Highlights
-
•
Trichobezoar is a rare clinical entity in which a ball of hair amasses within the alimentary tract, mainly in stomach.
-
•
Trichobezoars should be suspected in young females with long standing upper abdominal masses; as the possibility of malignancy is not very common in this age group.
-
•
While ultrasound is inconclusive, trichobezoar can be accurately diagnosed with computed tomography.
-
•
Convenient approach of treatment should be selected depending on the size and site of trichobezoars followed by psychiatric consultations in order to prevent its relapses.
Keywords: Trichobezoar, Gastric mass, Laparotomy
Abstract
Introduction
Trichobezoar is a rare clinical entity in which a ball of hair amasses within the alimentary tract. It can either be found as isolated mass in the stomach or may extend into the intestine. Trichobezoars mostly occur in young females with psychiatric disorders such as trichophagia and trichotillomania.
Case report
Authors present a giant trichobezoar in an 18 year old female presented with complaints of upper abdominal mass, epigastric area pain, anorexia and weight loss. The patient underwent trans-abdominal ultrasonography (USG), Computed tomography (CT), upper gastrointestinal endoscopy and subsequently laparotomy.
USG was inconclusive due to non-specific findings. It revealed a thick echogenic layer with posterior dirty shadowing extending from the left sub-diaphragmatic area to the right sub hepatic region obscuring the adjacent structures. Abdominal CT images revealed a huge, well defined, multi-layered, heterogeneous, solid appearing, non-enhancing mass lesion in the gastric lumen extending from the gastric fundus to the pyloric canal. An endoscopic attempt was performed for removal of this intraluminal mass, but due to its large size, and hard nature, the endoscopic removal was unsuccessful. Finally the large trichobezoar was removed with open laparotomy.
Conclusion
Trichobezoars should be suspected in young females with long standing upper abdominal masses; as the possibility of malignancy is not very common in this age group. While USG is inconclusive, trichobezoar can be accurately diagnosed with CT. In patient with huge trichobezoar, laparotomy can be performed firstly because of big size and location of mass, and psychiatric recommendation should be made to prevent relapse of this entity.
1. Introduction
A bezoar is collection of undigested foreign bodies inside the gastrointestinal tract. It has four types based on its content; trichobezoar consists of hair, Phytobezoar comprises undigested fruit and vegetable fibers, Lactobezoar has milk and Pharmacobezoar contains medications [1]. The main cause of trichobezoar formation is the resistance of human hair to peristalsis and digestion [2]. The continuous ingestion of hair together with food particles increases its volume producing symptoms such as abdominal pain, abdominal distension and vomiting. Untreated cases may result in serious complications like gastric erosion and ulceration, gastric and small bowel perforation, gastric outlet obstruction, pancreatitis, obstructive jaundice, protein-losing enteropathy, intussusception and death [3].
Herein we aimed to present an interesting case of this rare entity diagnosed with sonography, computed tomography and endoscopy and subsequently treated with laparotomy.
2. Case presentation
A 18 years old, unmarried female presented with large and hard upper abdominal mass. She complained from dull abdominal pain, anorexia and weight loss for last 4 years.
The patient had abnormal gait since birth. No specific psychiatric history was given. The patient denied trichophagia. Her previous medical and surgical records were insignificant.
On physical examination the patient looked pale with lean body mass. A giant, firm and hard mass was palpated in the epigastric and right hypochondriac regions.
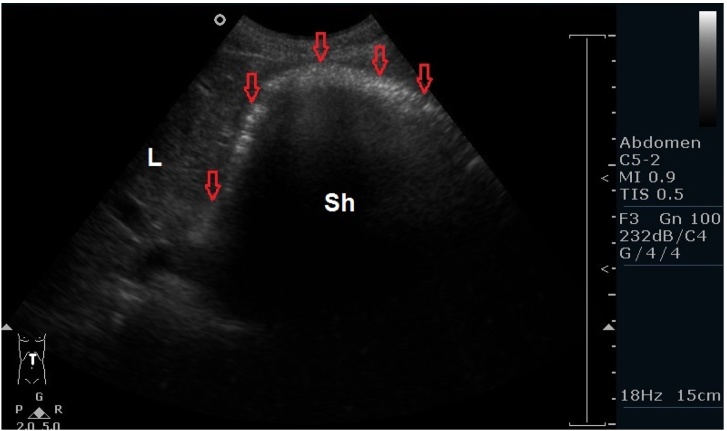
The patient underwent abdominal ultrasonography (USG). USG demonstrated a large area of abnormal thick echogenicity with dirty posterior shadowing extending from the left sub diaphragmatic area to the right sub hepatic region (Fig. 1). Due to extensive posterior shadowing, the exact size, internal texture and extent of the mass lesion could not be assessed with USG. The patient subsequently underwent contrast enhanced abdominal Computed Tomography (CT) examination with 128 slice Siemens scanner.
Fig. 1.
Trans-abdominal ultrasound: Large abnormal thick echogenicity (Red open arrows) with dirty posterior shadowing (Sh) extending from the left sub diaphragmatic area to the right sub hepatic region. Due to extensive posterior shadowing the exact size, internal texture and extent of the mass lesion cannot be assessed. L = liver, Sh = Shadow.
The CT images revealed a huge, well defined, multi-layered, heterogeneous, solid appearing, non-enhancing mass in the gastric lumen extending from the gastric fundus to the pyloric canal. Some of the layers of this mass were heterogeneously hyperdense (Fig. 2a). The mass lesion was separated from the gastric walls by gastric fluid. No evidence of abnormal gastric mural thickening was noted. This abnormal mass did not extend from the pyloric canal into the duodenum. (Fig. 2b) The large mass lesion measured 27 × 10 × 15 cm in size. Rest of the abdominal organs were normal.
Fig. 2.
a) Contrast enhanced CT, Coronal view: Huge, well defined, multi-layered, heterogeneous, solid appearing, non-enhancing mass in the gastric lumen extending from the gastric fundus to the pyloric canal. Some of the layers of the mass are heterogeneously hyperdense. The mass lesion with separated from the gastric walls by gastric fluid. No evidence of abnormal gastric mural thickening. b) Contrast enhanced CT, sagittal view at the level of pyloric canal: No passage of the large mass lesion is noted through the pyloric canal (Open arrow to the duodenum (D). D- Duodenum.
Review of the bony skeleton revealed incidental finding of left sided untreated severe developmental dysplasia of the hip joint.
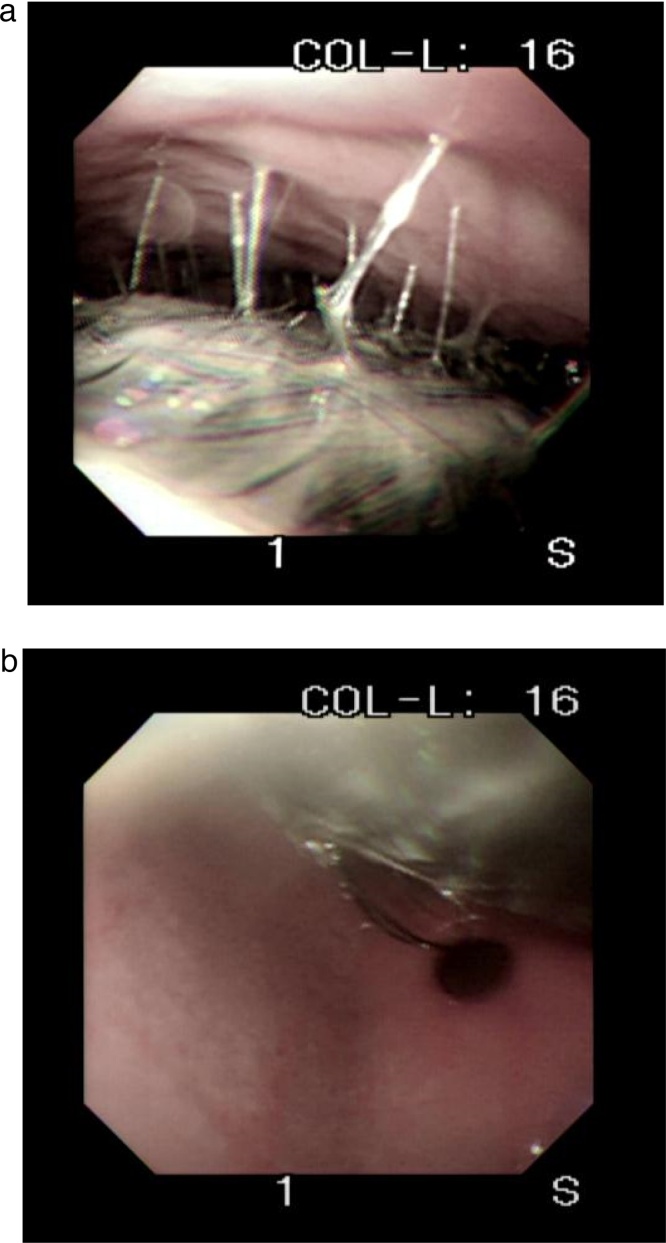
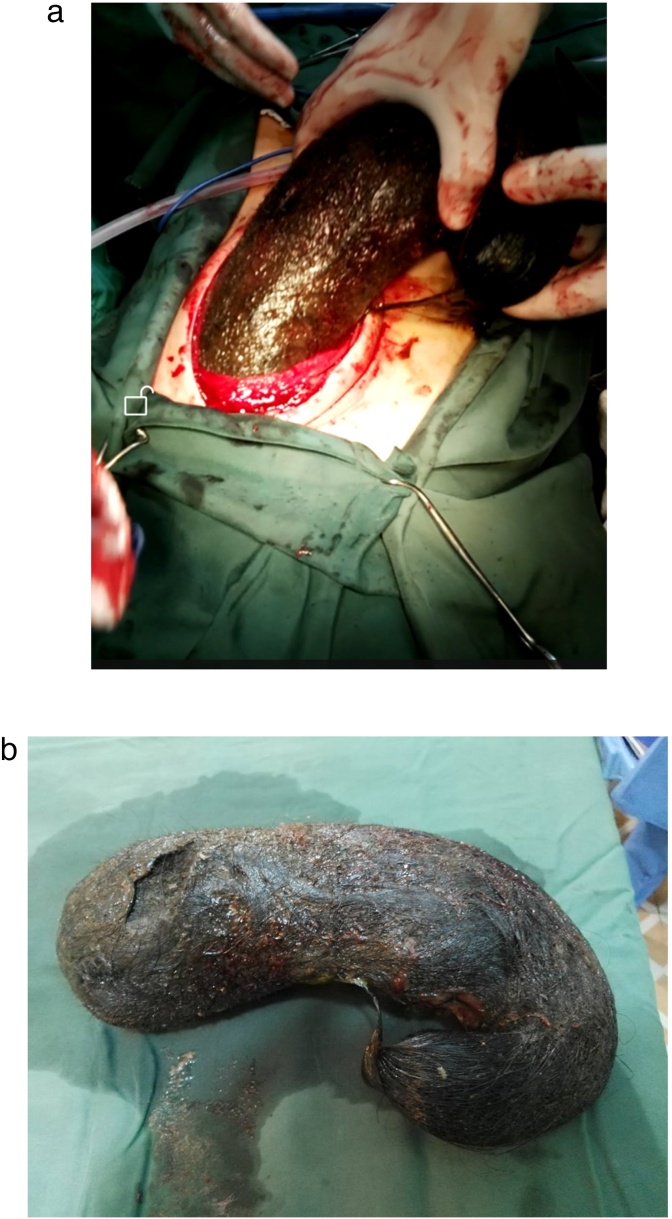
Endoscopy revealed a collection of large black and hard hair ball occupying entire lumen of stomach from fundus up to pylorus. The scope passed with difficulty in the space between the hair ball and stomach to the pyloric region (Fig. 3a). Endoscopy confirmed the absence of trichobezoar’s extension into duodenum through pyloric canal (Fig. 3b). An attempt was made to remove the huge mass, but due to its large size and hard nature, we failed to excise and remove it. Following failed attempt at endoscopic removal, we elected to perform a laparotomy. A 10 cm upper midline incision was made. A large solid mass was palpated in fixed location of the stomach. Anterior wall of the stomach was incised parallel to the greater curvature nearly from fundus to pyloric area. After digital examination a huge trichobezoar was excised (Fig. 4a). The stomach was repaired in two layers with continuous 3.0 Vicryl. The abdominal incision was closed in two layers with 1.0 absorbable suture and skin was closed with stapler. Total operation time was 70 min. Weight of bezoar was 6.20 kg (Fig. 4b).
Fig. 3.
a) Endoscopy revealed a large black and hard hair ball occupying entire lumen of stomach from fundus up to pylorus. The scope passed with difficulty in the space between the hair ball and stomach wall. b) Endoscopy confirms no passage of the mass through the pyloric canal to the duodenum. The pyloric canal is open.
Fig. 4.
a) Huge, intra-luminal solid mass lesion excised from the stomach. b) Huge, intra-luminal solid mass lesion excised from the stomach.
The postoperative course was uneventful and the patient was discharged on 8th post-operative day in stable condition. The patient's parents were advised a psychiatric consultation for patient to avoid recurrence of her condition.
3. Discussion
Trichobezoars are the second most common bezoars after phytobezoars. Swain reported human trichobezoars in a post mortem case for the first time in 1854 [2] and the first surgical removal was performed by Schonbern in 1883 [4].
Debakey and Oshner revealed that 90% of trichobezoars occur in females and 80% of these cases occur before 30 years of age [5]. Trichobezoars are predominantly found in young females with psychiatric disorders [6] however they can also be found in postsurgical cases; post-partial gastrectomy, post-vagotomy, patients with diabetes mellitus related gastroparesis, GuillaineBarre’s syndrome, myotonic dystrophy, hypothyroidism and cretinism [7]. Trichobezoars are most commonly found in the stomach but in approximately 10 percent of cases they extend into small bowel and even into colon [8], [9].
As hair is indigestible in gastrointestinal tract, it accumulates within the alimentary tract mostly in the stomach. Due to the denaturation of proteins in acidic gastric juice, the ingested hairs become black colored irrespective of their original color [10]. The hair together with ingested food and trapped air increases the volume of the mass and gives the mottled appearance to the trichobezoar visible on CT. The mass may enlarge and cause gastric outlet obstruction or it may extend distally into the bowel loops. Extension of the bezoar from the stomach into the jejunum or further into bowel is referred to as “Rapunzel syndrome” [8].
More than 80% of the Patients with trichobezoars present with palpable abdominal mass. Approximately 80% of patients have epigastric discomfort, up to 70% complain of abdominal pain, 65% complain of nausea and vomiting, 38% have asthenia with weight loss and 33% of patients have intestinal transit problems like diarrhea or constipation [11].
Untreated cases can result in harmful complications such as upper gastrointestinal hemorrhage, gastric or duodenal perforation, peritonitis, sub-phrenic abscess, digestive fistula, acute pancreatitis and obstructive jaundice [12].
Imaging plays an important role in the diagnosis of trichobezoar. USG used as the first line imaging modality for the evaluation of Intra-abdominal masses provides limited information regarding trichobezoar. This is because of high echogenicity of hair and multiple acoustic reflections of trapped air bubbles [13]. USG can demonstrate curved echogenic layer with a posterior shadow [14]. Upper gastrointestinal series may show a large filling defect in the stomach, occasionally extending into the small bowel [9]. Abdominal CT scan is the preferred modality for evaluation of suspected cases of trichobezoar. It can depict an intraluminal, well-demarcated, heterogeneous, non-enhancing mass with mottled appearance due to the entrapped air among the hair ball [15]. It can depict the exact size, site and extent of the lesion. It can also give detailed information about simultaneous abnormalities and complications. No specific advantage of Magnetic resonance imaging over computed tomography is described in the literature in detection of trichobezoar [16]. Upper gastrointestinal endoscopy cannot only visualize the mass, but also determine its extension beyond pylorus (As per our case) and in suspicious cases, sample of the mass can be also be taken.
Once diagnosed, trichobezoar needs immediate surgery as it can ensue in a number of harmful events. The treatment approaches include endoscopic removal (which may involve fragmentation using electrohydraulic lithotripsy, tripod forceps), chemical dissolution, laparoscopic removal or laparotomy depending on the size and site of trichobezoar [6]. What leads to recurrences of this condition is the negligence paid to the major triggering factor which is the psychiatric condition of the patients. Patients with trichophagia and trichotillomania along with other psychopathological problems should undergo behavioral therapy [17]. Parental counselling can help in prevention of relapses [18]. Prognosis of trichobezoars is quite good only if psychiatric follow-up is strictly maintained [19], [20], therefore psychiatric follow-up should be made a compulsory part of the management.
4. Conclusion
Trichobezoars should be suspected in young females with long standing upper abdominal masses; as the possibility of malignancy is not very common in this age group. While ultrasound is inconclusive, trichobezoar can be accurately diagnosed with computed tomography. Authors present the diagnostic work up and laparotomy approach to a huge trichobezoar in an 18 years old girl.
Competing interests
Authors declare that no competing interest exists.
Funding
No funding source exists.
Ethical approval
The article has got approval of exemption from Ethical Review Committee of French Medical institute for Children, as case reports are exempted from ethical review according to this institute’s policy.
Consent
Written informed consent was obtained from the patient for publication of this case report and accompanying images. A copy of the written consent is available for review by the Editor-in-Chief of this journal on request.
Author contribution
Dr Hidayatullah hamidi: The main concept of paper, providing USG and Ct images and communication between authors.
Dr Marzia Muhammadi: Review of literature, writing the template of paper.
Dr Bismillah Saberi: Endoscopic findings and images.
Dr Mohammad Arif Sarwari: Surgical findings and images.
Guarantor
Hidayatullah Hamidi.
References
- 1.Ibuowo A.A., Saad A., Okonkwo T. Giant gastric trichobezoar in a young female. Int. J. Surg. 2008;6(6):e4–e6. doi: 10.1016/j.ijsu.2006.08.004. [DOI] [PubMed] [Google Scholar]
- 2.Mewa Kinoo S., Singh B. Gastric trichobezoar: an enduring intrigue. Case Rep. Gastrointest. Med. 2012;2012 doi: 10.1155/2012/136963. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Ahmad Z., Sharma A., Ahmed M., Vatti V. Trichobezoar causing gastric perforation: a case report. Iran. J. Med. Sci. 2016;41(1):67. [PMC free article] [PubMed] [Google Scholar]
- 4.Kadian R., Rose J., Mann N.S. Gastric bezoars–spontaneous resolution*. Am. J. Gastroenterol. 1978;70(1):s1. [PubMed] [Google Scholar]
- 5.Duke D.C., Keeley M.L., Geffken G.R., Storch E.A. Trichotillomania: a current review. Clin. Psychol. Rev. 2010;30(2):181–193. doi: 10.1016/j.cpr.2009.10.008. [DOI] [PubMed] [Google Scholar]
- 6.Czerwińska K., Bekiesińska-Figatowska M., Brzewski M., Gogolewski M., Wolski M. Trichobezoar, rapunzel syndrome, tricho-plaster bezoar-a report of three cases. Pol. J. Radiol. Pol. Med. Soc. Radiol. 2014;80:241–246. doi: 10.12659/PJR.893478. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Andrus C.H., Ponsky J.L. Bezoars: classification, pathophysiology, and treatment. Am. J. Gastroenterol. 1988;83(5) [PubMed] [Google Scholar]
- 8.Jensen A.R., Trankiem C.T., Lebovitch S., Grewal H. Gastric outlet obstruction secondary to a large trichobezoar. J. Pediatr. Surg. 2005;40(8):1364–1365. doi: 10.1016/j.jpedsurg.2005.05.021. [DOI] [PubMed] [Google Scholar]
- 9.Hoover K., Piotrowski J., Pierre K.S., Katz A., Goldstein A.M. Simultaneous gastric and small intestinal trichobezoars—a hairy problem. J. Pediatr. Surg. 2006;41(8):1495–1497. doi: 10.1016/j.jpedsurg.2006.04.003. [DOI] [PubMed] [Google Scholar]
- 10.Khattak S., Kamal A., Trichobezoar Gomal J. Med. Sci. 2004;2(1) [Google Scholar]
- 11.Ersoy Y., Ayan F., Ayan F., Ersan Y. Gastro-intestinal bezoars: thirty-five years experience. Acta Chir. Belg. 2009;109(2):198–203. doi: 10.1080/00015458.2009.11680405. [DOI] [PubMed] [Google Scholar]
- 12.Balik E., Ulman I., Taneli C., Demircan M. The Rapunzel syndrome: a case report and review of the literature. Eur. J. Pediatr. Surg. 1993;3(03):171–173. doi: 10.1055/s-2008-1063536. [DOI] [PubMed] [Google Scholar]
- 13.McCracken S., Jongeward R., Silver T.M., Jafri S. Gastric trichobezoar: sonographic findings. Radiology. 1986;161(1):123–124. doi: 10.1148/radiology.161.1.3532177. [DOI] [PubMed] [Google Scholar]
- 14.Ripollés T., García-Aguayo J., Martínez M.-J., Gil P. Gastrointestinal bezoars: sonographic and CT characteristics. Am. J. Roentgenol. 2001;177(1):65–69. doi: 10.2214/ajr.177.1.1770065. [DOI] [PubMed] [Google Scholar]
- 15.West W.M., Duncan N.D. CT appearances of the Rapunzel syndrome: an unusual form of bezoar and gastrointestinal obstruction. Pediatr. Radiol. 1998;28(5):315–316. doi: 10.1007/s002470050362. [DOI] [PubMed] [Google Scholar]
- 16.Hernández-Peredo-Rezk G., Escárcega-Fujigaki P., Campillo-Ojeda Z.V., Sánchez-Martínez M.E., Rodríguez-Santibáñez M.A., Ángel-Aguilar A.D. Trichobezoar can be treated laparoscopically. J. Laparoendosc. Adv. Surg. Tech. 2009;19(1):111–113. doi: 10.1089/lap.2008.0068. [DOI] [PubMed] [Google Scholar]
- 17.Grant J.E., Odlaug B.L. Clinical characteristics of trichotillomania with trichophagia. Compr. Psychiatry. 2008;49(6):579–584. doi: 10.1016/j.comppsych.2008.05.002. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.El-Mazary A.-A.M., Ahmed M.F., Hasanin A., Abdel-Hamed W.M. 2014. Rapunzel Syndrome in a 7-year-old Egyptian Girl with Primary Biliary Cirrhosis: A Case Report and Literature Review. [Google Scholar]
- 19.Tiwary S., Kumar S., Khanna R., Khanna A. Recurrent rapunzel syndrome. Singapore Med. J. 2011;52(6):e128–e130. [PubMed] [Google Scholar]
- 20.Kırpınar İ, Kocacenk T., Koçer E., Memmi N. Recurrent trichobezoar due to trichophagia: a case report. Gen. Hosp. Psychiatry. 2013;35(4):439–441. doi: 10.1016/j.genhosppsych.2013.01.013. [DOI] [PubMed] [Google Scholar]