Abstract
Background
People aged 26–34 represent the greatest proportion of uninsured, and have the highest incidence of testicular cancers. The aim of this study was to investigate the association between insurance status and cancer outcomes in men diagnosed with germ cell tumors.
Methods
We used the SEER database to identify 10,211 men diagnosed with germ cell gonadal neoplasms from 2007–2011. We examined associations between insurance status and characteristics at diagnosis and receipt of treatment using log-binomial regression. The association between insurance status and mortality was assessed using Cox proportional hazards regression.
Results
Uninsured patients had an increased risk of metastatic disease at diagnosis (RR: 1.26, 95% CI: 1.15–1.38), compared with insured patients, as did Medicaid patients (RR: 1.62, 95% CI: 1.51–1.74). Among men with metastatic disease, uninsured and Medicaid patients were more likely to be diagnosed with intermediate/poor risk disease (uninsured RR: 1.22, 95% CI: 1.04–1.44; Medicaid RR: 1.39, 95% CI: 1.23–1.57), and were less likely to receive lymph node dissection (uninsured RR: 0.74, 95% CI: 0.57–0.94; Medicaid RR: 0.76, 95% CI: 0.63–0.92), compared with insured patients. Men without insurance were more likely to die from their disease (HR: 1.88, 95% CI: 1.29–2.75), compared with insured men, as were those with Medicaid (HR: 1.58, 95% CI: 1.16–2.15).
Conclusions
Patients without insurance and with Medicaid have an increased risk of presenting with advanced disease and dying from the disease, compared with those who have insurance. Future studies should examine whether implementation of the Patient Protection and Affordable Care Act reduces these disparities.
Keywords: Insurance, germ cell tumors, disparities, cancer, outcomes
Introduction
The Health Insurance Coverage report states that 42 million people, or 13.4% of the US population, were uninsured for the entire 2013 calendar period, while 64.2% were covered by private health insurance1. Age is strongly associated with insurance status; the greatest proportion of the uninsured are between 26 to 34 years of age (23.5%). This age disparity is particularly concerning for testicular cancer, since the median age of diagnosis is 33 years, and 73% of cases are diagnosed between the ages of 20 and 44 years2.
The 2010 Patient Protection and Affordable Care Act (PPACA) was designed in part to expand the proportion of individuals eligible for Medicaid and to improve access to private insurance, thereby providing insurance coverage to those who are currently under- or uninsured. It is estimated that the PPACA will expand health insurance coverage to 32 million individuals by 20193 and that over 30% of currently uninsured cancer survivors will be eligible for Medicaid or tax credits4. Furthermore, the expansion in coverage is aimed to improve insurance for young adults through Medicaid expansion, subsidies, prohibiting denial of coverage based on pre-existing conditions, and allowing young adults to remain on their parents’ insurance until 26 years of age.
The PPACA has potential to significantly impact both primary and secondary prevention of cancer. Previous studies have shown that uninsured patients are more likely to present with advanced disease, less likely to receive definitive treatment, and are more likely to die of their disease5–8. Furthermore, a recent study showed uninsured testicular cancer patients were more likely to present at later stages9. However, to our knowledge, research has not examined associations between insurance status - divided into insurance, Medicaid and no insurance - and cancer outcomes among men diagnosed with testicular germ cell tumors, a disease that is curable even when metastatic. This is important since the PPACA will likely involve a major expansion of Medicaid10, a joint federal and state program that helps low-income individuals pay for medical care, which is run by the states where individuals reside and is therefore subject to considerable variations in coverage. Furthermore, prior studies have found conflicting results regarding the association between Medicaid coverage and cancer outcomes, including extent of disease at diagnosis and receipt of guideline-concordant treatments5,6,8,11–15.
Therefore, the aim of this study was to evaluate associations between insurance status and: 1) stage of disease at presentation, 2) receipt of treatment, and 3) survival among men diagnosed with a germ cell tumor using the Surveillance, Epidemiology, and End Results (SEER) program, which collects population-based data from cancer registries, capturing approximately 97% of incident cancer cases from seventeen cancer registries representing 28% of the United States population16,17. We hypothesized that men without any insurance would be more likely to have more advanced disease at presentation and poorer outcomes compared with those with insurance, and that the outcomes of men with Medicaid would be intermediate between the uninsured and insured groups.
Patients and Methods
Study population
We utilized the SEER*stat software program to identify 11,515 men diagnosed with germ cell or trophoblastic gonadal neoplasms between 2007 and 2011, since insurance information was collected by SEER beginning in 200718. Testicular germ cell diagnoses were obtained from the International Classification of Diseases for Oncology, third edition (ICD-O-3), and were classified as either seminoma (n = 5,709) or nonseminoma (n = 4,502). Patients ≥65 years old were excluded from this analysis because of lack of reliable Medicare data in SEER and because we were interested in testicular germ cell tumors, which are more commonly diagnosed in men <65 years (n=206). We also excluded men with incomplete TNM staging information (n=564) and those with missing insurance information (n=534). Thus, our analytic cohort included 10,211 men in the United States.
Primary predictor
Insurance status was classified according to the SEER categories: 1) insured, including private insurance (fee-for-service, managed care, health maintenance organization, or preferred-provider organization), insured (no specifics), and coverage from the military or Veterans Affairs, 2) Medicaid (Indian/Public Health Service, Medicaid, Medicaid - administered through a Managed Care plan, Medicare with Medicaid eligibility), or 3) uninsured. We compared men with Medicaid and men without insurance to men with insurance, respectively.
Outcomes
Metastatic disease was defined as stage II or III disease at diagnosis based on the TNM staging system. Among men with metastatic disease, good, intermediate and poor risk was defined according to the International Germ Cell Consensus Classification (IGCCC) system. Receipt of radical orchiectomy among all men was obtained based on SEER variables. Additional treatment with radiation therapy (RT) for patients with stage I seminomas and with lymph node dissection for patients with stage II or higher disease at diagnosis was also examined; chemotherapy use could not be examined because SEER does not release this information. Finally, we utilized information collected by the SEER Program on cause of death (e.g., from treating physicians and links to the National Death Index) to evaluate both all-cause and cancer-specific mortality. Survival was defined as the time from diagnosis to death, or end of follow-up (December 31, 2011), whichever came first.
Covariates
We obtained information on covariates from the SEER*Stat program. Race was classified as non-Hispanic white, African-American, Non-black Hispanic, Asian and other. Geographic region (Northeast, Midwest, South, West), tumor histology (seminoma versus non-seminoma) and year of diagnosis (2007–2011) were also obtained at the individual level. Income (median household income) and educational level (percentage of residents >25 years of age with at least a high school education) were obtained at the county level from SEER*Stat through linkage to the United States Census, and were both modeled as categorical variables19. Residence type (rural/urban) was also obtained at the county level by linkage to the United States Department of Agriculture (USDA)20.
Statistical analysis
Data were extracted from the SEER*Stat program. We used log-binomial regression models to calculate relative risks (RRs) and 95% confidence intervals (95% CIs) for the association between insurance status and presentation at diagnosis (metastatic disease, IGCCC category, and tumor size). All multivariable models were adjusted for sociodemographic and clinical factors, including: age, race/ethnicity, income, education level, urban/rural setting, geographic region, tumor histology, and year of diagnosis. All factors were measured at the individual level, with the exception of income, education and urban/rural setting (county level data linked by ZIP codes).
We examined associations between insurance status and receipt of additional treatment among men who were initially treated with radical orchiectomy using log-binomial models. First, we evaluated associations between insurance status and receipt of radiation therapy among men who were diagnosed with a stage I seminomatous tumors. Next we assessed the use of lymph node dissection among men who presented with metastatic disease.
Unadjusted associations between insurance status and GCT-specific mortality were plotted using Kaplan-Meier curves. Cox proportional hazards regression models were used to calculate adjusted hazard ratios (HRs) and 95% confidence intervals (CIs) for the association between all-cause and cancer-specific mortality, using time since diagnosis as the underlying time scale. Cox models were adjusted for sociodemographic and clinical characteristics mentioned above, as well as stage at diagnosis, and tumor size. In sensitivity analyses, we conducted competing risks analyses utilizing the Fine and Gray method.21 We also conducted propensity-score analyses to balance measurable confounders between those who had private insurance, Medicaid or no insurance.22 Next we stratified race to further evaluate potential confounding by race. Finally, we evaluated the association between insurance status and stage of disease at presentation and survival stratified by state/registry.
All statistical analyses were performed with SAS v9.4 (SAS Institute, Cary, NC). Two-sided p-values <0.05 were considered to be statistically significant.
Results
There were 10,211 germ cell and trophoblastic gonadal neoplasms identified from 2007–2011 in the SEER database. Over seventy-five percent of the men (n=7,818, 77%) had insurance, 13% had Medicaid insurance (n=1,330) and 10% (n=1,063) were uninsured. Table 1 shows the characteristics of the study population according to insurance status at diagnosis. Men who were uninsured were more likely to be younger, have a lower household income, and live in the South, and were less likely to be non-Hispanic white and live in a metropolitan area, compared to men with insurance. There were no differences in year of diagnosis by insurance status.
Table 1.
Patient demographics and clinical characteristics among men with germ cell or trophoblastic gonadal neoplasms by insurance status, SEER database 2007–2011
| Characteristic | Total (n=10,211) |
Uninsured (n=1,063) |
Medicaid (n=1,330) |
Insured (n=7,818) |
P-value |
|---|---|---|---|---|---|
| Age, years | |||||
| <=29 | 4099 (40%) | 558 (52%) | 701 (53%) | 2840 (36%) | <0.001 |
| 30–39 | 3117 (31%) | 297 (28%) | 350 (26%) | 2470 (32%) | |
| 40–64 | 2995 (29%) | 208 (20%) | 279 (21%) | 2508 (32%) | |
| Race | |||||
| Non-Hispanic White | 6928 (68%) | 621 (58%) | 629 (47%) | 5678 (73%) | <0.001 |
| African American | 613 (6%) | 48 (5%) | 67 (5%) | 498 (6%) | |
| Non-black Hispanic | 2207 (22%) | 377 (35%) | 552 (42%) | 1278 (16%) | |
| Asian | 309 (3%) | 10 (1%) | 43 (3%) | 256 (3%) | |
| Other | 154 (1%) | 7 (1%) | 39 (3%) | 108 (1%) | |
| Year of Diagnosis | |||||
| 2007 | 2000 (20%) | 197 (19%) | 227 (17%) | 1576 (20%) | 0.004 |
| 2008 | 2032 (20%) | 198 (19%) | 230 (17%) | 1604 (21%) | |
| 2009 | 2081 (20%) | 222 (21%) | 268 (20%) | 1591 (20%) | |
| 2010 | 2063 (20%) | 238 (22%) | 307 (23%) | 1518 (19%) | |
| 2011 | 2035 (20%) | 208 (20%) | 298 (22%) | 1529 (20%) | |
| Household income, USD* | |||||
| < 53590 | 2555 (25%) | 396 (37%) | 384 (29%) | 1775 (23%) | <0.001 |
| 53590–58370 | 2452 (24%) | 286 (27%) | 409 (31%) | 1757 (22%) | |
| 58370–70570 | 2635 (26%) | 217 (20%) | 308 (23%) | 2110 (27%) | |
| > 70570 | 2569 (25%) | 164 (15%) | 229 (17%) | 2176 (28%) | |
| High school education* | |||||
| >86% | 181 (2%) | 30 (3%) | 48 (4%) | 103 (1%) | <0.001 |
| 81–86% | 2801 (27%) | 385 (36%) | 571 (43%) | 1845 (24%) | |
| 70–80% | 2571 (25%) | 228 (21%) | 317 (24%) | 2026 (26%) | |
| <70% | 4658 (46%) | 420 (40%) | 394 (30%) | 3844 (49%) | |
| Residence | |||||
| Metro | 9231 (90%) | 903 (85%) | 1177 (88%) | 7151 (91%) | <0.001 |
| Non-metro | 964 (9%) | 160 (15%) | 142 (12%) | 662 (8%) | |
| Unknown | 16 (1%) | 0 | 0 | 5 (0%) | |
| Geographic Region | |||||
| West | 6223 (61%) | 515 (48%) | 1027 (77%) | 4681 (60%) | <0.001 |
| Midwest | 868 (9%) | 75 (7%) | 75 (6%) | 718 (9%) | |
| South | 1695 (17%) | 321 (30%) | 147 (11%) | 1227 (16%) | |
| Northeast | 1425 (14%) | 152 (14%) | 81 (6%) | 1192 (15%) | |
| Histology | |||||
| Nonseminoma | 4502 (44%) | 523 (49%) | 762 (57%) | 3217 (41%) | <0.001 |
| Seminoma | 5709 (56%) | 540 (51%) | 568 (43%) | 4601 (59%) | |
| Tumor size at Diagnosis | |||||
| <4cm | 5230 (51%) | 408 (38%) | 511 (38%) | 4311 (55%) | <0.001 |
| >=4cm | 4981 (49%) | 655 (62%) | 819 (62%) | 3507 (45%) | |
| Stage at Diagnosis | |||||
| I | 7418 (73%) | 718 (68%) | 742 (56%) | 5958 (76%) | <0.001 |
| II | 1229 (12%) | 133 (13%) | 185 (14%) | 911 (12%) | |
| III | 1564 (15%) | 212 (20%) | 403 (30%) | 949 (12%) | |
| Radical Orchiectomy | |||||
| Not performed | 236 (2%) | 30 (3%) | 61 (5%) | 145 (2%) | <0.001 |
| Performed | 9973 (98%) | 1033 (97%) | 1268 (95%) | 7672 (98%) | |
| Unknown | 2 (0%) | 0 | 1 (0%) | 1 (0%) |
county-level data linked by patient ZIP codes
Characteristics at Diagnosis
Thirty-two percent of uninsured men, 44% of men with Medicaid and 24% of men with insurance were diagnosed with metastatic disease (stage II or III disease) at presentation. After adjusting for potential confounding variables, men without any insurance had a 26% increased risk of being diagnosed with metastatic disease, compared to men with insurance, and those with Medicaid had over a 60% increased risk (Table 2). Among men with metastatic disease, those with Medicaid or without insurance were more likely to have intermediate or poor-risk disease, compared to men with insurance (Table 2). Men with Medicaid insurance and those without insurance were also more likely to present with a larger tumor compared to those who had insurance (Table 2). When the reference group was changed to uninsured, those with Medicaid were more likely to present with advanced stage (Supplementary Table 1).
Table 2.
Presentation of disease by insurance status among men with germ cell or trophoblastic gonadal neoplasms, SEER database 2007–2011
| Insured | Any Medicaid | Uninsured | |||
|---|---|---|---|---|---|
| RR | RR (95% CI) |
p | RR (95% CI) |
p | |
| Metastatic disease at diagnosis | (ref) | 1.62 (1.51–1.74) |
<0.001 | 1.26 (1.15–1.38) |
<0.001 |
| Intermediate or poor IGCCC category at diagnosis** | (ref) | 1.39 (1.23–1.57) |
<0.001 | 1.22 (1.04–1.44) |
0.01 |
| Tumor size ≥4cm at diagnosis | (ref) | 1.32 (1.25–1.39) |
<0.001 | 1.36 (1.29–1.43) |
<0.001 |
Abbreviations: RR = relative risk; IGCCC = International germ cell consensus classification.
Multivariable model adjusted for age, income, education level, race/ethnicity, geographic region, year of diagnosis, urban/rural setting, and tumor histology.
Among men with metastatic disease
Receipt of Treatment
There was no association between radical orchiectomy and insurance status (data not shown); >95% of men in all groups received radical orchiectomy (Table 1). However, as shown in Table 3, uninsured men who were diagnosed with a stage I seminoma were less likely to receive additional radiation after radical orchiectomy, compared to those with insurance (RR: 0.82, 95% CI: 0.70–0.95). There was no association between radiation therapy and Medicaid insurance. Among men diagnosed with metastatic disease, those without insurance or with Medicaid insurance had a reduced likelihood of undergoing a lymph node dissection (Table 3).
Table 3.
Association between receipt of treatment and insurance status among men with germ cell or trophoblastic gonadal neoplasms, SEER database 2007–2011
| Insured | Any Medicaid | Uninsured | |||
|---|---|---|---|---|---|
| RR | RR (95% CI) |
p | RR (95% CI) |
p | |
| Radiation therapy* | (ref) | 1.01 (0.89–1.15) |
0.87 | 0.82 (0.70–0.95) |
0.007 |
| Lymph node dissection** | (ref) | 0.76 (0.63–0.92) |
0.005 | 0.74 (0.57–0.94) |
0.02 |
Abbreviations: RR = relative risk
Among Stage 1 Seminoma patients who had previously undergone radical orchiectomy. Multivariable model adjusted for age, income, education level, race, geographic region, year of diagnosis, and urban/rural setting.
Among patients with metastatic disease who had previously undergone radical orchiectomy. Multivariable model adjusted for age, income, education level, race, geographic region, year of diagnosis, urban/rural setting and tumor histology
All-cause and cause-specific survival
As shown in Figure 1, insurance was associated with improved GCT-specific survival in unadjusted analyses, compared with Medicaid or no insurance. Median time from diagnosis to GCT-specific death was 2.4 years. In multivariable analyses, men with Medicaid insurance had an increased risk of GCT-specific mortality (HR: 1.51, 95% CI: 1.08–2.10) and of all-cause mortality (HR: 1.69, 95% CI: 1.31–2.19), compared with men with insurance. Similarly, men without insurance had an increased risk of both GCT-specific mortality (HR: 1.88, 95% CI: 1.29–2.75) and all-cause mortality (HR: 1.58, 95% CI: 1.16–2.15) (Figure 2). Results were similar for GCT-mortality when conducted using a competing risks approach (Medicaid HR: 1.60, 95% CI: 1.17–2.18; Uninsured HR: 1.71, 95% CI: 1.32–2.21). When we changed the reference group to uninsured, there was not a statistically significant difference between uninsured and Medicaid for all-cause or GCT-specific mortality (Supplementary Table 1). Similarly, propensity-score adjusted models yielded similar results (Supplementary Table 2).
Figure 1.
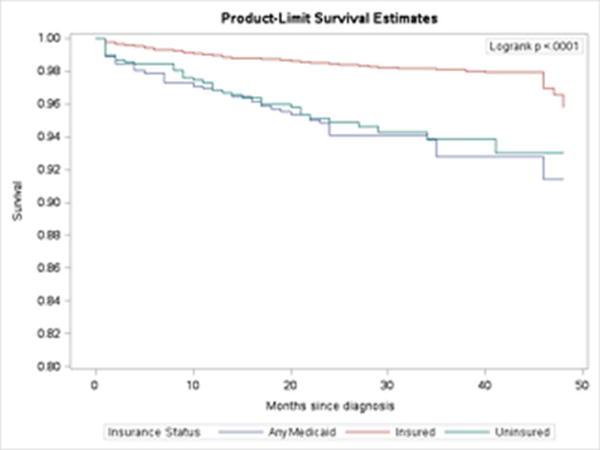
Kaplan-Meier survival curve for GCT-specific death by insurance status among men with germ cell or trophoblastic gonadal neoplasms, SEER database 2007–2011
Figure 2.
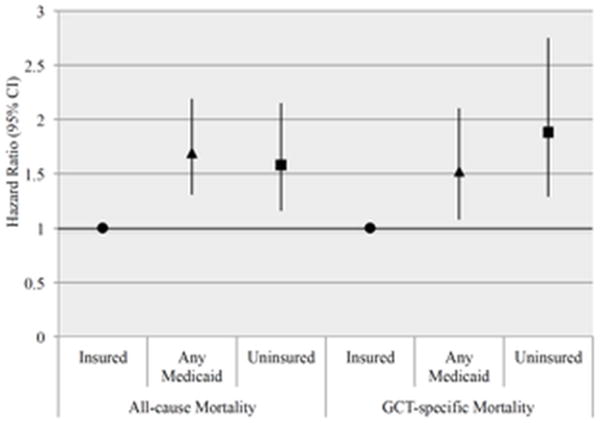
Risk of all-cause and GCT-specific mortality by insurance status among men with germ cell or trophoblastic gonadal neoplasms, SEER database 2007–2011
*Multivariable model adjusted for age, income, education level, race, geographic region, year of diagnosis, urban/rural setting, tumor histology, stage at diagnosis, and tumor size.
Because Medicaid programs differ by state, we evaluated the association between stage of disease at presentation and survival in California (combining Greater California, San Jose, San Francisco, and Los Angeles), New Jersey, and Georgia. We did not find a significant interaction between state/registry and insurance status on disease presentation or survival, and found similar results for metastatic disease at presentation (Supplementary Table 3). In New Jersey, we did not find an association between insurance status and GCT-specific or all-cause mortality (Supplementary Table 4), although this analysis was based on small numbers. To further investigate potential confounding by race, we stratified the analyses by race. Although based on small numbers, the results were similar. Among white men, uninsured men had an increased risk of all-cause and GCT-specific mortality, compared to insured (Supplementary Figure 1 and Supplementary Table 5).
Discussion
In this study utilizing the SEER database, we found many potential opportunities for improvement in access to care at disease presentation and follow-up, as men without traditional insurance were at risk for multiple adverse outcomes. We found that men without insurance and those with Medicaid had a higher risk of death compared to men with traditional insurance. Uninsured men had a 58% increased risk of all-cause mortality and 88% increased risk of GCT-specific mortality, compared with men with insurance. Similarly, men with Medicaid had a 69% and 51% increased risk of all-cause and GCT-specific mortality, respectively, compared with men with insurance.
Our findings suggest that men without insurance are more likely to present with a later stage of disease at diagnosis and worse tumor characteristics, including both a larger tumor size and intermediate/poor risk classification, compared with men who have traditional insurance. We found similar results among men with Medicaid insurance, who were more likely to present with advanced disease at diagnosis and receive fewer treatments compared with men who had traditional insurance. We found that men with Medicaid or without insurance were less likely to undergo a lymph node dissection (RPLND) for metastatic disease. An important part of GCT care and a metric of quality is receipt of RPLND for residual masses post-chemotherapy. Our findings of lower use of RPLND among uninsured men and those with Medicaid could be a surrogate for less access to pathway concordant care. We hypothesized that men with Medicaid would have worse outcomes than men with insurance, but better than men who were uninsured. For some of our outcomes, such as tumor size at diagnosis, receipt of additional treatment, and cause-specific mortality, men with Medicaid were in between men with insurance and men without any insurance. However, consistent with prior studies5,12, for other outcomes such as stage and risk category at disease presentation, Medicaid performed similarly or worse than uninsured.
These findings confirm and extend results from prior studies by examining associations between insurance status and cancer outcomes in a well-characterized, population-based study of male germ cell tumors. While other studies have demonstrated that broad groups of patients with different cancers who are uninsured were more likely to present with metastatic disease, less likely to receive definitive treatment, and more likely to die of any cause, compared to those with traditional insurance,6,7 our study showed that these results are persistent even among patients with Medicaid in highly curable germ cell tumors. Notably, we found that both men without insurance and those with Medicaid had a persistently increased risk of both germ-cell-specific and all-cause mortality, compared to men with traditional insurance. These results suggest that efforts to eliminate cancer disparities through the expansion of Medicaid alone may be insufficient.
To our knowledge, this is the first study to rigorously examine associations between germ cell tumors and three levels of insurance status in a population-based study. Although a recent study reported that lack of insurance was associated with more advanced stage at diagnosis and poorer outcomes among men with testicular cancer, compared to those with insurance or Medicaid, this study had important limitations9. Notably, this study did not separate out Medicaid and non-Medicaid insurance – a potentially important distinction as highlighted in this analysis, omitted important confounders (e.g., ethnicity, education, income), and included fewer cases.
There are some possible explanations for the mixed findings on the impact of Medicaid coverage on cancer outcomes. First, Medicaid-insured men may have lower socioeconomic status and poorer access to healthcare than uninsured men. While we lacked individual-level data on socioeconomic factors, we found that men with Medicaid were more likely to have a higher household income, compared to men without insurance, despite having less education. Another possible explanation is misclassification of insurance type. In most states when an individual is diagnosed with cancer, they can qualify for Medicaid with the eligibility date assigned as the date of diagnosis. Thus, they can move from the uninsured group to Medicaid-insured. Consistent with this hypothesis, Bradley et al. found that subjects who enrolled in Medicaid after their cancer diagnosis were more likely to present with advanced stage disease and have lower survival rates compared to those were enrolled in Medicaid before their cancer diagnosis13. Future studies should include timing of diagnoses and enrollment in Medicaid to better classify insurance status.
Insurance status in the context of germ cell tumors is particularly interesting as there are differences in insurance prevalence by age in the United States. Age is associated with whether a person has insurance, and the type of insurance they have, with 19–34 year olds accounting for about 38% of the uninsured population under the age of 651. Furthermore, testicular cancer is most commonly diagnosed in men between the ages of 20–34, with a median age of 33. Thus, expanding insurance availability through the Affordable Care Act may have a large impact on cancer outcomes in men diagnosed with germ cell tumors since earlier studies have demonstrated that previously uninsured adults increase their use of basic clinical services after gaining Medicare or Medicaid coverage and this results in improvements in self-reported health23–26. In our study, lack of insurance was associated with an increased risk of both cause-specific and all-cause mortality.
Implementation of the ACA could result in a 70% reduction in uninsured individuals27, and is also estimated to increase Medicaid-eligibility among the uninsured, with enrollment in Medicaid expected to increase from 55 million to 105 million by 201928. However, as highlighted in this and other analyses, Medicaid insurance in its current form was associated with poorer cancer outcomes compared to traditional insurance. Therefore, expansion of the current form of Medicaid may be insufficient. Medicaid may require significant reform, as recently recommended by the American Society of Clinical Oncology, to reduce the significant morbidity and mortality associated with cancer diagnoses29. Furthermore, the ACA will likely result in an increase in insurance availability to previously uninsured cancer survivors; however, 21% of uninsured cancer survivors in non-expansion states will remain without coverage4. A recent survey found 27% of childhood cancer survivors reported familiarity with the ACA and only 21% believed it would help them get high quality coverage30. In addition, another study found survivors of adolescent and young adult cancers were more likely to report forgoing care due to high cost, compared to controls31. Thus, strategies to improve understanding of the ACA, and improve access and reduce cost burdens should be developed to strengthen the impact of expansion of insurance coverage to young men diagnosed with testicular cancer on their overall future health. We were unable to examine the impact of the ACA insurance expansion on disease presentation and outcomes in men with testicular germ cell tumors, but future research should.
There are a few limitations that should be considered. First, SEER does not release information on chemotherapy, which is a crucial component of treatment for germ cell tumors. While this information is available in other databases (e.g., SEER-Medicare), germ cell tumors are significantly more rare in older men. Similarly, although the National Cancer Database provides detailed treatment information, including chemotherapy, it does not have survival data. When this study began insurance status data in SEER was only available between 2007–2011, thus limiting follow-up time for survival analyses. However, nearly all GCT deaths occur within 2 years of diagnosis. In addition, SEER does not include individual-level information on insurance plans and lumping different plans together into ‘insured’ may have led to some misclassification of the exposure in addition to the possible misclassification of Medicaid mentioned above. Finally, the variables for income and education in SEER are based on county-level data, not individual, which may have led to misclassification of these socioeconomic variables, although both higher levels of education and income are associated with health insurance coverage and health insurance type1.
In conclusion, in this study we found that traditional health insurance—but not Medicaid insurance—was associated with earlier stage of disease at diagnosis, increased treatment, and better survival among men diagnosed with germ cell tumors in this large, population-based study. Our results suggest that increasing access to health care is required to decrease the deaths of young men with GCT, a disease that is curable even when metastatic. Further research into the role of insurance status and adverse outcomes will be necessary with the uptake of the ACA and expanded insurance coverage, particularly for those most at risk for germ cell tumors.
Supplementary Material
Acknowledgments
SCM is supported by the National Cancer Institute at the National Institutes of Health (NCI) Training Grant NIH T32 CA09001 and AAW is supported by an NCI K07 CA166210.
Footnotes
Author Contributions: Sarah C. Markt: Conceptualization, methodology, software, formal analysis, data curation, writing – original draft, writing – review and editing, visualization, supervision, and project administration. Carlos A. Lago-Hernandez: Conceptualization, methodology, software, writing – review and editing, and visualization. Rowan E. Miller: Conceptualization, methodology, writing – review and editing, visualization, and supervision. Brandon Mahal: Conceptualization, methodology, writing – review and editing, visualization, and supervision. Brandon Bernard: Conceptualization, methodology, writing – review and editing, visualization, and supervision. Laurence Albiges: Conceptualization, methodology, writing – review and editing, visualization, and supervision. Lindsay Frazier: Conceptualization, methodology, writing – review and editing, visualization, and supervision. Clair Beard: Conceptualization, methodology, writing – review and editing, visualization, and supervision. Alexi A. Wright: Conceptualization, methodology, writing – original draft, writing – review and editing, visualization, supervision, and project administration. Christopher J. Sweeney: Conceptualization, methodology, writing – original draft, writing – review and editing, visualization, supervision, project administration, and funding acquisition.
All authors report no conflicts of interest to disclose
References
- 1.Smith JCaMC. Health Insurance Coverae in the United States: 2013. Washington, DC: U.S. Government Printing Office; 2014. [Google Scholar]
- 2.Howlader NNA, Krapcho M, Garshell J, Miller D, Altekruse SF, Kosary CL, Yu M, Ruhl J, Tatalovich Z, Mariotto A, Lewis DR, Chen HS, Feuer EJ, Cronin KA, editors. SEER Cancer Statistics Review, 1975–2011. National Cancer Institute; http://seer.cancer.gov/csr/1975_2011/ [Google Scholar]
- 3.Moy B, Polite BN, Halpern MT, et al. American Society of Clinical Oncology policy statement: opportunities in the patient protection and affordable care act to reduce cancer care disparities. Journal of clinical oncology : official journal of the American Society of Clinical Oncology. 2011;29(28):3816–3824. doi: 10.1200/JCO.2011.35.8903. [DOI] [PubMed] [Google Scholar]
- 4.Davidoff AJ, Hill SC, Bernard D, Yabroff KR. The Affordable Care Act and Expanded Insurance Eligibility Among Nonelderly Adult Cancer Survivors. J Natl Cancer Inst. 2015;107(9) doi: 10.1093/jnci/djv181. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Robbins AS, Lerro CC, Barr RD. Insurance status and distant-stage disease at diagnosis among adolescent and young adult patients with cancer aged 15 to 39 years: National Cancer Data Base, 2004 through 2010. Cancer. 2014;120(8):1212–1219. doi: 10.1002/cncr.28568. [DOI] [PubMed] [Google Scholar]
- 6.Walker GV, Grant SR, Guadagnolo BA, et al. Disparities in stage at diagnosis, treatment, and survival in nonelderly adult patients with cancer according to insurance status. Journal of clinical oncology : official journal of the American Society of Clinical Oncology. 2014;32(28):3118–3125. doi: 10.1200/JCO.2014.55.6258. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Aizer AA, Falit B, Mendu ML, et al. Cancer-specific outcomes among young adults without health insurance. Journal of clinical oncology : official journal of the American Society of Clinical Oncology. 2014;32(19):2025–2030. doi: 10.1200/JCO.2013.54.2555. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Rosenberg AR, Kroon L, Chen L, Li Ci, Jones B. Insurance status and risk of cancer mortality among adolescents and young adults. doi: 10.1002/cncr.29187. LID [doi]. (1097-0142 (Electronic)) [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Kamel MH, Elfaramawi M, Jadhav S, Saafan A, Raheem OA, Davis R. Insurance Status and Differences in Treatment and Survival of Testicular Cancer Patients. Urology. 2015 doi: 10.1016/j.urology.2015.06.059. [DOI] [PubMed] [Google Scholar]
- 10.Medicaid.gov. Affordable Care Act. 2015 http://www.medicaid.gov/affordablecareact/affordable-care-act.html.
- 11.Gray PJ, Lin CC, Sineshaw H, Paly JJ, Jemal A, Efstathiou JA. Management trends in stage I testicular seminoma: Impact of race, insurance status, and treatment facility. Cancer. 2015;121(5):681–687. doi: 10.1002/cncr.29094. [DOI] [PubMed] [Google Scholar]
- 12.Lerro CC, Robbins AS, Fedewa SA, Ward EM. Disparities in stage at diagnosis among adults with testicular germ cell tumors in the National Cancer Data Base. Urol Oncol. 2014;32(1):23 e15–21. doi: 10.1016/j.urolonc.2012.08.012. [DOI] [PubMed] [Google Scholar]
- 13.Bradley CJ, Gardiner J, Given CW, Roberts C. Cancer, Medicaid enrollment, and survival disparities. Cancer. 2005;103(8):1712–1718. doi: 10.1002/cncr.20954. [DOI] [PubMed] [Google Scholar]
- 14.Farkas DT, Greenbaum A, Singhal V, Cosgrove JM. Effect of insurance status on the stage of breast and colorectal cancers in a safety-net hospital. J Oncol Pract. 2012;8(3 Suppl):16s–21s. doi: 10.1200/JOP.2012.000542. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Ward E, Halpern M, Schrag N, et al. Association of insurance with cancer care utilization and outcomes. CA Cancer J Clin. 2008;58(1):9–31. doi: 10.3322/CA.2007.0011. [DOI] [PubMed] [Google Scholar]
- 16.Zippin C, Lum D, Hankey BF. Completeness of hospital cancer case reporting from the SEER Program of the National Cancer Institute. Cancer. 1995;76(11):2343–2350. doi: 10.1002/1097-0142(19951201)76:11<2343::aid-cncr2820761124>3.0.co;2-#. [DOI] [PubMed] [Google Scholar]
- 17.National Cancer Institute. Surveillance, Epidemiology, and End Results Program: SEER data, 1973–2010. http://seer.cancer.gov/data/
- 18.Surveillance, Epidemiology, and End Results (SEER) Program (http://www.seer.cancer.gov) SEER*Stat Database: Incidence - SEER 9 Regs Research Data, Nov 2013 Sub (1973–2011) <Katrina/Rita Population Adjustment> - Linked To County Attributes - Total U.S., 1969–2012 Counties, National Cancer Institute, DCCPS, Surveillance Research Program, Surveillance Systems Branch, released April 2014, based on the November 2013 submission.
- 19.United States Census Bureau. Census 2000 Gateway.
- 20.United States Department of Agriculture. Rural-Urban Continuum Codes. http://www.ers.usda/gov/data-products/rural-urban-continuum-codes.aspx.
- 21.Fine JP, Gray RT. A Proportional Hazards Model for the Subdistribution of a Competing Risk. Journal of the American Statistical Association. 1999;94(446):496–509. [Google Scholar]
- 22.Rosenbaum PR, Rubin DB. Reducing Bias in Observational Studies Using Subclassification on the Propensity Score. J Am Stat Assoc. 1984;79(387):516–524. [Google Scholar]
- 23.McWilliams JM, Meara E, Zaslavsky AM, Ayanian JZ. Health of previously uninsured adults after acquiring Medicare coverage. JAMA. 2007;298(24):2886–2894. doi: 10.1001/jama.298.24.2886. [DOI] [PubMed] [Google Scholar]
- 24.McWilliams JM, Zaslavsky AM, Meara E, Ayanian JZ. Impact of Medicare coverage on basic clinical services for previously uninsured adults. JAMA. 2003;290(6):757–764. doi: 10.1001/jama.290.6.757. [DOI] [PubMed] [Google Scholar]
- 25.Sommers BD, Gunja MZ, Finegold K, Musco T. Changes in Self-reported Insurance Coverage, Access to Care, and Health Under the Affordable Care Act. JAMA. 2015;314(4):366–374. doi: 10.1001/jama.2015.8421. [DOI] [PubMed] [Google Scholar]
- 26.Sommers BD, Long SK, Baicker K. Changes in mortality after Massachusetts health care reform: a quasi-experimental study. Ann Intern Med. 2014;160(9):585–593. doi: 10.7326/M13-2275. [DOI] [PubMed] [Google Scholar]
- 27.Schoen C, Doty MM, Robertson RH, Collins SR. Affordable Care Act reforms could reduce the number of underinsured US adults by 70 percent. Health Aff (Millwood) 2011;30(9):1762–1771. doi: 10.1377/hlthaff.2011.0335. [DOI] [PubMed] [Google Scholar]
- 28.Iglehart J. Medicaid expansion offers solutions, challenges. Health Aff (Millwood) 2010;29(2):230–232. doi: 10.1377/hlthaff.2010.0010. [DOI] [PubMed] [Google Scholar]
- 29.Polite BN, Griggs JJ, Moy B, et al. American Society of Clinical Oncology policy statement on medicaid reform. Journal of clinical oncology : official journal of the American Society of Clinical Oncology. 2014;32(36):4162–4167. doi: 10.1200/JCO.2014.56.3452. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 30.Park ER, Kirchhoff AC, Perez GK, et al. Childhood Cancer Survivor Study participants’ perceptions and understanding of the Affordable Care Act. Journal of clinical oncology : official journal of the American Society of Clinical Oncology. 2015;33(7):764–772. doi: 10.1200/JCO.2014.58.0993. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 31.Kirchhoff AC, Lyles CR, Fluchel M, Wright J, Leisenring W. Limitations in health care access and utilization among long-term survivors of adolescent and young adult cancer. Cancer. 2012;118(23):5964–5972. doi: 10.1002/cncr.27537. [DOI] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.


