Abstract
The literature including correlates of parental distress as related to childhood cancer is abundant. It is important to identify predictive factors and outcomes of this distress in parents. The objective of this review was to update previous syntheses on factors of distress and to identify outcomes of parents’ distress in the recent literature (2007–2012). We performed a systematic review to identify all quantitative studies including measures of parental distress and associated factors during the study period. We found 56 eligible studies, of which 43 had a Low risk of bias (Cochrane guidelines). Forty‐two reports included potential predictive factors. Significant relationships were found with clinical history of the child, sex of the parent, coping response and personal resources, pre‐diagnosis family functioning, but not education/income or marital status. Twenty‐five reports studied potential consequences of distress and focused on psychological adjustment in parents and children. Compared to past periods, a higher proportion of studies included fathers. Measures used to evaluate distress were also more homogeneous in certain domains of distress. This review underscores the need for appropriate methods for selecting participants and reporting results in future studies. Appropriate methods should be used to demonstrate causality between factors/consequences and distress.
Keywords: cancer, quality of life, psychological, emotional, families
Introduction
Childhood cancer has been described as a life‐changing experience for parents. Following diagnosis, parents are expected to rapidly learn a substantial amount of cancer‐related information, adopt particular caregiving skills, as well as reorganise their family roles and routines. These adjustments are all aimed at transitioning their focus from parent to parent and primary caregiver of a child with cancer. However, this transition to a dual role is not necessarily a seamless one, and for many it may lead to experiencing considerable emotional strain, which may persist over time (Brown et al. 2003; Wijnberg‐Williams et al. 2006). The most extensive review on the subject indicated that approximately 27% of parents suffered from clinical levels of psychological distress up to 5 years post‐diagnosis (Vrijmoet‐Wiersma et al. 2008). Nevertheless, the literature mentioned in this review as well as more recent empirical studies show important differences in frequencies of distress across samples. Various factors may explain this phenomenon, but recent research has not been synthesised.
Parental stress or distress may refer to a vast array of symptoms, such as uncertainty, anxiety, depression, traumatic stress, psychological health, etc. According to the National Comprehensive Cancer Network (NCCN), distress is defined as ‘a multifactorial unpleasant emotional experience of a psychological (cognitive, behavioural, emotional), social, and/or spiritual nature that may interfere with the ability to cope with cancer, its physical symptoms and its treatment’ (National Comprehensive Cancer Network, 2013). Although it was originally proposed for adult oncology patients, we used this definition in paediatric oncology settings to identify parents’ distress in relation to their child's cancer. As such, parental distress can be approached by a variety of measures including psychological symptom inventories, mixed distress scales, anxiety–depression inventories, mental quality of life (QoL) subscales or traumatic stress inventories. These make it possible to evaluate subclinical distress in the form of frequency or severity of symptoms and infer the presence of clinically significant distress when levels exceed predetermined cut‐points.
Prior to undertaking the present review, we identified two wide‐scope reviews on parental distress published in the last 15 years (Klassen et al. 2007; Vrijmoet‐Wiersma et al. 2008) and three focused reviews on post‐traumatic stress symptoms (PTSS), sex differences or long‐term effects (Kazak & Baxt 2007; Rabineau et al. 2008; Ljungman et al. 2014). These reviews offered a portrait of parental distress as being more elevated at diagnosis for both parents and more elevated in mothers as compared to fathers. Early distress may also have detrimental effects for some parents in the long term (anxiety, depression and traumatic stress). These reviews underlined the fact that data on fathers were lacking and encouraged future longitudinal studies to provide a more representative depiction of parental distress across the cancer trajectory. Identified risk factors in the two wide‐scope reviews included demographic factors (e.g. low socioeconomic status), child factors (e.g. behaviour problems), high caregiving demands, individual coping (e.g. low social support, high emotional coping) and family conflict. To date, only one review has included outcomes of parental distress, but focused predominantly on parenting (Rabineau et al. 2008). It found that parenting stress probably impaired cognitive skills necessary for caregiving (e.g. information processing), thus leading to poorer parental long‐term adjustment to the illness and PTSS, and disrupted emotional adjustment and adherence behaviour in children.
Recent longitudinal follow‐ups have found that parental distress tends to decline from diagnosis to the post‐treatment period, generally reaching normative levels around 3 years post‐diagnosis (Dolgin et al. 2007; Maurice‐Stam et al. 2008b; Barrera et al. 2012; Tremolada et al. 2013). However, other reports suggested that a significant proportion of parents continue to experience psychological difficulties in the long run (between 18% and 30%) (Hardy et al. 2008; Diseth et al. 2011; Ljungman et al. 2014). Large differences were also found when exploring frequencies of psychological symptoms in parents. For example, the frequency of clinical anxiety was found to vary across studies from normative levels (Greening & Stoppelbein 2007; Hardy et al. 2008; Dunn et al. 2012) to more than 37% (Fotiadou et al. 2008). Although these differences may result from differences in measurement, they also seem attributable to factors pertaining to the cancer trajectory, individual coping resources, and social environment, to name a few possibilities.
Although previous reviews have described parental distress, they did not include a clear definition of it. For example, mental QoL was not included in the review by Vrijmoet‐Wiersma et al. (2008), and health was defined very broadly in that of Klassen et al. (2007). Moreover, these reviews did not cover the recent literature. Finally, none of the wide‐scope reviews on the subject included a precise analysis of bias. Despite a rigorous narrative review process, these reviews may have been influenced by studies with High risk of bias. Only one focused review included a risk of bias assessment in a limited sample of 15 studies (Ljungman et al. 2014).
In addition, recent developments plead for an update in the review of factors of parental distress along the cancer trajectory. First, there is ample evidence that medical treatments for childhood cancer have become both more effective and efficient in the past decade (Pui et al. 2008). Although it is unclear to what extent this would impact parental distress, we can assume that better prognosis and general outlooks for children have favourable impacts on distress levels in parents. This may also increase contrast between conditions where such treatment may or may not be available. Second, the recent developments in comprehensive care have placed an increased emphasis on including parents and the family as a strong resource for the child's development and future rehabilitation (Meyler et al. 2010). Diverse types of supportive care have been available for children and their families, including rehabilitation (e.g. occupational therapy), psychological support and information about cancer, which in turn could provide parents with previously unknown resources and assist in alleviating distress (Pai et al. 2006). Parents who received psychological care have reported lower distress (Bennett Murphy et al. 2008). Further, social changes have impacted paediatric care, such that professionals are increasingly giving fathers, as well as mothers, an active role in caring for the ill child. Just as children with diabetes have been shown to benefit from fathers’ involvement in disease management (Dashiff et al. 2008), this trend may also be evident in paediatric cancer. Finally, the attention given to distress in patients and caregivers has dramatically increased as a result of the recognition of distress as the 6th vital sign in adult oncology in 2007 (Holland & Bultz 2007; Accreditation Canada, 2013). It is thus probable that factors and effects of parental distress have changed in recent years.
Interestingly, although previous reviews underscored the issue of consequences of parental distress, none included a detailed examination of this issue. Beyond the significant impact that paediatric cancer can have on parents themselves, parental distress could also be related to major outcomes for the family and the children themselves. Indeed, results have suggested a detrimental effect on the child's emotional adjustment (Merrill et al. 2007) or mental QoL (Roddenberry & Renk 2008; Penn et al. 2009; Yagc‐Kupeli et al. 2012). These hypotheses are consistent with a large body of literature in psychopathology linking parental psychological status with children well‐being (Hammen et al. 2012). Although much effort has been dedicated to describe levels and the evolution of distress in parents (Vrijmoet‐Wiersma et al. 2008), no recent systematic review is available on identifying the factors and the consequences of distress.
The present review has two objectives: (1) to synthesise knowledge on factors of emotional distress in parents confronted by the cancer of their child. We will rely on the definition of distress given earlier and focus on studies measuring one or several aspects of emotional distress in conjunction with factors interpreted by authors as antecedents, risk factors or moderators of distress; (2) to synthesise knowledge on the consequences of parental emotional distress. The objective of this review was not to summarise descriptions, frequencies or evolution of distress over time since these aspects have been extensively studied. Given existing syntheses on the literature prior to 2007, we focus on the 2007–2012 period. We systematically examine the quality of information, and during the interpretation process, we prioritise data from high‐quality studies.
Method
This systematic review was conducted according to the Preferred Reporting Items for Systematic Reviews and Meta‐Analyses (PRISMA) (Moher et al. 2009) and A Measurement Tool to Assess Systematic Reviews (AMSTAR) guidelines (Shea et al. 2007). The protocol was registered on Prospero on 20 September 2013, number CRD42013005772.
Search strategy
The literature search was performed in PubMed, PsycINFO, and CINAHL databases. Articles pertaining to parental distress in paediatric cancer were identified by using the following search terms: MeSH terms for parents (parents; mothers; fathers; family; parent‐child relations) were combined with MeSH terms for distress (mental health; depression; anxiety; adjustment disorder; adaptation psychological; stress, psychological; stress disorders, post‐traumatic; quality of life) and MeSH terms for cancer (neoplasms, brain neoplasms, leukaemia, lymphoma). The review was limited to articles in English published between 1 January 2007 and 31 December 2012.
Inclusion and exclusion criteria
To be selected, studies had to include parents of children that have suffered from cancer during childhood (0–18 years). Studies had to include a valid measure of parental distress, consistent with the definition given in the introduction. As reflected in the search strategy, target studies could include any reference to psychological symptoms (e.g. PTSS), psychiatric conditions (e.g. major depressive disorder), mental health (e.g. mental QoL) or emotional stress and distress (e.g. perceived stress). In the following lines, measures of mixed anxiety/depression symptoms (e.g. HADS total score) or measures integrating various symptoms designed for case identification (e.g. SCL‐90) are referred to as ‘mixed distress’. Studies also included factors associated with measures of distress. Only quantitative studies published in peer‐reviewed journals were included. Studies were excluded if they assessed distress during the end‐of‐life or palliative period, or if they referred to deceased children, as parental distress within these specialised groups was presumed to be different than that experienced by parents during other stages of the illness or survivorship. Finally, because we wished to focus on quantitative empirical studies that were able to yield association estimates, we excluded commentaries, editorials, abstracts, case reports, qualitative studies, review articles, book chapters and dissertations.
Data extraction
Articles were independently screened and assessed by two separate investigators (TL, ER) by examining titles and abstracts to identify relevant studies. In cases of doubt, the full text was reviewed and discussed with all authors. The full texts of retained abstracts were screened by the investigators for final inclusion and data extraction. Studies included in the review were then independently classified by the investigators as relevant to either factors or effects of distress. Records could be relevant to both aspects. Omissions or discrepancies were resolved by consensus. Next, study characteristics (first author, year, country, number of mothers and fathers, proportion of girls in the child sample, child diagnosis, distress instruments, study design, time since diagnosis) and results were extracted by the investigators. Two independent summary tables were elaborated independently (TL and ER) and discrepancies were discussed with all authors.
Risk of bias
According to the standard guidelines for reporting data in systematic reviews (Cochrane guidelines, Higgins & Green 2011), articles included in the review were assessed for risk of bias. We rated the following domains independently: Selection, Attrition, Reporting and Other. Table 1 summarises criteria used for the present evaluation. In the ‘Other’ domain, we adapted Cochrane guidelines to behavioural observational research and rated the criteria on the basis of: Sample size, Measurement quality, Response rate maximisation, Research design and Appropriateness of analyses for hypothesis testing. The rating of biases was performed by two investigators independently (TL and ER). Discrepancies were resolved through discussion involving all authors.
Table 1.
Criteria for judging risk of bias of selected studies, adapted from the criteria suggested by the Cochrane Handbook for systematic reviews of interventions
| Selection bias of participants | |
| ‘Low risk’ of bias |
Sites
|
Recruitment
| |
Inclusion/Exclusion
| |
| ‘High risk’ of bias |
Sites
|
Recruitment
| |
Inclusion/Exclusion
| |
| ‘Unclear risk’ of bias | Insufficient information to permit judgement of ‘Low risk’ or ‘High risk’ |
| Attribution bias (incomplete outcome data from participants) | |
| ‘Low risk’ of bias |
|
| ‘High risk’ of bias |
|
| ‘Unclear risk’ of bias | Insufficient information to permit judgement of ‘Low risk’ or ‘High risk’ |
| Reporting bias (from authors) due to selective outcome reporting | |
| ‘Low risk’ of bias |
Objectives/Hypotheses
|
Demographics
| |
Outcome data/confounds
| |
Discussion/Conclusions
| |
| ‘High risk’ of bias |
Objectives/Hypotheses
|
Demographics
| |
Outcome data/Confounds
| |
Discussion/Conclusions
| |
| ‘Unclear risk’ of bias |
Insufficient information to permit judgment of ‘Low risk’ or ‘High risk’
|
| Other bias | |
| ‘Low risk’ of bias |
Participants
|
Measures
| |
Procedures
| |
Design
| |
| ‘High risk’ of bias |
Participants
|
Measures
| |
Procedures
| |
Design
| |
| ‘Unclear risk’ of bias | Insufficient information to permit judgement of ‘Low risk’ or ‘High risk’ |
Arber S. (2001) Designing samples. In: Researching Social Life (ed. Gilbert N). SAGE Publications, London.
Tabachnick B.G. & Fidell, L.S. (2007) Using Multivariate Statistics, 5th edn. Pearson, Boston, MA.
Of the 56 articles included, 43 had an overall Low risk of bias, 11 had a High risk of bias and 2 had an Unclear risk of bias (Table S1). Most frequent reasons for rating High or Unclear risk were: convenience samples, insufficient description of children diagnoses or lack of socio‐demographic data on participants, recruitment or selection procedure not specified or too vague, small sample size with regard to analyses, unspecified response rate, time since diagnosis not specified or heterogeneous. Most frequent biases domains in the 56 articles were Selection biases (18 High risk and 2 Unclear risk) and Other (18 High risk and 2 Unclear risk). Domains were aggregated into one global rating, using recommendations from the Cochrane guidelines. In case of tie (e.g. two Low risk and two Unclear risk ratings), we adopted a conservative approach by rating the lowest level (in the example the global rating was Unclear risk). Studies being globally rated as Low risk were retained for further analysis and interpretation. A summary table describing studies rated as Unclear or High risk of bias is available as an online supplement (Table S2).
Results
Study selection
The search initially identified 1212 articles. After screening titles and abstracts, 930 articles were excluded because they did not include data on childhood cancer or parental distress. Two hundred and eighty‐two full‐text articles were then examined for eligibility, of which 228 were discarded, most of them because they were not quantitative empirical studies (see flow chart in Fig. 1). Fifty‐four articles fulfilled the inclusion criteria. Reference lists of all eligible articles were also reviewed. We identified two additional studies meeting our criteria in these reference lists, making up a total of 56 articles reviewed. Among these reports, 43 were rated as bearing a Low risk of bias and are the focus of the present review.
Figure 1.
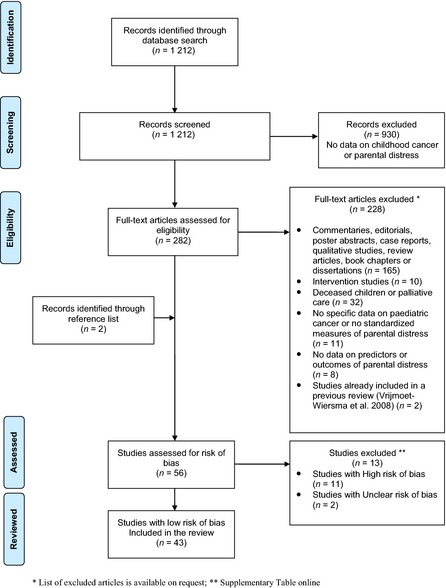
Flow of information through the different phases of the systematic review.
Study characteristics
Between 2007 and 2012, we found 42 studies pertaining to factors of parental distress and 25 studies on consequences of parental distress. The studies are summarised in Table 2. Most studies were cross‐sectional (n = 37, 66%), the others being prospective follow‐ups (n = 18, 32%) or retrospective studies (n = 1, 2%). Thirteen studies were group comparisons, of which nine were case–control designs. Although overlap was probable in a number of studies, it can be estimated that approximately 7000 parents participated during the review period, from 15 countries. Participants were predominantly mothers (72%). Eleven studies included exclusively mothers, and two studies did not report parent sex. Overall, parents of girls comprised approximately 45% of the total retrieved studies. Most studies (88%) were comprised of parents of children with heterogeneous cancer diagnoses (Leukaemia, CNS tumour or other). Seven studies also included children with other diagnoses than cancer.
Table 2.
Summary table of reviewed articles on factors and outcomes of parental distress in the context of paediatric cancer (N = 43, 2007–2012, low risk of bias)
| Author (year) | Sample | Child diagnosis (%) | Measure (distress) | Design | Summary of results | ||||||
|---|---|---|---|---|---|---|---|---|---|---|---|
| Parents | Girls (%) | Time post‐diagnosis | Country | LK | CNS | Other | Type | Times of assessment | |||
| Predictors | |||||||||||
| Dolgin et al. (2007) | 212 M | 45 | – | USA/Israel | 43 | 18 | 30 | POMS | L | T1: 2 months PD | Mixed distress, depression and PTSS not associated with age (child and M), gender, diagnosis, marital status and education over time. General distress and depression associated with neuroticism and poor social problem‐solving skills over time. PTSS associated with immigrant status over time |
| BDI‐II | T2: 5 months PD | ||||||||||
| IES‐R | T3: 8 months PD | ||||||||||
| Gerhardt et al. (2007) |
Cases: 48 M 33 F |
37 | 18 months | USA | 51 | – | 49 | SCL‐90‐R | C | – | No association between mixed distress and social support |
|
Controls: 49 M 29 F |
37 | ||||||||||
| Greening and Stoppelbein (2007) |
141 M 9 F |
53 | 4 years | USA | 50 | – | 50 | BDI‐II | C | – | Depression and PTSD associated with more negative self‐blame/affect and substance use. State anxiety associated with more negative self‐blame/affect and active coping. Lower state anxiety associated with more religious coping/optimism and social support/advice seeking |
| PTSD‐RI | |||||||||||
| STAI‐State | |||||||||||
| Ozono et al. (2007) |
87 M 72 F |
56 | 5–10 years (44%) | Japan | 67 | – | 33 | IES‐R | C | – | Severe PTSS associated with higher trait anxiety, poorer family functioning and shorter time since diagnosis in M, and with higher trait anxiety in F |
| >10 years (56%) | STAI | ||||||||||
| Fotiadou et al. (2008) |
Cases: 70 M 30 F |
34 | n/a | UK | 66 | 8 | 27 | HADS | C | – | Lower anxiety and depression associated with higher levels of optimism in both groups |
|
Controls: 87 M 30 F |
39 | SF‐36v2 | |||||||||
| Hoven et al. (2008) |
182 M 139 F |
n/a | 19 months | Sweden | 65 | 26 | 9 | PPD‐C | C | – | Depression associated with more complicated cancer diagnosis |
| Klassen et al. (2008) |
358 M 50 F |
43 | ≤1 year (69%) | Canada | 61 | 11 | 28 | SF‐36 | C | – | Higher mental QoL associated with more exercise, better eating habits, better sleep quality, better child's health, less intense treatment and longer time since diagnosis. Mental QoL not associated with parental age, sex, marital status, education, income and smoking status |
| >1 year (31%) | |||||||||||
| Maurice‐Stam et al. (2008b) |
122 M 109 F |
42 | 14 months | NET | 48 | 5 | 47 | GHQ‐30 | L | T1: 2 months PT | Lower mixed distress associated with older maternal age, lower perceived intensity of treatments, longer treatments, family cohesion and optimism over time. General distress associated with recent important family events in M and passive and lower palliative (leisure) coping in F over time |
| T2: 1 year PT | |||||||||||
| T3: 2 years PT | |||||||||||
| SSERQ | T4: 3 years PT | ||||||||||
| T5: 4 years PT | |||||||||||
| T6: 5 years PT | |||||||||||
| Patiño‐Fernandez et al. (2008) |
129 M 72 F |
44 | 1–2 weeks | USA | 38 | 23 | 39 | ASDS | C | – | General anxiety associated with symptoms of acute stress in both M and F |
| STAI‐Y | |||||||||||
| Pöder et al. (2008) |
107 M 107 F |
47 | ≤14 days | Sweden | 44 | 12 | 44 | PCL‐C | L | T1: 1 week PD | ASD/PTSD associated with unemployment (T1, T2, T3), immigrant status (T2), female child gender, younger parental age, lone child status (T1) and past trauma (T1 and T3) |
| T2: 2 months PD | |||||||||||
| T3: 4 months PD | |||||||||||
| Han et al. (2009) | 200 M | n/a | <6 months (49%) | Korea | 45 | 9 | 46 | PAIS | C | – | Lower mixed distress related with family integration, cooperation, optimistic definition of the situation, social support, self‐esteem, psychological stability and understanding the healthcare situation through communication with other parents and with the healthcare team |
| Hutchinson et al. (2009) |
On‐treatment: 38 M 19 F |
51 | 12 months | USA | – | 100 | – | BSI | C | – | Mixed distress, anxiety, depression and PTSS associated with active treatment status. Both groups reported high PTSS |
|
Off‐treatment: 35 M 8 F |
51 | 57 months | IES | ||||||||
| Iobst et al. (2009) | Alone: 87 M | n/a | 2–16 weeks | USA | 49 | 13 | 38 | POMS | C | – | Lower PTSS and better mood associated with positive problem‐solving skills |
| Married/partnered: 377 M | n/a | BDI‐II | |||||||||
| IES‐R | |||||||||||
| Jobe‐Shields et al. (2009) |
119 M 18 F |
43 | 26 months | USA | 67 | – | 33 | CES‐D | C | – | Lower depression moderated the association between family cohesion/expressiveness and child‐reported distress |
| Jurbergs et al. (2009) |
On‐treatment: 60 M 8 F |
41 | ≤1–6 months (56%) | USA | 39 | 17 | 44 | IES‐R | C | – | PTSS not associated with case/control status. PTSS elevated in the on‐treatment group. PTSS associated with longer time since diagnosis and relapse |
|
Off‐treatment: 100 M 25 F |
52 | >5 years (41%) | 23 | 25 | 52 | ||||||
|
Controls: 98 M 9 F |
59 | ||||||||||
| Robinson et al. (2009) |
Cases: 53 M 31 F |
35 | 7 years (survivors) | USA | 36 | – | 64 | SCL‐90‐R | L | T1: 18 months PD | The association between mixed distress (in M, T1) and survivor‐reported depression (T2) moderated by male child gender and lower treatment intensity. The association between general distress (in F, T1) and survivor‐reported negative mood (T2) moderated by higher treatment intensity. The association between general distress (in M, T1) and M‐reported child internalising symptoms (T2) and survivor‐reported negative mood (T2) moderated by more late effects |
|
Controls: 60 M 46 F |
27 | BDI | T2: 7 years PD | ||||||||
| POMS | |||||||||||
| Ozono et al. (2010) |
87 M 72 F |
55 | 10.8 years | Japan | 68 | ‐ | 32 | IES‐R | C | – | PTSS, depression and state‐trait anxiety associated with low family cohesiveness and expressiveness and elevated conflict |
| STAI | |||||||||||
| SDS | |||||||||||
| Bruce et al. (2011) |
46 M 6 F |
n/a | n/a | UK | – | 100 | – | IES‐R | C | – | PTSS associated with higher number of tumour recurrences and lower conflict resolution |
| Demirtepe‐Saygili and Bozo (2011b) | 90 M | n/a | 14 months since first symptoms | Turkey | 100 | – | – | BDI | C | – | Depression associated with lower satisfaction with basic needs and daily activities and more role strain at work. Association between stressors and depression mediated by emotion‐focussed coping and social support |
| Gudmundsdottir et al. (2011) |
114 M 76 F |
33 | 4–18 months | Sweden/Iceland | 47a | 13a | 32a | PPD‐C | C | – | Mixed distress associated with lower sense of coherence |
| GHQ‐12 | |||||||||||
| Hoekstra‐Weebers et al. (2012) |
85 M 79 F |
33 | – | NET | 40–38 | 12–7 | 48–55 | GHQ | L | T1: 14 days PD | Mixed distress not associated with parent gender, education and number of children (T1, T2, T3, T4), but associated with parent age (T1). In F, mixed distress associated cross‐sectionally with palliative (T2), avoidant (T2, T3), passive coping (T2), social support seeking (T2, T3) and expression of emotions (T2, T3). Mixed distress (T2, T3, T4) associated with passive, avoidant coping and expression of emotions (T1); lower general distress (T4) associated with problem‐focused coping (T1). In M, general distress (T3) associated with lower social support seeking (T1). General distress (T2, T3, T4) asso ciated with passive coping and social support seeking (T1) |
| T2: 6 months PD | |||||||||||
| T3: 1 year PD | |||||||||||
| T4: 5 years PD | |||||||||||
| Klassen et al. (2011) |
Cases 1: 245 M 40 F |
45 | Case 1: <12 months | Canada | 56–72 | 11–11 | 33–17 | SF‐36v2 | C | – | Higher mental QoL associated with higher mastery and self‐esteem and perceiving more family‐centred services for the child in the Case 1 group, and with caregiver strain in both groups |
|
Cases 2: 113 M 13 F |
39 | Case 2: >12 months | |||||||||
| Norberg et al. (2011) |
111 M 109 F |
47 | From diagnosis | Sweden | 39 | 12 | 49 | PCL‐C | L | T1: 8 days PD | PTSS/PTSD (T5) associated with avoidance coping (T1–T4) |
| T2: 61 days PD | |||||||||||
| T3: 120 days PD | |||||||||||
| T4: 13 days PT | |||||||||||
| T5: 374 days PT or child's death | |||||||||||
| Miller et al. (2011)b |
162 M 57 F |
n/a | 11 months | USA | 30 | – | 70 | POMS‐Bi | C | ‐ | Mixed distress associated with external influence. This association mediated by decision‐making (autonomy) and task‐focused coping |
| Barrera et al. (2012)c |
49 M 35 F |
n/a | 24 months | Canada | 49 | – | 41 | SF‐36 | L | T1: pre‐SCT | Lower mental QoL (T3) associated with child behaviour problems (T1), poor health (T1) and female child gender in M and F as well as treatment severity in F |
| T2: 1 year post‐SCT | |||||||||||
| T3: 2 years post‐SCT | |||||||||||
| Klassen et al. (2012) |
Two‐parent: 237 M 38 F |
41 | 0.5 year | Canada | 68 | 12 | 20 | SF‐36v2 | C | – | Lower mental QoL associated with lower mastery and self‐esteem, greater impact on the family and poorer child's mental QoL |
|
Single‐parent: 37 M 3 F |
53 | 80 | 8 | 12 | |||||||
| Landolt et al. (2012)d |
68 M 57 F |
39 | – | SWI | n/a | n/a | n/a | PDS | L | T1: 5–6 weeks PD/accident | PTSS (T1) associated with more days spent in hospital (T1). Parental PTSS (T1) not associated with child's PTSS (T1) |
| T2: 1 year PD/accident | |||||||||||
| Norberg et al. (2012) |
112 M 112 F |
47 | ‐ | Sweden | 40 | 12 | 48 | PCL‐C | L | T1: 8 days PD | PTSS (T6) associated with Nordic ethnicity, being unemployed at diagnosis, perception of their child's psychological, physical and total symptoms (T3), and death of the child, but not with parent gender, family income, previous trauma, child's prognosis, treatment intensity, non‐fatal relapse and satisfaction with the child's care |
| T2: 61 days PD | |||||||||||
| T3: 120 days PD | |||||||||||
| T4: 13 days PT | |||||||||||
| T5: 96 days PT | |||||||||||
| T6: 374 days PT | |||||||||||
| McCarthy et al. (2012) |
135 M 85 F |
42 | – | Australia | 41–44 | 14–9 | 45–47 | ASDS (T1) | L | T1: diagnosis | ASD (T1) associated with being a M, psychosocial risk factors, trait anxiety, poor family functioning and brain tumour diagnosis. PTSS (T2) associated with younger maternal age and trait anxiety (T1), and parent‐reported child QoL (T2) |
| PCL‐C (T2) | T2: 6–8 months PD | ||||||||||
| Rodriguez et al. (2012) |
191 M 95 F |
43 | 2 months | USA | 38 | 11 | 51 | RSQ | C | – | PTSS associated with cancer communication stress and caregiving stress, but not with child age and family income |
| PSS | |||||||||||
| IES‐R | |||||||||||
| Tremolada et al. (2012) | 94 M | 48 | – | Italy | 100 | – | – | PTSD‐S‐C | L | T1: 1 week PD | The association between emotional‐focused coping and general distress cross‐sectionally mediated by memory problems (T1). The association between social support and general distress mediated by current life perception (T1). The association between routine and time reorganisation and PTSS mediated by state anxiety and cognitive problems (T3, T4). |
| T2: 1 month PD | |||||||||||
| BSI‐18 | T3: 6 months PD | ||||||||||
| T4: 12 months PD | |||||||||||
| Tremolada et al. (2013) | 76 M | 50 | – | Italy | 100 | – | – | BSI‐18 | L | T1: 1 week PD | PTSS (T2, T3, T3, T4) was associated with more days of hospitalisation (T1, T3), mothers’ education (T1, T2), stress events (T1), child's age (T5), cognitive functioning (T1, T2, T3, T4, T5) |
| PTSD‐SC | T2: 1 month PD | ||||||||||
| T3: 6 months PD | |||||||||||
| T4: 12 months PD | |||||||||||
| T5: 24 months | |||||||||||
| Outcomes | |||||||||||
| Norberg and Boman (2007) |
29 M 22 F |
n/a | – | Sweden | 20 | 8 | 72 | STAI‐State | L | T1: 1–6 months | Depression (T1) predicted a greater decrease in perceived social support. Anxiety (T1) and gender not associated with change in perceived support |
| T2: 12–24 months | |||||||||||
| Barrera et al. (2008) | 103 parents | n/a | 20 months | Canada | 48 | – | 52 | BDI | L | T1: transplant | Depression moderates the effect of time on child verbal IQ. Depression predicted lower perceptual IQ over time, lower verbal IQ (T2 and T3) and lower visual motor scores (T2) |
| T2: 12 months PT | |||||||||||
| T3: 24 months PT | |||||||||||
| Colletti et al. (2008) |
53 M 9 F |
45 | 9 months | USA | 52 | 11 | 37 | PSI‐SF | C | – | Parenting stress predicted poor parent‐rated behavioural, emotional and social adjustment in children |
| Maurice‐Stam et al. (2008a) |
34 M 19 F |
51 | 15 months | NET | 45 | – | 55 | GHQ‐30 | L | T1: 2 months PT | Longer treatments, poor prognosis and parental mixed distress predicted worse children physical QoL, but not child mental QoL (parent‐reported) over time |
| T2: 1 year PT | |||||||||||
| T3: 2 years PT | |||||||||||
| T4: 3 years PT | |||||||||||
| Pöder et al. (2008) |
107 M 107 F |
47 | ≤14 days | Sweden | 44 | 12 | 44 | PCL‐C | L | T1: 1 week PD | ASD (T1) predicted PTSD (T3) in half of the sample |
| T2: 2 months PD | |||||||||||
| T3: 4 months PD | |||||||||||
| Barrera et al. (2009) | 99 M | 66 | 19 months | Canada | 46 | – | 54 | BDI | L | T1: pre‐SCT | Depression predicted child externalising and internalising behaviours (parent‐reported) but not competence scores, and problem behaviour and social competence (child‐reported) |
| T2: 12 months after SCT | |||||||||||
| T3: 24 months after SCT | |||||||||||
| Jobe‐Shields et al. (2009) |
119 M 18 F |
43 | 26 months | USA | 67 | – | 33 | CES‐D | C | – | Depression predicted child‐reported distress |
| Robinson et al. (2009) |
Cases: 53 M 31 F |
35 | 7 years (survivors) | USA | 36 | – | 64 | SCL‐90‐R | L | T1: 18 months PD | Mixed distress (T1) predicted child internalising symptoms (parent‐reported, not child‐reported, T2) |
|
Controls: 60 M 46 F |
27 | BDI | T2: 7 years PD | ||||||||
| POMS | |||||||||||
| Davis et al. (2010) |
160 M 33 F |
48 | 1–18 months (50%) | USA | 30 | 22 | 48 | IES‐R | C | – | PTSS predicted child emotional (self‐ and parent‐reported) and behavioural difficulties (parent‐reported). Child anger regulation moderated the association between PTSS and child emotional (parent and child‐reported) and behavioural difficulties (parent‐reported) |
| 18 months–5 years (24%) | |||||||||||
| ≥5 years (26%) | |||||||||||
| Norberg (2010) |
24 M 20 F |
n/a | 42 months | Sweden | – | 100 | – | PSS | C | T1 | Stress (T1) predicted burnout symptoms (T2) |
| T2: 7 months after T1 | |||||||||||
| Pöder et al. (2010) |
107 M 107 F |
47 | ≤14 days | Sweden | 44 | 12 | 44 | PCL‐C | L | T1: 1 week PD | PTSD (T2–T3) is associated with more severe perception of children's symptom burden |
| T2: 2 months PD | |||||||||||
| T3: 4 months PD | |||||||||||
| Witt et al. (2010) |
Cases: 68 M 6 F |
47 | ≤2 years (50%) | USA | 47 | 36 | 17 | SF‐12v2 | C | – | Stress mediated the effect of being a parent of a child with cancer on poorer mental QoL |
|
Controls: 113 M 16 F |
52 | ≥3 years (50%) | C‐SOSI | ||||||||
| PSS | |||||||||||
| Wolfe‐Christensen et al (2010) | 36 M | 42 | 12 months | USA | 60 | 14 | 26 | PSI‐SF | C | – | Parenting stress predicted poorer child adjustment (parent‐reported problems of internalising, externalising and prosocial behaviour) |
| Hoekstra‐Weebers et al. (2012) |
85 M 79 F |
33 | – | NET | 40–38 | 12–7 | 48–55 | GHQ | L | T1: 14 days PD | Mixed distress (T1) predicted mixed distress at T2 and T3 in M and F |
| T2: 6 months PD | |||||||||||
| T3: 1 year PD | |||||||||||
| T4: 5 years PD | |||||||||||
| Landolt et al. (2012)d |
68 M 57 F |
39 | – | SWI | n/a | n/a | n/a | PDS | L | T1: 5–6 weeks PD/accident | Higher PTSS in parents (T1) predicted poorer recovery from PTSS in the child (T2). PTSS change in parents (T1–T2) not associated with PTSS change in children (T1–T2) |
| T2: 1 year PD/accident | |||||||||||
| McCarthy et al. (2012) |
135 M 85 F |
42 | – | Australia | 41–44 | 14–9 | 45–47 | ASDS (T1) | L | T1: diagnosis | Severity of ASD symptoms (T1) predicted PTSS (T2) |
| PCL‐C (T2) | T2: 6–8 months PD | ||||||||||
| Tremolada et al. (2012) | 94 M | 48 | – | Italy | 100 | – | – | PTSD‐S‐C | L | T1: 1 week PD | Mixed distress (T1) predicted PTSS (T2) |
| T2: 1 month PD | |||||||||||
| BSI‐18 | T3: 6 months PD | ||||||||||
| T4: 12 months PD | |||||||||||
| Yagc‐Kupeli et al. (2012) |
Cases: 128 M 154 F |
42 | <1 year PT (17%) | Turkey | – | 14 | 86 | BSI | C | – | Mixed distress predicted lower school, physical, emotional and social functioning of children in both groups (parent‐ and child‐reported) |
|
Controls: 170 M 99 F |
56 | 1–5 years PT (45%) | |||||||||
| >5 years PT (38%) | |||||||||||
LK, leukaemia; CNS, central nervous system tumours; L, longitudinal; C, cross‐sectional; M, mothers; F, fathers; PD, post‐diagnosis; PT, post‐treatment; SCT, stem cell transplantation; ASD, acute stress disorder; PTSD, post‐traumatic stress disorder; PTSS, post‐traumatic stress symptoms; QoL, quality of life; USA, United States of America; UK, United Kingdom; NET, the Netherlands; SWI, Switzerland; n/a, not applicable.
Data missing (8%).
Cancer = 84%; Congenital heart disease = 11%; other serious illness = 5%.
Cancer = 90%; Blood disorders = 10%.
Cancer = 27%; Accident = 48%; Diabetes = 25%.
When examining instruments used to evaluate distress in parents (Table 3), we found they predominantly assessed mixed distress (32 studies) using instruments evaluating general stress (such as the PSS) or mixed symptoms especially in the anxiety and depression domains (such as the SCL‐90‐R or its short forms). In this category, a wide variety of instruments were used. Eight studies also assessed mental QoL. Twenty‐one studies assessed post‐traumatic stress or PTSD. Half of these used the IES/IES‐R, which underscores a higher homogeneity among measures in this domain. Depression and anxiety were explored independently in 15 and 11 studies respectively. We noted a remarkable homogeneity of measures in depression where 12/15 studies used the Beck inventories. Finally, as reflected in Table 3, the vast majority of studies used self‐description and only one used a structured interview to diagnose clinical depression and anxiety.
Table 3.
Instruments used to measure emotional distress in 56 studies
| Category | Acronym | Instrument | N studiesa |
|---|---|---|---|
| Mixed distress | BSI | Brief Symptom Inventory | 5 |
| C‐SOSI | Calgary Symptoms of Stress Inventory | 2 | |
| GHQ | General Health Questionnaire | 5 | |
| HADS | Hospital Anxiety and Depression Scale | 1 | |
| PAIS | Psychosocial Adjustment to Illness Scale | 1 | |
| POMS | Profile of Mood States | 4 | |
| PPD‐C | Parental Psychosocial Distress in Cancer | 2 | |
| PSI‐SF | Parenting Stress Inventory‐Short Form | 3 | |
| PSS | Perceived Stress Scale | 5 | |
| RSQ | Response to Stress Questionnaire‐Paediatric Cancer Version | 1 | |
| SCL‐R | Symptom Checklist 35 and 90 Revised | 3 | |
| Mental QoL | SF‐12v2 | Short‐Form 12 Health Survey Version 2 | 2 |
| SF‐36 | Short‐Form 36 Health Survey Version 1 and 2 | 6 | |
| Anxiety | BAI | Beck Anxiety Inventory | 3 |
| SBAS | State‐based Anxiety Scale | 1 | |
| STAI | State‐Trait Anxiety Inventory | 6 | |
| SCID I | Structured Clinical Interview for DSM‐IV, Axis I disorders | 1 | |
| Depression | BDI | Beck Depression Inventory, First and Second Edition | 12 |
| CES‐D | Center for Epidemiologic Studies Depression Scale | 1 | |
| SDS | Zung Self‐Rating Depression Scale | 1 | |
| SCID I | Structured Clinical Interview for DSM‐IV, Axis I disorders | 1 | |
| Traumatic stress | ASDS | Acute Stress Disorder Scale | 2 |
| IES | Impact of Event Scale, Original and Revised | 10 | |
| PCL‐C | PTSD Checklist‐Civilian Version | 5 | |
| PDS | Post‐traumatic Diagnostic Scale | 1 | |
| PTSD‐RI | Post‐traumatic Stress Disorder Reaction Index | 1 | |
| PTSD‐S‐C | PTSD Symptom Checklist | 2 |
Note (full references available on request): BSI, Brief Symptom Inventory (Derogatis & Spencer, 1982; Derogatis, 1992, 2000); C‐SOSI, Calgary Symptoms of Stress Inventory (Carlson & Thomas, 2007); GHQ, General Health Questionnaire (Goldberg & Williams, 1988, 1991; Goldberg, 1992); HADS, Hospital Anxiety and Depression Scale (Zigmond & Snaith, 1983); PAIS, Psychosocial Adjustment to Illness Scale (Derogatis, 1986); POMS, Profile of Mood States (McNair et al. 1992; Lorr & McNair, 1988); PPD‐C, Parental Psychosocial Distress in Cancer (Van Dongen‐Melman et al. 1995); PSI‐SF, Parenting Stress Inventory‐Short Form (Abdin, 1990); PSS, Perceived Stress Scale (Cohen & Kamarck, 1983); RSQ, Response to Stress Questionnaire‐Paediatric Cancer Version (Miller et al. 2009); SCL‐R, Symptom Checklist 35 and 90 Revised (Derogatis, 1994, 1983); SF‐12v2, Short‐Form 12 Health Survey Version 2 (Ware et al. 1996); SF‐36, Short‐Form 36 Health Survey Version 1 and 2 (Ware, Snow & Kosinski, 2000; Ware, Kosinski & Dewey, 2000); BAI, Beck Anxiety Inventory (Beck & Steer, 1990); SBAS, State‐based Anxiety Scale (Marteau & Bekker, 1992); STAI, State‐Trait Anxiety Inventory (Spielberger et al. 1983); SCID I, Structured Clinical Interview for DSM‐IV, Axis I disorders (First et al. 1997); BDI, Beck Depression Inventory, First and Second Edition (Beck, 1978; Beck & Steer, 1993; Beck et al. 1996); CES‐D, Center for Epidemiologic Studies Depression Scale (Radloff, 1977; Shrout & Yager, 1989); SDS, Zung Self‐Rating Depression Scale (Zung, 1965); ASDS, Acute Stress Disorder Scale (Bryant et al. 2000); IES, Impact of Event Scale, Original and Revised (Horowitz et al. 1979; Weiss & Marmar, 1997); PCL‐C, PTSD Checklist‐Civilian Version (Weathers et al. 1993); PDS, Post‐traumatic Diagnostic Scale (Foa et al, 1997); PTSD‐RI, Post‐traumatic Stress Disorder Reaction Index (Frederick, 1985); PTSD‐S‐C, PTSD Symptom Checklist (Manne et al. 1998).
References available on request.
Study findings
Factors of distress
When focusing on studies with a low risk of bias, we found that factors explaining distress could be classified in three groups, those exploring illness/trajectory factors, factors related to individual characteristics, or family factors.
Illness and trajectory
Twelve studies explored how the child's cancer trajectory and treatment may impact parental distress. Coherent with the psychological theory of adaptation, a shorter time since diagnosis was associated with higher general distress and PTSS beyond 5 years post‐diagnosis (Ozono et al. 2007; Klassen et al. 2008), and an active treatment status was associated with higher levels of general distress, depression, anxiety and PTSS (Hutchinson et al. 2009; Jurbergs et al. 2009) in comparison to off‐treatment or survivorship periods. Complicated cancer types (e.g. brain tumours), intense treatments, more hospitalisation days and activity limitations were also related to higher levels of general distress, anxiety, depression and PTSS (Hoven et al. 2008; Klassen et al. 2008; Robinson et al. 2009), as confirmed by prospective studies controlling for baseline distress (McCarthy et al. 2012; Tremolada et al. 2013). Except for one study (Norberg et al. 2012), tumour relapse was associated with higher PTSS (Jurbergs et al. 2009; Bruce et al. 2011). The association between parental distress and demanding clinical situations is reflected in the fact that higher levels of caregiving strain (time and effort dedicated to the child) were consistently related to higher levels of mixed distress, anxiety and PTSS over the first year post‐diagnosis (Klassen et al. 2011; Rodriguez et al. 2012). Interestingly, parents of children diagnosed at a young age did not report higher distress in medium length follow‐ups (Rodriguez et al. 2012; Tremolada et al. 2013).
Individual factors
Eighteen studies included demographic predictors of parental distress.
Mothers reported overall higher distress levels (Gerhardt et al. 2007; Fotiadou et al. 2008) but cross‐sectional results suggested that this is the case only at time of diagnosis and during active treatment. Higher levels and rates of PTSS, mixed distress, anxiety and depressive symptoms are noted in mothers when compared to controls during the first year post‐diagnosis (Gerhardt et al. 2007; Fotiadou et al. 2008; Rodriguez et al. 2012). Notably, these differences in distress between mothers and fathers tend to even out across the cancer trajectory. The higher rates of significant distress observed in mothers following the completion of treatment decreased to levels similar to those of fathers at 1–5 years post‐treatment when comparing parents of the same cancer patient (Maurice‐Stam et al. 2008b). Levels of distress within parental dyads were alike during the off‐treatment and survivorship period (Ozono et al. 2007). Consistent with this pattern, mental QoL improved over 2 years in mothers of children who underwent stem cell transplantation, while no such improvement was found for fathers (Barrera et al. 2012). Interestingly, only seven studies included formal comparisons of parental dyads from the same family (Ozono et al. 2007; Maurice‐Stam et al. 2008b; Pöder et al. 2008; Robinson et al. 2009; Witt et al. 2010; Barrera et al. 2012; McCarthy et al. 2012).
Studies suggested that younger parental age, particularly in mothers, predicted higher mixed distress and PTSS up to 5 years post‐diagnosis (Maurice‐Stam et al. 2008b; Pöder et al. 2008; Hoekstra‐Weebers et al. 2012; McCarthy et al. 2012) with the exception of (Dolgin et al. 2007; Klassen et al. 2008). Three of the four studies finding a significant association controlled for initial distress levels. Moreover, having an immigrant status prospectively predicted traumatic stress within the first year post‐diagnosis (Dolgin et al. 2007; Pöder et al. 2008).
Marital status was not associated with mixed distress, depression, anxiety or PTSS (Dolgin et al. 2007; Klassen et al. 2008; Iobst et al. 2009; Hoekstra‐Weebers et al. 2012). Mixed results were found with regard to parental education. Three studies found no association between parental education and mixed distress, depression and PTSS over the first 5 years post‐diagnosis (Dolgin et al. 2007; Klassen et al. 2008; Hoekstra‐Weebers et al. 2012). One study found that lower education was associated with higher depression scores and PTSS up to 1 year post‐diagnosis (Demirtepe‐Saygili & Bozo 2011a; Tremolada et al. 2013). Notably, family income was not associated with distress (Klassen et al. 2008; Norberg et al. 2012; Rodriguez et al. 2012). In a Jordanian study, a greater distance from home to the hospital was related with lower levels of mixed distress for mothers and higher levels for fathers (Masa'Deh et al. 2012), perhaps because fathers traditionally drive mothers to the hospital in this country. The literature also suggested that within the first year post‐diagnosis, underemployment, lower career achievement and general role strain (e.g. from work) were associated with higher distress, anxiety, depression and PTSS in parents (Fotiadou et al. 2008; Demirtepe‐Saygili & Bozo 2011b; Norberg et al. 2012). On the contrary, having a healthier lifestyle (e.g. exercise, nutrition, sleep, leisure) was cross‐sectionally associated with lower parental mixed distress, anxiety and depression (Klassen et al. 2008; Demirtepe‐Saygili & Bozo 2011b).
Nineteen studies pertained to psychological factors such as coping. Except for one study (Norberg et al. 2012), prospective studies suggested that negative affectivity (i.e. neuroticism, trait anxiety), psychosocial risk, cognitive functioning and poor problem‐solving were vulnerability factors for later mixed distress, depression and traumatic stress in the first 2 years post‐diagnosis (Dolgin et al. 2007; McCarthy et al. 2012; Tremolada et al. 2013). These reports controlled for baseline distress in their analyses. Cross‐sectional studies also found these associations (in addition to an association with anxiety) over more than 10 years post‐diagnosis (Ozono et al. 2007, Iobst et al. 2009). They also reported that parents with lower self‐esteem and mastery suffered from higher mixed distress within the first year post‐diagnosis (Han et al. 2009; Klassen et al. 2011, 2012). In these studies on psychological factors, it is probable that candidate factors and distress be partly confounded though. An original finding was that in an environment in which much external influence is received (by doctors, family), parents who are more autonomous and task‐focused experience elevated mixed distress when taking decisions about treatments (Miller et al. 2011).
With regard to coping strategies, prospective studies controlling for baseline distress indicated that avoidant and passive (withdrawal) coping around the time of diagnosis predicted higher mixed distress and PTSS 1–5 years later (Maurice‐Stam et al. 2008b; Hoekstra‐Weebers et al. 2012). On the contrary, using more problem‐focused coping at diagnosis predicted lower mixed distress 1 year later (Hoekstra‐Weebers et al. 2012), a result which was also found in a cross‐sectional study assessing anxiety and depression in conjunction with coping (Demirtepe‐Saygili & Bozo 2011b). Religious beliefs, optimism and resilience were also associated with lower mixed distress, anxiety, depression and traumatic stress in both prospective (Maurice‐Stam et al. 2008b; Tremolada et al. 2012) and cross‐sectional studies (Greening & Stoppelbein 2007; Fotiadou et al. 2008; Han et al. 2009; Gudmundsdottir et al. 2011) up to 5 years post‐diagnosis. Palliative coping (leisure) in fathers longitudinally predicted lower distress over 5 years post‐diagnosis (Maurice‐Stam et al. 2008b), but these variables were not significantly associated when measured concurrently (Hoekstra‐Weebers et al. 2012). A prospective study including a mixed mother/father sample suggested that social support seeking around the time of diagnosis predicted elevated mixed distress 5 years later, particularly in fathers (Hoekstra‐Weebers et al. 2012) suggesting that looking for support may be a sign of early difficulties in fathers. In these prospective studies, baseline distress levels were controlled. Cross‐sectional designs of mostly mother samples found that social support seeking and perceived social support were associated with lower mixed distress, anxiety and depression throughout the first year post‐diagnosis (Greening & Stoppelbein 2007; Han et al. 2009; Demirtepe‐Saygili & Bozo 2011b; Hoekstra‐Weebers et al. 2012). This is consistent with the observation that increased communication about cancer in the early stages of the illness was associated with lower general distress in mothers (Han et al. 2009), and that early stress about this communication was associated with higher PTSS in both parents (Rodriguez et al. 2012). Cross‐sectional studies reported that emotion‐focused coping, substance use, and negative self‐blame were associated with higher mixed distress, anxiety, depression and PTSS (Greening & Stoppelbein 2007; Demirtepe‐Saygili & Bozo 2011b).
Family factors
Reports suggested that parents’ negative perception of their child's adjustment, as well as the child being a girl was associated with elevations or deterioration of general distress and PTSS in the first year post‐diagnosis (Klassen et al. 2008; Pöder et al. 2008; Barrera et al. 2012; McCarthy et al. 2012; Norberg et al. 2012). The literature reviewed, including two reports controlling for distress at baseline, suggested that important stressful family events prior to the diagnosis (e.g. new job, divorce) as well as the perception that cancer has a greater impact on the family, correlated with higher mixed distress and PTSS over the 5 years post‐diagnosis (Maurice‐Stam et al. 2008b; Klassen et al. 2012; Tremolada et al. 2013). Moreover, poorer family functioning (i.e. lower cohesiveness, expressiveness and support, and more conflict) was cross‐sectionally associated with elevations in general distress and traumatic stress (Maurice‐Stam et al. 2008b; McCarthy et al. 2012). This was also reported in cross‐sectional studies more than 10 years post‐diagnosis, which also included associations with depression and anxiety (Ozono et al. 2007; Han et al. 2009, Ozono et al. 2010; Bruce et al. 2011). One study explored dyadic relations within the parental couple, and found that fathers’ instrumental support related favourably with mothers’ anxiety over the first year post‐diagnosis (Gudmundsdottir et al. 2011).
Mixed results were found concerning the association with the number of children in the family within the first year post‐diagnosis. One study suggested that having more children was associated with lower parental PTSS and lower maternal general distress (Pöder et al. 2008). When considering a longer period of 5 years post‐diagnosis and controlling for baseline distress, this relationship was not significant (Hoekstra‐Weebers et al. 2012). The possible effect of having other children may be moderated by other factors like burden or social support. In fact, cross‐sectional studies also indicated that mental QoL was either associated or mediated by caregiver burden and stress levels at various times of assessment, up to 10 years post‐diagnosis (Witt et al. 2010).
In summary, the recent literature has found some evidence from controls and within‐dyad comparison suggesting that mothers experienced higher distress levels than fathers only at diagnosis and during active treatment. Higher levels of distress in parents in the medium‐long term were associated with a clinical history of more serious conditions and intense treatment. Such levels were also associated with personal characteristics, including negative affectivity and poorer personal resources (e.g. self‐esteem). Finally, emotional or avoidant coping (in mothers and fathers), and support seeking (in fathers) during the early stages also predicted higher distress in the long run. Contrasting with expectations, the literature suggested that having other children is probably not, as such, a vulnerability factor for distress. Notably, education and income did not appear as significant factors either in recent studies.
Consequences of distress
Six studies investigated different consequences of parental distress on the parents themselves. Longitudinal studies suggested that levels of mixed distress and traumatic stress in the early stages predicted future levels from 1 month to 1 year later (Pöder et al. 2008; Hoekstra‐Weebers et al. 2012; McCarthy et al. 2012; Tremolada et al. 2012). Moreover, depression symptoms at 6 months post‐diagnosis predicted lower levels of perceived social support over the first and second year post‐diagnosis (Norberg & Boman 2007), and mixed distress 3 years post‐diagnosis was associated with burnout symptoms a year later in parents of brain tumour survivors (Norberg 2010). Eleven articles indicated consequences of parental distress on their children, either through parent proxy measures or child‐reported measures. With the exception of one study (Maurice‐Stam et al. 2008a), longitudinal reports found that parental mixed distress, anxiety, depression and traumatic stress within the first year post‐diagnosis predicted higher child distress, internalising and externalising symptoms, PTSS, and social competence problems up to 7 years post‐diagnosis (Barrera et al. 2009; Robinson et al. 2009; Pöder et al. 2010; Landolt et al. 2012). Two of four of these reports controlled for baseline outcomes (Robinson et al. 2009; Landolt et al. 2012). One original prospective finding was that maternal depression predicted children's verbal, perceptual and motor skills both 1 and 2 years post‐diagnosis, but not their educational achievements (Barrera et al. 2008). Similar results were found in cross‐sectional studies up to 10 years post‐diagnosis (Colletti et al. 2008; Jobe‐Shields et al. 2009; Davis et al. 2010; Wolfe‐Christensen et al. 2010; Yagc‐Kupeli et al. 2012). These also found an association between parental distress and children's school functioning. Yet, this may also reflect the effect of children's limitations on parental distress.
In summary, the current evidence suggests that early intense negative reactions in parents could predict long‐term psychological suffering in parents themselves, which is coherent with a certain stability of mood. These might also be associated with psychological suffering of children, but the evidence is weaker on this aspect given the cross‐sectional designs used.
Discussion
During the study period 2007–2012, we found 56 studies correlating parental distress with other factors b eing interpreted as precursors or effects of parental distress. Of these, 43 studies were assessed as bearing Low risk of bias. In this literature, distress referred to mixed anxiety–depression symptoms, undifferentiated mental health issues, mental QoL, depression, anxiety or post‐traumatic stress. The most probable factors explaining distress found in this recent literature were severity of the condition and intensity of treatment, being a mother (shortly after diagnosis), negative affectivity and poor personal resources, family stressors or weaknesses before the diagnosis. As for outcomes of parental distress, we found studies to support the effect of acute short‐term distress on long‐term parental adjustment. Studies suggested that parental distress may impact the child's adjustment. This overall pattern is fairly consistent with previous literature reviews in this domain (Klassen et al. 2007; Rabineau et al. (2008); Vrijmoet‐Wiersma et al. 2008).
Compared to the most comprehensive review to date (Vrijmoet‐Wiersma et al. 2008), the current review performed on a more recent period of time highlighted a few differences pertaining to sample composition and scope of factors. Although we found a similar number of studies using both mothers and fathers as participants, we also noted that more studies were equally distributed between sexes (12% in the recent period as compared to 6% in Vrijmoet‐Wiersma et al. 2008). The recent literature was also composed of more homogenous samples in terms of cancer site or trajectory phase. This is pertinent given the growing refinement and standardisation of treatment, which can have unique stressors and late effects (Goldsby et al. 2010, 2011; Whelan et al. 2010). We found that the recent literature studied predictors which had not been related to parental distress in the past, such as treatment intensity and coping reaction (e.g. palliative coping). Moreover, associations which appeared fairly consistent before were not observed here, specifically as for marital status, education and income levels, perhaps reflecting social trends as new social networks and recent changes in care accessibility for the underserved. Further research will be needed to confirm these hypotheses.
Previous reviews did not analyse distress measurement and thus comparisons are difficult to make. In the present pool of studies, we observed that very few studies used measures other than self‐reports (Yalug et al. 2008). We also observed that measures were not as homogeneous across distress domains. High homogeneity characterised depression, PTSS and mental QoL, whereas much lower homogeneity was observed in mixed distress or anxiety. This may be important for future meta‐analyses.
Original findings regarding sex differences and coping were explored. Findings on distress in mothers and fathers were somewhat mixed, but the general tendency indicated that post‐treatment and long‐term levels of distress were similar for mothers and fathers (Ozono et al. 2007, Maurice‐Stam et al. 2008b). In the 20 studies in which both parents were equally represented, mothers seemed particularly vulnerable to distress during the first year post‐diagnosis. Mothers tended to report higher distress both at diagnosis and during active treatment (except for Hoekstra‐Weebers et al. 2012). In fact, the majority of the studies in this review suggested that mothers experienced greater mixed distress than fathers (Ozono et al. 2007; Maurice‐Stam et al. 2008b, Norberg & Boman 2008; Reinfjell et al. 2009; Barrera et al. 2012). Mothers were also more vulnerable to PTSS than fathers (Pöder et al. 2008; Landolt et al. 2012; McCarthy et al. 2012; Rodriguez et al. 2012).
Beside parental sex, important stressful family events prior to the child's diagnosis (e.g. divorce, poor family functioning) appeared as vulnerability factors for parental distress (Ozono et al. 2007; Maurice‐Stam et al. 2008b; Han et al. 2009; Penn et al. 2009; Ozono et al. 2010; Bruce et al. 2011; Gudmundsdottir et al. 2011; Klassen et al. 2012, McCarthy et al. 2012; Tremolada et al. 2013). Tumour relapse was also as a significant predictor for the prevalence of traumatic stress, with traumatic stress nearly doubling following relapse (Jurbergs et al. 2009). This exemplifies a vulnerability factor that is also consistent with the traumatic stress literature, whereby relapse was seen as a ‘second hit’ on the parents and subsequently made them more vulnerable to experiencing clinically significant traumatic distress (Jurbergs et al. 2009). Longitudinal studies identified that the initial reaction to the child's cancer (i.e. mixed distress and traumatic stress) predicted long‐term parental mental health from 4 months to 5 years post‐diagnosis (Pöder et al. 2008; Hoekstra‐Weebers et al. 2012; McCarthy et al. 2012).
In the 6‐year span of this review, the literature on coping was substantial. Researchers agree that adopting an active (problem‐focused) coping style as opposed to a passive/emotional style may be beneficial (for mothers and fathers). Essentially, parents using active coping reported less mixed distress, anxiety and depression in the year following the cancer diagnosis. These observations are consistent with the literature on coping (Zeidner & Endler 1996). Besides having an ‘active/fighting spirit’, other positive coping mechanisms included religious beliefs, optimism, cancer‐related communication, hope regarding the situation (i.e. reframing) and social support. These links found in the recent literature underline the need to articulate coping responses with other moderators from the situation or from social resources. Although the selection of coping strategies can be dependent on the parent's individual characteristics or attributes, it is often quite gender specific. In particular, fathers have been found to use more avoidant/passive and palliative coping (e.g. work, leisure), while mothers use more family and social support coping. This finding corresponds with each parent's traditional role in the cancer experience (Bennett Murphy et al. 2008; Hall 2010). However, it is unclear whether consideration of primary caregiver status would blur this difference. A better understanding of this phenomenon would benefit from a close analysis of both partners’ roles and status in future research. Moreover, a subset of longitudinal follow‐ups did not control for baseline distress weakening the evidence of a causal relationship between correlates and distress (e.g. Norberg et al. 2012).
One comment should be made on the status of predictors or moderators of parental distress. In the recent literature, there has not been any increase in the number of longitudinal designs. In fact, the present review includes a similar proportion of longitudinal studies as the former exhaustive review (i.e. less than a third). The majority of the studies on potential factors and outcomes of parental distress had cross‐sectional designs, notably more than half of them. This as well leads to difficulties in interpreting directionality, dissecting confounding effects of interrelated concepts and inferring causality. For example, in one study, PTSS was associated with cancer‐related communication stress, but this relationship could be bidirectional (Rodriguez et al. 2012). Although it has become almost a tradition at the end of such a review to call for more longitudinal designs, we would like to draw the attention of researchers and practitioners on different status of factors of distress. In our review, it was notable that a large proportion (66%) of studies including both self‐reported factors and distress were cross‐sectional. These were clearly unable to disentangle the effect of factors on parents’ distress. In these cases, longitudinal follow‐up and appropriate analysis including the effect of time would be recommended in the future. It should be made clear yet that some factors, although not qualifying for causal risk factors (Kraemer et al. 1997), are by nature stronger than others as they are clear antecedents of distress, e.g. sex, treatment history or family structure. To generate causal hypotheses involving these factors, cross‐sectional designs may be suitable, as long as the analysis includes appropriate controls (Kazdin 2003).
When considering consequences of distress, we found longitudinal evidence that early intense emotional response could partly explain long‐term distress levels in parents. Although this association makes sense, it is also important to recognise that intense emotional reaction is to be expected, especially if the situation is serious and depending on moderating aspects such as the social support available to parents. However, none of the reports systematically explored interactions between initial responses and these moderators to predict long‐term adjustment. Factors such as restrictions in social networks, pre‐diagnosis psychological distress and adhesion to traditional masculine roles of coping could either predict or moderate the effects of parental distress. Such refined analyses were seldom available in the literature we reviewed (Litzelman et al. 2011; Tremolada et al. 2012).
Finally, the limited body of research exploring for the effects of parental distress on the child suggested deleterious effects on children's mental health as well as cognitive performance. Although the former result is a traditional observation in child psychopathology, the latter deserves further discussion. Cognitive status and school achievement may depend on the condition and on the treatment late effects. The dynamics of degradation have not yet been fully understood as they pertain to a wide range of interconnected factors. Therefore, the association observed in the reviewed studies may be due to common factors including risk status, intensity of treatment, etc., which may explain both increased parental distress and deteriorated cognitive status of the child. Given the lack of appropriate longitudinal studies on this topic, it is not possible to conclude on causal links.
We must finally recognise the limitations of this review. First, this is not a meta‐analysis. Given the heterogeneity of the illness and treatment variables, the array of factors and the rarity of proposed moderators, a quantitative review would not be meaningful. Second, the classification of correlates as factors or consequences of distress may be questioned given the observational design of studies. For classification purposes, we relied on the aims of studies and interpretations given by authors. We then chose to systematically assess biases to identify the strength of the evidence. Our view is that this classification offers an original description of current attempts to study factors and consequences of parental distress as well as it makes it possible to identify avenues for methodological improvements. Third, in reviewing the evidence, we chose to rely exclusively on low risk of bias studies. Although the results of excluded reports may be subjected to higher bias, they may well be informative. To cope with this issue and remain consistent with common standards on systematic reviews, we included a supplementary table (Table S2) summarising characteristics and findings of these studies. Improvements in research quality could easily be made in future studies especially if appropriate sample selection procedures were systematically implemented (Elkin et al. 2007; Bennett Murphy et al. 2008; Roddenberry & Renk 2008; Yalug et al. 2008; Currier et al. 2009; Hall 2010; Liu & Yeh 2010; Demirtepe‐Saygili & Bozo 2011a; Litzelman et al. 2011; Masa'Deh et al. 2012) and reporting was more complete (e.g. response rate, sample description, recruitment procedures, etc.) (Merrill et al. 2007; Bayat et al. 2008; Bennett Murphy et al. 2008; Penn et al. 2009). Finally, this review was performed on quantitative studies correlating parent distress with other factors. It is probable that qualitative studies would bear valuable information on risk factors and effects of distress. Specific methods could be used in the future to articulate qualitative and quantitative findings in the future (Sandelowski et al. 2007).
Despite these limitations, the present review underlines the need for more research in the field. For instance, it is still not clear why mothers typically report greater distress than fathers near diagnosis, and why this difference is not significant later in the cancer trajectory. Perhaps, fathers are experiencing just as much distress as mothers near the time of diagnosis but they are masking their concerns and relying on avoidant coping instead of openly expressing their distress. Alternatively, it is also plausible that mothers have heightened reactivity to stress in general as compared to their partners. Future studies could address this by implementing a more routine use of clinical and non‐clinical comparison groups and exploring appropriate underlying concepts when examining sex differences. It would also be beneficial if future research provided greater specifications on core elements, which contribute to parental distress (e.g. ask parents to rate a list of potential sources of distress in terms of most to least important factor contributing to their current distress). This avenue could benefit from a large body of qualitative research involving parents. It will require methodological refinements to accurately identify causal relationships. As the idea of ‘factor’ or ‘consequence’ of distress implies causality, future research should favour research designs able to bring stronger evidence, including prospective group follow‐ups, multiple single‐case designs and quasi‐experimental studies (Kazdin 2003). Moreover, a focus of researchers on modifiable factors of distress should help identify targets for future intervention (Kraemer et al. 1997). A good example of a modifiable factor is social support. Discrepancies between parents’ desired support (e.g. social support, instrumental support, informational support) and their actual or perceived support could be partially responsible for their distress levels, because this would constitute an additional source of stress. Future research could empirically examine both of these types of supports among parents. This is very relevant as promising self‐help parent‐directed interventions have been developed recently (Cernvall et al. 2015). Finally, the research on consequences of parental distress on the family and the child should be expanded. Although it is desirable to evaluate and help the parents who need it, the systematic screening of parental distress is still not common practice (Barrera et al. 2014). Weighing precisely the burden of cancer‐related distress for the family will be essential to advance our standards of care.
As a conclusion, we systematically updated a previous literature review (Vrijmoet‐Wiersma et al. 2008) while focusing on factors and effects of parental distress following child cancer. This review was based on an operational definition of distress and included a systematic assessment of biases. We identified the main probable factors in the illness and trajectory, individual and family domains. A lot of the results confirmed previous syntheses. We also found original results pertaining to differences between mothers and fathers and socio‐demographic factors. Interestingly, the research on psychosocial factors of parental distress in the recent literature was fairly consistent when compared with the older literature. The recent literature suggested that parental distress may predict further deterioration of adjustment in parents and may have a negative impact on the child. Quality assessment of reviewed studies revealed that widespread biases could easily be dealt with during the research process (e.g. selection and reporting biases). Despite methodological limitations of the literature, the recent literature confirms the need for distress assessment in parents. Following the increasing survival rates in childhood cancer and specific survivorship issues, more research is needed on long‐term parental distress as well as long‐term effects of heightened distress in parents.
Supporting information
Table S1. Assessment of risk of bias in 56 studies on factors and outcomes of parental distress 2007–2012.
Table S2. Summary of 13 excluded articles on parental distress by category from January 2007 to December 2012.
Acknowledgements
This study was supported by the Foundation CHU Sainte‐Justine, the Rossy Family Foundation, and Industrielle Alliance Inc. The authors are grateful to Sarah Bérubé for helping in the data extraction procedure.
Sultan S., Leclair T., Rondeau É., Burns W. & Abate C. (2016) European Journal of Cancer Care 25, 616–637 A systematic review on factors and consequences of parental distress as related to childhood cancer
References
- Accreditation Canada . 2013. Cancer Care and Oncology Services [Online]. Available at: http://www.accreditation.ca/accreditation-programs/qmentum/standards/cancer-care/ (accessed April 27, 2013).
- Barrera M., Atenafu E., Andrews G.S. & Saunders F. (2008) Factors related to changes in cognitive, educational and visual motor integration in children who undergo hematopoietic stem cell transplant. Journal of Pediatric Psychology 33, 536–546. [DOI] [PubMed] [Google Scholar]
- Barrera M., Atenafu E. & Pinto J. (2009) Behavioral, social, and educational outcomes after pediatric stem cell transplantation and related factors. Cancer 115, 880–889. [DOI] [PubMed] [Google Scholar]
- Barrera M., Atenafu E., Doyle J., Berlin‐Romalis D. & Hancock K. (2012) Differences in mothers’ and fathers’ health‐related quality of life after pediatric SCT: a longitudinal study. Bone Marrow Transplantation 47, 855–859. [DOI] [PubMed] [Google Scholar]
- Barrera M., Hancock K., Rokeach A., Cataudella D., Atenafu E., Johnston D., Punnett A., Nathan P.C., Bartels U., Silva M., Cassidy M., Jansen P., Shama W. & Greenberg C. (2014) External validity and reliability of the psychosocial assessment tool (PAT) among Canadian parents of children newly diagnosed with cancer. Pediatric Blood and Cancer 61, 165–170. [DOI] [PubMed] [Google Scholar]
- Bayat M., Erdem E. & Gül Kuzucu E. (2008) Depression, anxiety, hopelessness, and social support levels of the parents of children with cancer. Journal of Pediatric Oncology Nursing 25, 247–253. [DOI] [PubMed] [Google Scholar]
- Bennett Murphy L.M., Flowers S., McNamara K.A. & Young‐Saleme T. (2008) Fathers of children with cancer: involvement, coping, and adjustment. Journal of Pediatric Health Care 22, 182–189. [DOI] [PubMed] [Google Scholar]
- Brown R.T., Madan‐Swain A. & Lambert R. (2003) Posttraumatic stress symptoms in adolescent survivors of childhood cancer and their mothers. Journal of Traumatic Stress 16, 309–318. [DOI] [PubMed] [Google Scholar]
- Bruce M., Gumley D., Isham L., Fearon P. & Phipps K. (2011) Post‐traumatic stress symptoms in childhood brain tumour survivors and their parents. Child: Care Health and Development 37, 244–251. [DOI] [PubMed] [Google Scholar]
- Cernvall M., Carlbring P., Ljungman L., Ljungman G. & von Essen L. (2015) Internet‐based guided self‐help for parents of children on cancer treatment: a randomized controlled trial. Psycho‐Oncology doi: 10.1002/pon.3788. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Colletti C.J., Wolfe‐Christensen C., Carpentier M.Y., Page M.C., McNall‐Knapp R.Y., Meyer W.H., Chaney J.M. & Mullins L.L. (2008) The relationship of parental overprotection, perceived vulnerability, and parenting stress to behavioral, emotional, and social adjustment in children with cancer. Pediatric Blood and Cancer 51, 269–274. [DOI] [PubMed] [Google Scholar]
- Currier J.M., Jobe‐Shields L.E. & Phipps S. (2009) Stressful life events and posttraumatic stress symptoms in children with cancer. Journal of Traumatic Stress 22, 28–35. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Dashiff C., Morrison S. & Rowe J. (2008) Fathers of children and adolescents with diabetes: what do we know? Journal of Pediatric Nursing 23, 101–119. [DOI] [PubMed] [Google Scholar]
- Davis G.L., Parra G.R. & Phipps S. (2010) Parental posttraumatic stress symptoms due to childhood cancer and child outcomes: investigation of the role of child anger regulation. Children's Health Care 39, 173–184. [Google Scholar]
- Demirtepe‐Saygili D. & Bozo O. (2011a) Correlates of depressive and anxiety symptoms among the caregivers of leukemic children. Journal of Clinical Psychology in Medical Settings 18, 46–54. [DOI] [PubMed] [Google Scholar]
- Demirtepe‐Saygili D. & Bozo O. (2011b) Predicting depressive symptoms among the mothers of children with leukaemia: a caregiver stress model perspective. Psychology and Health 26, 585–599. [DOI] [PubMed] [Google Scholar]
- Diseth T.H., Tangeraas T., Reinfjell T. & Bjerre A. (2011) Kidney transplantation in childhood: mental health and quality of life of children and caregivers. Pediatric Nephrology (Berlin, Germany) 26, 1881–1892. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Dolgin M.J., Phipps S., Fairclough D.L., Sahler O.J., Askins M., Noll R.B., Butler R.W., Varni J.W. & Katz E.R. (2007) Trajectories of adjustment in mothers of children with newly diagnosed cancer: a natural history investigation. Journal of Pediatric Psychology 32, 771–782. [DOI] [PubMed] [Google Scholar]
- Dunn M.J., Rodriguez E.M., Barnwell A.S., Grossenbacher J.C., Vannatta K., Gerhardt C.A. & Compas B.E. (2012) Posttraumatic stress symptoms in parents of children with cancer within six months of diagnosis. Health Psychology 31, 176–185. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Elkin T.D., Jensen S.A., McNeil L., Gilbert M.E., Pullen J. & McComb L. (2007) Religiosity and coping in mothers of children diagnosed with cancer: an exploratory analysis. Journal of Pediatric Oncology Nursing 24, 274–278. [DOI] [PubMed] [Google Scholar]
- Fotiadou M., Barlow J.H., Powell L.A. & Langton H. (2008) Optimism and psychological well‐being among parents of children with cancer: an exploratory study. Psycho‐Oncology 17, 401–409. [DOI] [PubMed] [Google Scholar]
- Gerhardt C.A., Gutzwiller J., Huiet K.A., Fischer S., Noll R.B. & Vannatta K. (2007) Parental adjustment to childhood cancer: a replication study. Families, Systems, and Health 25, 263–275. [Google Scholar]
- Goldsby R.E., Liu Q., Nathan P.C., Bowers D.C., Yeaton‐Massey A., Raber S.H., Hill D., Armstrong G.T., Yasui Y., Zeltzer L., Robison L.L. & Packer R.J. (2010) Late‐occurring neurologic sequelae in adult survivors of childhood acute lymphoblastic leukemia: a report from the Childhood Cancer Survivor Study. Journal of Clinical Oncology 28, 324–331. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Goldsby R., Chen Y., Raber S., Li L., Diefenbach K., Shnorhavorian M., Kadan‐Lottick N., Kastrinos F., Yasui Y., Stovall M., Oeffinger K., Sklar C., Armstrong G.T., Robison L.L. & Diller L. 2011. Survivors of childhood cancer have increased risk of gastrointestinal complications later in life. Gastroenterology, 140, 1464–1471 e1. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Greening L. & Stoppelbein L. (2007) Brief report: pediatric cancer, parental coping style, and risk for depressive, posttraumatic stress, and anxiety symptoms. Journal of Pediatric Psychology 32, 1272–1277. [DOI] [PubMed] [Google Scholar]
- Gudmundsdottir E., Schirren M. & Boman K.K. (2011) Psychological resilience and long‐term distress in Swedish and Icelandic parents’ adjustment to childhood cancer. Acta Oncologica 50, 373–380. [DOI] [PubMed] [Google Scholar]
- Hall J.A. (2010) An exploratory study of communication, gender‐role conflict, and social support of parents of children treated at children's hospital. Journal of Psychosocial Oncology 28, 511–525. [DOI] [PubMed] [Google Scholar]
- Hammen C., Hazel N.A., Brennan P.A. & Najman J. (2012) Intergenerational transmission and continuity of stress and depression: depressed women and their offspring in 20 years of follow‐up. Psychological Medicine 42, 931–942. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Han H.R., Cho E.J., Kim D. & Kim J. (2009) The report of coping strategies and psychosocial adjustment in Korean mothers of children with cancer. Psycho‐Oncology 18, 956–964. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Hardy K.K., Bonner M.J., Masi R., Hutchinson K.C., Willard V.W. & Rosoff P.M. (2008) Psychosocial functioning in parents of adult survivors of childhood cancer. Journal of Pediatric Hematology/oncology 30, 153–159. [DOI] [PubMed] [Google Scholar]
- Higgins J.P.T. & Green S.; The Cochrane Collaboration , 2011. Cochrane Handbook for Systematic Reviews of Interventions, Version 5.1.0 [updated March 2011] [Online]. Available at: www.cochrane-handbook.org (accessed 14 October 2013).
- Hoekstra‐Weebers J.E., Wijnberg‐Williams B.J., Jaspers J.P., Kamps W.A. & Wiel H.B. (2012) Coping and its effect on psychological distress of parents of pediatric cancer patients: a longitudinal prospective study. Psycho‐Oncology 21, 903–911. [DOI] [PubMed] [Google Scholar]
- Holland J.C. & Bultz B.D. (2007) The NCCN guideline for distress management: a case for making distress the sixth vital sign. Journal of the National Comprehensive Cancer Network 5, 3–7. [PubMed] [Google Scholar]
- Hoven E., Anclair M., Samuelsson U., Kogner P. & Boman K.K. (2008) The influence of pediatric cancer diagnosis and illness complication factors on parental distress. Journal of Pediatric Hematology/Oncology 30, 807–814. [DOI] [PubMed] [Google Scholar]
- Hutchinson K.C., Willard V.W., Hardy K.K. & Bonner M.J. (2009) Adjustment of caregivers of pediatric patients with brain tumors: a cross‐sectional analysis. Psycho‐Oncology 18, 515–523. [DOI] [PubMed] [Google Scholar]
- Iobst E.A., Alderfer M.A., Sahler O.J., Askins M.A., Fairclough D.L., Katz E.R., Butler R.W., Dolgin M.J. & Noll R.B. (2009) Problem solving and maternal distress at the time of a child's diagnosis of cancer in two‐parent versus lone‐parent households. Journal of Pediatric Psychology 34, 817–821. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Jobe‐Shields L., Alderfer M.A., Barrera M., Vannatta K., Currier J.M. & Phipps S. (2009) Parental depression and family environment predict distress in children before stem cell transplantation. Journal of Developmental and Behavioral Pediatrics 30, 140–146. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Jurbergs N., Long A., Ticona L. & Phipps S. (2009) Symptoms of posttraumatic stress in parents of children with cancer: are they elevated relative to parents of healthy children? Journal of Pediatric Psychology 34, 4–13. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Kazak A.E. & Baxt C. (2007) Families of infants and young children with cancer: a post‐traumatic stress framework. Pediatric Blood and Cancer 49, 1109–1113. [DOI] [PubMed] [Google Scholar]
- Kazdin A.E. 2003. Research Design in Clinical Psychology. Allyn and Bacon, Boston, MA, USA. [Google Scholar]
- Klassen A., Raina P., Reineking S., Dix D., Pritchard S. & O'Donnell M. (2007) Developing a literature base to understand the caregiving experience of parents of children with cancer: a systematic review of factors related to parental health and well‐being. Supportive Care in Cancer 15, 807–818. [DOI] [PubMed] [Google Scholar]
- Klassen A.F., Klaassen R., Dix D., Pritchard S., Yanofsky R., O'Donnell M., Scott A. & Sung L. (2008) Impact of caring for a child with cancer on parents’ health‐related quality of life. Journal of Clinical Oncology 26, 5884–5889. [DOI] [PubMed] [Google Scholar]
- Klassen A.F., Raina P., McIntosh C., Sung L., Klaassen R.J., O'Donnell M., Yanofsky R. & Dix D. (2011) Parents of children with cancer: which factors explain differences in health‐related quality of life. International Journal of Cancer 129, 1190–1198. [DOI] [PubMed] [Google Scholar]
- Klassen A.F., Dix D., Papsdorf M., Klaassen R.J., Yanofsky R. & Sung L. (2012) Impact of caring for a child with cancer on single parents compared with parents from two‐parent families. Pediatric Blood and Cancer 58, 74–79. [DOI] [PubMed] [Google Scholar]
- Kraemer H.C., Kazdin A.E., Offord D.R., Kessler R.C., Jensen P.S. & Kupfer D.J. (1997) Coming to terms with the terms of risk. Archives of General Psychiatry 54, 337–343. [DOI] [PubMed] [Google Scholar]
- Landolt M.A., Ystrom E., Sennhauser F.H., Gnehm H.E. & Vollrath M.E. (2012) The mutual prospective influence of child and parental post‐traumatic stress symptoms in pediatric patients. Journal of Child Psychology and Psychiatry 53, 767–774. [DOI] [PubMed] [Google Scholar]
- Litzelman K., Catrine K., Gangnon R. & Witt W.P. (2011) Quality of life among parents of children with cancer or brain tumors: the impact of child characteristics and parental psychosocial factors. Quality of Life Research 20, 1261–1269. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Liu Y.‐M. & Yeh C.H. (2010) Pediatric oncology: the use of cluster analysis to examine maternal concerns. Oncology Nursing Forum 37, E304–E311. [DOI] [PubMed] [Google Scholar]
- Ljungman L., Cernvall M., Gronqvist H., Ljotsson B., Ljungman G. & von Essen L. 2014. Long‐term positive and negative psychological late effects for parents of childhood cancer survivors: a systematic review. PLoS ONE 9, e103340. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Masa'Deh R., Collier J. & Hall C. (2012) Parental stress when caring for a child with cancer in Jordan: a cross‐sectional survey. Health and Quality of Life Outcomes 10, 88. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Maurice‐Stam H., Oort F.J., Last B.F., Brons P.P., Caron H.N. & Grootenhuis M.A. (2008a) Longitudinal assessment of health‐related quality of life in preschool children with non‐CNS cancer after the end of successful treatment. Pediatric Blood and Cancer 50, 1047–1051. [DOI] [PubMed] [Google Scholar]
- Maurice‐Stam H., Oort F.J., Last B.F. & Grootenhuis M.A. (2008b) Emotional functioning of parents of children with cancer: the first five years of continuous remission after the end of treatment. Psycho‐Oncology 17, 448–459. [DOI] [PubMed] [Google Scholar]
- McCarthy M.C., Ashley D.M., Lee K.J. & Anderson V.A. (2012) Predictors of acute and posttraumatic stress symptoms in parents following their child's cancer diagnosis. Journal of Traumatic Stress 25, 558–566. [DOI] [PubMed] [Google Scholar]
- Merrill R.M., Brown R.J., Alder S., Baker R.K., Byrd A.D., White G.L. Jr & Lyon J.L. (2007) Psychological disorders among children and the parents of children undergoing cancer workup. Journal of Psychosocial Oncology 25, 1–18. [DOI] [PubMed] [Google Scholar]
- Meyler E., Guerin S., Kiernan G. & Breatnach F. (2010) Review of family‐based psychosocial interventions for childhood cancer. Journal of Pediatric Psychology 35, 1116–1132. [DOI] [PubMed] [Google Scholar]
- Miller V.A., Luce M.F. & Nelson R.M. (2011) Relationship of external influence to parental distress in decision making regarding children with a life‐threatening illness. Journal of Pediatric Psychology 36, 1102–1112. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Moher D., Liberati A., Tetzlaff J., & Altman D.G. Group T.P. (2009). Preferred reporting items for systematic reviews and meta‐analyses: the PRISMA statement. PLoS Medicine, 151, 264–269. [PMC free article] [PubMed] [Google Scholar]
- National Comprehensive Cancer Network . 2013. Clinical Practice Guidelines in Oncology (NCCN Guidelines) Distress Management V.2.2013 [Online]. Available at: http://www.nccn.org/professionals/physician_gls/pdf/distress.pdf (accessed 11 April 2013).
- Norberg A.L. (2010) Parents of children surviving a brain tumor: burnout and the perceived disease‐related influence on everyday life. Journal of Pediatric Hematology/Oncology 32, e285–e289. [DOI] [PubMed] [Google Scholar]
- Norberg A.L. & Boman K.K. (2007) Parents’ perceptions of support when a child has cancer: a longitudinal perspective. Cancer Nursing 30, 294–301. [DOI] [PubMed] [Google Scholar]
- Norberg A.L. & Boman K.K. (2008) Parent distress in childhood cancer: a comparative evaluation of posttraumatic stress symptoms, depression and anxiety. Acta Oncologica 47, 267–274. [DOI] [PubMed] [Google Scholar]
- Norberg A.L., Pöder U. & von Essen L. (2011) Early avoidance of disease‐and treatment‐related distress predicts post‐traumatic stress in parents of children with cancer. European Journal of Oncology Nursing 15, 80–84. [DOI] [PubMed] [Google Scholar]
- Norberg A.L., Poder U., Ljungman G. & von Essen L. (2012) Objective and subjective factors as predictors of post‐traumatic stress symptoms in parents of children with cancer – a longitudinal study. PLoS ONE 7, e36218. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Ozono S., Saeki T., Mantani T., Ogata A., Okamura H. & Yamawaki S. (2007) Factors related to posttraumatic stress in adolescent survivors of childhood cancer and their parents. Supportive Care in Cancer 15, 309–317. [DOI] [PubMed] [Google Scholar]
- Ozono S., Saeki T., Mantani T., Ogata A., Okamura H., Nakagawa S., Ueda K., Inada H. & Yamawaki S. (2010) Psychological distress related to patterns of family functioning among Japanese childhood cancer survivors and their parents. Psycho‐Oncology 19, 545–552. [DOI] [PubMed] [Google Scholar]
- Pai A.L., Drotar D., Zebracki K., Moore M. & Youngstrom E. (2006) A meta‐analysis of the effects of psychological interventions in pediatric oncology on outcomes of psychological distress and adjustment. Journal of Pediatric Psychology 31, 978–988. [DOI] [PubMed] [Google Scholar]
- Patiño‐Fernández A.M., Pai A.L., Alderfer M., Hwang W.T., Reilly A. & Kazak A.E. (2008) Acute stress in parents of children newly diagnosed with cancer. Pediatric Blood and Cancer 50, 289–292. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Penn A., Lowis S.P., Stevens M.C., Hunt L.P., Shortman R.I., McCarter R.J., Pauldhas D., Curran A.L. & Sharples P.M. (2009) Family, demographic and illness‐related determinants of HRQL in children with brain tumours in the first year after diagnosis. Pediatric Blood and Cancer 53, 1092–1099. [DOI] [PubMed] [Google Scholar]
- Pöder U., Ljungman G. & von Essen L. (2008) Posttraumatic stress disorder among parents of children on cancer treatment: a longitudinal study. Psycho‐Oncology 17, 430–437. [DOI] [PubMed] [Google Scholar]
- Pöder U., Ljungman G. & von Essen L. (2010) Parents’ perceptions of their children's cancer‐related symptoms during treatment: a prospective, longitudinal study. Journal of Pain and Symptom Management 40, 661–670. [DOI] [PubMed] [Google Scholar]
- Pui C.H., Robison L.L. & Look A.T. (2008) Acute lymphoblastic leukaemia. Lancet 371, 1030–1043. [DOI] [PubMed] [Google Scholar]
- Rabineau K.M., Mabe P.A. & Vega R.A. (2008) Parenting stress in pediatric oncology populations. Journal of Pediatric Hematology/Oncology 30, 358–365. [DOI] [PubMed] [Google Scholar]
- Reinfjell T., Lofstad G.E., Nordahl H.M., Vikan A. & Diseth T.H. (2009) Children in remission from acute lymphoblastic leukaemia: mental health, psychosocial adjustment and parental functioning. European Journal of Cancer 18, 364–370. [DOI] [PubMed] [Google Scholar]
- Robinson K.E., Gerhardt C.A., Vannatta K. & Noll R.B. (2009) Survivors of childhood cancer and comparison peers: the influence of early family factors on distress in emerging adulthood. Journal of Family Psychology 23, 23–31. [DOI] [PubMed] [Google Scholar]
- Roddenberry A. & Renk K. (2008) Quality of life in pediatric cancer patients: the relationships among parents’ characteristics, children's charac‐teristics, and informant concordance. Journal of Child and Family Studies 17, 402–426. [Google Scholar]
- Rodriguez E.M., Dunn M.J., Zuckerman T., Vannatta K., Gerhardt C.A. & Compas B.E. (2012) Cancer‐related sources of stress for children with cancer and their parents. Journal of Pediatric Psychology 37, 185–197. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Sandelowski M., Barroso J. & Voils C.I. (2007) Using qualitative metasummary to synthesize qualitative and quantitative descriptive findings. Research in Nursing and Health 30, 99–111. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Shea B.J., Grimshaw J.M., Wells G.A., Boers M., Andersson N., Hamel C., Porter A.C., Tugwell P., Moher D. & Bouter L.M. (2007) Development of AMSTAR: a measurement tool to assess the methodological quality of systematic reviews. BMC Medical Research Methodology 7, 10. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Tremolada M., Bonichini S., Aloisio D., Schiavo S., Carli M. & Pillon M. (2013) Post‐traumatic stress symptoms among mothers of children with leukemia undergoing treatment: a longitudinal study. Psycho‐Oncology 22, 1266–1272. [DOI] [PubMed] [Google Scholar]
- Tremolada M., Bonichini S., Schiavo S. & Pillon M. (2012) Post‐traumatic stress symptoms in mothers of children with leukaemia undergoing the first 12 months of therapy: predictive models. Psychology and Health 27, 1448–1462. [DOI] [PubMed] [Google Scholar]
- Vrijmoet‐Wiersma C.M., van Klink J.M., Kolk A.M., Koopman H.M., Ball L.M. & Maarten Egeler R. (2008) Assessment of parental psychological stress in pediatric cancer: a review. Journal of Pediatric Psychology 33, 694–706. [DOI] [PubMed] [Google Scholar]
- Whelan K.F., Stratton K., Kawashima T., Waterbor J.W., Castleberry R.P., Stovall M., Sklar C.A., Packer R.J., Mitby P., Aitken C.L., Blatt J., Robison L.L. & Mertens A.C. (2010) Ocular late effects in childhood and adolescent cancer survivors: a report from the childhood cancer survivor study. Pediatric Blood and Cancer 54, 103–109. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Wijnberg‐Williams B.J., Kamps W.A., Klip E.C. & Hoekstra‐Weebers J.E. (2006) Psychological adjustment of parents of pediatric cancer patients revisited: five years later. Psycho‐Oncology 15, 1–8. [DOI] [PubMed] [Google Scholar]
- Witt W.P., Litzelman K., Wisk L.E., Spear H.A., Catrine K., Levin N. & Gottlieb C.A. (2010) Stress‐mediated quality of life outcomes in parents of childhood cancer and brain tumor survivors: a case‐control study. Quality of Life Research 19, 995–1005. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Wolfe‐Christensen C., Mullins L.L., Fedele D.A., Rambo P.L., Eddington A. & Carpentier M.Y. (2010) The relation of caregiver demand to adjustment outcomes in children with cancer: the moderating role of parenting stress. Children's Health Care 39, 108–124. [Google Scholar]
- Yagc‐Kupeli B., Akyuz C., Kupeli S. & Buyukpamukcu M. (2012) Health‐related quality of life in pediatric cancer survivors: a multifactorial assessment including parental factors. Journal of Pediatric Hematology/Oncology 34, 194–199. [DOI] [PubMed] [Google Scholar]
- Yalug I., Corapcioglu F., Fayda M., Aksu G., Basar E., Yalug K. & Aker T. (2008) Posttraumatic stress disorder and risk factors in parents of children with a cancer diagnosis. Pediatric Hematology and Oncology 25, 27–38. [DOI] [PubMed] [Google Scholar]
- Zeidner M. & Endler N.S. 1996. Handbook of Coping: Theory, Research, Applications. Wiley, J.Wiley, New York; Toronto. [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Supplementary Materials
Table S1. Assessment of risk of bias in 56 studies on factors and outcomes of parental distress 2007–2012.
Table S2. Summary of 13 excluded articles on parental distress by category from January 2007 to December 2012.


