Abstract
Percutaneous endoscopic colostomy (PEC) is a minimally invasive endoscopic procedure that offers an alternative treatment for high-risk patients with sigmoid volvulus or intestinal pseudo-obstruction who have tried conventional treatment options without success or those who are unfit for surgery. The procedure acts as an irrigation or decompressing channel and provides colonic ‘fixation’ to the anterior abdominal wall. The risk of complications highlights the importance of informed consent for patients and relatives.
Keywords: Colostomy, volvulus, intestinal pseudo-obstruction
Introduction
Percutaneous endoscopic colostomy (PEC) is a minimally invasive procedure usually recommended for high-risk patients not candidate for surgical intervention as an alternative. The procedure was first described in 1986. Since then it has been more widely practiced although there is scarce literature regarding technique, efficacy and safety. National Institute of Clinical Excellence (NICE) latest guidelines were published in 2006. They state “current evidence on the safety and efficacy of PEC appears to be adequate to support it in elderly and frail patients with recurrent sigmoid volvulus and colonic motility problems provided that the normal arrangements are in place for audit and clinical governance” [2]. The procedure acts as an irrigation or decompressing channel or, via direct traction and secondary fibrosis, provides colonic ‘fixation’ to the anterior abdominal wall [3].
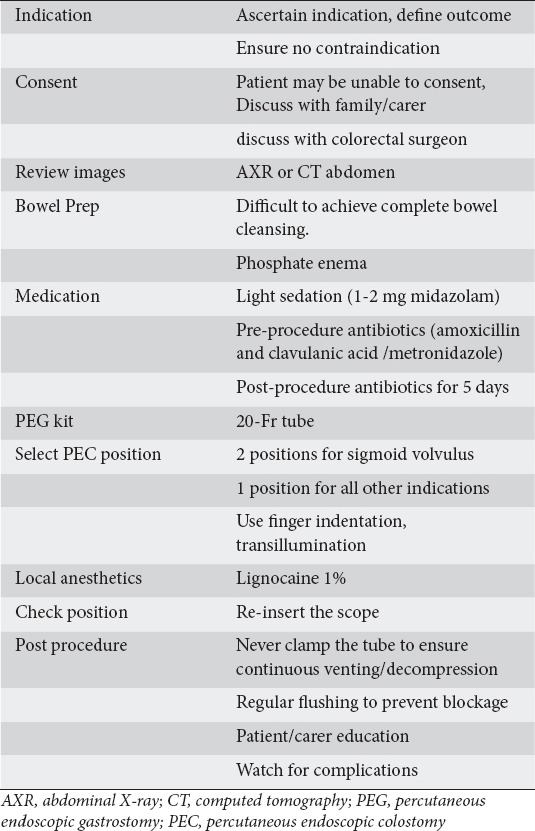
Herein we describe describe 2 case histories to highlight the preparation, method and technique and propose a check list for the procedure (Table 1).
Table 1.
Percutaneous endoscopic colostomy checklist
Case history 1
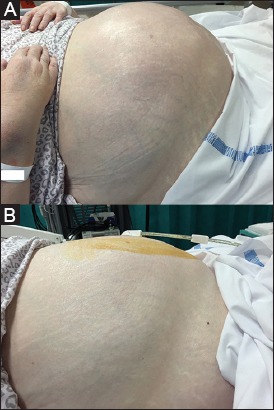
A 75-year-old female with multiple sclerosis was admitted with abdominal pain, distention and diarrhea (Fig. 1A). Following abdominal X-ray (Fig. 2) and surgical review she was diagnosed with intestinal pseudo-obstruction. PEC was recommended to decompress the abdomen and releive the pain. The procedure was performed under light sedation of 2 mg of midazolam. A single dose of intravenous antibiotics was given (amoxicillin and clavulanic acid). The abdomen was prepped with aqueous Betadine.
Figure 1.
(A) Abdominal distension in intestinal pseudo obstruction. (B) Percutaneous endoscopic colostomy is inserted in one position to facilitate decompression
Figure 2.
Abdominal X-ray: Distended bowel loops in intestinal pseudo obstruction
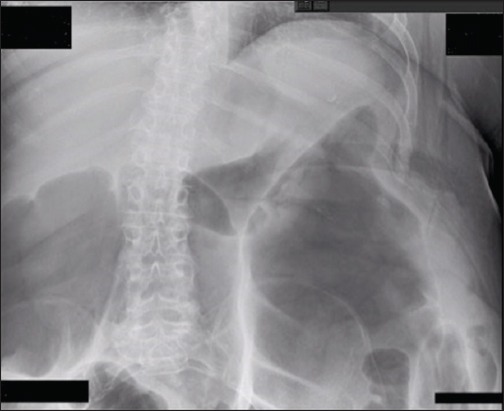
The colonoscope was introduced to the hepatic flexure and then withdrawn to the level of proximal descending colon. Trans-illumination was performed with the lighted tip of the endoscope pressing outward against the abdominal wall to identify point of insertion. Local anesthetic was infiltrated into the skin and the sheath. Using the percutaneous endoscopic gastrostomy (PEG) kit, a needle was used to enter the colon under direct vision. The wire was grasped by a snare (Fig. 3). A 20-Fr PEG tube was then pulled and trailed into the colon and out through the abdominal wall (Ponsky technique). The position was checked by reinsertion of the colonoscope (Fig. 4).
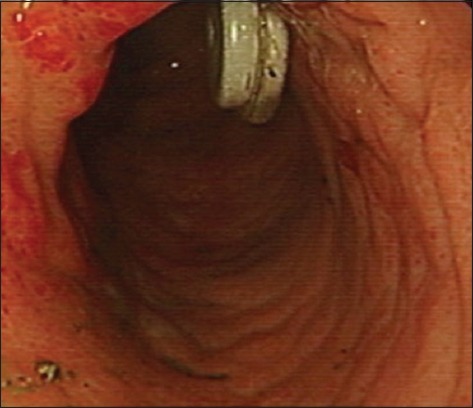
Figure 3.
The wire was grasped by a snare
Figure 4.
The position was checked with the colonoscope
Case history 2
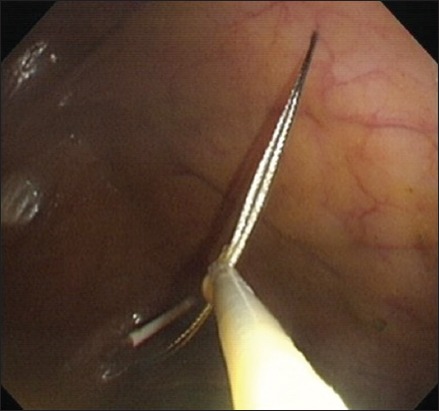
A 91-year-old male was admitted with abdominal pain and distention (Fig. 5A). Computed tomography scan of the abdomen (CT) confirmed sigmoid volvulus (Fig. 6). The patient was deemed not fit for surgery (sigmiodoplexy) and PEC recommended to fix and decompress the colon. Initial preparations were similar to case 1.
Figure 5.
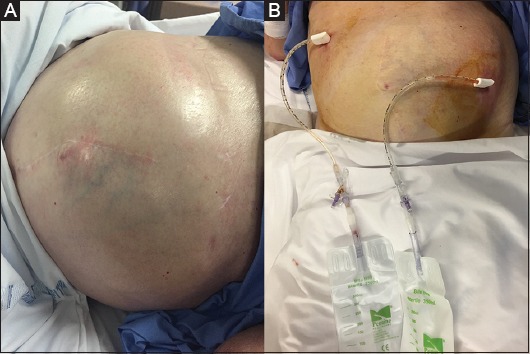
(A) Abdominal distension in sigmoid volvulus. (B) Percutaneous endoscopic colostomy inserted in 2 positions to fix the colon and prevent further twisting
Figure 6.
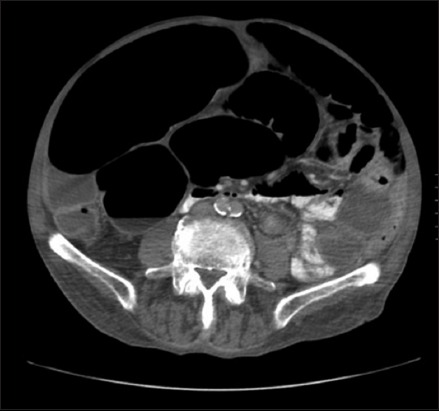
Computed tomography scan abdomen of sigmoid volvulus
The colonoscope was introduced to the ascending colon then withdrawn to proximal limb of the volvulus (Fig. 7). Transillumination was performed to identify the first point of insertion. Local anesthetic was infiltrated into the skin and the sheath. A 20-Fr PEG tube was then pulled and trailed into the colon, through the abdominal wall (Ponsky technique).
Figure 7.
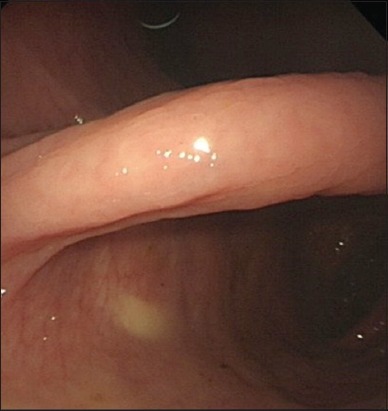
The two limbs of sigmoid volvulus
The colonoscope was further withdrawn to the distal limb of the volvulus. Transillumination was performed to identify the second point of insertion. Another 20-Fr PEG tube was inserted through the abdominal wall.
Discussion
PEC offers an alternative treatment for high-risk patients who have tried conventional treatment options without success or those who are unfit for surgery. Indications for the procedure include: fixation of the colon in recurrent sigmoid volvulus [4]; intermittent or continuous decompression of colonic pseudo-obstruction/megacolon [5]; and antegrade distal colonic and rectal irrigation/enema in some cases of evacuatory disorder or constipation not responding to other treatment options [6].
There is no clear guideline about the number of PECs to be inserted per individual. For patients with sigmoid volvulus, we recommend that the PEC is inserted in two locations, preferably on both limbs of the volvulus to fix the colon and prevent further “twisting” of the bowel (Fig. 5B). For patients with all other indications, a PEC is inserted in one position, proximal left colon, to provide irrigation or decompressing channel (Fig. 1B).
Contraindications include: failure of transillumination; anterior abdominal infection and sepsis; colonic ischemia; and mechanical intestinal obstruction. Patients and/or their parents should be fully informed about the potential risk of peritonitis, the most serious complication associated with PEC [7-9]. This carries significant mortality as the patients for whom the procedure is used for are often elderly and frail and, in most, deemed unfit for surgery. The risk of complications can be as high as 42% [7] and range from local infection, pain at PEC site, PEC leakage, granuloma formation, buried internal bolster, and tube erosion [2,7-9]. Local infections, if not responsive to conservative treatment with antibiotics may need removal of the PEC tube. Delayed complications can occur with one case report described peritonitis 2 months after PEC insertion due to traction injury to the bowel wall leaving a hole in the colon, which allowed fecal spillage [7].
The risk of complications highlights the importance of informed consent for patients and relatives. However, despite the risk of complications, PEC offers an effective treatment option for patients who otherwise would require repeat hospital admissions, multiple endoscopic decompressions (in the case of sigmoid volvulus) and in whom the conditions themselves and surgery carry significant mortality.
Biography
Barnsley Hospital NHS Foundation Trust, South Yorkshire, UK
Footnotes
Conflict of Interest: None
References
- 1.Ponsky J, Aszodi A, Perse D. Percutaneous endoscopic cecostomy: a new approach to nonobstructive colonic dilation. Gastrointest Endosc. 1986;32:108–111. doi: 10.1016/s0016-5107(86)71770-7. [DOI] [PubMed] [Google Scholar]
- 2.National Institute of Clinical Excellence; Interventional procedure guidance (IPG) Percutaneous endoscopic colostomy [Internet] 2006. Available from: www.nice.org.uk/IPG161 .
- 3.Baraza W1, Brown S, McAlindon M, Hurlstone P. Prospective analysis of percutaneous endoscopic colostomy at a tertiary referral centre. Br J Surg. 2007;94:1415–1420. doi: 10.1002/bjs.5858. [DOI] [PubMed] [Google Scholar]
- 4.Daniels IR, Lamperelli MJ, Chave H, Simson JNL. Recrrent sigmoid volvulus treated by percutaneous endoscopic colostomy. Br J Surg. 2000;87:1419. doi: 10.1046/j.1365-2168.2000.01537.x. [DOI] [PubMed] [Google Scholar]
- 5.Heriot AG, Tilney HS, Simson JNL. Percutaneous endoscopic colostomy for obstructed defaecation. Dis Colon Rectum. 2002;45:700–702. doi: 10.1007/s10350-004-6273-2. [DOI] [PubMed] [Google Scholar]
- 6.Gauderer MW, Decou JM, Boyle JT. Sigmoid irrigation tube for the management of chronic evacuation disorders. J Pediatr Surg. 2002;37:348–351. doi: 10.1053/jpsu.2002.30812. [DOI] [PubMed] [Google Scholar]
- 7.Bertolini D, De Saussure P, Chilcott M, Girardin M, Dumonceau JM. bold>Severe delayed complication after percutaneous endoscopic colostomy for chronic intestinal pseudo-obstruction: A case report and review of the literature. World J Gastroenterol. 2007;13:2255–2257. doi: 10.3748/wjg.v13.i15.2255. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Khan A, Ullah S, Beckly D, Oppong C. Percutaneous endoscopic colostomy (PEC): an effective alternative in high risk patients with recurrent sigmoid volvulus. J Coll Physicians Surg Pak. 2013;23:806–808. [PubMed] [Google Scholar]
- 9.Cowlam S, Watson C, Elltringham M, et al. Percutaneous endoscopic colostomy of the left side of the colon. World J Gastroenterol. 2007;13:2255–2257. doi: 10.1016/j.gie.2007.01.012. [DOI] [PubMed] [Google Scholar]


