Abstract
Aim
The present study was planned to investigate the etiology of injuries and to analyze correlation between clinical and radiological findings in cases of craniomaxillofacial trauma.
Study Design
An 18 months cross-sectional study was done and 325 patients with maxillofacial fractures were analyzed from January 2013 to June 2014 who reported to the department of oral and maxillofacial surgery, Aligarh, Uttar Pradesh. Data was recorded in a preformed case sheet which included: patient’s demographic data, cause of injury, type of injury, treatment plan.
Results
Out of the 325 patients, 74.4 % were males with a male: female ratio of 2.91:1. The 21–30 year age group was found to be maximum. Road traffic accidents accounted for 71.3 %, followed by fall from height (19 %) and assault (9.5 %). Most commonly involved vehicles were two wheelers followed by public transport. Mandibular fractures (65 %) were most prevalent, followed by zygomaticomaxillary complex (44.27 %), parietal bone (48 %) and orbital fractures (21.3 %). Thirty-seven fractures (7.14 %) were missed clinically which were confirmed later by radiographic technique. Maximum were in cranium region (57 %) followed by mandible (27 %), mid face region (16.21 %). Thirty-three fractures (6.37 %) were overestimated or suspected clinically which could not be confirmed by radiographic technique. Maximum were in mandible (48.5 %) followed by mid face (36.33 %) and cranium (15.15 %).
Conclusion
The idea behind this article is to analyze the various trends and affecting factors and correlation between clinical and radiological findings. A better understanding of the above said would help in future treatment planning and management of facial injuries.
Keywords: Meta analysis, Craniomaxillofacial trauma, RTA, Assault, Clinical diagnosis, Sensitivity, Specificity
Introduction
All aspects regarding trauma have a great importance in the world today, being among the main causes of morbimortality. Each day, about 16,000 people die because of trauma [1]. Among the numerous injuries seen in urban trauma centers, facial trauma is one of the most prevalent. Since it is the most exposed part of the body, and the one least protected, the face is the region which is most associated with other organs or systems in emergency centers [2]. Craniomaxillofacial traumas are of common occurrence and their etiology depends on literacy level, socioeconomic, cultural and environmental factors [3]. This is an important health issue since most of the causes are preventable causes [4] and clear understanding of the demographic patterns of craniomaxillofacial injuries is necessary. Maxillofacial fractures lead to severe morbidity, cosmetic disfigurement as well as problems in oral functioning. Such epidemiological information can also be used to guide the future funding of public health programs geared towards prevention. Long term study data on craniomaxillofacial trauma are available for western countries. However, their finding cannot be correlated with Indian population because of different cultural and educational level and different weather conditions.
To our knowledge, no studies have been done so far to find out the etiological factors and to estimate the extent of craniomaxillofacial trauma in Western Uttar Pradesh, India. Oral and Maxillofacial Surgery Department of Dr. Ziauddin Ahmed Dental College, Aligarh is the major craniomaxillofacial trauma center which caters to the need of treatment to a large population of this region. Thus, this study was planned to study the demographic characteristics of craniomaxillofacial trauma in this region.
Aims and Objectives
The study was conducted to assess the etiological factors, pattern and demographic distribution of fractures at different sites of craniomaxillofacial skeleton and establishment of clinical and radiological correlation between the incidences of craniomaxillofacial trauma.
Materials and Methods
All the patients reporting to the outpatient Department of Oral and Maxillofacial Surgery, Dr. Ziauddin Ahmed Dental College and emergency department of Jawaharlal Nehru Medical College and Hospital, Aligarh, Uttar Pradesh from January 2013 to June 2014 having craniomaxillofacial injuries were evaluated and data was recorded in preformed case sheet. Data collected included: patient’s demographic data, cause of injury, type of injury, associated injuries, treatment plan. It was a prospective cross-sectional descriptive hospital based study. Patients with fatal injuries and patients or relatives (in case the patient is unconscious) who did not consent were excluded from the study. Institutional ethical clearance and patient consent were taken. The diagnosis was based on clinical and radiological findings. Routine radiographs included Occipitomental (OM) views, Submentovertex (SMV), Orthopantomograph (OPG), and Computer tomography (CT) scans. Obtained data was checked for completeness and clarity then entered into the computer and analysis was done using Statistical package for social sciences programme (SPSS) windows 7 version .19.
Observations and Results
Demographic Profile of Patients
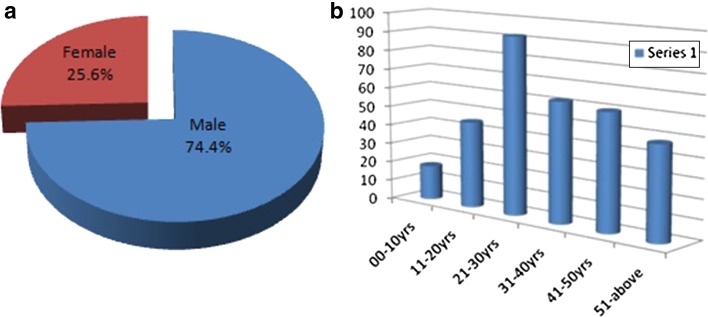
A total of 325 patients with craniomaxillofacial injuries were studied. Craniomaxillofacial fractures were more frequent in males (242 cases) (74.4 %) than in females (83 cases) (25.6 %) patients (Fig. 1a). Age group which was most affected by craniomaxillofacial trauma was 21–30 years (92 cases) (28.30 %) followed by 31–40 years (62 cases) (19 %) and was lowest among 00–10 years (15 cases) (4.6 %) (Fig. 1b). Among gender distribution, males and females both showed maximum frequency of craniomaxillofacial trauma in the age group of 21–30 years (27 % for males and 33 % for females).
Fig. 1.
a Gender distribution of Craniomaxillofacial trauma. b Age distribution of Craniomaxillofacial trauma
Etiology of Injury
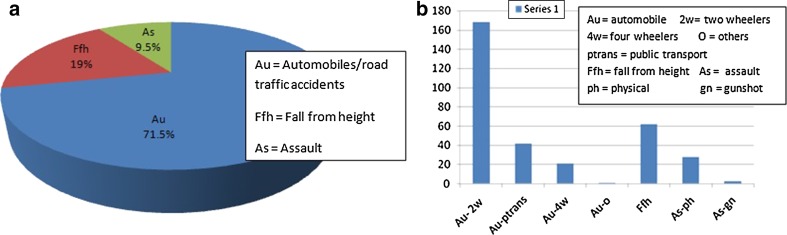
The main causes of fractures in the overall population of patients were: Traffic accident (71.3 %, n = 232), fall from height (19 %, n = 62), assault (9.5 %, n = 31). Traffic accident or automobile accidents was by far the most common (71.3 %) cause of fractures in patients. The main cause of fractures was road traffic accident both in males (71 %, n = 173) and in females (73 %, n = 60) (Fig. 2a, b).
Fig. 2.
a Etiological distribution among craniomaxillofacial trauma. b Individual etiological distribution among Craniomaxillofacial injuries
Fractures Pattern
Totally 325 patients were studied with 518 fractures. Most of the fractures involved the mandible (65 %, n = 337) followed by mid face fractures (25.3 %, n = 13). Among fractures involving two of the three components of our study, fractures involving mid face and mandible were highest (08 %, n = 28) and fractures involving all the three, cranium, mid face and mandible bone (0.9 %, n = 03) were the least.
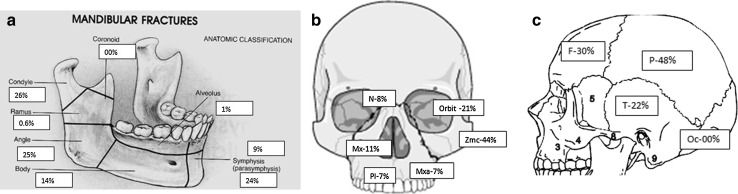
Mandibular fractures were mostly of condylar region (26.11 %, n = 88) followed by angle fractures (25.22 %, n = 85). Other fractures in mandible were parasymphysis (24 %, n = 81), followed by body (14.24 %, n = 48), symphysis (09 %, n = 29), mandibular alveolus (1.1 %, n = 04) and ramus (0.6 %, n = 02). There was no fracture noticed in coronoid region in our study (Fig. 3a). Mid face fractures were mostly of zygomaticomaxillary complex region (44.27 %, n = 58) followed by orbital fractures (21.3 %, n = 20). Other fractures in mid face were maxillary bone fractures (11.4 %, n = 15), followed by nasal bone (8.3 %, n = 11), maxillary alveolus (7.6 %, n = 10) and palatal bone fractures (6.8 %, n = 09) (Fig. 3b). Cranium fractures were mostly of parietal bone (48 %, n = 24) followed by frontal bone fractures (30 %, n = 15) and temporal bone fractures (22 %, n = 11). There was no fracture noticed in occipital bone region in our study (Fig. 3c).
Fig. 3.
a Mandibular fracture site distribution. b Midface fracture site distribution. c Cranium fracture site distribution
Missed Fractures
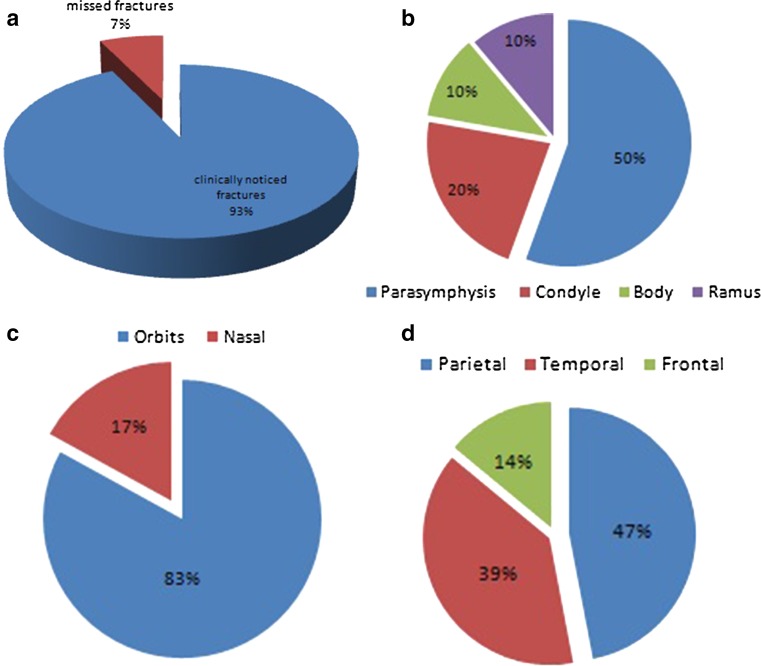
Totally 37 fractures (07.14 %) were missed clinically in our study which was confirmed later by radiographic technique. Out of these, maximum were in cranium region (57 %, n = 21) followed by mandible (27 %, n = 10) and mid face region (16.21 %, n = 06) (Fig. 4a). Site distribution of missed fractures among mandible, mid face and cranium is shown in Fig. 4b–d respectively.
Fig. 4.
a Missed fracture distribution. b Site distribution of missed fractures in mandible. c Site distribution of missed fractures in mid face. d Site distribution of missed fractures in cranium
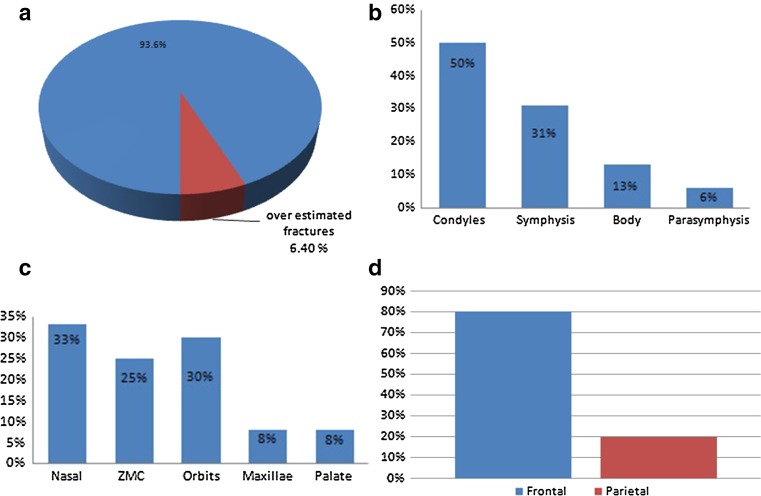
Overestimated Fractures
Totally 33 fractures (6.37 %) were over estimated or suspected clinically in our study which could not be confirmed by radiographic technique. Out of these, maximum were in mandible region (48.5 %, n = 16) followed by mid face (36.33 %, n = 12) and cranium (15.15 %, n = 05) (Fig. 5a). Site distribution of overestimated fractures among mandible, mid face and cranium is shown in Fig. 5b–d respectively.
Fig. 5.
a Overestimated fracture distribution. b Site distribution of overestimated fractures in mandible. c Site distribution of overestimated fractures in mid face. d Site distribution of overestimated fractures in cranium
Sensitivity of Clinical Diagnosis
Sensitivity of a test is defined as the proportion of people with disease who will have a positive result [5]. In the present study, sensitivity of clinical diagnosis can be defined as the proportion of actual number of fractures of total fractures which were clinically identified. Sensitivity was 70 % in cranium fractures and 95.60 and 97.11 % in mid face fractures and mandibular fractures respectively.
Specificity of Clinical Diagnosis
Specificity of a test is defined as the proportion of people without the disease who will have a negative result [5]. Specificity was 98.9 % in cranium fractures and 97.00 and 92.30 % in mid face fractures and mandibular fractures respectively.
Positive Predictive Value of Clinical Diagnosis
The positive predictive value (PPV) of a test is defined as the proportion of people with a positive test result who actually have the disease [6]. Positive predictive value can be defined as total proportion of clinically suspected fractures out of total fractures which were actually having fractures. It was 91 % in cranium fractures, 91.60 and 95.40 % in mid face and mandibular fractures respectively.
Negative Predictive Value of Clinical Diagnosis
The NPV of a test is the proportion of people with a negative test result who do not have disease [6]. Negative predictive value can be defined as total proportion of clinically suspected normal or non fractured bones out of total fractured bones which were actually not fractured. It was 97.70 % in cranium fractures, 98.50 and 95.02 % in mid face and mandibular fractures respectively. In our study, “Disease” is fracture of craniomaxillofacial bones and the diagnostic test is the “Clinical diagnosis”.
So, the ability of clinical diagnosis to detect all fractured bones in cranium and mid face is good but poor in mandible whereas the ability of clinical diagnosis to exclude fractured sites is good for mid face and mandible but very poor for cranium.
Discussion
In the present study, there was male prevalence with a male to female ratio of 2.91:1. Prasad [7] studied the characteristics of associated craniofacial trauma in patients with head injuries in 100 cases in Mangalore and found a male to female ratio of 8.09:1. Adebayo et al. [8] also recorded in their epidemiological survey report of maxillofacial fractures and concomitant injuries in Kaduna, Nigeria a male–female sex ratio of 3.7:1. Our finding correlates with the above surveys and that from Uganda (7.7:1) [9], Switzerland (6.2:1) [10] and Nairobi (8.4:1) [11]. When compared with studies from United Arab Emirates (11:1) [12] and Nigeria (16.9:1) [13], this figure is relatively low but is in unisense with studies from Korea (3.2:1) [14], Scotland (3:1) [15], Innsbruck (2.1:1) [16] and Finland (1.6:1) [17]. The higher percentage of males in this regard is related to the observation that in most of the families, males extensively work outdoors in order to earn the livelihood for the family which in turn makes them more susceptible to involve in RTA and assault. Mohajerani and Asghari [18] analysed the pattern of maxillofacial fractures in north western Iran and state that road traffic accident was the commonest cause (40 %) and the age group of 21–30 comprised the biggest group (30 %). Adebayo et al. [8] reported in their epidemiologic survey that the age range was from 3½ years to 67 years (mean = 39.7) with a peak incidence in the 4th decade (n = 197, 36.3 %) with a male–female sex ratio of 3.7:1. In the present study, most commonly affected age group was 21–30 years as found in many other studies [9, 13, 19, 20]. This could be because people in this age group usually complete their education and venture out in search of jobs; are involved in more outdoor activity making them more vulnerable to injuries as compared to other age groups. The predominance of injured males in the age group 21–30 years is consistent with the findings of previous published work [21–23].
Craniomaxillofacial injuries, like injuries elsewhere in the body, are caused by a known and relatively constant set of etiological factors. The results of epidemiological surveys on the causes and incidence of maxillofacial fractures tend to vary with geographic region, socioeconomic status, culture, religion, and era [21–25]. Road traffic accidents, assaults and fights, falls, sports injuries, industrial accidents, home accidents and domestic violence, firearm/firearm injuries and animal bites/accidents are the commonly recognized and reported etiological factors. Also, it is evident from the results that the majority of injuries occurred due to road traffic accidents, firearm wounds, and fall from height, etc., where men are often exposed to such hazards. Batista [26] studied 1121 patients with 790 instances of oral and maxillofacial trauma in Public Hospital in Guanhae, Brazil and found the cause of injury differed greatly between rural and urban areas, with car accidents, violence, and sports accidents being the most common cause in urban areas and accidents involving animals causing most injuries in rural areas. Hwang and You [27] after analyzing facial bone fractures in an 11-year study of 2094 patients found that the most common etiology was violent assault or nonviolent traumatic injury (49.4 %). Road traffic accident is a major cause of maxillofacial injury in our study. Our finding correlates with the findings of other studies [9, 12, 28–30] in respect to RTAs being the main etiological factor for maxillofacial fractures. This could be due to the fact that there is lack of individual sensitization about importance of safety devices of the vehicle, people are less adherent to safety rules and regulation, (most of the vehicles do not have all the safety devices), ambiguity of clear road traffic signal, congestion on the road because of either no separate pathways for pedestrians or less space, large numbers of overloaded buses and poorly maintained two wheelers.
Analytic data of different modes of injury in different studies is given in Table 1. Maryam et al. [34] suggested that the use of seat belts reduces the number of mid face injuries. The relationship between use of seat belts and the incidence of mid facial injuries requires further study. There are general indications that interpersonal violence is the leading cause of maxillofacial injuries in developed nations and that traffic accidents are the main cause of such injuries in developing countries [36–40]. According to the World Health Organization (WHO), road traffic injuries are the sixth leading cause of death in India with a greater share of hospitalization, deaths, disabilities and socioeconomic losses in the young and middle-aged population [40]. Road traffic injuries also place a huge burden on the health sector in terms of pre-hospital and acute care and rehabilitation [41]. Hill et al. [37] and Voss [38] reported assault as the predominant cause of craniomaxillofacial fractures in England and Norway, respectively. The 9.5 % incidence of craniomaxillofacial bone fractures in our study caused by assault contrast vividly with the figure of 55 % reported from Scotland [31], a finding that may be related to differences in social customs and alcohol intake.
Table 1.
Analytical data of different modes of injury in different studies
| Region | Total patients (n) | RTA (%) | Assault (%) | Fall from height (%) | Sports (%) |
|---|---|---|---|---|---|
| Jeju, Korea (Lee et al. [14]) | 318 | 17 | 40.9 | 9.1 | 11.9 |
| Ugandan (Kamulegeya et al. [9]) | 132 | 56.06 | 34.84 | – | 3.79 |
| Brazil (Maliska et al. [31]) | 132 | 48.4 | 36.4 | 9.8 | – |
| Southern Bulgaria (Bakardjiev and Pechalova [19]) | 1706 | 15.5 | 61 | 12.5 | – |
| Piracicaba, Brazil (Brasileiro and Passeri [32]) | 1024 | 45 | 22.6 | 17.9 | 7.8 |
| Hamedan, Iran (Ansari [33]) | 2268 | 60 | 10 | 18.9 | 1.05 |
| Diyrbakir, Turkey (Erol et al. [34]) | 2901 | 38 | 10 | 36.7 | 1.1 |
| Northern Nigeria (Olasoji et al. [35]) | 306 | 36 | 48 | 9 | 4 |
| Ibadan, Nigeria (Fasola et al. [29]) | 483 | 69.2 | 12 | 9.1 | 5.2 |
Hwang and You [27] after analyzing facial bone fractures in an 11-year study of 2,094 patients found that the most common isolated fracture site was the nasal bone (37.7 %), followed by the mandible (30 %), orbital bones (7.6 %), Zygoma (5.7 %), maxilla (1.3 %) and the frontal bone (0.3 %). Kapoor and Kalra [42] found in retrospective analysis of maxillofacial injuries, in patients reporting to a tertiary care hospital in East Delhi, that the injuries were most frequently observed in the mandible followed by the midface. In the present study, the most common location of the craniomaxillofacial fractures was found to be lower third (65 %). This finding correlates with the findings of other studies where lower third fractures were found to be maximum [9, 17, 28, 43, 44] but in contrast with other studies where mid face was involved most [9, 16, 45–47]. Mandible/lower third of face was the most commonly involved bone in our study. Although being the heaviest and strongest facial bone, the mandible is more prone to fracture because of its anatomical peculiarity in form and location and being the only movable facial bone. Various studies have also shown the mandible to be the most affected bone [9, 12, 17, 25, 28, 31, 32, 35, 47–50] But other studies accounted Zygoma to be the maximally involved bone [50, 51]. A report with high values of RTA tended to present predominantly condylar fracture in the present study. Other studies have confirmed this finding [12, 15, 48–50]. Some studies reported fractures of the body to be the most frequent mandibular fracture sites [9, 15] while many others showed symphysis [52] and parasymphysis [53] related to road traffic accident mode. This can be explained due to the fact that most of the commercially available helmets for two wheelers do not cover the total facial area especially the chin. Trauma on chin due to road traffic accidents results in indirect trauma to the condyle. It is a known fact that condylar fractures are often a result of an indirect trauma to the chin. This is the trauma mechanism for more number of condylar fractures seen in our study. In case of trauma from assault, angle of the mandible was the common site for fracture which is in accordance to other studies [9, 15, 32, 47, 53]. This is because as the angle is a weak region due to thinner cross-section and presence of third molar, lateral impact forces enforced on angle region leads to its fracture.
Kamulegeya [54] in his study found that symphysis and maxillary fractures were the most common mandibular and mid-facial fractures. Bali and Sharma [55] concluded in their study that mandible was the most commonly fractured bone with parasymphysis being the commonest affected site. In our study, condylar fracture was the most common fracture that occurred in the mandible. This finding correlates with findings of other studies [12, 16, 32, 50, 56–58]. However, in contrast to our study, various studies have reported that most common mandibular fracture site was body of the mandible [15, 28, 31, 35, 52, 59–61] followed by parasymphysis [62–64] symphysis [9] and angle of the mandible [14]. This could be explained by the fact that there are high chances of impact transfer to the condylar region in cases of injuries to mandible due to the high velocity road traffic accidents.
Ravindran [65] carried out a met analysis of Maxillofacial Trauma and found that there was an increased incidence of mid face fractures when compared to mandibular fractures. Most common site of mandibular fracture was in the parasymphysis region and in the mid face was the zygomatic complex region. In our study, Zygomatic complex was most common site of fracture, which correlates with other studies [10, 16, 28, 31, 32] whereas maxillary bone was found to be most commonly involved in some studies [9, 12, 47] and nasal bone fractures in others [14]. This finding may be correlated because of the fact that zygomatimaxillary complex is most prominent portion on the face and apart from mandible it is most vulnerable to the injuries caused by the road traffic accident or assault.
Several studies dealing with missed injuries and delayed diagnoses have been published and report an incidence of 1.3–39 %. Analytic data of different studies regarding missed injuries is given in Table 2. Many authors limited their investigations to a special field of interest. Different studies have used different definitions to determine clinical significance. Some publications focused on those missed injuries that were associated with high morbidity and mortality because of delayed diagnosis [70, 72]. Others used the requirement of further surgical procedures as criteria to define clinically significant missed injuries [68]. In our study many fractures were missed clinically or were diagnosed as other fractures because of local condition, unusual presentation. Such as parasymphysis fractures were diagnosed as symphysis fractures due to no appreciative step deformation on lower border of mandible. Condylar fractures were not clinically suspected as they present with little or no loss/limitation of function. In mid face, orbital fractures could not be appreciated because of circumorbital oedema and ecchymosis. In cranium, parietal bone fractures were very difficult to find out clinically. Many a time, patient noncooperation was a major factor. In our study, we found that 37 fractures (07.14 %) were missed clinically in our study which was confirmed later by radiographic technique. Out of these, maximum were in cranium region (57 %, n = 21) followed by mandible (27 %, n = 10) and mid face region (16.21 %, n = 06) (Fig. 4a). Site distribution of missed fractures among mandible, mid face and cranium is shown in Fig. 4b–d respectively.
Table 2.
Analytical data of different studies regarding missed injuries
| Study | Total patients | Population | Total missed injuries (%) |
|---|---|---|---|
| Wei et al. [66] | 3081 | Emergency radiology patients | 3.7 |
| Kalemoglu et al. [67] | 709 | Major trauma patients | 4.8 |
| Brooks et al. [68] | 65 | Major trauma patients | 22.2 |
| Vles et al. [69] | 3879 | Trauma patients | 1.3 |
| Buduhan et al. [70] | 567 | Multiple trauma patients | 8.1 |
| Janjua et al. [71] | 206 | Trauma patients | 39 |
Many fractures were clinically suspected because of the extreme tenderness of the overlying soft tissue and history of trauma, fracture pattern and sometimes due to the patient’s noncooperation. In our study, 33 fractures (6.37 %) were over estimated or suspected clinically which could not be confirmed by radiographic technique. Out of these, maximum were in mandible region (48.5 %, n = 16) followed by mid face (36.33 %, n = 12) and cranium (15.15 %, n = 05). (Figure 5a) Site distribution of overestimated fractures among mandible, mid face and cranium is shown in Fig. 5b–d respectively.
The sensitivity of clinical diagnosis in case of cranium was found to be 70 % of total fractures. In case of mid face and mandible, 95.60 % of total fractures having mid face involvement and 97.11 % of total fractures involving mandible were noticed clinically. Specificity of clinical diagnosis in case of cranium was 98.95 % whereas in mid face and mandible, 97 and 92.3 % of normal bones were clinically approved as none fractured respectively.
Positive and Negative predictive values describe a patient’s probability of having disease once the results of his or her tests are known. In case of cranium, only 91 % of clinically suspected fractures were actually having fractures. Whereas in case of mid face and mandible, 91.6 and 95.40 % of clinically identified fractures were actually fractured.
In cranium, 97.7 % of clinically non fractured bones out of total fractured bones were actually not having fractures whereas in mid face and mandible, 98.50 and 95.02 % clinically normal appearing bones were actually normal or not fractured.
Conclusion
In the present study, males were more affected with a male to female ratio of 3:1. Most commonly affected age group was 21–30 years. Majority of injuries occurred due to road traffic accidents, fall from height and physical assault and firearm wounds. The most common location of the craniomaxillofacial fractures was found to be lower third (65 %). A report with high values of RTA tended to present predominantly condylar fracture in the present study. In case of trauma from assault, angle of the mandible was the common site for fracture and condylar fracture was the most common fracture that occurred in the mandible. Zygomatic complex was most common site of fracture in mid face region. Sensitivity and specificity testing of clinical diagnosis showed that, cranium was involved in 70 % cases, mid face and mandible were involved in 95.6 and 97.11 % respectively. Predictive values reveal that, 98.95 % of non fractured bones out of total fractures were clinically identified as normal in cranium region whereas in 97 and 92.3 % of normal bones were clinically approved as non-fractured in mid face and mandibular regions respectively. The ability of clinical diagnosis to detect all fractured bones in cranium and mid face is good but poor in mandible whereas the ability of clinical diagnosis to exclude fractured sites is good for mid face and mandible but very poor for cranium. In the management of craniomaxillofacial trauma patients, radiographic examination should precede the planning by any treatment. Computerized CT scans with 3D reconstruction should also be used rather than prescribing plain radiograph only as the former would give complete information about the fractures.
Contributor Information
Ritesh Kumar, Email: ritesh3036@gmail.com, Email: drritesh3036@gmail.com.
Syed Saeed Ahmed, Email: drssahmed@msn.com.
Gulam Sarwar Hashmi, Email: sarwarhashmi@rediffmail.com.
Md. Kalim Ansari, Email: drmdkalimansari@gmail.com.
Sajjad Abdur Rahman, Email: sajjad_ar@rediffmail.com.
References
- 1.Krug EG, Sharma GK, Lozano R. The global burden of injuries. Am J Public Health. 2000;90:523–526. doi: 10.2105/ajph.90.4.523. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Alvi A, Dohert T, Lewen G. Facial fractures and concomitant injuries in trauma patients. Laryngoscope. 2003;113:102–106. doi: 10.1097/00005537-200301000-00019. [DOI] [PubMed] [Google Scholar]
- 3.Ellis E, Moos KF, EL-Attar A. Ten years of mandibular fractures. An analysis of 2137 cases. Oral Surg. 1985;59:120–129. doi: 10.1016/0030-4220(85)90002-7. [DOI] [PubMed] [Google Scholar]
- 4.Adebayo, et al. The pattern of fractures of facial skeleton in Kaduna, Nigeria. Oral Surg Oral Med Oral Path. 1980;49:491–495. doi: 10.1016/0030-4220(80)90068-7. [DOI] [PubMed] [Google Scholar]
- 5.Mayer D. Essential evidence based medicine. Cambridge: Cambridge University Press; 2004. [Google Scholar]
- 6.Altman DG, Bland JM. Diagnostic tests 2: predictive values. BMJ. 1994;309:102. doi: 10.1136/bmj.309.6947.102. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Rajendra PB. Characteristics of associated craniofacial trauma in patients with head injuries: an experience with 100 cases. J Emerg Trauma Shock. 2009;2(2):89–94. doi: 10.4103/0974-2700.50742. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Ajike SO, Adebayo ET, Amanyiewe EU, Ononiwu CN. An epidemiologic survey of maxillofacial fractures and concomitant injuries in Kaduna, Nigeria. Niger J Surg Res. 2005;7(3):251–255. [Google Scholar]
- 9.Kamulegeya A, Lakor F, Kabenge K. Oral maxillofacial fractures seen at a Ugandan tertiary hospital: a six-month prospective study. Clinics. 2009;64(9):843–848. doi: 10.1590/S1807-59322009000900004. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Eggensperger N, Smolka K, Scheidegger B, Zimmermann H, Iizuka T. A 3-year survey of related maxillofacial fractures in central Switzerland. J Craniomaxillofac Surg. 2007;35(3):161–167. doi: 10.1016/j.jcms.2007.01.002. [DOI] [PubMed] [Google Scholar]
- 11.Mwaniki DL, Guthua SW. Occurrence and characteristics of mandibular fractures in Nairobi, Kenya. Br J Oral Maxillofac Surg. 1990;28(3):200–202. doi: 10.1016/0266-4356(90)90089-4. [DOI] [PubMed] [Google Scholar]
- 12.AlAhmed HE, Jaber MA, Abu Fanas SH, Karas M. The pattern of maxillofacial fractures in Sharjah, United Arab Emirates: a review of 230 cases. Oral Surg Oral Med Oral Pathol Oral Radiol Endod. 2004;98(2):166–170. doi: 10.1016/j.tripleo.2004.01.020. [DOI] [PubMed] [Google Scholar]
- 13.Adekeye EO. The pattern of fractures of the facial skeleton in Kanduna, Nigeria. A survey of 1447 cases. Oral Surg Oral Med Oral Pathol. 1980;49(6):491–495. doi: 10.1016/0030-4220(80)90068-7. [DOI] [PubMed] [Google Scholar]
- 14.Lee JH, Cho BK, Park WJ. A 4 year retrospective study of facial fractures in Jeju, Korea. J Craniomaxillofac Surg. 2010;38(3):192–196. doi: 10.1016/j.jcms.2009.06.002. [DOI] [PubMed] [Google Scholar]
- 15.Ellis E, 3rd, Moos KF, El-Attar A. Ten years of mandibular fractures: an analysis of 2137 cases. Oral Surg Oral Med Oral Pathol. 1985;59(2):120–129. doi: 10.1016/0030-4220(85)90002-7. [DOI] [PubMed] [Google Scholar]
- 16.Gassner R, Tuli T, Hachl O, Rudisch A, Ulmer H. Craniomaxillofacial trauma: a 10 year review of 9543 cases with 21067 injuries. J Craniomaxillofac Surg. 2003;31(1):51–61. doi: 10.1016/s1010-5182(02)00168-3. [DOI] [PubMed] [Google Scholar]
- 17.Thorén H, Iso-Kungas P, Iizuka T, Lindqvist C, Törnwall J. Changing trends in causes and patterns of facial fractures in children. Oral Surg Oral Med Oral Pathol Oral Radiol Endod. 2009;107(3):318–324. doi: 10.1016/j.tripleo.2008.09.024. [DOI] [PubMed] [Google Scholar]
- 18.Mohajerani SH, Asghari S. Pattern of mid-facial fractures in Tehran, Iran. Dent Traumatol. 2011;27:131–134. doi: 10.1111/j.1600-9657.2011.00979.x. [DOI] [PubMed] [Google Scholar]
- 19.Bakardjiev A, Pechalova P. Maxillofacial fractures in Southern Bulgaria: retrospective study of 1706 cases. J Craniomaxillofac Surg. 2007;35(3):147–15021. doi: 10.1016/j.jcms.2007.01.005. [DOI] [PubMed] [Google Scholar]
- 20.Devadiga A, Prasad K. Epidemiology of maxillofacial fractures and concomitant injuries in a craniofacial unit: a retrospective study. Internet J Epidemiol. 2007;5(2):1–7. [Google Scholar]
- 21.Cheema SA. Zygomatic bone fracture. J Coll Phys Surg Pak. 2004;14:337–339. [PubMed] [Google Scholar]
- 22.Ferrerira PC, Amarante JM, Sliva AC, Pereira JM, Cardoso MA, Rodrigues JM. Etiology and pattern of pediatric mandibular fracture in Portugal: a retrospective study of 10 years. J Craniofac Surg. 2004;15:384–391. doi: 10.1097/00001665-200405000-00008. [DOI] [PubMed] [Google Scholar]
- 23.Afzal A, Shah R. Causes of maxillofacial injury: a three-year study. J Surg Pak. 2001;6:25–27. [Google Scholar]
- 24.Bataineh AB. Etiology and incidence of maxillofacial fractures in the north of Jordan. Oral Surg Oral Med Oral Pathol Oral Radiol Endod. 1998;86:31–35. doi: 10.1016/s1079-2104(98)90146-9. [DOI] [PubMed] [Google Scholar]
- 25.Adi M, Ogeden GR, Chisholm DM. An analysis of mandibular fracture in Dundee, Scotland (1977–1985) Br J Oral Maxillofac Surg. 1990;28:194–199. doi: 10.1016/0266-4356(90)90088-3. [DOI] [PubMed] [Google Scholar]
- 26.Ferreira MC, Batista AM, Ferreira FDO, Ramos-Jorge ML, Marques LS. Pattern of oral-maxillofacial trauma stemming from interpersonal physical violence and determinant factors. Dent Traumatol. 2014;30(1):15–21. doi: 10.1111/edt.12047. [DOI] [PubMed] [Google Scholar]
- 27.Hwang K, You SH. Analysis of facial bone fractures: an 11-year study of 2094 patients. Indian J Plast Surg. 2010;43:42–48. doi: 10.4103/0970-0358.63959. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 28.Ansari MH. Maxillofacial fractures in Hamedan province, Iran: a retrospective study (1987–2001) J Craniomaxillofac Surg. 2004;32(1):28–34. doi: 10.1016/j.jcms.2003.07.010. [DOI] [PubMed] [Google Scholar]
- 29.Fasola AO, Nyako EA, Obiechina AE, Arotiba JT. Trends in the characteristics of maxillofacial fractures in Nigeria. J Oral Maxillofac Surg. 2003;61(10):1140–1143. doi: 10.1016/s0278-2391(03)00671-2. [DOI] [PubMed] [Google Scholar]
- 30.Kadkhodaie MH. Three-year review of facial fractures at a teaching hospital in northern Iran. Br J Oral Maxillofac Surg. 2006;44(3):229–231. doi: 10.1016/j.bjoms.2005.06.016. [DOI] [PubMed] [Google Scholar]
- 31.Maliska MC, Lima Junior SM, Gil JN. Analysis of 185 maxillofacial fractures in the state of Santa Catarina, Brazil. Braz Oral Res. 2009;23(3):268–274. doi: 10.1590/s1806-83242009000300008. [DOI] [PubMed] [Google Scholar]
- 32.Brasileiro BF, Passeri LA. Epidemiological analysis of maxillofacial fractures in Brazil: a 5-year prospective study. Oral Surg Oral Med Oral Pathol Oral Radiol Endod. 2006;102:28–34. doi: 10.1016/j.tripleo.2005.07.023. [DOI] [PubMed] [Google Scholar]
- 33.Ansari MH. Maxillofacial fractures in Hamedan province, Iran: a retrospective study (1987–2001) J Craniomaxillofac Surg. 2004;32:28–34. doi: 10.1016/j.jcms.2003.07.010. [DOI] [PubMed] [Google Scholar]
- 34.Erol B, Tanrikulu R, Gorgun B. Maxillofacial fractures. Analysis of demographic distribution and treatment in 2901 patients (25-year experience) J Craniomaxillofac Surg. 2004;32(5):308–313. doi: 10.1016/j.jcms.2004.04.006. [DOI] [PubMed] [Google Scholar]
- 35.Olasoji HO, Tahir A, Arotiba GT. Changing picture of facial fractures in northern Nigeria. Br J Oral Maxillofac Surg. 2002;40(2):140–143. doi: 10.1054/bjom.2001.0716. [DOI] [PubMed] [Google Scholar]
- 36.Maryam A, Saud AA, Hassan EA. Effects of seat belts on incidence, aetiology, and severity of maxillofacial injuries in eastern province, Saudi Arabia: a four year prospective study. J Pak Dent Assoc. 2003;12:170–175. [Google Scholar]
- 37.Hill CM, Crosher RF, Caroll MJ, Mason DA. Facial fractures; the result of a prospective four-year-study. J Maxillofac Surg. 1984;12:267–270. doi: 10.1016/s0301-0503(84)80257-x. [DOI] [PubMed] [Google Scholar]
- 38.Voss R. The etiology of maxillofacial fractures in Norwegian patients. J Maxillofac Surg. 1982;10:146–148. doi: 10.1016/s0301-0503(82)80031-3. [DOI] [PubMed] [Google Scholar]
- 39.Khan M, Ahmed W. A comparative study of zygomatic bone fracture with transcutaneous hook traction versus Gillies approach. Pak Armed Forces Med J. 2003;53:47–50. [Google Scholar]
- 40.Grene D, Raven R. Epidimiology of facial injury in blunt assault. Arch Otolaryngol Head Neck Surg. 1997;123:923–928. doi: 10.1001/archotol.1997.01900090029005. [DOI] [PubMed] [Google Scholar]
- 41.Gururaj G (2006) Road traffic injury prevention in India. Bangalore, National Institute of Mental Health and Neuro Sciences, (Publication No. 56) (http://www.nimhans.kar.nic.in/epidemiology/doc/ep_ft22.pdf, consultado el 7 de abrilde 2009)
- 42.Kapoor P, Kalra N. A retrospective analysis of maxillofacial injuries in patients reporting to a tertiary care hospital in East Delhi. Int J Crit Illn Inj Sci. 2012;2(1):6–10. doi: 10.4103/2229-5151.94872. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 43.Olasoji HO, Tahir A, Arotiba GT. Changing picture of facial fractures in northern Nigeria. Br J Oral Maxillofac Surg. 2002;40(2):140–143. doi: 10.1054/bjom.2001.0716. [DOI] [PubMed] [Google Scholar]
- 44.Abiose BO. Maxillofacial skeleton injuries in the western states of Nigeria. Br J Oral Maxillofac Surg. 1986;24(1):31–39. doi: 10.1016/0266-4356(86)90037-9. [DOI] [PubMed] [Google Scholar]
- 45.Van Beek GJ, Merkx CA. Changes in the pattern of fractures of the maxillofacial skeleton. Int J Oral Maxillofac Surg. 1999;28(6):424–428. doi: 10.1034/j.1399-0020.1999.280605.x. [DOI] [PubMed] [Google Scholar]
- 46.Afzelius LE, Rosén C. Facial fractures. A review of 368 cases. Int J Oral Surg. 1980;9(1):25–32. doi: 10.1016/s0300-9785(80)80003-2. [DOI] [PubMed] [Google Scholar]
- 47.Lida S, Matsuya T. Paediatric maxillofacial fractures: their aetiological characters and fracture patterns. J Craniomaxillofac Surg. 2002;30(4):237–241. doi: 10.1054/jcms.2002.0295. [DOI] [PubMed] [Google Scholar]
- 48.Ugboko VI, Odusanya SA, Fagade OO. Maxillofacial fractures in a semi-urban Nigerian teaching hospital: a review of 442 cases. Int J Oral Maxillofac Surg. 1998;27(4):286–289. doi: 10.1016/s0901-5027(05)80616-2. [DOI] [PubMed] [Google Scholar]
- 49.Hosein M, Motamedi K. An assessment of maxillofacial fractures: a 5-year study of 237 patients. J Oral Maxillofac Surg. 2003;61(1):61–64. doi: 10.1053/joms.2003.50049. [DOI] [PubMed] [Google Scholar]
- 50.Lindqvist C, Sorsa S, Hyrkas T, Santavitra S. Maxillofacial fractures sustained in bicycle accidents. Int J Oral Maxillofac Surg. 1986;15(1):12–18. doi: 10.1016/s0300-9785(86)80005-9. [DOI] [PubMed] [Google Scholar]
- 51.Scherer M, Sullivan WG, Smith DJ, Jr, Phillips LG, Robson MC. An analysis of 1423 facial fractures in 788 patients at an urban trauma center. J Trauma. 1989;29(3):388–390. doi: 10.1097/00005373-198903000-00020. [DOI] [PubMed] [Google Scholar]
- 52.Martini MZ, Takahashi A, de Oliveira Neto HG, De Carvalho JP, Jr Curcio R, Shinohara EH. Epidemiology of mandibular fractures treated in a Brazilian level I trauma public hospital in the city of São Paulo, Brazil. Braz Dent J. 2006;17(3):243–248. doi: 10.1590/s0103-64402006000300013. [DOI] [PubMed] [Google Scholar]
- 53.King RE, Scianna JM, Petruzzelli GJ. Mandible fracture patterns: a suburban trauma center experience. Am J Otolaryngol. 2004;25(5):301–307. doi: 10.1016/j.amjoto.2004.03.001. [DOI] [PubMed] [Google Scholar]
- 54.Kamulegeya A. Oral maxillofacial fractures seen at a Ugandan tertiary hospital: a six-month prospective study. Clinics. 2009;64(9):843–848. doi: 10.1590/S1807-59322009000900004. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 55.Bali R, Sharma P. A comprehensive study on maxillofacial trauma conducted in Yamunanagar, India. J Inj Violence Res. 2010;5(2):108–116. doi: 10.5249/jivr.v5i2.331. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 56.Van Beek GJ, Merkx CA. Changes in the pattern of fractures of the maxillofacial skeleton. Int J Oral Maxillofac Surg. 1999;28(6):424–428. doi: 10.1034/j.1399-0020.1999.280605.x. [DOI] [PubMed] [Google Scholar]
- 57.Roccia F, Bianchi F, Zavattero E, Tanteri G, Ramieri G. Characteristics of maxillofacial trauma in females: a retrospective analysis of 367 patients. J Craniomaxillofac Surg. 2010;38(4):314–319. doi: 10.1016/j.jcms.2009.10.002. [DOI] [PubMed] [Google Scholar]
- 58.Hosein M, Motamedi K. An assessment of maxillofacial fractures: a 5-year study of 237 patients. J Oral Maxillofac Surg. 2003;61(1):61–64. doi: 10.1053/joms.2003.50049. [DOI] [PubMed] [Google Scholar]
- 59.Ugboko VI, Odusanya SA, Fagade OO. Maxillofacial fractures in a semi-urban Nigerian teaching hospital: a review of 442 cases. Int J Oral Maxillofac Surg. 1998;27(4):286–289. doi: 10.1016/s0901-5027(05)80616-2. [DOI] [PubMed] [Google Scholar]
- 60.Abiose BO. Maxillofacial skeleton injuries in the western states of Nigeria. Br J Oral Maxillofac Surg. 1986;24(1):31–39. doi: 10.1016/0266-4356(86)90037-9. [DOI] [PubMed] [Google Scholar]
- 61.Nair KB, Paul B. Incidence and aetiology of fractures of the facio-maxillary skeleton in Trivandrum. Br J Oral Maxillofac Surg. 1986;24(1):40–43. doi: 10.1016/0266-4356(86)90038-0. [DOI] [PubMed] [Google Scholar]
- 62.King RE, Scianna JM, Petruzzelli GJ. Mandible fracture patterns: a suburban trauma center experience. Am J Otolaryngol. 2004;25(5):301–307. doi: 10.1016/j.amjoto.2004.03.001. [DOI] [PubMed] [Google Scholar]
- 63.Subhashraj K, Nandakumar N, Ravindran C. Review of maxillofacial injuries in Chennai, India: a study of 2748 cases. Br J Oral Maxillofac Surg. 2007;45(8):637–639. doi: 10.1016/j.bjoms.2007.03.012. [DOI] [PubMed] [Google Scholar]
- 64.Thapliyal GK, Sinha R, Menon PS, Chakranarayan A. Management of mandibular fractures. MJAFI. 2008;64:218–220. doi: 10.1016/S0377-1237(08)80096-2. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 65.Ravindran V. Metaanalysis of maxillofacial trauma in the northern districts of Kerala: one year prospective study. J Maxillofac Oral Surg. 2011;10(4):321–327. doi: 10.1007/s12663-011-0264-3. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 66.Wei CJ, et al. Systematic analysis of missed extremity fractures in emergency radiology. Acta Radiol. 2006;47:710–717. doi: 10.1080/02841850600806340. [DOI] [PubMed] [Google Scholar]
- 67.Kalemoglu M, et al. Missed injuries in military patients with major trauma: original study. Mil Med. 2006;171:598–602. doi: 10.7205/milmed.171.7.598. [DOI] [PubMed] [Google Scholar]
- 68.Brooks A, et al. Missed injury in major trauma patients. Injury. 2004;35:407–410. doi: 10.1016/S0020-1383(03)00219-5. [DOI] [PubMed] [Google Scholar]
- 69.Vles WJ, et al. Consequences of delayed diagnoses in trauma patients: a prospective study. J Am Coll Surg. 2003;197:596–602. doi: 10.1016/S1072-7515(03)00601-X. [DOI] [PubMed] [Google Scholar]
- 70.Buduhan G, et al. Missed injuries in patients with multiple trauma. J Trauma. 2000;49:600–605. doi: 10.1097/00005373-200010000-00005. [DOI] [PubMed] [Google Scholar]
- 71.Janjua KJ, et al. Prospective evaluation of early missed injuries and the role of tertiary trauma survey. J Trauma. 1998;44:1000–1007. doi: 10.1097/00005373-199806000-00012. [DOI] [PubMed] [Google Scholar]
- 72.Houshian S, et al. Missed injuries in a level I trauma center. J Trauma. 2002;52:715–719. doi: 10.1097/00005373-200204000-00018. [DOI] [PubMed] [Google Scholar]