Abstract
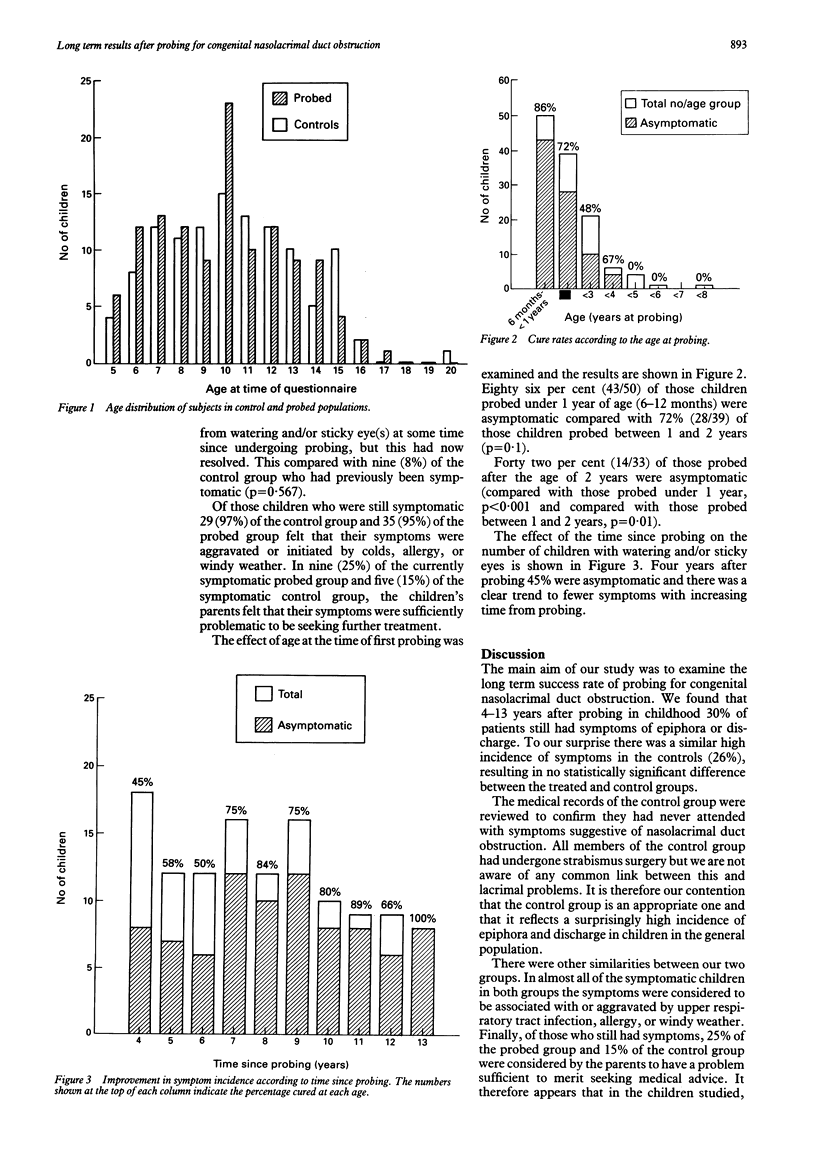
The long term results of probing for congenital nasolacrimal duct obstruction were reviewed using a parental questionnaire issued to both treated and age-matched control groups. On follow up 4-13 years after probing in childhood 30% of patients still had symptoms of epiphora or discharge. Surprisingly, a similar high symptom rate was found in the controls, such that there was no statistically significant difference in the rate of symptoms between the two groups. Probing had therefore apparently reduced the symptom rate to a level close to normal for the age group concerned. All studies on the incidence of congenital nasolacrimal duct obstruction must be interpreted with reference to the known high rate of spontaneous resolution as a clear trend has been demonstrated towards a lower incidence of symptoms the longer the follow up after probing. This finding would support a policy of delay before further intervention in patients with mild residual symptoms after a technically successful probing.
Full text
PDF

Selected References
These references are in PubMed. This may not be the complete list of references from this article.
- BROGGI R. J. The treatment of congenital dacryostenosis. AMA Arch Ophthalmol. 1959 Jan;61(1):30–36. doi: 10.1001/archopht.1959.00940090032004. [DOI] [PubMed] [Google Scholar]
- Baker J. D. Treatment of congenital nasolacrimal system obstruction. J Pediatr Ophthalmol Strabismus. 1985 Jan-Feb;22(1):34–36. doi: 10.3928/0191-3913-19850101-12. [DOI] [PubMed] [Google Scholar]
- CASSADY J. V. Developmental anatomy of nasolacrimal duct. AMA Arch Ophthalmol. 1952 Feb;47(2):141–158. doi: 10.1001/archopht.1952.01700030146003. [DOI] [PubMed] [Google Scholar]
- Ffooks O. O. DACRYOCYSTITIS IN INFANCY. Br J Ophthalmol. 1962 Jul;46(7):422–434. doi: 10.1136/bjo.46.7.422. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Katowitz J. A., Welsh M. G. Timing of initial probing and irrigation in congenital nasolacrimal duct obstruction. Ophthalmology. 1987 Jun;94(6):698–705. doi: 10.1016/s0161-6420(87)33392-5. [DOI] [PubMed] [Google Scholar]
- MacEwen C. J., Young J. D. Epiphora during the first year of life. Eye (Lond) 1991;5(Pt 5):596–600. doi: 10.1038/eye.1991.103. [DOI] [PubMed] [Google Scholar]
- Nucci P., Capoferri C., Alfarano R., Brancato R. Conservative management of congenital nasolacrimal duct obstruction. J Pediatr Ophthalmol Strabismus. 1989 Jan-Feb;26(1):39–43. doi: 10.3928/0191-3913-19890101-10. [DOI] [PubMed] [Google Scholar]
- Paul T. O. Medical management of congenital nasolacrimal duct obstruction. J Pediatr Ophthalmol Strabismus. 1985 Mar-Apr;22(2):68–70. doi: 10.3928/0191-3913-19850301-09. [DOI] [PubMed] [Google Scholar]
- Petersen R. A., Robb R. M. The natural course of congenital obstruction of the nasolacrimal duct. J Pediatr Ophthalmol Strabismus. 1978 Jul-Aug;15(4):246–250. doi: 10.3928/0191-3913-19780701-14. [DOI] [PubMed] [Google Scholar]
- Wobig J. L. Lacrimal probing complications. Ophthal Plast Reconstr Surg. 1985;1(1):75–76. doi: 10.1097/00002341-198501000-00013. [DOI] [PubMed] [Google Scholar]
- el-Mansoury J., Calhoun J. H., Nelson L. B., Harley R. D. Results of late probing for congenital nasolacrimal duct obstruction. Ophthalmology. 1986 Aug;93(8):1052–1054. doi: 10.1016/s0161-6420(86)33621-2. [DOI] [PubMed] [Google Scholar]



