytic lesion involving the mandible. Bottom Intraoperative stent in place with the fibula flap conforming to the intra operative stent
Fig. 2.
Left Immediate postoperative panoramic radiograph showing functional reconstruction with implants in the ideal position. Right 6-month postoperative clinical profile picture showing functional reconstruction
Care is taken to provide about 2–3 mm of relief under the denture to accommodate for the soft tissue thickness. If a skin paddle is planned that would replace the intra-oral lining, a larger relief is provided. As it is difficult to predict the soft tissue outcomes immediately post reconstruction, the soft tissue flange extensions are kept minimal.
Once the wax-up denture seems to be arranged in a functionally ideal position, it is then acrylized. The acrylized denture is then reintroduced onto the mounted altered cast with the fibula analogue, and the positions of the implants are decided. Once again, the position of the fibula analogue is checked to be in a functionally ideal position. Drill holes are introduced into the denture to pass through the fibula analogue. This denture will serve as the surgical stent that will guide the position of the fibula in the oral cavity. It is useful to provide some means by which the surgical stent can be attached onto the remaining dentition (or the opposing dentition), either with wire holes or clasps or denture hooks.
Surgical Steps
The resection is carried out according to plan. The denture stent is then wired onto the remaining mandible (or attached to the maxilla in cases where it is not possible to attach the stent onto the remaining mandible). The fibula bone is harvested and the required osteotomies done. The fibula is then introduced into the recipient site. The denture stent now determines the position of the fibula bone. The fibula bone is manipulated till it sits in the preoperatively determined position that is ideal for functional rehabilitation and plated with osteosynthesis screws or plates.
Through the implant drill guides incorporated in the denture-stent implant osteotomies are made into the underlying fibula. The denture-stent is then removed and implant inserted as per manufacturers protocol. If an implant is used which comes with an implant carrier, the denture is placed on (through) the implant carrier to confirm the positions of the implants as well as the fibula bone. This makes sure that the position of the fibula is ideal to result in a functional rehabilitation.
Discussion
Various reviews have shown that only about 15–25 % of patients who have been reconstructed end up with dental rehabilitation, the remainder of patients staying functionally crippled [5, 6]. One of the causes for such a low rate of rehabilitation is that the reconstructed bone is in a poor relation to support implants. Hence it is of prime importance to predictively reconstruct jawbones with occlusal rehabilitation in mind. Rohner et al. [7] had stressed on the importance of occlusal rehabilitation centered functional reconstruction as early as 2002.
Among various methods to reconstruct the jaws, prefabricated planning of fibula with computer assisted design and computer assisted manufacturing have brought in cutting edge technology into reconstructive surgery. These image guided treatment planning and execution improves the accuracy of reconstruction as well as the rates of rehabilitation [7]. Recently, Koch et al. [8] had described a method of planning and executing mandibular reconstruction using CAD CAM technology that produces dentures and dolder bars which act as external fixators. These techniques definitely provide far superior and predictable outcomes. However, they are expensive treatment modalities that are not practically possible for all patients in a resource-constricted setting.
The technique described in this paper has been aptly named “Jugaad technique”. “Jugaad” as per the definition from Financial Times Lexicon (www.lexicon.ft.com) is a word taken from Hindi, which means “finding a low-cost solution to a problem in an intelligent way, by not seeking sophistication or perfection by over-engineering products, but rather about developing a ‘good-enough’ solution that gets the job done”.
Jugaad technique requires the use of commonly available dental materials such as polymethyl metha acrylate, polymeric impression compounds as index material and fabrication of interim dentures as surgical guides. Not only are the costs for such planning minimal, it also produces the desired functional outcome. The authors use high-end planning solutions for affordable patients, but reserve this technique for the patients who cannot bear the costs for CAD CAM based solutions. To conclude, the described “Jugaad technique” is not meant to be superior in terms of accuracy, but is a low cost option. Using this technique, it is possible to provide functional reconstruction even in cases where there is no access to high-end, state-of-the-art technological solutions.
Acknowledgments
The authors acknowledge the support of the ITI Foundation for Promotion of Oral Implantology.
Compliance with Ethical Standards
Conflict of interest
All the authors declare that they have no conflict of interests.
References
- 1.Bodard AG, Salino S, Desoutter A, Deneuve S. Assessment of functional improvement with implant-supported prosthetic rehabilitation after mandibular reconstruction with a microvascular free fibula flap: a study of 25 patients. J Prosthet Dent. 2015;113(2):140–145. doi: 10.1016/j.prosdent.2014.08.005. [DOI] [PubMed] [Google Scholar]
- 2.Chen YS, Hu KY, Lin TW. The concept of “two arches” in mandibular reconstruction. Ann Plast Surg. 2012;69(6):616–621. doi: 10.1097/SAP.0b013e318273f92a. [DOI] [PubMed] [Google Scholar]
- 3.Thankappan K, Trivedi NP, Subash P, Pullara SK, Peter S, Kuriakose MA, et al. Three-dimensional computed tomography-based contouring of a free fibula bone graft for mandibular reconstruction. J Oral Maxillofac Surg. 2008;66(10):2185–2192. doi: 10.1016/j.joms.2008.01.035. [DOI] [PubMed] [Google Scholar]
- 4.Pramesh CS, Badwe RA, Borthakur BB, Chandra M, Raj EH, Kannan T, et al. Delivery of affordable and equitable cancer care in India. Lancet Oncol. 2014;15(6):e223–e233. doi: 10.1016/S1470-2045(14)70117-2. [DOI] [PubMed] [Google Scholar]
- 5.Chiapasco M, Biglioli F, Autelitano L, Romeo E, Brusati R. Clinical outcome of dental implants placed in fibula-free flaps used for the reconstruction of maxillo-mandibular defects following ablation for tumors or osteoradionecrosis. Clin Oral Implant Res. 2006;17(2):220–228. doi: 10.1111/j.1600-0501.2005.01212.x. [DOI] [PubMed] [Google Scholar]
- 6.Raoul G, Ruhin B, Briki S, Lauwers L, Haurou Patou G, Capet JP, et al. Microsurgical reconstruction of the jaw with fibular grafts and implants. J Craniofac Surg. 2009;20(6):2105–2117. doi: 10.1097/SCS.0b013e3181bec611. [DOI] [PubMed] [Google Scholar]
- 7.Rohner D, Bucher P, Hammer B. Prefabricated fibular flaps for reconstruction of defects of the maxillofacial skeleton: planning, technique, and long-term experience. Int J Oral Maxillofac Implants. 2013;28(5):e221–e229. doi: 10.11607/jomi.te01. [DOI] [PubMed] [Google Scholar]
- 8.Koch FP, Götze E, Kumar VV, Schulz P, Wentaschek S, Wagner W. A bar retained overdenture as an external fixator device in a 3D CAD/CAM based surgical reconstruction of the mandible. J Craniomaxillofac Surg. 2015;43(8):1447–1451. doi: 10.1016/j.jcms.2015.06.019. [DOI] [PubMed] [Google Scholar]