Abstract
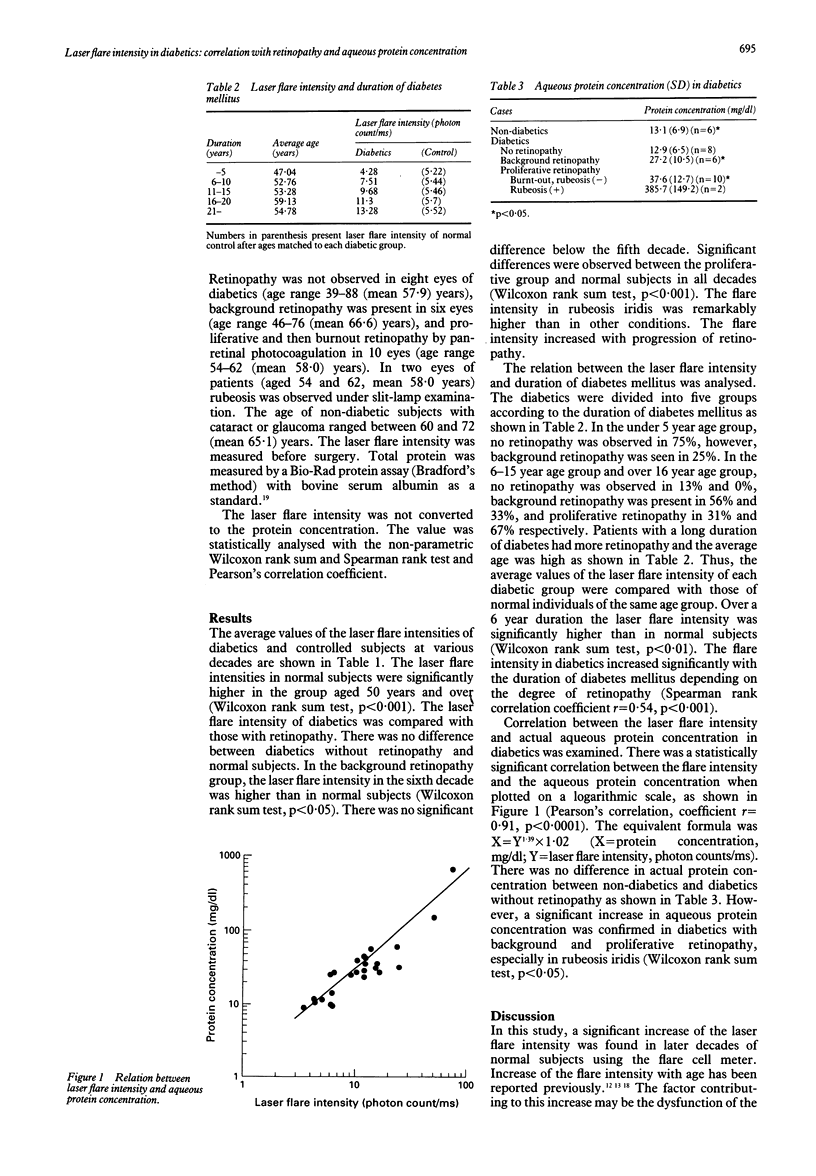
The laser flare intensity in diabetics, measured with the scattering of a light beam, was evaluated and compared with actual aqueous protein concentration obtained during surgery. Measurement of the laser flare intensity in 120 diabetics and 108 normal subjects was performed with the laser flare cell meter (FC1000 Kowa, Tokyo). Aqueous protein concentration in 26 diabetics and six controls who underwent intraocular surgery was measured by the method of Bradford. No significant difference in the laser flare intensity was found between normal subjects and diabetics without retinopathy. A significant increase in the laser flare intensity was observed after six decades in diabetics with background retinopathy and all with proliferative retinopathy. The laser flare intensity correlated with the duration of diabetes mellitus. There was a significant linear relation between the laser flare intensity and actual aqueous protein concentration. The linear regression formula was X = Y1.39 x 1.02 (X = protein concentration, mg/dl; Y = flare intensity, photon counts/ms). The precise value of the laser flare intensity provides a new indicator to evaluate the diabetic change in the function of the ocular barrier.
Full text
PDF


Selected References
These references are in PubMed. This may not be the complete list of references from this article.
- Bradford M. M. A rapid and sensitive method for the quantitation of microgram quantities of protein utilizing the principle of protein-dye binding. Anal Biochem. 1976 May 7;72:248–254. doi: 10.1016/0003-2697(76)90527-3. [DOI] [PubMed] [Google Scholar]
- Dernouchamps J. P. The proteins of the aqueous humour. Doc Ophthalmol. 1982 Nov 1;53(3):193–248. doi: 10.1007/BF00140422. [DOI] [PubMed] [Google Scholar]
- Hayashi M., Yablonski M. E., Boxrud C., Fong N., Berger C., Jovanovic L. J. Decreased formation of aqueous humour in insulin-dependent diabetic patients. Br J Ophthalmol. 1989 Aug;73(8):621–623. doi: 10.1136/bjo.73.8.621. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Ikebe H., Terubayashi H., Akagi Y., Kador P. F., Kinoshita J. H. [Ciliary body changes associate with aldose reductase in galactosemic rats]. Nippon Ganka Gakkai Zasshi. 1989 Jul;93(7):758–762. [PubMed] [Google Scholar]
- Ishibashi T., Tanaka K., Taniguchi Y. Disruption of iridial blood-aqueous barrier in experimental diabetic rats. Graefes Arch Clin Exp Ophthalmol. 1982;219(4):159–164. doi: 10.1007/BF02156840. [DOI] [PubMed] [Google Scholar]
- Kato S., Oshika T., Funatsu H., Kokutei K., Yamashita H., Sawa M. [Aqueous protein concentration in diabetics. Report 5. Relationship between aqueous protein concentration and pathological findings of iridial vessels]. Nippon Ganka Gakkai Zasshi. 1992 Aug;96(8):1000–1006. [PubMed] [Google Scholar]
- Kayazawa F., Tamura S., Tsuji T., Matsuda T., Kuwayama W., Machida T. [Influence of aging on vitreous fluorophotometry]. Nippon Ganka Gakkai Zasshi. 1983 Jun;87(6):380–383. [PubMed] [Google Scholar]
- Klein S., Marré E., Zenker H. J., Koza K. D. Zur Korrelation von diabetischer Irido- und Retinopathie. Fortschr Ophthalmol. 1983;79(5):428–430. [PubMed] [Google Scholar]
- Küchle M., Nguyen N. X., Horn F., Naumann G. O. Quantitative assessment of aqueous flare and aqueous 'cells' in pseudoexfoliation syndrome. Acta Ophthalmol (Copenh) 1992 Apr;70(2):201–208. doi: 10.1111/j.1755-3768.1992.tb04124.x. [DOI] [PubMed] [Google Scholar]
- Miyake K., Miyake T., Kayazawa F. Blood-aqueous barrier in eyes with retinal vein occlusion. Ophthalmology. 1992 Jun;99(6):906–910. doi: 10.1016/s0161-6420(92)31875-5. [DOI] [PubMed] [Google Scholar]
- Nguyen N. X., Küchle M. Aqueous flare and cells in eyes with retinal vein occlusion--correlation with retinal fluorescein angiographic findings. Br J Ophthalmol. 1993 May;77(5):280–283. doi: 10.1136/bjo.77.5.280. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Ogawa T., Ohara K., Shimizu H. [Correlation between total aqueous protein concentrations and photon counts in rabbits]. Nippon Ganka Gakkai Zasshi. 1990 Nov;94(11):1001–1006. [PubMed] [Google Scholar]
- Ohara K., Okubo A., Miyazawa A., Miyamoto T., Sasaki H., Oshima F. Aqueous flare and cell measurement using laser in endogenous uveitis patients. Jpn J Ophthalmol. 1989;33(3):265–270. [PubMed] [Google Scholar]
- Okamura R., Lütjen-Drecoll E. Elektronenmikroskopische Untersuchungen über die Altersveränderungen der menschlichen Iris. Albrecht Von Graefes Arch Klin Exp Ophthalmol. 1973 Apr 17;186(4):249–269. doi: 10.1007/BF00428673. [DOI] [PubMed] [Google Scholar]
- Oshika T., Kato S., Funatsu H. Quantitative assessment of aqueous flare intensity in diabetes. Graefes Arch Clin Exp Ophthalmol. 1989;227(6):518–520. doi: 10.1007/BF02169443. [DOI] [PubMed] [Google Scholar]
- Oshika T., Kato S., Sawa M., Masuda K. Aqueous flare intensity and age. Jpn J Ophthalmol. 1989;33(2):237–242. [PubMed] [Google Scholar]
- Sawa M. Clinical application of laser flare-cell meter. Jpn J Ophthalmol. 1990;34(3):346–363. [PubMed] [Google Scholar]
- Sawa M., Tsurimaki Y., Tsuru T., Shimizu H. New quantitative method to determine protein concentration and cell number in aqueous in vivo. Jpn J Ophthalmol. 1988;32(2):132–142. [PubMed] [Google Scholar]
- Shah S. M., Spalton D. J., Smith S. E. Measurement of aqueous cells and flare in normal eyes. Br J Ophthalmol. 1991 Jun;75(6):348–352. doi: 10.1136/bjo.75.6.348. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Shah S. M., Spalton D. J., Taylor J. C. Correlations between laser flare measurements and anterior chamber protein concentrations. Invest Ophthalmol Vis Sci. 1992 Sep;33(10):2878–2884. [PubMed] [Google Scholar]
- Shimizu T. [Electron microscopic studies of age changes in the human iris. Part I. The anterior border layer of non-glaucomatous eyes (author's transl)]. Nippon Ganka Gakkai Zasshi. 1980 Sep 10;84(9):1352–1359. [PubMed] [Google Scholar]
- Taniguchi Y., Sameshima M. [Fine structure of small blood vessels in the iris of human diabetics]. Nippon Ganka Gakkai Zasshi. 1971;75(8):1685–1697. [PubMed] [Google Scholar]
- Waltman S. R., Oestrich C., Krupin T., Hanish S., Ratzan S., Santiago J., Kilo C. Quantitative vitreous fluorophotometry. A sensitive technique for measuring early breakdown of the blood-retinal barrier in young diabetic patients. Diabetes. 1978 Feb;27(2):85–87. doi: 10.2337/diab.27.2.85. [DOI] [PubMed] [Google Scholar]
- Yoshitomi T., Wong A. S., Daher E., Sears M. L. Aqueous flare measurement with laser flare-cell meter. Jpn J Ophthalmol. 1990;34(1):57–62. [PubMed] [Google Scholar]
- el-Maghraby A., Marzouki A., Matheen T. M., Souchek J., Van der Karr M. Reproducibility and validity of laser flare/cell meter measurements as an objective method of assessing intraocular inflammation. Arch Ophthalmol. 1992 Jul;110(7):960–962. doi: 10.1001/archopht.1992.01080190066030. [DOI] [PubMed] [Google Scholar]



