Abstract
Objectives
Favorable attitudes, emotions, personality characteristics, and self-rated health have been associated with successful aging in late life. However, less is known regarding these constructs and their relationships to mental health outcomes in the oldest old persons. This study examined cross-sectional relationships of these psychological factors to depressive symptoms in centenarians and near-centenarians.
Methods
A selected sample of Ashkenazi Jewish older adults ages 98 to 107 (n = 54, 78% female) without significant cognitive impairment participated. Cognitive function was assessed by Mini Mental Status Exam (MMSE), Positive Attitude Towards Life and Emotional Expression by the Personality Outlook Profile Scale (POPS), self-rated health by participants’ subjective rating of their present health, and depressive symptoms by the Geriatric Depression Scale (GDS).
Results
Results demonstrated inverse associations of the Positive Attitude Towards Life domain of the POPS and self-rated health with participants’ levels of depressive symptoms even after adjusting for the effects of history of medical illnesses, cognitive function, and demographic variables. Additionally, participants with high levels of care showed higher levels of depressive symptoms. Path analysis supported the partially mediating role of Positive Attitude Towards Life in the relationship between self-rated health and depressive symptoms.
Conclusion
These findings emphasized the important roles of positive attitudes and emotions as well as self-rated health in mental health outcomes in the oldest old. Although, limited by its cross-sectional design, findings suggest these psychological factors may exert protective effects on mental health outcomes in advanced age.
Keywords: Positive attitude, personality, depression, self-rated health, successful aging
Introduction
According to the 2010 Census Special Reports, living to be 100 years of age is still a rare event (1.73 centenarians per 10,000 residents in the U.S). However, the number of centenarians has been rapidly increasing at a rate of 8% per year in the U.S. (Perls, 2008). Centenarians are considered to be a model for successful aging as they have delayed or escaped major illnesses (Jeune, 2002), yet, they represent a diverse group in regard to characteristics of behavior, functional status, environments and contributors to their longevity (Poon & Perls, 2008).
Positive psychology has emphasized the value of positive attitudes and emotions to successful aging (Ruch, Proyer, & Weber, 2010). Centenarians have been reported to have favorable emotional characteristics and personality including being more easygoing, relaxed, and efficient but less likely to be anxious as compared to the normal adult population (Samuelsson et al., 1997). Similarly, a qualitative study with community-dwelling centenarians and near-centenarians in Hong Kong emphasized the importance of positive life attitudes, relationships, and events as well as happiness and hopefulness in emotional well-being (Wong et al., 2014).
In younger older adults, positive attitudes and affect have been linked to successful aging possibly due to their protective function against disease, depression, and disability. For example, positive attitudes and ability to adapt to change were reported to compensate for physical impairment (Reichstadt, Depp, Palinkas, Folsom, & Jeste, 2007). Another study showed that happiness, laughter, and humor led to better bereavement adjustment and reduced depressive symptoms (Lund, Utz, Caserta, & De Vries, 2008). Among the disabled elderly in Taiwan, positive attitudes toward disability through the use of positive coping strategies (e.g., acceptance-action coping), active self-management skills, and external resources was associated with successful adaptation and emotional well-being (Hsu & Tung, 2010). Additionally, older adults with higher positive affect were associated with more daily walking despite osteoarthritis while those with higher depressive symptoms showed less daily walking (White et al., 2012). Therefore, tendency toward positive attitudes and affect seem to represent a protective factor against depression, disability, and pain through engaging in positive coping strategies and healthy behaviors. Specifically, attitudes have been reported to predict future behavior by a number of studies (Glasman & Albarracin, 2006).
Interestingly, centenarians who have maintained exceptional longevity have been reported to have higher levels of positive attitudes and life satisfaction as compared to young-older adults (Dello Buono, Urciuoli, & De Leo, 1998). Further, findings from personality research have consistently demonstrated that centenarians have favorable emotional and personality characteristics. Our previous study examined cross-sectional personality traits using the NEO-Five Factor Inventory (NEO-FFI: Costa & McCrae, 1995) in a sample of Ashkenazi Jewish centenarians, and findings showed that centenarians demonstrated lower levels of neuroticism and higher levels of conscientiousness than the US population norms (Kato, Zweig, Barzilai, & Atzmon, 2012). Similarly, Martin and colleagues (2006) investigated cross-sectional personality characteristics using of the NEO Personality Inventory (NEO-PI: Costa & McCrae, 1995) among centenarians and found that they have lower levels of neuroticism and higher levels of extraversion as compared to the U.S. population norms (Martin et al., 2006).
Attitude has been a well-studied construct in the social and behavioral sciences; however, its relation to health outcome and successful aging has not been well investigated. Attitude refers to a summary evaluation of an object which includes attribute dimensions (e.g., good-bad, pleasant-unpleasant). Attitude is related to personality as it is a bi-product of cognition, affect, and behaviors. The expectancy-value model of attitude suggests that the evaluative function of attitude arises automatically from an individual's beliefs about certain objects. Also, affect has been suggested to be the antecedent of evaluation as affective states may influence the evaluative quality (Ajzen, 2001). Some propose that attitude can be dispositional and stable over time and may represent aspects of personality as it involves an individual's long-held inherent affective and cognitive characteristics (Wilson et al., 2000). As personality refers to a relatively stable set of cognitive-motivational and social emotional traits and behavioral patterns (McCrae & Costa, 1990), we speculate that attitude, particularly dispositional attitude, can be closely related to personality. Our previous study showed the relationship between Positive Attitude Towards Life, positive emotional characteristics, and personality traits in a small sample of Ashkenazi Jewish centenarians. More specifically, the oldest old persons, who were more optimistic, easygoing, outgoing and considered laugher more important, showed higher levels of favorable personality traits including emotional stability, extraversion, and conscientiousness of the Five Factor Model(FFM) as well as dispositional optimism of the Life Orientation Test-Revised (Kato, Zweig, Atzmon, & Barzilai, 2012).
Affect is an important aspect of both attitude and personality, which has been associated with health outcomes and longevity/mortality. The long-term health benefit of positive affect has been well demonstrated in previous studies; however, one review emphasized that it is positive affect as a trait, rather than as a state, which has been linked to longevity (Pressman & Cohen, 2005). Positive affect along with subjective well-being and life satisfaction has been reported to predict a lower risk of all-cause mortality in a 28-year longitudinal study (Xu & Roberts, 2010). Other longitudinal studies suggest that positive affect may be beneficial for health outcomes in part because it is closely linked to other protective psychosocial factors and healthy lifestyles (Steptoe, O'Donnell, Marmot, & Wardle, 2008). Personality research has consistently demonstrated the link between favorable personality traits (McCrae & Costa, 1990) and longevity (Kern & Friedman, 2008; Martin et al., 2006; Terracciano, Lockenhoff, Zonderman, Ferrucci, & Costa, 2008; Weiss & Costa, 2005; Wilson et al., 2005; Wilson et al., 2004). For example, higher extraversion has been linked to positive mental health outcomes and positive affect, whereas higher neuroticism has been associated with poor mental health outcomes, negative affect, and depression (Boyd et al., 2000;(de Jonge et al., 2006; Steunenberg, Beekman, Deeg, & Kerkhof, 2006; 2010) as well as early mortality (Wilson, Mendes de Leon, Bienias, Evans, & Bennett, 2004).
Self-rated (or perceived) health, comprised of physical, emotional, and psychosocial aspects of health (Mavaddat et al., 2011), appears to be another important psychological factor as it seems to exert stronger effects than objective medical illness on depression, pain, and daily functioning in older adults (Hampson, Goldberg, Vogt, & Dubanoski, 2006; Mulsant, Ganguli, & Seaberg, 1997; Nutzel et al., 2014). It has also been linked to the FFM traits including neuroticism, extraversion, and conscientiousness (Hampson, Goldberg, Vogt, & Dubanoski, 2006; Lockenhoff, Terracciano, Ferrucci, & Costa, 2012; Mossey, 1995; Svedberg, Gatz, & Pedersen, 2009). Maladaptive personality styles have been shown to contribute to distorted perceptions of health status (Zweig & Agronin, 2011). Further, self-rated health has been associated with depression in mixed-age adults (Herrman et al., 2002; Goldney et al., 2010; Gunn et al., 2012). Specifically, one longitudinal study reported that self-rated health predicted recurrence of major depressive disorder up to five years later (Ambresin et al., 2014). However, the direction of the relationship between self-rated health and depression remains uncertain as depression has also been reported to be a risk factor for subsequent decline in self-rated health (Han & Jylha, 2006). Further, this association may be age-graded, as a meta-analysis showed that the association of self-perceived health with mental health outcomes was stronger in the oldest old as compared to the young-old adults (Pinquart, 2001).
In sum, findings from previous research emphasize an important role of psychological factors including positive attitudes, affect, and favorable personality characteristics in successful aging. Having these characteristics in conjunction with better self-rated health may promote emotional and physical well-being in late life. Therefore, we speculate that positive attitudes and emotional characteristics may contribute to better mental health outcomes; further, as attitudes or emotions may influence an individual's perception of health status, they may have a mediating role in the relationship between self-rated health and depressive symptoms.
Aims
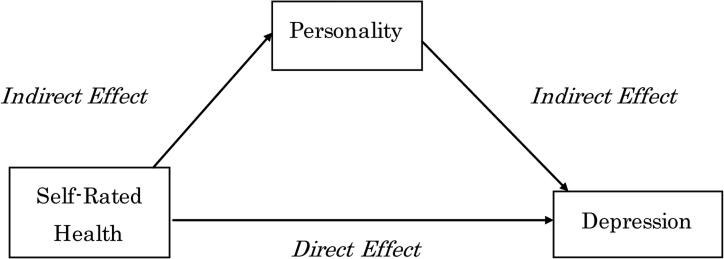
The present study attempted to better understand the role of positive attitudes and emotional expression as well as self-rated health in mental health outcomes through investigating cross-sectional relationships among Positive Attitude Towards Life (PATL), Emotional Expression (EE), self-rated health, and depressive symptoms in a sample of Ashkenazi Jewish centenarians and near-centenarians. It was hypothesized that 1) PATL and EE as assessed by the Personality Outlook Profile Scale (POPS) would be negatively associated with depressive symptoms as assessed by Geriatric Depression Scale (GDS) and that 2) self-rated health would be negatively associated with depressive symptoms after adjusting for the effects of history of medical illnesses, MMSE scores, and demographic variables. Further, it was also hypothesized that 3) PATL and/or EE as assessed by the POPS would mediate the relationship between self-rated health and depressive symptoms as assessed by the GDS after adjusting for the effects of covariates (See the proposed model, Figure 1).
Figure 1.
A Diagram of a Mediation Model of Personality as a Medicating Variable in the Relationship between Self-Rated Health and Depressive Symptoms
Methods
Participants
The present study was based on the analyses of archival data derived from the Longevity Genes Study, in which 357 Ashkenazi Jewish oldest old participants (ages 94-109y) were recruited. Ashkenazi Jews have been a well-studied group for the purposes of gene mapping as well as identifying other factors associated with exceptional longevity due to their genetic as well as socio-cultural homogeneity, although their survival and causes of death are similar to those reported for the majority U.S. population (Barzilai et al., 2003; Rajpathak et al., 2011). Of 357, a sample of 133 centenarians and near-centenarians who were 98 years old or older were selected. 71 participants who scored 23 or less on the MMSE were excluded due to the possible effect of cognitive difficulty on their self-report measures. Cutoff scores of 24 for the general adult population and 21 for centenarians have been recommended to detect dementia (Crum, Anthony, Bassett, & Folstein, 1993;Freudenberg-Hua et al., 2014; Gondo et al., 2006). 8 participants were also excluded from the analyses due to their missing responses. Thus, 54 participants were included in the analyses.
Demographic, psychological, behavioral, and clinical characteristics of the sample are presented in Table 1. Participants’ ages ranged from 98 to 107 with a mean age of 100.13 (SD = 1.85) and were predominantly female (78%). 85% of the participants were widowed, 11% were married/cohabitating, 2% were never married, and 2% were separated or divorced. Years of education ranged from 6 (2%) to 20 years (2%) with a mean level of 13.31 years (SD = 3.01). The MMSE mean score was 28.04 (SD = 2.07). The GDS mean score was 4.67 (SD = 4.01). 35 participants (35%) scored the cut-off score of 5 or higher, which is suggestive of clinically significant depression (Yesavage et al., 1983). Regarding participants’ living arrangements and levels of care, 15% of the sample resided in skilled nursing homes, 41% lived in private home or senior housing with full-time aide, 15% lived in private home or senior housing with part-time aide, and another 29% lived in private home without any aide.
Table 1.
Demographic and Clinical Characteristics of Centenarians (N = 54)
| Variables | Mean ±SD | N(%) | |
|---|---|---|---|
| Age | 100.13±1.85 | ||
| Gender | Males | 12(22) | |
| Females | 42(78) | ||
| Marital Status | Married/Cohabitating | 6(11) | |
| Separated/Divorced | 1(2) | ||
| Widowed | 46(85) | ||
| Never Married | 1(2) | ||
| Years of Education | 13.31±3.01 | ||
| POPS – Personality Domains | PATL (z-score composite) | .17±.64 | |
| Optimism | 3.61±1.19 | ||
| Easygoing | 3.30±1.14 | ||
| Laughter | 3.41±.66 | ||
| Introversion/Outgoing | 4.02±.94 | ||
| EE (z-score composite) | −.05±.82 | ||
| Bottle Up Emotions | 2.57±.94 | ||
| Express Feelings Openly | 2.54±.84 | ||
| GDS | 4.67±4.01 | ||
| MMSE | 28.04±2.07 | ||
| Self-Rated Health | 2.69±.91 | ||
| History of Medical Illnesses | 1.28±1.07 | ||
| Cancer | 23(42) | ||
| Heart Attack | 14(26) | ||
| Stroke/TIA | 7(13) | ||
| Diabetes | 2(4) | ||
| High Blood Pressure | 23(43) | ||
| Living Arrangements | |||
| Nursing Home with Full-Time Skilled Care | 8(15) | ||
| Private Home or Senior Housing with Full-Time Care | 22(41) | ||
| Private Home or Senior Housing with Part-Time Care | 8(15) | ||
| Private Home without Aide or Care | 16(29) | ||
Note. GDS = Geriatric Depression Scale; MMSE = Mini Mental Status Exam; POPS = Personality Outlook Profile Scale; PATL = Positive Attitude Towards Life; EE = Emotional Expression.
Further, the results of the one-way ANOVAs conducted to examine differences between participants and those excluded found that the excluded individuals (N = 148) were younger, 96.61 (SD = 2.26, p < .001) with the lower MMSE mean score (18.79, SD = 12.06, p < .001) and higher GDS mean score (6.15, SD = 4.08, p < .05). Significantly more participants resided in skilled nursing homes (36%), or resided in private home or senior housing but needed full-time care (34%).
Procedure
In the Longevity Genes Study, the participants’ ages were verified by the date of birth on valid birth certificates or passports. A single research nurse visited participants in their homes to obtain a medical history and administer the MMSE. Information about participants’ medical history, demographics, and other characteristics were obtained using the Centenarian Questionnaire (Barzilai et al., 2003). The Centenarian Questionnaire was distributed in person with an instruction to each participant who was asked to complete it with the assistance of their adult children if participants had any physical or sensory difficulties which would interfere in completing self-report measures.
Measures
The Centenarian Questionnaire
The structured 98-item questionnaire, developed by the Longevity Genes Study, measures demographics, personality/psychological characteristics, health/medical history, self-rated health, and health-related behaviors (Barzilai et al., 2003; Kato et al., 2012).
Self-Rated Health
Participants’ current self-rated (perceived) health was assessed by a single-item question “How would you rate your health presently?” with four choices of responses including “Very Good, Good, Average, and Not Good” (Kato, Zweig, Schechter, Verghese, Barzilai, & Atzmon, 2013). Self-rated health has been typically measured by a similar single-item question. A single-item indicator of general self-rated health has shown adequate reliability and validity (Bombak, 2013) and linked to important health outcome including mortality (DeSalvo, Bloser, Reynolds, He, & Muntner, 2006).
The Personality Outlook Profile Scale (POPS)
This is a brief self- and informant-report measure consisting of two domains and six items: Positive Attitude Towards Life (PATL: optimism, easygoing, laughter, and introversion/outgoing) and Emotional Expression (EE: expressing emotions openly and not bottling up emotions). Items were derived from extant longevity research and theoretical concepts and reflected the oldest old persons’ attitudes, emotions, styles of emotional expression, and aspects of personality. In order to assess their characteristics in most of their adulthood, participants were asked about their “general” tendencies (e.g., “In general, how easygoing are you on a scale of 1 to 5?” “In general, do you consider yourself introverted or outgoing on a scale of 1 to 5?”). A composite score of each domain is based on a mean z-score of respective items for each domain, and higher scores reflect more favorable characteristics. These domains showed moderate internal consistency (α =.65 for PATL and α =.63 for EE). Internal consistency findings in this range are within the expected range for scales that are only few items in length (Harlan & Clark, 1999). Further, the POPS was cross-validated with the NEO-FFI and Life Orientation Test-Revised (LOT-R) in self- and informant-report groups. It relates to aspects of the personality traits such as extraversion (r = .72−.82 with PATL, .45 with EE), neuroticism (r = −.51 with EE & −.52 with PATL), and conscientiousness (r = .53 with PATL), as well as dispositional optimism (r = .69 with PATL) (Kato et al., 2012).
Geriatric Depression Scale
The Geriatric Depression Scale (GDS) is a 15-item (short version) self-report measure of depressive symptoms in older adults with well-established reliability (split half reliability, r = .94 & test-retest reliability, r = .85). The internal consistency of the 15-item GDS for oldest olds participants ranged from .64 to .82 (Conradsson et al., 2013). The general cut-off score of 5 has been suggested to detect a clinically significant level of depression (Sheikh & Yesavage, 1986; Yesavage et al., 1983). The 30-item version has also been validated in the centenarian population although it was reported that centenarians might show higher scores on some items reflecting fatigue, cognition, and physical functioning and lower scores on other items including dysphoric mood and worry as compared to the scores of the younger adult population (Scheetz, Martin, & Poon, 2012).
Mini Mental Status Exam (MMSE)
MMSE is a brief measure of cognitive status with sufficient reliability and validity in adults as well as oldest old persons. Its internal consistency has been reported to be between .54 and .96 in the adult population (Tombaugh & McIntyre, 1992). The test-retest reliability in older adults with dementia ranged from .75 to .94 (Folstein, Folstein, & Fanjiang, 2001; Folstein, Folstein, & McHugh, 1975). In this study, if a participant was unable to respond to an item due to any sensory deficits, an extrapolated score was computed by multiplying the obtained score by 30 and dividing by the maximum obtainable score (the possible sum score for all the items that the participant attempted).
History of Medical Illnesses
History of medical illnesses was assessed by self-report affirmative responses to questions about if they ever had (or have been diagnosed with or treated for) cancer, heart attack, stroke/transient ischemic attack, diabetes, and/or high blood pressure, which represent the leading causes of death in the U.S. (Heron, 2007). The composite score of medical illnesses was computed by the summation of participants’ affirmative (yes) responses to questions about whether they had these illnesses.
Statistical Methods
Regression analyses were completed with SPSS Statistics (Version 17.0). Multiple regression analyses were used to evaluate the relationships of the two POPS domains, history of medical illnesses, and self-rated health to the GDS scores. Hierarchical regression analyses were conducted to adjust for the effects of history of medical illnesses, MMSE scores, and demographic variables. Mediation analyses were conducted using Stata Version 13.1MP, wherein a path analysis was used to determine the mediating role (indirect effect) of any POPS domain in the relationship between self-rated health and GDS. Gender (male/female) was included as a two level categorical variable with the female category as the reference category. Marital Status was also included as a four level categorical variable with the first variable (married or cohabitating) as the reference variable. Similarly, living arrangements were included in the analyses as a four level categorical variable with the nursing home category as the reference category.
Results
Associations of the POPS, Self-Rated Health and Depressive Symptoms
Correlation coefficients were computed among GDS, POPS, self-rated health, history of medical illnesses, MMSE, and demographic variables (Table 2). In order to assess the relationships of the POPS domains and self-rated health to depressive symptoms, multiple regression analyses were conducted (Table 3). The results showed that PATL accounted for a significant proportion of the GDS score variability (R2 = .17, β = −.41, p < .01), while EE did not display a significant relationship to the GDS. Further, self-rated health also accounted for a significant proportion of the GDS score variability (R2 = .24, β = −.49, p < .001).
Table 2.
Summary of Correlations among GDS, POPS, Self-Rated Health, History of Medical Illnesses, MMSE, and Demographic Variables
| Variables | 1 | 2 | 3 | 4 | 5 | 6 | 7 | 8 | 9 | 10 |
|---|---|---|---|---|---|---|---|---|---|---|
| 1. GDS | ||||||||||
| 2. PATL | −.41** | |||||||||
| 3. EE | −.06 | −.05 | ||||||||
| 4. Self-Rated Health | −.49*** | .36** | −.02 | |||||||
| 5. Hx of Medical Ill | .10 | −.15 | −.24 | −.24 | ||||||
| 6. MMSE | −.08 | .06 | .31* | .06 | .01 | |||||
| 7. Age | .10 | −.18 | .19 | −.04 | −.05 | .03 | ||||
| 8. Gender | .31* | −.01 | .10 | −.34* | .10 | .18 | .09 | |||
| 9. Education Years | −.13* | −.05 | .07 | .26 | −.09 | −.01 | .11 | −.09 | ||
| 10. Marital Status | −.13 | .10 | −.07 | .01 | .06 | .06 | −.24 | .23 | −.13 | |
| 11. Living Arrangement | −.38** | −.06 | .21 | .10 | −.16 | .20 | −.18 | −.25 | .17 | .19 |
Note. GDS = Geriatric Depression Scale; POPS = Personality Outlook Profile Scale; PATL = Positive Attitude Towards Life; EE = Emotional Expression; Hx of Medical Ill = History of medical illnesses; MMSE = Mini Mental Status Exam; Living Arr = Living arrangement / Levels of Care; SR Health = Self-Rated Health.
p < .05
p < .01
p < .001
Table 3.
Summary of Regression Analysis for POPS and Self-Rated Health Predicting GDS
| IV | R | R2 | B | SEB | β |
|---|---|---|---|---|---|
| PATL | .41 | .17** | −2.55 | .79 | −.41** |
| EE | .06 | .00 | −.27 | .68 | −.06 |
| Self-Rated Health | .49 | . 24*** | −2.15 | .54 | −.49*** |
Note. POPS = Personality Outlook Profile Scale; IV = Independent Variable; PATL = Positive Attitude Towards Life; EE = Emotional Expression; GDS = Geriatric Depression Scale.
*p < .05
p < .01
p < .001
Subsequently, hierarchical regression analyses were conducted to examine the relationships of PATL and self-rated health to GDS scores after adjusting for the effects of demographic variables (age, gender, marital status, education, and living arrangement/levels of care), history of medical illnesses, and MMSE scores. All demographic variables were entered as one group (Step 1); illness-related variables such as history of medical illnesses and MMSE scores were entered as another group (Step2). Then, psychological constructs such as PATL and self-rated health were entered as a group (Step 3). The results of the hierarchical regression analyses (Table 4) showed that the relationships of the PATL and self-rated health to GDS remained significant after adjusting for the effects of demographic variables, history of medical illnesses, and MMSE scores (R2 change = .24, F = 9.77, p < .001). Both PATL and self-rated health accounted for a significant proportion of the GDS score variability (β = −.35, p < .01, & β = .30, p < .05, respectively) even after adjusting for these variables. However, there were significant effects on GDS by living arrangement/levels of care (β = −.36, p < .01) (Table 4). These suggest that participants with high levels of care may have higher levels of depressive symptoms than those with low levels of care.
Table 4.
Summary of Hierarchical Regression Analysis for PATL, Self-Rated Health, History of Medical Illnesses, MMSE, and Demographic Variables Predicting GDS
| IV | R2 | R2 change | F change | β |
|---|---|---|---|---|
| Step 1 | .22* | - | 2.71* | |
| Age | −.08 | |||
| Gender | .15 | |||
| Marital Status | −.07 | |||
| Education Years | −.00 | |||
| Living Arrangement / Levels of Care | −.36** | |||
| Step 2 | .23 | .01 | .17 | |
| History of Medical Illnesses | −.10 | |||
| MMSE | .01 | |||
| Step 3 | .46*** | .24*** | 9.77*** | |
| PATL | −.35** | |||
| Self-Rated Health | −.30* | |||
Note. GDS = Geriatric Depression Scale; IV = Independent Variable; PATL = Positive Attitude Towards Life; MMSE = Mini Mental Status Exam.
p < .05
p < .01
p < .001
A Mediational Model of Self-Rated Health, PATL, and Depressive Symptoms
We conducted path analysis to test a mediation model in which PATL mediates the relationship between self-rated health and the GDS (Table 5 and Figure 1). Specifically, the total, direct, and indirect effects among variables were computed, and the model adjusted for the effects of participants’ history of medical illness, MMSE scores, and demographic variables (Table 5). Using this approach, a total effect represents the association between self-rated health and the GDS, a direct effect represents the direct association between self-rated health and the GDS controlling for a mediating variable (PATL), and an indirect effect corresponds to the mediating effect of PATL in that relationship. The results showed that the total effect of self-rated health on GDS was −2.17 (z = −3.60, p < .001). The direct effect of self-rated health on GDS was −1.65 (z = −2.71, p < .01), suggesting a smaller effect than the total effect. The indirect effect of Self-Rated Health that passed through PATL was −.52 (z = −1.98, p < .05). Therefore, the proportion of the total effect that is possibly mediated by the effect of PATL was 24%, suggesting a small but significant partial mediation. Further, the ratio of the indirect effect to the direct effect was .31, which was almost one-third of the direct effect. Therefore, the results supported the mediation model, and these results remained significant after adjusting for covariates. Additionally, participants with higher levels of care showed higher scores on GDS.
Table 5.
Summary of Direct, Indirect, and Total Effects of POPS, Self-Rated Health, History of Medical Illnesses, and Other Covariates on GDS by Path Analysis
| Path | Standardized Coefficients | Direct Effect Coefficients | Indirect Effect Coefficients | Total Effect Coefficients |
|---|---|---|---|---|
| PATL → GDS | −.32** | −2.03** | −2.03** | |
| EE → GDS | −.08 | −.40 | −.40 | |
| SR Health → GDS | −.37** | −1.65** | −.52* | −2.17*** |
| Hx of Med Illnesses → GDS | −.14 | −.53 | ||
| MMSE → GDS | .04 | .07 | ||
| Age → GDS | −.09 | −.19 | ||
| Gender (Male) → GDS | −.16 | −1.55 | ||
| Education → GDS | .05 | .07 | ||
| Marital Status 2 → GDS | .42 | 5.38 | ||
| Marital Status 3 → GDS | .04 | 1.04 | ||
| Marital Status 4 → GDS | .42 | 4.78 | ||
| Living Arr 2 → GDS | −.24 | −1.94 | ||
| Living Arr 3 → GDS | −.27 | −3.03 | ||
| Living Arr 4 → GDS | −.42* | −3.74* | ||
| SR Health → PATL | .36** | .25** | .25** | |
Note. EE = Emotional Expression; GDS = Geriatric Depression Scale; Hx of Medical Illnesses = History of medical illnesses; Living Arr 2 = Living arrangement as living independently in private home with a full-time aide or living in a senior living facility providing meals, medical, and nursing care; Living Arr 3 = Living arrangement as living independently in private home with a part-time aide, living in a senior housing facility; living with friend/relative who helps; Living Arr 4 = Living arrangement as living independently in private home without aide or with friend/relative who does not help; Marital Status 2 = Separated/divorced; Marital Status 3 = Widowed; Marital Status 4 = Never married; POPS = Personality Outlook Profile Scale; PATL = Positive Attitude Towards Life; SR Health = Self-Rated Health.
p < .05
p < .01
p < .001
Discussion
The present study investigated the cross-sectional relationships of Positive Attitude Towards Life (PATL), Emotional Expression (EE), and self-rated health to depressive symptoms in a sample of Ashkenazi Jewish centenarians and near-centenarians who were free of cognitive impairment. Findings showed inverse associations of the PATL and self-rated health with participants’ levels of depressive symptoms after adjusting for the effects of demographic variables, history of medical illnesses, and MMSE scores. However, EE was not associated with depressive symptoms. Subsequent path analysis demonstrated that these associations of the PATL and self-rated health with depressive symptoms remained significant even after adjusting for multiple covariates and that PATL had a small but significant partially mediating role in the relationship between self-rated health and depressive symptoms. Findings of path analysis also showed that participants with high levels of care showed higher levels of depressive symptoms while those with low levels of care had lower levels of depressive symptoms. These findings support our hypotheses regarding associations between positive attitudes, which involve positive affect and favorable personality characteristics, , self-rated health and depressive symptoms and the partially mediating role of the PATL in the relationship between self-rated health and depressive symptoms. Overall, findings suggest that positive attitudes contribute to better mental health outcomes through the combined influence by self-rated health in advanced age.
Our findings are similar to previous studies, in that personality characteristics have been reported as an important risk factor for depressive symptoms in both mixed-age and older adults (Steunenberg, Beekman, Deeg, & Kerkhof, 2010; Steunenberg, Braam, Beekman, Deeg, & Kerkhof, 2009; Weber, 2013). Specifically, the FFM traits have been linked to positive health outcomes and longevity/mortality (Martin et al., 2006; Terracciano, Lockenhoff, Zonderman, Ferrucci, & Costa et al., 2008; Weiss & Costa, 2005; Wilson et al., 2005; Wilson et al., 2004). Although the current study did not utilize the FFM measure, the POPS has previously been associated with aspects of the FFM personality traits (Kato, Zweig, Barzilai, & Atzmon, 2012). In line with previous studies (Hampson, Goldberg, Vogt, & Dubanoski, 2006; Nutzel et al., 2014), this study also demonstrated that self-rated health was associated with depressive symptoms. Therefore, our study provides support for the notion that having more favorable attitudes/affect or personality characteristics in conjunction with better self-rated health may promote better mental health outcomes and quality of life in the latest life. Although the mechanism through which positive attitudes may influence the oldest old persons’ self-rated health and mood remains unknown, it is possible that maladaptive attitudes or personality styles may lead to distorted perceptions of health status (Zweig & Agronin, 2011), and thereby increase risk of depressive symptoms. However, given the study's cross-sectional design, findings of this study cannot establish any causal relationship. Interestingly, a recent review suggests a bidirectional association between depression and personality through which one's personality or general emotionality may be altered as a consequence of depressive episodes (Klein, Kotov, & Bufferd, 2011).
Finally, while many oldest old persons face physical, emotional, functional and social challenges in their latest lives, some seem to sustain remarkable functional capacities (Martin, Baenziger, MacDonald, Siegler, & Poon, 2009). Jopp and Rott (2006) suggest that people with exceptional longevity may have a psychological resilience which leads to successful aging and that such resilience is comprised of personality characteristics, health, cognition, and other psychosocial factors. It is possible that PATL may reflect psychological resilience. Previous studies showed that centenarians may have favorable personality and positive affect including lower levels of neuroticism, higher levels of extraversion (Kato, Zweig, Barzilai, & Atzmon, 2012; Martin et al., 2006) and being happy, easygoing, relaxed, and less anxious (Jopp & Rott, 2006; Samuelsson et al., 1997). Similarly, the age-related positivity effect has been reported as older adults have shown an information processing bias towards positive information (Reed, Chan, & Mikels, 2014). Therefore, having favorable attitudes and personality characteristics may represent general tendencies towards positive affect and cognition as well as positive coping strategies and psychological resilience against depression in the oldest old. Findings of this study also showed that participants with high levels of care had higher levels of depressive symptoms than those who lived in the community and required low levels of care. Positive attitudes have been suggested to be one of the major coping mechanisms against depression used by older nursing home residents (Choi, Ransom, & Wyllie, 2008). As poor mental health may have significant implications for daily, physical, and social functioning in this population (Margrett et al., 2010), having a tendency toward positive attitudes, affect, and personality characteristics may be a key protective factor which may enhance emotion regulation and overall functioning in advanced age.
Study Limitations
This study has a number of limitations. The study's design was limited to cross-sectional analyses; thus, findings were unable to imply any causal relationships or specify the direction of relationships among psychological factors, self-rated health, and depressive symptoms. It is possible that a participant's momentary affective state may have affected responses to measures; thus, the POPS cannot be assumed to reflect participants’ life-long attitudes or emotional characteristics. Findings should be replicated utilizing a longitudinal design to clarify attitudes’ long-term effects on mental health outcomes, successful aging, and/or longevity.
Additionally, participants in advanced age presented with a number of challenges in assessment including their sensory impairment, cognitive constraints, and physical disabilities. This study used only brief measures including the MMSE and POPS to assess cognition and emotional/personality characteristics and may lack sufficient coverage of these constructs. The POPS was used in this study due to its brevity and suitability to centenarians and near-centenarians as they may show difficulty tolerating lengthier personality measures; however, it has low levels of internal consistency possibly due to its brevity. Although a standardized personality measure was not used, it is important to note that in our previous study, the POPS was associated with the NEO-FFI (Kato et al., 2012). Therefore, PATL may still represent aspects of personality and be relevant to what has been found in personality and health outcomes research. Further, responses to the POPS were provided by participants with their adult children's assistance to ease participants’ difficulties responding to measures due to their sensory and physical decline. The degree/type of assistance provided by their adult children was unclear. Although previous studies have shown partial agreement between self- and informant-reports (Duchek et al., 2007; Rankin et al., 2005) and a minority of participants likely needed assistance in the current sample, responses of personality measures may have been biased and not represented the true subjective personality characteristics of the participants.
Further, the associations among all variables found in this study were relatively modest. This may be related to the limitations with measures and other confounding factors. The severity of medical illnesses or disability may have contributed to depressive symptoms as the findings showed the association between high levels of care and depressive symptoms. Distance to death is another factor which has been linked to diminished life satisfaction in older adults (Carmel, Shrira, & Shmotkin, 2013). Future studies should continue examining the effects of these factors on mental health outcomes in advanced age.
Lastly, the participants of this study were recruited from one ethnicity in order to maintain genetic and environmental/cultural homogeneity. Therefore, findings of this study may reduce the generalizability of its findings to other groups although this population has not been shown to have more longevity than other groups and does share common environmental health risks with other populations (Barzilai et al., 2003; Rajpathak et al., 2011). In sum, findings of this study should be replicated with the use of full scale personality measures, a larger sample, other heterogeneous populations, and a longitudinal design.
Conclusion
The purpose of this study was to examine cross-sectional associations of positive attitudes, emotional characteristics, and self-rated health to depressive symptoms in Ashkenazi Jewish centenarians and near-centenarians. This study adds to a growing body of knowledge which suggests that positive attitudes/affect and favorable personality in conjunction with self-rated health may play an important role in mental health outcomes in advanced age. Particularly, PATL was found to have a partially mediating role in the relationship between self-rated health and depressive symptoms. Therefore, more favorable attitudes, affect, and personality characteristics in conjunction with better perceived health status may represent psychological determinants which may positively influence mental health outcomes and subsequently lead to better emotional well-being and successful aging. Although findings must be interpreted cautiously given the study's limitations, this study points towards possible protective factors against depression in advanced age. It is also important to note that living in a nursing home or needing higher levels of care emerged as risk factors for depressive symptoms. As findings were limited to cross-sectional analyses, the mechanisms to explain relationships among these variables and the long-term effects of these factors on health outcomes and successful aging remain unclear. Because both attitudes and personality are multi-faceted constructs, they may lead to health outcomes and longevity through a complex interaction among cognitive/affective processes, behaviors, genetic/neurophysiological processes, and environmental factors. The clarification of such mechanisms and the long-term effects of these factors may also help identify preventative strategies against clinical depression and/or treatment interventions for depression in the oldest old persons.
Acknowledgements
We thank many centenarians and near-centenarians and their families for their dedication and contribution to this study. We also thank Mr. William Greiner, the research nurse and other members of the Longevity Genes Project for their contributions and support. This work was supported in part by the National Institute of Health (AG024391; AG027734; AG17242; AG038072) and the Glenn Center for the Biology of Human Aging.
References
- Ajzen I. Nature and operation of attitudes. Annual Review of Psychology. 2001;52:27–58. doi: 10.1146/annurev.psych.52.1.27. [DOI] [PubMed] [Google Scholar]
- Ambresin G, Chondros P, Dowrick C, Herrman H, Gunn JM. Self-rated health and long-term prognosis of depression. Annals of Family Medicine. 2014;12(1):57–65. doi: 10.1370/afm.1562. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Barzilai N, Atzmon G, Schechter C, Schaefer EJ, Cupples AL, Pipton R, Shuldiner AR. Unique lipoprotein phenotype and genotype in humans with exceptional longevity. The Journal of the American Medical Association. 2003;290:2030–2040. doi: 10.1001/jama.290.15.2030. [DOI] [PubMed] [Google Scholar]
- Bombak AE. Self-rated health and public health: A critical perspective. Front Public Health. 2013;20(1):15. doi: 10.3389/fpubh.2013.00015. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Boyd J, McKiernan F, Waller G. Early-onset and late-onset depression in older adults: Psychological perspectives. Reviews in Clinical Gerontology. 2000;10:149–159. [Google Scholar]
- Carmel S, Shrira A, Shmotkin D. The will to live and death-related decline in life satisfaction. Psychology and Aging. 2013;28(4):1115–1123. doi: 10.1037/a0034649. [DOI] [PubMed] [Google Scholar]
- Choi NG, Ransom S, Wyllie RJ. Depression in older nursing home residents: The influence of nursing home environmental stressors, coping, and acceptance of group and individual therapy. Aging and Mental Health. 2008;12(5):536–547. doi: 10.1080/13607860802343001. [DOI] [PubMed] [Google Scholar]
- Conradsson M, Rosendahl E, Littbrand H, Gustafson Y, Olofsson B, Lovheim H. Usefulness of the Geriatric Depression Scale 15-item version among very old people with and without cognitive impairment. Aging and Mental Health. 2013;17(5):638–645. doi: 10.1080/13607863.2012.758231. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Costa PT, Jr., McCrae RR. Domains and facets: Hierarchical personality assessment using the Revised NEO Personality Inventory. Journal of Personality assessment. 1995;64(1):21–50. doi: 10.1207/s15327752jpa6401_2. [DOI] [PubMed] [Google Scholar]
- Crum RM, Anthony JC, Bassett SS, Folstein MF. Population-based norms for the Mini-Mental State Examination by age and educational level. The Journal of the American Medical Association. 1993;269:2386–2391. [PubMed] [Google Scholar]
- de Jonge P, Kempen GI, Sanderman R, Ranchor AV, vanJaarsveld CH, van Sonderen E, Ormel J. Psychosomatics. 2006;47(1):33–42. doi: 10.1176/appi.psy.47.1.33. [DOI] [PubMed] [Google Scholar]
- Dello Buono M, Urciuoli O, De Leo D. Quality of life and longevity: A study of centenarians. Age and Ageing. 1998;27(2):207–216. doi: 10.1093/ageing/27.2.207. [DOI] [PubMed] [Google Scholar]
- DeSalvo KB, Bloser N, Reynolds K, He J, Muntner P. Mortality prediction with a single general self-rated health question. A meta-analysis. Journal of General Internal Medicine. 2006;21(3):267–275. doi: 10.1111/j.1525-1497.2005.00291.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Duchek JM, Balota DA, Storandt M, Larsen R. The power of personality in discriminating between health and early-state Alzheimer's disease. Journal of Gerontology: Psychological Sciences. 2007;62B:353–361. doi: 10.1093/geronb/62.6.p353. [DOI] [PubMed] [Google Scholar]
- Folstein MF, Folstein SE, McHugh PR. “Mini-mental state.” A practical method for grading the cognitive state of patients for the clinician. Journal of Psychiatric Research. 1975;12:189–98. doi: 10.1016/0022-3956(75)90026-6. [DOI] [PubMed] [Google Scholar]
- Folstein FF, Folstein SE, Fanjiang G. MMSE: Mini-mental state examination clinical guide. Psychological Assessment Resources, Inc.; Lutz, FL: 2001. [Google Scholar]
- Freudenberg-Hua Y, Freudenberg J, Vacic V, Abhyankar A, Emde A-K, Ben-Avraham D, Davies P. Disease variants in genomes of 44 centenarians. Molecular Genetics & Genomic Medicine. 2014:1–13. doi: 10.1002/mgg3.86. Doi:10.1002/mgg3.86. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Geerlings S, Beekman A, Deeg D, Twisk J, van Tilburg W. Duration and severity of depression predict mortality in older adults in the community. Psychological Medicine. 2002;32:609–618. doi: 10.1017/s0033291702005585. [DOI] [PubMed] [Google Scholar]
- Glasman LR, Albarracin D. Forming attitudes that predict future behavior: A meta-analysis of the attitude-behavior relation. Psychological Bulletin. 2006;132(5):778–822. doi: 10.1037/0033-2909.132.5.778. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Goldney RD, Eckert KA, Hawthorne G, Taylor AW. Changes in the prevalence of major depression in an Australian community sample between 1998 and 2008. The Australian and New Zealand Journal of Psychiatry. 2010;44(10):901–910. doi: 10.3109/00048674.2010.490520. [DOI] [PubMed] [Google Scholar]
- Gondo Y, Hirose N, Arai Y, Inagaki H, Masui Y, Yamamura K, Kitagawa K. Functional status of centenarians in Tokyo, Japan: Developing better phenotypes of exceptional longevity. The Journals of Gerontology Series A: Biological Sciences and Medical Sciences. 2006;61(3):305–310. doi: 10.1093/gerona/61.3.305. [DOI] [PubMed] [Google Scholar]
- Gunn JM, Ayton DR, Densley K, Pallant JF, Chondros P, Herrman HE, Dowrick CF. The association between chronic illness, multimorbidity and depressive symptoms in an Australian primary care cohort. Social Psychiatry and Psychiatric Epidemiology. 2012;47(2):175–184. doi: 10.1007/s00127-010-0330-z. [DOI] [PubMed] [Google Scholar]
- Hampson SE, Goldberg LR, Vogt TM, Dubanoski JP. Forty years on: Teachers’ assessments of children's personality traits predict self-reported health behaviors and outcomes at midlife. Health-psychology. 2006;25:57–64. doi: 10.1037/0278-6133.25.1.57. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Han B, Jylha M. Depressive symptoms and self-rated health in community-dwelling older adults: A longitudinal study. Journal of the American Geriatrics Society. 2002;50(9):1549–1556. doi: 10.1046/j.1532-5415.2002.50411.x. [DOI] [PubMed] [Google Scholar]
- Harlan E, Clark LA. Short forms of the Schedule for Nonadaptive and Adaptive Personality (SNAP) for self- and collateral ratings: Development, reliability, and validity. Assessment. 1999;6(2):131–145. doi: 10.1177/107319119900600203. [DOI] [PubMed] [Google Scholar]
- Heron M. Deaths: Leading causes for 2004. National Vital Statistics Reports. 2007;56(5):1–95. [PubMed] [Google Scholar]
- Herrman H, Patrick DL, Diehr P, Martin ML, Fleck M, Simon GE, Buesching DP. Longitudinal investigation of depression outcomes in primary care in six countries: The LIDO study. Functional status, health service use and treatment of people with depressive symptoms. Psychological Medicine. 2002;32(5):889–902. doi: 10.1017/s003329170200586x. [DOI] [PubMed] [Google Scholar]
- Hsu HC, Tung HJ. What makes you good and happy? Effects of internal and external resources to adaptation and psychological well-being for the disabled elderly in Taiwan. Aging and Mental Health. 2010;14(7):851–860. doi: 10.1080/13607861003800997. [DOI] [PubMed] [Google Scholar]
- Jeune B. Living longer - but better? Aging Clinical and Experimental Research. 2002;14:72–93. doi: 10.1007/BF03324421. [DOI] [PubMed] [Google Scholar]
- Jopp D, Rott C. Adaptation in very old age: Exploring the role of resources, beliefs, and attitudes for centenarians' happiness. Psychology and Aging. 2006;21(2):266–280. doi: 10.1037/0882-7974.21.2.266. [DOI] [PubMed] [Google Scholar]
- Kato K, Zweig R, Barzilai N, Atzmon G. Positive attitude towards life and emotional expression as personality phenotypes for centenarians. Aging. 2012;4:359–367. doi: 10.18632/aging.100456. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Kato K, Zweig R, Schechter CB, Verghese J, Barzilai N, Atzmon G. Personality, self-rated health, and cognition in centenarians: Do personality and self-rated health relate to cognitive function in advanced age? Aging. 2013;5(3):183–191. doi: 10.18632/aging.100545. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Kern ML, Friedman HS. Do conscientious individuals live longer? A quantitative review. Health Psychology. 2008;27(5):505–512. doi: 10.1037/0278-6133.27.5.505. [DOI] [PubMed] [Google Scholar]
- Klein DN, Kotov R, Bufferd SJ. Personality and depression: Explanatory models and review of the evidence. Annual Review of Clinical Psychology. 2011;7:269–295. doi: 10.1146/annurev-clinpsy-032210-104540. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Lockenhoff CE, Terracciano A, Ferrucci L, Costa PT., Jr. Five-factor personality traits and age trajectories of self-rated health: The role of question framing. Journal of Personality. 2012;80(2):375–401. doi: 10.1111/j.1467-6494.2011.00724.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Lund DA, Utz R, Caserta MS, De Vries B. Humor, laughter, and happiness in the daily lives of recently bereaved spouses. Omega. 2008-2009;58(2):87–105. doi: 10.2190/om.58.2.a. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Margrett J, Martin P, Woodard JL, Miller LS, MacDonald M, Baenziger J, Arnold J. Depression among centenarians and the oldest old: Contributions of cognition and personality. Gerontology. 2010;56(1):93–99. doi: 10.1159/000272018. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Martin P, Baenziger J, MacDonald M, Siegler IC, Poon LW. Engaged lifestyle, personality, and mental status among centenarians. Journal of Adult Development. 2009;16(4):199–208. doi: 10.1007/s10804-009-9066-y. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Martin P, da Rosa G, Siegler I, Davey A, MacDonald M, Poon LW. Personality and longevity: Findings from the Georgia Centenarian Study. Age. 2006;28:343–352. doi: 10.1007/s11357-006-9022-8. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Matthews G, Deary IJ. Personality traits. Cambridge University Press; Cambridge: 1998. [Google Scholar]
- Mavaddat N, Kinmonth AL, Sanderson S, Surtees P, Bigham S, Khaw KT. What determines Self-Rated Health (SRH)? A cross-sectional study of SF-36 health domains in the EPIC-Norfolk cohort. Journal of Epidemiology and Community Health. 2011;65(9):800–806. doi: 10.1136/jech.2009.090845. [DOI] [PubMed] [Google Scholar]
- McCrae RR, Costa PT. Personality in adulthood. The Guilford Press; New York: 1990. [Google Scholar]
- McGuire LC, Strine TW, Okoro CA, Ahluwalia IB, Ford ES. Modifiable characteristics of a healthy lifestyle in U.S. older adults with or without frequent mental distress: 2003 Behavioral risk factor surveillance system. American Journal of Geriatric Psychiatry. 2007;15:754–761. doi: 10.1097/JGP.0b013e3180986125. [DOI] [PubMed] [Google Scholar]
- Mossey JM. Importance of self-perceptions for health status among older persons. In: Gatz M, editor. Emerging issues in mental health and aging. American Psychological Association; Washington, DC: 1995. pp. 124–162. [Google Scholar]
- Mulsant BH, Ganguli M, Seaberg EC. The relationship between self-rated health and depressive symptoms in an epidemiological sample of community-dwelling older adults. Journal of the American Geriatric Society. 1997;45(8):954–958. doi: 10.1111/j.1532-5415.1997.tb02966.x. [DOI] [PubMed] [Google Scholar]
- Nutzel A, Dahlhaus A, Fuchs A, Gensichen J, Konig HH, Riedel-Heller S, Bickel H. Self-rated health in multimorbid older general practice patients: A cross-sectional study in Germany. BMC Family Practice. 2014;15(1):1–12. doi: 10.1186/1471-2296-15-1. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Penninx BW, Geerlings SW, Deeg DJ, van Eijk JT, van Tilburg W, Beekman AT. Minor and major depression and the risk of death in older persons. Archives of General Psychiatry. 1999;56(10):889–895. doi: 10.1001/archpsyc.56.10.889. [DOI] [PubMed] [Google Scholar]
- Perls T. Centenarians and genetics. In: Read CY, Green RC, Smyer MA, editors. Aging, biotechnology and the future. Johns Hopkins University Press; Baltimore, MD: 2008. pp. 89–99. [Google Scholar]
- Pinquart M. Correlates of subjective health in older adults: A meta-analysis. Psychology and Aging. 2001;16(3):414–426. doi: 10.1037//0882-7974.16.3.414. [DOI] [PubMed] [Google Scholar]
- Poon LW, Perls TT. The trials and tribulations of studying the oldest old. In: Poon LW, Perls TT, editors. Annual review of gerontology and geriatrics. Vol. 27. Springer; New York: 2008. pp. 1–10. [Google Scholar]
- Pressman SD, Cohen S. Does positive affect influence health? Psychological Bulletin. 2005;131(6):925–971. doi: 10.1037/0033-2909.131.6.925. [DOI] [PubMed] [Google Scholar]
- Rajpathak SN, Liu Y, Ben-David O, Reddy S, Atzmon G, Crandall J, Barzilai N. Lifestyle factors of people with exceptional longevity. Journal of the American Geriatric Society. 2011;59:1509–1512. doi: 10.1111/j.1532-5415.2011.03498.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Rankin KP, Baldwin E, Pace-Savitsky C, Kramer JH, Miller BL. Self awareness and personality change in dementia. Journal of Neurology, Neurosurgery, and Psychiatry. 2005;76:632–639. doi: 10.1136/jnnp.2004.042879. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Reed AE, Chan L, Mikels JA. Meta-analysis of the age-related positivity effect: Age differences in preferences for positive over negative information. Psychology and Aging. 2014;29(1):1–15. doi: 10.1037/a0035194. [DOI] [PubMed] [Google Scholar]
- Reichstadt J, Depp CA, Palinkas LA, Folsom DP, Jeste DV. Building blocks of successful aging: A focus group study of older adults' perceived contributors to successful aging. American Journal of Geriatric Psychiatry. 2007;15(3):194–201. doi: 10.1097/JGP.0b013e318030255f. [DOI] [PubMed] [Google Scholar]
- Ruch W, Proyer RT, Weber M. Humor as a character strength among the elderly: Empirical findings on age-related changes and its contribution to satisfaction with life. Zeitschrift fur Gerontologie und Geriatrie. 2010;43(1):13–18. doi: 10.1007/s00391-009-0090-0. [DOI] [PubMed] [Google Scholar]
- Samuelsson SM, Alfredson BB, Hagberg B, Samuelsson G, Nordbeck B, Brun A, et al. The Swedish centenarian study: A multidisciplinary study of five consecutive cohorts at the age of 100. International Journal of Aging and Human Development. 1997;45(3):223–253. doi: 10.2190/XKG9-YP7Y-QJTK-BGPG. [DOI] [PubMed] [Google Scholar]
- Scheetz LT, Martin P, Poon LW. Do centenarians have higher levels of depression? Findings from the Georgia Centenarian Study. Journal of the American Geriatric Society. 2012;60(2):238–242. doi: 10.1111/j.1532-5415.2011.03828.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Schulz R, Drayer RA, Rollman BL. Depression as a risk factor for non-suicide mortality in the elderly. Biological Psychiatry. 2002;52(3):205–225. doi: 10.1016/s0006-3223(02)01423-3. [DOI] [PubMed] [Google Scholar]
- Sheikh JI, Yesavage JA. Geriatric Depression Scale (GDS): Recent evidence and development of a shorter version. In: Brink TL, editor. Clinical Gerontology: A Guide to Assessment and Intervention. The Haworth Press; NY: 1986. pp. 165–173. [Google Scholar]
- Steptoe A, O'Donnell K, Marmot M, Wardle J. Positive affect and psychosocial processes related to health. British Journal of Psychology. 2008;99(2):211–227. doi: 10.1111/j.2044-8295.2008.tb00474.x. [DOI] [PubMed] [Google Scholar]
- Steunenberg B, Beekman AT, Deeg DJ, Breemer MA, Kerkhof AJ. Mastery and neuroticism predict recovery of depression in later life. The American Journal of Geriatric Psychiatry. 2007;15:234–242. doi: 10.1097/01.JGP.0000236595.98623.62. [DOI] [PubMed] [Google Scholar]
- Steunenberg B, Beekman AT, Deeg DJ, Kerkhof AJ. Personality predicts recurrence of late-life depression. Journal of Affective Disorders. 2010;123(1-3):164–172. doi: 10.1016/j.jad.2009.08.002. [DOI] [PubMed] [Google Scholar]
- Steunenberg B, Braam AW, Beekman AT, Deeg DJ, Kerkhof AJ. Evidence for an association of the big five personality factors with recurrence of depressive symptoms in later life. International Journal of Geriatric Psychiatry. 2009;24(12):1470–1477. doi: 10.1002/gps.2291. [DOI] [PubMed] [Google Scholar]
- Svedberg P, Gatz M, Pedersen NL. Genetic and environmental mediation of the associations between self-rated health and cognitive abilities. Experimental Aging Research. 2009;35(2):178–201. doi: 10.1080/03610730902720372. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Terracciano A, Lockenhoff CE, Zonderman AB, Ferrucci L, Costa PT., Jr. Personality predictors of longevity: Activity, emotional stability, and conscientiousness. Psychosomatic Medicine. 2008;70(6):621–627. doi: 10.1097/PSY.0b013e31817b9371. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Tombaugh TN, McIntyre NJ. The mini-mental state examination: A comprehensive review. Journal of the American Geriatric Society. 1992;40(9):922–935. doi: 10.1111/j.1532-5415.1992.tb01992.x. [DOI] [PubMed] [Google Scholar]
- Weber K, Giannakopoulos P, Herrmann FR, Bartolomei J, Digiorgio S, Ortiz Chicherio N, Canuto A. Stressful life events and neuroticism as predictors of late-life versus early-life depression. Psychogeriatrics. 2013;13(4):221–228. doi: 10.1111/psyg.12024. [DOI] [PubMed] [Google Scholar]
- Weiss A, Costa PT., Jr. Domain and facet personality predictors of all-cause mortality among Medicare patients aged 65 to 100. Psychosomatic Medicine. 2005;67:724–627. doi: 10.1097/01.psy.0000181272.58103.18. [DOI] [PubMed] [Google Scholar]
- White DK, Keysor JJ, Neogi T, Felson DT, LaValley M, Gross KD, Fredman L. When it hurts, a positive attitude may help: Association of positive affect with daily walking in knee osteoarthritis. Results from a multicenter longitudinal cohort study. Arthritis Care and Research. 2012;64(9):1312–1319. doi: 10.1002/acr.21694. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Wilson RS, Krueger KR, Gu L, Bienias JL, de Leon CFM, Evans DA. Neuroticism, extraversion, and mortality in a defined population of older persons. Psychosomatic Medicine. 2005;67:841–845. doi: 10.1097/01.psy.0000190615.20656.83. [DOI] [PubMed] [Google Scholar]
- Wilson RS, Mendes de Leon CF, Bienias JL, Evans DA, Bennett DA. Personality and mortality in old age. Journals of Gerontology: Psychological Sciences and Social Sciences. 2004;59B:110–116. doi: 10.1093/geronb/59.3.p110. [DOI] [PubMed] [Google Scholar]
- Wilson TD, Lindsey S, Schooler TY. A model of dual attitudes. Psychology Review. 2000;107:101–126. doi: 10.1037/0033-295x.107.1.101. [DOI] [PubMed] [Google Scholar]
- Wong WC, Lau HP, Kwok CF, Leung YM, Chan MY, Cheung SL. The well-being of community-dwelling near-centenarians and centenarians in Hong Kong: A qualitative study. BMC Geriatrics. 2014;14:63. doi: 10.1186/1471-2318-14-63. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Xu J, Roberts RE. The power of positive emotions: It's a matter of life or death – subjective well-being and longevity over 28 years in a general population. Health Psychology. 2010;29(1):9–19. doi: 10.1037/a0016767. [DOI] [PubMed] [Google Scholar]
- Yesavage JA, Brink TL, Rose TL, Lum O, Huang V, Adey MB, Leirer VO. Development and validation of a geriatric depression screening scale: A preliminary report. Journal of Psychiatric Research. 1983;17:37–49. doi: 10.1016/0022-3956(82)90033-4. [DOI] [PubMed] [Google Scholar]
- Zweig RA, Agronin ME. Personality disorders in late life. In: Agronin ME, Maletta GJ, editors. Principles and practice of geriatric psychiatry. 2nd ed Lippincott, Williams, and Wilkins; Philadelphia: 2011. [Google Scholar]