Abstract
Evidence‐based interventions differ for increasing hypertension awareness, treatment, and control and should be targeted for specific patient panels. This study developed a hypertension control cascade to identify patients with a usual source of care represented at each level of the cascade using the 2007–2012 National Health and Nutrition Examination Survey. Overall, 10.7 million adults in the United States were unaware of their condition, 3.8 million were aware but untreated, and 15.8 million were treated but uncontrolled. The results also suggest that failure to attain hypertension control because of lack of awareness or lack of treatment despite awareness occurs mainly among younger individuals and those with no annual healthcare visits, while the elderly and minorities are more likely to remain uncontrolled when aware and treated. Opportunities to leverage population health management functions in electronic health information systems to align the specific patient subgroups facing barriers to hypertension control at each level of the cascade with targeted hypertension management interventions are discussed.
Nearly 30% of adults in the United States have hypertension.1, 2 Hypertension was identified as the underlying or contributing cause in more than 360,000 deaths in 2010.1, 3 One goal of the US Health and Human Services Million Hearts® initiative is to prevent one million heart attacks and strokes between 2012–2016 through improving hypertension control to 70% or greater among patients currently in clinical care.4 Achieving that target could prevent approximately 50,000 deaths annually.5
Studies have shown that patients with a usual source of health care receive more effective care and have better hypertension control compared with those without a usual source of care.6, 7, 8 Recent data also show that among the 36 million US adults with uncontrolled hypertension, 89.4% report having a usual source of care. Among these individuals with care, just over half (51.2%) do not report taking prescription medication treatment for the condition.9 This led the American Medical Association to prioritize blood pressure (BP) control among patients in care for its multi‐year commitment to help improve health outcomes.10 This study develops a multi‐level cascade analysis of hypertension awareness, treatment, and control among US adults with a usual source of care. The analysis focuses on national level data stratified by patient characteristics commonly available to healthcare providers in ambulatory care practices from patient registries, electronic health record (EHR) systems, population health management tools, or practice location demographic information.11, 12, 13 The findings suggest that several layers of barriers to achieving hypertension control may be present for persons with a usual source of care: lack of awareness, lack of any treatment, and lack of effective treatment. If discrete patient populations experience lack of control for different reasons, patient panels should be stratified to reflect that variation in barriers to awareness, treatment, or control and then paired with targeted evidence‐based interventions. We illustrate how functions embedded within population health management tools, EHRs, or data registries are available to support this strategy.14, 15, 16, 17, 18, 19
Methods
We used a combination of three 2‐year cycles of the National Health and Nutrition Examination Survey (NHANES) data: 2007–2008, 2009–2010, and 2011–2012 with demographic, healthcare access, and healthcare use–related information from the interview component and BP measurements from the physical examination component. A participant was defined as having elevated BP if their systolic BP (SBP) was ≥140 mm Hg or their diastolic BP (DBP) was ≥90 mm Hg based on an average of up to three measurements collected under a standard protocol.20 A participant was defined as being hypertensive if they had an elevated BP or reported being treated for the condition. Among those with hypertension: (1) hypertension awareness was present if a participant reported being told by a health professional that they had hypertension; (2) hypertension treatment was defined as a participant reporting that they had been prescribed antihypertensive medicine by a healthcare provider and were currently taking the prescribed medication to lower their BP; and (3) hypertension control was defined as a BP<140/90 mm Hg.
The focus of this study was on participants with a usual source of medical care, defined by confirming a usual or more than one place to go when sick or in need of advice about health. Number of annual visits for ambulatory care (0, 1, 2–3, or 4 or more visits) were also included.
To mimic the analyses an ambulatory practice can use to help identify subgroups among their hypertensive patients,16, 17, 21 variation in status and prevalence at each level of the hypertension control cascade––awareness, treatment, and control––were examined by demographic data that practices are likely to collect including sex, age, race/ethnicity, insurance coverage type, and number of healthcare visits in the last year. Adults were classified as aged 18 to 44 years, 45 to 64 years, and 65 years and older. Participants' self‐reported race/ethnicity was defined as non‐Hispanic white, non‐Hispanic black, Hispanic, or other (results not reported). Participants' health insurance was described as Medicare (any Medicare, including Medicare Advantage, or Fee for Service), private (including Medigap), public (Medicaid, State Children's Health Insurance Plan, military health care, Indian Health Service, state‐sponsored, health plan, or other government insurance), or uninsured (none or single service plan).
A sample of 16,820 adults was obtained after applying the exclusions described in the [Link].22 Within this sample, patients with hypertension and a usual source of care (n=5,615) are used to estimate patient awareness, treatment, and attainment of hypertension control. Estimates of population totals were generated using the US Census adult population at the mid‐point of each survey cycle and averaged across the three cycles of NHANES data used in the analysis.22
Statistical Analysis
Two‐tailed chi‐square tests were used for multinomial data comparisons. Two‐tailed t tests were performed to assess differences between characteristic subgroups, using a Bonferroni adjustment for multiple comparisons. Statistical significance was defined as a P value <.05.23 All analyses were conducted using SAS version 9.3 (SAS Institute, Cary, NC) and SUDAAN version 10 (RTI International, Research Triangle Park, NC) and accounted for the complex sample design.
Results
The prevalence of hypertension among US adults during 2007–2012 was 30.7% (95% confidence interval [CI], 29.3%–32.1%), representing 69.8 million individuals, which is presented in the hypertension control cascade illustrated in the Figure. Of this sample, 65.4 million individuals, or 93.7% (95% CI, 92.5%–94.7%) reported having a usual source of medical care. Overall, 13.1 million adults (data not shown) were unaware that they had hypertension and 10.7 million, or 16.3% (95% CI, 14.7%–18.1%), of them reported having a usual source of care. Among individuals with a usual source of care who were aware of their hypertension, 3.8 million, or 7.0% (95% CI, 5.9%–8.2%), were not receiving treatment. Finally, 15.8 million, or 31.1% (95% CI, 29.3%–32.9%), of adults with a usual source of care had uncontrolled hypertension even though they were aware and treated.
Figure 1.
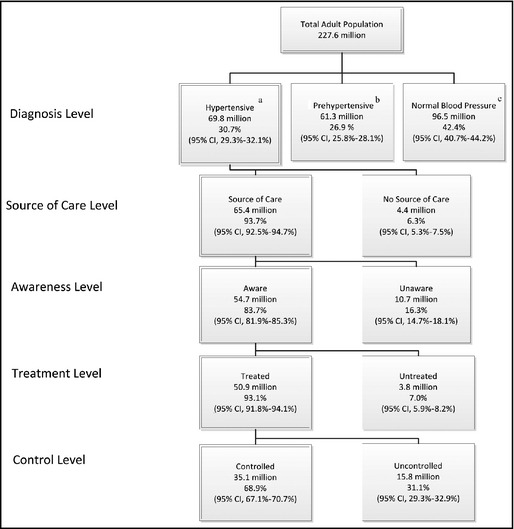
Hypertension control cascade. aSystolic blood pressure ≥140 mmHg or diastolic blood pressure ≥90 mmHG; bSystolic blood pressure ≥120 and <140 mmHg or diastolic blood pressure ≥80 BP and <90 range; cSystolic blood pressure <120 mmHg or diastolic blood pressure <80. CI indicates confidence interval.
Lack of Hypertension Awareness Among Persons With a Usual Source of Care
Table 1 presents the prevalence of being unaware and the number of individuals unaware of their hypertension among the 65.4 million US adults with hypertension and a usual source of care, by select characteristics. Results from univariate chi‐square tests found that awareness was associated with all of the select characteristics (P<.001 to P=.013). The prevalence of hypertension unawareness was found to be significantly higher among the 2.4 million individuals aged 18 to 44 years compared with individuals in the two older age categories (26.6% vs 15.2% and 26.6% vs 14.1%, respectively; P<.001 for both). The likelihood of being unaware was also higher among the 1.7 million adults who had no healthcare visits in the past year compared with the 1.8 million adults with one visit (55.5% vs 27.1%; P<.001). For the 4.1 million adults who had four or more visits in the past year and the 3.1 million adults who had two or three visits, the lack of awareness was lower than that for adults who had only one visit (11.0% vs 27.1% [P<.001] and 16.5% vs 27.1% [P=.019], respectively).
Table 1.
Prevalence of Being Unaware of Their High Blood Pressure Among Adults (≥18 Years) With Hypertension Who Have a Usual Source of Health Care, by Select Characteristics––NHANES 2007–2012
| Characteristics | Usual Source of Care | Unaware of Hypertension | χ 2 a/t Testb | |||||
|---|---|---|---|---|---|---|---|---|
| Sample, No. | % | (95% CI) | No | % | (95% CI) | No | P Value | |
| Total | 5615 | 93.7 | (92.5–94.7) | 65.4 | 16.3 | (14.7–18.1) | 10.7 | |
| Sex | .006a | |||||||
| Male | 2713 | 91.1 | (89.3–92.7) | 30.6 | 18.2 | (16.1–20.4) | 5.6 | |
| Female | 2902 | 96.1 | (95.1–96.9) | 34.8 | 14.7 | (12.8–16.9) | 5.1 | .069b |
| Age group, y | <.001a | |||||||
| 18–44 | 613 | 85.9 | (82.1–89.0) | 9.0 | 26.6 | (21.3–32.6) | 2.4 | [Reference] |
| 45–64 | 2255 | 92.7 | (91.0–94.1) | 30.0 | 15.2 | (13.1–17.6) | 4.6 | .001b |
| 65+ | 2747 | 97.9 | (97.2–98.5) | 26.5 | 14.1 | (12.3–16.2) | 3.7 | .001b |
| Race/ethnicity | .013a | |||||||
| Non‐Hispanic white | 2649 | 95.3 | (93.8–96.4) | 47.4 | 16.5 | (14.3–19.1) | 7.8 | [Reference] |
| Non‐Hispanic black | 1555 | 93.2 | (91.6–94.5) | 9.5 | 13.1 | (11.0–15.5) | 1.2 | .335b |
| Hispanic | 1086 | 84.7 | (81.5–87.3) | 5.3 | 19.3 | (15.9–23.2) | 1.0 | 1.000b |
| Insurance coverage type | <.001a | |||||||
| Medicare | 2870 | 98.2 | (97.6–98.7) | 27.9 | 13.5 | (11.7–15.6) | 3.8 | .108b |
| Private | 1580 | 95.1 | (93.8–96.1) | 26.2 | 18.6 | (15.5–22.2) | 4.9 | [Reference] |
| Public | 579 | 95.1 | (91.6–97.2) | 5.7 | 11.3 | (7.7–16.2) | 0.6 | .134b |
| Uninsured | 586 | 71.3 | (65.4–76.6) | 5.5 | 25.1 | (21.7–28.8) | 1.4 | .060b |
| Times received health care in past year | <.001a | |||||||
| 0 | 252 | 60.0 | (52.9–66.7) | 3.1 | 55.5 | (47.0–63.8) | 1.7 | <.001b |
| 1 | 536 | 89.9 | (86.5–92.5) | 6.8 | 27.1 | (21.4–33.7) | 1.8 | [Reference] |
| 2–3 | 1557 | 95.3 | (93.1–96.8) | 18.7 | 16.5 | (13.9–19.5) | 3.1 | .019b |
| ≥4 | 3270 | 98.3 | (97.3–98.9) | 36.9 | 11.0 | (9.3–12.9) | 4.1 | <.001b |
Abbreviations: CI, confidence interval; NHANES, National Health and Nutrition Examination Survey. a P values for univariate chi‐square test of independence between characteristics and hypertension awareness status. b P values for univariate t test for difference in hypertension awareness status against the reference category, Bonferroni adjusted (univariate P value times the number of comparisons).
Aware of Hypertension But Not Treated Among Persons With a Usual Source of Care
Univariate chi‐square tests (Table 2) showed that hypertension treatment was associated with the select characteristics (P≤.001). The results also showed that untreated hypertension prevalence was higher among the 2.3 million men than the 1.5 million women (9.1% vs 5.2%; P<.001), the 1.1 million individuals aged 18 to 44 years vs the 1.9 million aged 45 to 64 years (17.1% vs 7.3%; P=.005) and vs the 0.8 million aged 65 years or older (17.1% vs 3.7%; P<.001). Finally, the 0.6 million adults who had not received medical care in the past year had a higher prevalence of untreated hypertension compared with those 0.7 million adults seen once (40.6% vs 14.7%; P<.001). Also, untreated hypertension prevalence for persons seen once in the previous year was higher compared with the 1.1 million adults who had 2 or 3 visits (14.7% vs 7.0%; P=.01) and compared with the 1.4 million adults with four or more visits (14.7% vs 4.4%; P<.001).
Table 2.
Prevalence of Being Untreated for High Blood Pressure Among Adults (≥18 Years) With Hypertension Who Have a Usual Source of Health Care and Are Aware of Their Hypertension, by Select Characteristics––NHANES 2007–2012
| Characteristics | Aware | Untreated | χ 2 a/t Testb | |||||
|---|---|---|---|---|---|---|---|---|
| Sample, No. | % | (95% CI) | No | % | (95% CI) | No | P Value | |
| Total | 4737 | 83.7 | (81.9–85.3) | 54.7 | 7.0 | (5.9–8.2) | 3.8 | |
| Sex | <.001a | |||||||
| Male | 2240 | 81.8 | (79.6–83.9) | 25.0 | 9.1 | (7.6–10.8) | 2.3 | |
| Female | 2497 | 85.3 | (83.1–87.2) | 29.7 | 5.2 | (4.2–6.5) | 1.5 | <.001b |
| Age group, y | <.001a | |||||||
| 18–44 | 450 | 73.4 | (67.4–78.7) | 6.6 | 17.1 | (12.9–22.3) | 1.1 | [Reference] |
| 45–64 | 1929 | 84.8 | (82.4–86.9) | 25.4 | 7.3 | (5.7–9.2) | 1.9 | .005b |
| 65+ | 2358 | 85.9 | (83.8–87.7) | 22.7 | 3.7 | (2.8–4.9) | 0.8 | <.001b |
| Race/ethnicity | .001a | |||||||
| Non‐Hispanic white | 2220 | 83.5 | (80.9–85.7) | 39.6 | 6.4 | (5.1–7.9) | 2.5 | [Reference] |
| Non‐Hispanic black | 1363 | 86.9 | (84.5–89.0) | 8.2 | 9.4 | (7.6–11.6) | 0.8 | .072b |
| Hispanic | 893 | 80.7 | (76.8–84.1) | 4.3 | 6.4 | (4.2–9.6) | 0.3 | 1.000b |
| Insurance coverage type | <.001a | |||||||
| Medicare | 2480 | 86.5 | (84.4–88.3) | 24.2 | 3.9 | (2.9–5.2) | 0.9 | .002b |
| Private | 1283 | 81.4 | (77.8–84.5) | 21.3 | 8.5 | (6.6–11.0) | 1.8 | [Reference] |
| Public | 511 | 88.7 | (83.8–92.3) | 5.1 | 7.5 | (4.9–11.3) | 0.4 | 1.000b |
| Uninsured | 455 | 74.9 | (71.2–78.3) | 4.1 | 16.2 | (12.4–20.8) | 0.7 | .057b |
| Times received health care in past year | <.001a | |||||||
| 0 | 109 | 44.5 | (36.2–53.0) | 1.4 | 40.6 | (30–52.1) | 0.6 | <.001b |
| 1 | 379 | 72.9 | (66.3–78.6) | 5.0 | 14.7 | (10.5–20.3) | 0.7 | [Reference] |
| 2–3 | 1311 | 83.5 | (80.5–86.1) | 15.6 | 7.0 | (5.1–9.5) | 1.1 | .010b |
| ≥4 | 2930 | 89.0 | (87.1–90.7) | 32.8 | 4.4 | (3.4–5.6) | 1.4 | <.001b |
Abbreviations: CI, confidence interval; NHANES, National Health and Nutrition Examination Survey. a P values for univariate chi‐square test of independence between characteristics and hypertension awareness status. b P values for univariate t test for difference in hypertension awareness status against the reference category, Bonferroni adjusted (univariate P value times the number of comparisons).
Aware and Receiving Treatment But Not in Control Among Persons With a Usual Source of Care
Results from univariate chi‐square tests (Table 3) showed that hypertension control was dependent on age (P<.001), race/ethnicity (P<.001), and type of insurance coverage (P<.001) but independent of sex (P=.27) and frequency of annual care (P=.58). Uncontrolled hypertension was more prevalent among the 8.2 million individuals aged 65 years or older compared with the 1.2 million individuals 18 to 44 years (37.4% vs 22.0%; P<.001). Among those treated for their hypertension, the 2.8 million non‐Hispanic blacks and the 1.5 million Hispanics had higher prevalences of uncontrolled hypertension compared with the 10.8 million non‐Hispanic whites (37.6% vs 29.1% [P<.001] and 36.4% vs 29.1% [P=.008], respectively). The 8.5 million Medicare beneficiaries had a higher prevalence of uncontrolled hypertension than the 5.1 million individuals with private insurance (36.4% vs 25.9%; P<.001).
Table 3.
Prevalence of Uncontrolled Blood Pressure Among Adults (≥18 Years) With Hypertension Who Have a Usual Source of Health Care, Are Aware of Their Hypertension, and Are Currently Treated, by Select Characteristics––NHANES 2007–2012
| Characteristics | Treated | Uncontrolled | χ 2 a/t Testb | |||||
|---|---|---|---|---|---|---|---|---|
| Sample. No. | % | (95% CI) | No | % | (95% CI) | No | P Value | |
| Total | 4413 | 93.0 | (91.8–94.1) | 50.9 | 31.1 | (29.3–32.9) | 15.8 | |
| Sex | .265a | |||||||
| Male | 2050 | 90.9 | (89.2–92.4) | 22.8 | 30.1 | (28.0–32.4) | 6.9 | |
| Female | 2363 | 94.8 | (93.5–95.8) | 28.2 | 31.8 | (29.5–34.3) | 9.0 | 1.00b |
| Age group, y | <.001a | |||||||
| 18–44 | 367 | 82.9 | (77.7–87.1) | 5.5 | 22.0 | (17.6–27.3) | 1.2 | [Reference] |
| 45–64 | 1783 | 92.7 | (90.8–94.3) | 23.6 | 27.3 | (24.9–29.8) | 6.4 | .545b |
| 65+ | 2263 | 96.3 | (95.1–97.2) | 21.9 | 37.4 | (34.9–40.1) | 8.2 | <.001b |
| Race/ethnicity | <.001a | |||||||
| Non‐Hispanic white | 2086 | 93.6 | (92.1–94.9) | 37.1 | 29.1 | (27.1–31.2) | 10.8 | [Reference] |
| Non‐Hispanic black | 1249 | 90.6 | (88.4–92.4) | 7.5 | 37.6 | (34.8–40.4) | 2.8 | <.001b |
| Hispanic | 841 | 93.6 | (90.4–95.8) | 4.0 | 36.4 | (33.0–39.9) | 1.5 | .008b |
| Insurance coverage type | <.001a | |||||||
| Medicare | 2383 | 96.1 | (94.8–97.1) | 23.2 | 36.4 | (33.8–39.1) | 8.5 | <.001b |
| Private | 1170 | 91.5 | (89.0–93.4) | 19.5 | 25.9 | (23.3–28.8) | 5.1 | [Reference] |
| Public | 470 | 92.5 | (88.7–95.1) | 4.7 | 24.0 | (19.4–29.3) | 1.1 | 1.000b |
| Uninsured | 384 | 83.8 | (79.2–87.6) | 3.5 | 33.9 | (27.5–41.0) | 1.2 | .460b |
| Times received health care in past year | .579a | |||||||
| 0 | 58 | 59.4 | (47.9–70.0) | 0.8 | 40.9 | (26.3–57.4) | 0.3 | 1.000b |
| 1 | 324 | 85.3 | (79.7–89.5) | 4.2 | 30.6 | (24.0–38.0) | 1.3 | [Reference] |
| 2–3 | 1217 | 93.0 | (90.5–94.9) | 14.5 | 31.8 | (28.5–35.3) | 4.6 | 1.000b |
| ≥4 | 2808 | 95.6 | (94.4–96.6) | 31.4 | 30.5 | (28.6–32.5) | 9.6 | 1.000b |
Abbreviations: CI, confidence interval; NHANES, National Health and Nutrition Examination Survey. a P values for univariate chi‐square test of independence between characteristics and hypertension awareness status. b P values for univariate t test for difference in hypertension awareness status against the reference category, Bonferroni adjusted (univariate P value times the number of comparisons).
Discussion
Our analysis of nationally representative NHANES data demonstrates which subgroups of patients reporting a usual source of care are more or less likely to have uncontrolled hypertension as a result of being unaware of their condition, aware but untreated, or treated but remaining uncontrolled. We found that individuals of Hispanic ethnicity and non‐Hispanic blacks who were aware of their condition are no less likely to receive treatment compared with non‐Hispanic whites, but they were more likely to be uncontrolled despite receiving treatment. Similarly, Medicare beneficiaries were more often aware of their hypertension and receiving treatment, but had relatively high rates of uncontrolled hypertension. Besides the confounding effect of age, this may be due in part to treatment‐resistant hypertension being more prevalent among older patients.24, 25 In addition, despite being insured and receiving relatively low‐cost medications, Medicare patients may still face a financial barrier to adherence and, hence control, when they enter the Medicare prescription drug plan coverage gap, also known as the “donut hole.”26, 27 We also found that younger individuals and those with few or no visits for health care in the last year were often unaware of their hypertension, and when aware they were less likely to receive treatment.
These results provide physicians, other healthcare providers, public health practitioners, policy makers, insurers, community partners, and quality improvement experts with a basic framework for targeting patients most likely to be at‐risk at each level of the hypertension control cascade. While multiple stakeholders play important roles in improving hypertension management, the discussion will focus on the application of the framework in the ambulatory practice setting. While practices with limited EHR capabilities can apply the information from the cascade to help tailor interventions, this framework relies primarily on the functions available in data‐enabled population health management tools to help identify subgroups of patients with gaps in hypertension management, pair those patients with effective interventions, and facilitate the implementation of the interventions. Patient registries, population health management tools, and EHRs meeting the objectives of the meaningful use certification criteria11, 12, 13 include functions to generate lists of patients by specific conditions, send patient reminders, prompt offers of patient education material, provide embedded clinical content, and chart and report out changes in BP. More specifically, ambulatory practices can apply data query capabilities to select subgroups of underserved or at‐risk hypertensive patients and pair those patients with targeted interventions, such as a follow‐up visit to confirm an elevated BP reading, initiate treatment, or intensify treatment.15, 18, 19, 28
Numerous strategies and interventions have been found to be effective in controlling hypertension. For example, changes in care team strategies (ie, engaging the pharmacist in patient communications and having a standard algorithm for adding medications) have been found to reduce median SBP by 9.7 mm Hg and reduce median DBP by 4.2 mm Hg,29 modest reductions in therapeutic inertia have been shown to lower SBP by >5 mm Hg,21 and medication reminders can increase adherence to 66.6% compared with 54.7% in a control group.30 Large‐scale multifaceted initiatives to improve hypertension control have seen control rates increase from 49% to 66% between 2000 and 200518 and increase from 43.6% to 80.4% between 2001 and 2009.28
Addressing Lack of Awareness Among Persons With Hypertension
Individuals seen for care no more than once in the past year were the most likely to be unaware of their hypertension. Increasing the frequency of visits for this population could lead to improved BP control.19, 31 Providers might target these patients by employing follow‐up visit reminders15 or automated outreach call services aimed at increasing visit adherence.14 In addition, healthcare practices can engage in targeted outreach efforts with community partners by participating in BP screening events to identify persons unaware of their hypertension.17 In particular, insurers', employers', or community‐based hypertension awareness campaigns might also focus on adults younger than 45 years, who are at greatest risk for being unaware of their hypertension. Others may be unaware because of inaccurate BP readings in the office, inappropriate labeling as having white‐coat hypertension, or as a result of inadequate follow‐up. These patients could be better engaged in care if they were provided fact sheets or other patient education materials embedded within the EHR29 or if they self‐monitored their BP and brought in readings taken at home for review at an appointment when having limited access to EHRs. Health professionals and care teams might also employ population health management tools or conduct queries of their EHR or registry data to screen for patients and create patient lists of those with an elevated BP at the last reading who do not carry a diagnosis of hypertension in their record32 and those for whom hypertension might not be a priority or the primary reason for seeking care or attending an office visit.18, 33
Addressing Lack of Treatment Among Persons With Diagnosed Hypertension
The cascade analysis also shows that certain patient subgroups are more likely to remain untreated despite a recognized diagnosis of hypertension. Lack of treatment could be addressed through employing automated means to identify and reach out to younger patients and those who had not been seen for care in the last year.14, 15 In general, there are two possible causes for lack of current treatment for hypertension: noninitiation of therapy34 or lack of persistence with therapy.35, 36 An EHR or registry generated prior and active medication list might aid in determining the prevalence of each of these causes. In addition, some systems are able to generate a list of potentially hypertensive patients never prescribed antihypertensive medications or a list of patients who received an initial prescription but failed to refill it over time. Treatment protocols and standardized algorithms embedded within EHRs can aid in prioritizing the initiation of therapy.18, 34, 37, 38 Persons in low‐resource settings with limited access or use of EHRs can utilize certain communication techniques, such as using a “teach‐back” method, to improve medication adherence.39
Addressing Lack of Therapeutic Effectiveness
Racial and ethnic minorities and those older than 65 years (or on Medicare) are often taking antihypertensive therapy but not controlled. There are several common reasons for therapeutic ineffectiveness in these groups that might be remedied by changing improvement targets.40 For instance, failure to change or increase therapy for patients who are not at goal (“therapeutic inertia”)41, 42 can be addressed by leveraging EHRs to implement treatment algorithms and protocols,16, 28, 38 utilizing clinical decision support tools embedded within EHRs including a 2‐week follow‐up process and patient reminders,19 and changes in team care.43, 44, 45, 46 Treatment‐resistant hypertension is related to age, patient factors, and medical causes of secondary hypertension47 and can be explored by implementing streamlined referral pathways35 and pushing EHR alerts to providers when the BP is elevated.30
Research has also shown that non‐Hispanic black patients with hypertension may be less likely than their counterparts to be controlled with fewer than three drugs.48 Uncontrolled patients who are older, Hispanic, or non‐Hispanic black who are not taking at least three BP medications could be identified with customized queries of data registries or by reviewing patient records when facing limitations to EHR capabilites.21, 47 Nonadherence in these subgroups can also be addressed by using structured assessments of adherence,49 improving provider communication,29, 46 and overcoming language barriers.50 Other strategies rely on using population health management functions to identify patients in need of educational resources, offer patients topic‐specific materials, and track prescribing patterns (eg, use of dual‐agent therapies,28 90‐day prescriptions, and automatic refills).
Limitations
The findings in this study are subject to several limitations. First, NHANES data are restricted to the civilian noninstitutionalized population; thus, results from this study are not generalizable to individuals in long‐term care facilities or prisons or to military personnel. Second, although NHANES collects up to three BP readings for each participant, they are taken during a single visit to the Mobile Examination Center, while clinical hypertension diagnosis standards require two or more visits.35 Still, the standardized measurement of BP makes NHANES the best source of national data on hypertension. Third, usual source of care includes any place an individual goes for care, which can include emergency rooms, clinics, or other places not having a focus on preventive services. Our results might therefore overestimate the proportion of patients with regular primary care.
Conclusions
The analysis of national‐level data shows that opportunities for improvement in hypertension control exist at each level of the hypertension control cascade. Aided by the functions increasingly becoming available in EHRs and population health management tools, the analysis provides a framework to identify patient subgroups based on characteristics known to providers at the practice level and pair them with targeted interventions. By relying on strategies tailored to hypertension management at a specific level of the control cascade for the patients they serve, healthcare providers and the delivery system can move towards meeting national goals for hypertension control. The increased adoption of EHRs and the increased utilization of EHR‐embedded functions will continue to be key contributors to the success of these efforts.
Author Contributions
Dr Wozniak had full access to all the data in this study and takes responsibility for the integrity of the data and the accuracy of the data analysis. Study concept and design: Gillespie, Hasan, Kmetik, Ritchey, Wozniak, Wynia. Acquisition of data: Gillespie, Sifuentes, Wozniak. Analysis and interpretation of data: Gillespie, Khan, Ritchey, Sifuentes, Wozniak. Drafting of the manuscript: All. Critical revision of the manuscript for important intellectual content: Kmetik, Khan, Ritchey, Wozniak, Wynia. Statistical analysis: Gillespie, Sifuentes, Khan, Wozniak. Study supervision: Wozniak.
Funding/Support
None.
Disclosures
None.
Acknowledgments
The authors thank Annalynn Skipper and Donitta Ennis for their administrative, technical, and materials support.
The continuous survey uses a multistage, clustered sample, designed to be representative of the civilian, noninstitutionalized population of the United States. The average response rate across these cycles was 74.1% (75.4% in 2007–2008, 77.3% in 2009–2010, and 69.5% in 2011–2012).
During the 2007–2012 cycles of National Health and Nutrition Examination Survey (NHANES), 17,788 non‐pregnant adults 18 years and older were examined. A total of 986 participants were excluded because there were no blood pressure (BP) measurements (n=870) or there was missing information on BP‐lowering medication use (n=6), awareness (n=24), usual source of care (n=1), or there were missing data on covariates of interest (n=74). Some participants were excluded based on more than one criterion, yielding an analytic sample of 16,820 adults.
J Clin Hypertens (Greenwich). 2016;18:232–239. DOI: 10.1111/jch.12654 © 2015 The Authors. The Journal of Clinical Hypertension published by Wiley Periodicals, Inc.
References
- 1. Roger VL, Go AS, Lloyd‐Jones DM, et al. Executive summary: heart disease and stroke statistics–2011 update: a report from the American Heart Association. Circulation. 2011;123:459–463. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2. Nwankwo T, Yoon S, Burt V, Gu Q. Hypertension among adults in the United States: National Health and Nutrition Examination Survey, 2011‐2012. NCHS Data Brief. 2013;133:1–8. [PubMed] [Google Scholar]
- 3. Go AS, Mozaffarian D, Roger VL, et al. Heart disease and stroke statistics–2014 Update: a report from the American Heart Association. Circulation. 2014;129:e28–e292. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4. Ritchey M, Wall H, Gillespie C, et al. CDC Million Hearts: prevalence of leading cardiovascular disease risk factors‐United States, 2005‐2012. MMWR Morb Mortal Wkly Rep. 2014;63:462–467. [PMC free article] [PubMed] [Google Scholar]
- 5. Farley TA, Dalal MA, Mostashari F, Frieden TR. Deaths preventable in the US by improvements in use of clinical preventive services. Am J Prev Med. 2010;38:600–609. [DOI] [PubMed] [Google Scholar]
- 6. Viera AJ, Pathman DE, Garrett JM. Adults' lack of a usual source of care: a matter of preference? Ann Fam Med. 2006;4:359–365. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7. He J, Muntner P, Chen J, et al. Factors associated with hypertension control in the general population of the United States. Arch Intern Med. 2002;162:1051–1058. [DOI] [PubMed] [Google Scholar]
- 8. DeVoe JE, Fryer GE, Phillips R, Green L. Receipt of preventive care among adults: insurance status and usual source of care. Am J Public Health. 2003;93:786–791. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9. Valderrama AL, Gillespie C, King SC, et al. Vital signs: awareness and treatment of uncontrolled hypertension among adults – United States, 2003–2010. MMWR. Morb Mortal Wkly Rep. 2012;61:703–709. [PubMed] [Google Scholar]
- 10. American Medical Association . Improving Health Outcomes. www.ama-assn.org/ama/pub/about-ama/strategic-focus/improving-health-outcomes.page. Accessed November 23, 2014.
- 11. US Department of Health and Human Services . Medicare and Medicaid Programs; Electronic Health Record Incentive Program‐Stage 2 Final Rule. 2012. Available at: www.federalregister.gov/articles/2012/09/04/2012-21050/medicare-and-medicaid-programs-electronic-health-record-incentive-program-stage-2. Accessed November 23, 2014. [PubMed]
- 12. Gliklich R, Dreyer N, Leavy M, eds. Registries for Evaluating Patient Outcomes. A User's Guide, 2nd edn. Rockville, MD: Agency for Healthcare Research and Quality; September 2010. [PubMed] [Google Scholar]
- 13. Gliklich R, Dreyer N, Leavy M, eds. Registries for Evaluating Patient Outcomes: A User's Guide, 3rd edn. Rockville, MD: Agency for Healthcare Research and Quality; April 2014. www.effectivehealthcare.ahrq.gov/registries-guide-3.cfm. Accessed May 9, 2014. [PubMed] [Google Scholar]
- 14. Rai A, Prichard P, Hodach R, Courtemanche T. Using physician‐led automated communications to improve patient health. Popul Health Manag. 2011;14:175–180. [DOI] [PubMed] [Google Scholar]
- 15. Cusack CM, Knudson AD, Kronstadt JL, et al. Practice‐Based Population Health: Information Technology to Support Transformation to Proactive Primary Care. Rockville, MD: Agency for Healthcare Research and Quality; 2010. [Google Scholar]
- 16. Go AS, Bauman MA, King SMC, et al. An effective approach to high blood pressure control: a science advisory from the American Heart Association, the American College of Cardiology, and the Centers for Disease Control and Prevention. J Am Coll Cardiol. 2014;63:1230–1238. [DOI] [PubMed] [Google Scholar]
- 17. Pearson TA, Palaniappan LP, Artinian NT, et al. American Heart Association Guide for Improving Cardiovascular Health at the Community Level, 2013 update a scientific statement for public health practitioners, healthcare providers, and health policy makers. Circulation. 2013;127:1730–1753. [DOI] [PubMed] [Google Scholar]
- 18. Handler J, Lackland DT. Translation of hypertension treatment guidelines into practice: a review of implementation. J Am Soc Hypertens. 2011;5:197–207. [DOI] [PubMed] [Google Scholar]
- 19. Fletcher RD, Amdur RL, Kolodner R, et al. Blood pressure control among US Veterans: a large multiyear analysis of blood pressure data from the Veterans Administration health data repository. Circulation. 2012;125:2462–2468. [DOI] [PubMed] [Google Scholar]
- 20. Centers for Disease Control and Prevention . National Health and Nutrition Examination Survey Data. US Department of Health and Human Services. 2011. www.cdc.gov/nchs/nhanes.htm. Accessed September 1, 2013.
- 21. Okonofua EC, Simpson KN, Jesri A, et al. Therapeutic inertia is an impediment to achieving the Healthy People 2010 blood pressure control goals. Hypertension. 2006;47:345–351. [DOI] [PubMed] [Google Scholar]
- 22. Centers for Disease Control and Prevention National Center for Health Statistics. National Health and Nutrition Examination Survey: Analytic Guidelines, 2011‐2012. 2013. US Department of Health and Human Services. 2013. www.cdc.gov/nchs/data/nhanes/analytic_guidelines_11_12.pdf. Accessed September 1, 2013. [Google Scholar]
- 23. Bland JM, Altman DG. Multiple significance tests: the Bonferroni method. BMJ. 1995;310:170. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24. Calhoun DA, Jones D, Textor S, et al. Resistant hypertension: diagnosis, evaluation, and treatment: a scientific statement from the American Heart Association Professional Education Committee of the Council for High Blood Pressure Research. Circulation. 2008;117:e510–e526. [DOI] [PubMed] [Google Scholar]
- 25. Cushman WC, Ford CE, Cutler JA, et al. ALLHAT Collaborative Research Group: success and predictors of blood pressure control in diverse North American settings: the Antihypertensive and Lipid‐Lowering Treatment to Prevent Heart Attack Trial (ALLHAT). J Clin Hypertens (Greenwich). 2002;4:393–404. [DOI] [PubMed] [Google Scholar]
- 26. Polinski JM, Kilabuk E, Schneeweiss S, et al. Changes in drug use and out‐of‐pocket costs associated with Medicare Part D implementation: a systematic review. J Am Geriatr Soc. 2010;58:1764–1779. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 27. Li P, McElligott S, Bergquist H, et al. Effect of the Medicare Part D coverage gap on medication use among patients with hypertension and hyperlipidemia. Ann Intern Med. 2012;156:776–784. [DOI] [PubMed] [Google Scholar]
- 28. Jaffe MG, Lee GA, Young JD, et al. Improved blood pressure control associated with a large‐scale hypertension program. JAMA. 2013;310:699–705. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 29. Walsh JME, Sundaram V, McDonald K, et al. Implementing effective hypertension quality improvement strategies: barriers and potential solutions. J Clin Hypertens (Greenwich). 2008;10:311–316. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 30. Fenerty SD, West C, Davis SA, et al. The effect of reminder systems on patients' adherence to treatment. Patient Prefer Adherence. 2012;6:127–135. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 31. Egan BM, Li J, Hutchison FN, Ferdinand KC. Hypertension in the United States 1999‐2012: progress toward Healthy People 2020 goals. Circulation. 2014;19:1692–1699. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 32. Rakotz MK, Ewigman BG, Sarav M, et al. A technology‐based quality innovation to identify undiagnosed hypertension among active primary care patients. Ann Fam Med. 2014;12:352–358. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 33. Khatib R, Schwalm J‐D, Yusuf S, et al. Patient and healthcare provider barriers to hypertension awareness, treatment and follow up: a systematic review and meta‐analysis of qualitative and quantitative studies. PLoS One. 2014;9:e84238. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 34. Khanna RR, Victor RG, Bibbins‐Domingo K, et al. Missed opportunities for treatment of uncontrolled hypertension at physician office visits in the United States, 2005 through 2009. Arch Intern Med. 2012;172:1344–1345. [DOI] [PubMed] [Google Scholar]
- 35. Chobanian AV, Bakris GL, Black HR, et al. The seventh report of the Joint National Committee on Prevention, Detection, Evaluation, and Treatment of High Blood Pressure: The JNC 7 Report. Hypertension. 2003;42:1206–1252. [DOI] [PubMed] [Google Scholar]
- 36. Choudhry NK, Fischer MA, Avorn J, et al. The implications of therapeutic complexity on adherence to cardiovascular medications. Arch Intern Med. 2011;171:814–822. [DOI] [PubMed] [Google Scholar]
- 37. Østbye T, Yarnall KSH, Krause KM, et al. Is there time for management of patients with chronic diseases in primary care? Ann Fam Med. 2005;3:209–214. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 38. Frieden TR, King SMC, Wright JS. Protocol‐based treatment of hypertension: a critical step on the pathway to progress. JAMA. 2014;311:21–22. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 39. Esquivel J, White M, Carroll M, Brinker E. Teach‐back is an effective strategy for educating older heart failure patients. Circulation. 2011;124(Suppl 21):A10786. [Google Scholar]
- 40. Egan BM, Laken MA, Shaun Wagner C, et al. Impacting population cardiovascular health through a community‐based practice network: update on an ASH‐supported collaborative. J Clin Hypertens (Greenwich). 2011;13:543–550. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 41. Hyman DJ, Pavlik VN. Self‐reported hypertension treatment practices among primary care physicians: blood pressure thresholds, drug choices, and the role of guidelines and evidence‐based medicine. Arch Intern Med. 2000;160:2281–2286. [DOI] [PubMed] [Google Scholar]
- 42. Oliveria SA, Lapuerta P, McCarthy BD, et al. Physician‐related barriers to the effective management of uncontrolled hypertension. Arch Intern Med. 2002;162:413–420. [DOI] [PubMed] [Google Scholar]
- 43. Walsh JME, McDonald KM, Shojania KG, et al. Quality improvement strategies for hypertension management: a systematic review. Med Care. 2006;44:646–657. [DOI] [PubMed] [Google Scholar]
- 44. Baker R, Camosso‐Stefinovic J, Gillies C, et al. Tailored interventions to overcome identified barriers to change: effects on professional practice and health care outcomes. Cochrane Database Syst Rev 2010;3:CD005470. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 45. Carter BL, Rogers M, Daly J, et al. The potency of team‐based care interventions for hypertension: a meta‐analysis. Arch Intern Med. 2009;169:1748–1755. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 46. Hill MN, Miller NH, DeGeest S. ASH position paper: adherence and persistence with taking medication to control high blood pressure. J Clin Hypertens (Greenwich). 2010;12:757–764. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 47. Sarafidis PA, Bakris GL. Resistant hypertension: an overview of evaluation and treatment. J Am Coll Cardiol. 2008;52:1749–1757. [DOI] [PubMed] [Google Scholar]
- 48. Cushman WC, Ford CE, Einhorn PT, et al. Blood pressure control bydrug group in the Antihypertensive and Lipid‐Lowering Treatment to Prevent Heart Attack Trial (ALLHAT). J Clin Hypertens (Greenwich). 2008;10:751–760. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 49. Steiner JF. Rethinking adherence. Ann Intern Med. 2012;157:580–585. [DOI] [PubMed] [Google Scholar]
- 50. Karliner LS, Jacobs EA, Chen AH, Mutha S. Do professional interpreters improve clinical care for patients with limited English proficiency? A systematic review of the literature. Health Serv Res. 2007;42:727–754. [DOI] [PMC free article] [PubMed] [Google Scholar]


