This research study describes the level of interoperability of local health department information systems and identifies factors associated with lack of interoperability.
Keywords: business process analysis, informatics, information systems, information technology, interoperability, IT infrastructure, local health departments, local public health agencies
Background:
In the post-Affordable Care Act era marked by interorganizational collaborations and availability of large amounts of electronic data from other community partners, it is imperative to assess the interoperability of information systems used by the local health departments (LHDs).
Objectives:
To describe the level of interoperability of LHD information systems and identify factors associated with lack of interoperability.
Data and Methods:
This mixed-methods research uses data from the 2015 Informatics Capacity and Needs Assessment Survey, with a target population of all LHDs in the United States. A representative sample of 650 LHDs was drawn using a stratified random sampling design. A total of 324 completed responses were received (50% response rate). Qualitative data were used from a key informant interview study of LHD informatics staff from across the United States. Qualitative data were independently coded by 2 researchers and analyzed thematically. Survey data were cleaned, bivariate comparisons were conducted, and a multivariable logistic regression was run to characterize factors associated with interoperability.
Results:
For 30% of LHDs, no systems were interoperable, and 38% of LHD respondents indicated some of the systems were interoperable. Significant determinants of interoperability included LHDs having leadership support (adjusted odds ratio [AOR] = 3.54), control of information technology budget allocation (AOR = 2.48), control of data systems (AOR = 2.31), having a strategic plan for information systems (AOR = 1.92), and existence of business process analysis and redesign (AOR = 1.49).
Conclusion:
Interoperability of all systems may be an informatics goal, but only a small proportion of LHDs reported having interoperable systems, pointing to a substantial need among LHDs nationwide.
Local health departments (LHDs) are presented with an unprecedented opportunity to use real-time, standardized data to inform public health practice in a post–Affordable Care Act era marked by interorganizational collaborations and availability of large amounts of electronic health care data through health information exchanges.1–4 In a dynamic public health environment filled with emerging demands for evidence-based public health practice, it is ever more imperative for LHDs to harness these data and integrate them into their decision support systems in order to efficiently meet public health practice needs.5 Some of these public health needs dictating integration and exchange of data include information needs for emergency management,6 disease reporting, early detection of outbreaks,7,8 surveillance,9,10 assessment of community health status, needs and resources for evidence-based decision making,11 and enabling assessment of health disparities,12 to name a few.
Research shows that some LHD staff members already perceive an increased responsibility for collecting, analyzing, and reporting data to community partners and, in turn, growing greater epidemiologic and surveillance capacity.13 However, efficient data management and use may be hindered by the reality that LHDs' data needs vary considerably, as does their infrastructure. The complexity of data needs and availability present difficulty in using and managing data, particularly because much of these data are stored in noncomparable formats and cannot be easily combined with other data systems without additional work.14 Smaller LHDs are less likely to be informatics savvy due to lack of financial and human capital, so managing information systems and using information technology (IT) tools are bigger challenges for them.15–18
LHDs cannot take advantage of the opportunities to utilize large amounts of data from all sectors of society if their information systems are unable to interact with external, often more sophisticated, data systems. This issue is often referred to as lack of interoperability. Interoperability is the capacity of IT systems for bidirectional communication and exchange of information allowing the multiple agencies to use the exchanged information and communicate or work together.19,20 Interoperability between systems may improve communication, efficiency, and accuracy of information transmission, eventually leading to improvements in health outcomes and cost-effectiveness for patients and providers.20
Interoperability of health IT is generally classified into 3 levels—foundational, structural, and semantic.21 Foundational interoperability refers to the lowest and most basic level of interoperability, in which an IT system is required to allow the data transmitted by other health IT systems to be received, with no requirement of data interpretation for the system on the receiving end of the transmission.21 Structural interoperability encompasses use of defined formats and syntax of data exchange [eg, Health Level 7 (HL7)], thus the focus being on the packaging of the data via message format standards to ensure that clinical meanings of data are preserved. Semantic interoperability is the highest level of interoperability that involves exchange, codification, and interpretation of data, which further produces useful results as defined by the end users of information exchange systems.21
Incentivized by the HITECH Act, “Meaningful Use,” and related developments, health care industry and other community partners now generate massive amounts of data across various settings.4,22,23 The ability to electronically exchange health information has been a central goal of the ongoing digitization of the health care sector, resulting in many benefits.24,25 Use of big data and information science and technology can allow care coordination for LHDs providing clinical services.26,27 Data-driven assessments can help with detection of health inequities28 and reinforce efforts to promote Health in All Policies.23 Interoperable data available from community partners can be useful to many public health programs, for example, environmental health monitoring and protection,29,30 reportable disease surveillance and control,31–33 communicable disease prevention interventions,31 food and waterborne outbreaks detection,7,34,35 emergency response and program evaluation,30 and community health promotion.36 In addition, adequate informatics capacity and its efficient use can support quality improvement, research, reporting, culture of health, and efficient provision of public health services.37–39
Despite progress toward nationwide health information exchange, health departments are not fully engaged.39 It is vital to assess the level of interoperability of LHD information systems and factors associated with them in order to support advocacy and capacity-building efforts targeting public health agencies. There is a dearth of research assessing the interoperability levels of information systems managed and used by LHDs. This study aims to fill the evidence gap by investigating the extent to which LHDs' information systems are interoperable and factors associated with interoperability. Findings from this study show many modifiable aspects of LHD infrastructure that significantly condition LHDs' ability to improve their information systems, providing clear policy recommendations.
Data and Methods
This research is based on an exploratory mixed-methods design. The study first employed a qualitative key informant interview phase, followed by a national survey where the instrument was informed by the first phase. Results are analyzed and presented in an integrated fashion.
Interview phase
Key informant interviews were conducted with 50 LHD staff members in 2014 across the United States. Potential interviewees were selected on the basis of their LHD's geography, size of the population it served, and how sophisticated their LHD's information systems were, based on responses to the 2013 NACCHO Profile.40 These interviews were recorded by telephone, transcribed, verified, and independently coded by 2 researchers. One interview had a technical error, resulting in 49 interviews used in coding and analysis. A codebook was developed on the basis of the interview instrument, which had 3 major domains: data systems, informatics capacity, and perceptions around the future of informatics. Intercoder reliability was examined; in coded portions of transcripts that did not match, a consensus definition was established, and interviews were recoded. Interviewees were asked a number of questions about the types of information systems their LHD managed, had access to, and how interoperable these various systems were. Interview data were analyzed thematically in NVivo 10 (QSR International, Burlington, Massachusetts).41
Survey phase
The quantitative data were drawn from the 2015 Informatics Capacity and Needs Assessment Survey, conducted by the Jiann-Ping Hsu College of Public Health at Georgia Southern University in collaboration with National Association of County & City Health Officials (NACCHO). This Web-based survey had a target population of all LHDs in the United States. A representative sample of 650 LHDs was drawn using a stratified random sampling design, based on 7 population strata: less than 25 000; 25 000-49 999; 50 000-99 999; 100 000-249 999; 250 000-499 999; 500 000-999 999; and 1 000 000 and more. LHDs with larger population were systematically oversampled to ensure inclusion of a sufficient number of large LHDs in the completed surveys. The targeted respondents were informatics staff designated by the LHDs through a mini-survey conducted prior to the main survey. A structured questionnaire was constructed and pretested with 20 informatics staff members. The questionnaire included various measures to examine the current informatics capacity and needs of LHDs. The survey questionnaire was sent via the Qualtrics survey software to the sample of 650 LHDs. The survey remained open for 8 weeks in 2015. A total of 324 completed responses were received, with a 50% response rate. Given that only a sample of all LHDs participated in the study and the larger LHDs were oversampled and overrepresented, statistical weights were developed to account for 3 factors: (a) disproportionate response rate by population size (7 population strata, typically used in NACCHO surveys); (b) oversampling of LHDs with larger population sizes; and (c) sampling rather than the census approach. A multivariable logistic regression was conducted, using interoperability status of the information systems as a binary outcome (Yes/No). If an LHD answered “Some of the systems are interoperable,” “Most the systems are interoperable,” or “All of the systems are interoperable” to the question “How interoperable are the information systems used for your LHD?” then it was coded as “Yes” (1); otherwise, it was coded as “No” (0) if an LHD answered “None of the systems are interoperable.”
On the basis of previous studies on factors associated with IT capacities and information systems implementation,42–44 independent variables were selected, including jurisdiction characteristics (population size) and governance characteristics as independent variables. LHD governance structure was coded as state/shared versus local governance, and LHD jurisdiction population size was transformed into logarithmic values in logistic regression analysis because the absolute values resulted in skewed distribution. LHDs' informatics capacity building is shaped by whether it is formally included in LHDs' strategic plans and whether formal assessments are conducted to understand the gaps in capacities relative to the needs.45 Variables representing strategic priorities and formal assessment processes included completion of review of IT system in the past 2 years (Yes/No), creation of IT strategic plan throughout LHD (Yes/No), completion of business process analysis and redesign (Yes/No), and provision of project management (Yes/No). Other variables showing LHD's control over various aspects of informatics covered through variables such as control of data management (Yes/No), control of data quality (Yes/No), control of IT budget allocation (Yes/No), support from leadership (Yes/No), access to technical support (Yes/No), and LHD self-rating of IT infrastructure (poor/fair, average, and good/excellent). SPSS 23 (IBM Corporation, Armonk, New York) was used for conducting the multivariable logistic regression analysis of factors associated with interoperability.46
Results
Qualitative perspectives on barriers to interoperability and negative impacts
Barriers to interoperability
As displayed in Table 1, there are 5 main barriers reported by respondents, such as resource-intensive nature of initiatives of interoperable systems, lack of master-patient index, LHDs not being in control of the IT system, different codes/standards, different levels of sophistication, and lack of appropriate staff. Overall, the 3 main issues are lack of financial resources and IT expertise at LHDs, and different IT systems that are incompatible.
TABLE 1 •. Barriers to Interoperability of Information Systems and Impacts on LHD Functioning, Data From Qualitative Interviews.
| Themes | Selected Illustrative Quotes |
|---|---|
| Barriers to interoperability of information systems | |
| Interoperable systems are resource intensive | “I think the main reason we don't [have] it is because the technology is expensive and requires expertise that are not available; [our] county is a local rural health department, so ....” |
| “No, they do not cross over; that's one of our problems; they can create patches and sort of get them to work, but I heard that ... it takes a lot of IT hours and expertise and sometimes additional programs to do that.” | |
| No master-patient index for clinical data | “We were working on creating a master patient index so we can do that better, but we all may link somewhere now [manually], ....” |
| LHDs are not main developers of the systems used | “I think that there are certainly some opportunities for interoperability, but like I said, not being the main developer for some of those applications has definitely hindered our ability to maybe provide input or suggestions on future development efforts, but definitely when it is under our control we definitely try and do that but it's probably minimal at this point.” |
| Systems are developed by different organizations with different codes/standards, at different levels of sophistication | “Communicable disease and the environmental health are part of the same [information system]; they are from the same company vendor solutions and different aspects of their program. The Electronic health record that we pick is not from the same company. Because we are a primary health care provider, we needed a very robust health record.” |
| “They ... don't have necessarily uniformed formats. They're not kept in similar files, and so one of the things that I and some of my colleagues wind up doing is when we're pulling information from multiple sources, then we're doing sort of the reconciling and making, you know, making one coherent story based on all the various pieces of information.” | |
| “We basically log in to the system. So basically they have a system and we just log in to participate. I mean we do things internally and, most of it is Excel. Because of our staff capacity, we try to do a couple of things with Access and (laughs).” | |
| IT staff are not available | “I would say the state has a lot of data systems, but ...we are not able at this time [to have them communicate].... As far as we are concerned, we have a lot of data systems but they don't talk to each other; does that make sense?” |
| “Well, I have the ability to analyze data and store data and share data and I have some level of expertise to connect things. I don't have an IT staff that can prepare software to connect electronic medical records with a registry and, like I said, most of the registries belong or are maintained at the state level.” | |
| Negative impact of lack of interoperability | |
| Care coordination and continuation of care difficulties | “I think one of the challenges for us is we work in a community that has two very large health care systems, and our patients–for us, from our clinic–is [sic] one of the major health care systems. The electronic medical records do not communicate at all, and so that is then a major barrier as far as continuity of care for that patient; it would be helpful if there was cross-wiring that could occur or if we just had access to the other hospital system's record, but we don't. So that's a major barrier. I do think that our system is slow and so providers will say that it's a barrier to productivity. It's not the most fluid system I've ever worked in, so it does take a lot of time to document and sign off on labs and things like that.” |
| “I guess I would say I don't have a direct line into the state informatics system that they use. I do know that this is individual results that we get; a paper report is sent back to our clinic that is scanned into the person's chart, and then I have access to that.” | |
| “One of our big clinical data systems and billing system is called HMS in Florida, Health Management System; it was created by our state office. We do not have the ability at this point in time to look at another health department's data. So, if a patient came from Miami to where I live in [County], I could not go into Miami's HMS and look at that client's record. I mean it's not technically possible.” | |
| Difficulty coordinating activities across different programs within LHD | “They [information systems] are not really designed to do that [communicate with each other]. So if we were to have a death certificate that's tied to a property where a decedent passes in their home, if we get a complaint about a property being a hazard or we send an abatement order for them to clean the house up, there's no interoperability between the environmental dataset and the vital records dataset to join those two records by the property, currently. But we are actually moving towards one that would eventually join those two.” |
| Different levels of observation for different data make data integration difficult | “Well, the only information that we get is from the state; it's not integrated necessarily at the local level in terms of some of the other data that we get from the local organizations that may have it.... The information the programs are utilizing is much more meaningful for them versus some of the information that's gathered either [by] the funder or the state or even at the federal level. A lot of the data at those levels [are] really about units of service where the programs are looking for actual impact for the client served.” |
| Duplication of effort | “No, I would say that we find ourselves in the situation where some of our programs [ar] doing dual data entry because there is not a linkage between the two data systems. And then some of those systems actually request very similar but slightly different data, and we have not been able to get those individuals to take a look at the broader approach. In fact, many of them come out of the Iowa Department of Health and we do find ourselves in some of their programs doing the data, dual data entry.” |
| “For immunizations we have a statewide system that local physicians and clinics and hospitals can input that on immunization. That is interoperable throughout the state; that's a good system. As far as the others, they are pretty much stand-alone separate systems that are not really [interoperable]; they really don't talk to each other. We have to go into each system separately to obtain data.” | |
| Delay in detecting outbreaks | “The only thing that makes them connected is the person that says, ‘Oh my God’; we've been notified that we have one report of illness for Salmonella. And then the State Health Department, because they many times get reports more than we do or they could get a complaint. They will notify us and they say, ‘Oh, you've got a foodborne outbreak on your hands.’ So then we can start connecting the dots after the fact.” |
| Loss of efficiency in information retrieval due to multiple log-on required | “I would say not really; no they are not really interoperable, ..., but yeah there's not a lot of interoperability between like our communicable disease surveillance system, and the immunization register like that; people have to have multiple logons, like go into those different systems and cross-check that way; yeah, so there's not a lot of interoperability.” |
| Timeliness of data jeopardized | “We have a real hard time especially with the local hospital of getting information in a timely fashion. We are still even struggling with the physician clinic which is a separate corporation. Physician clinic is Mayo; the hospital ownership is by a big company up in the twin cities called the Allina. They have different EMR systems of their own. They have trouble talking to each other even. So communications and timeliness are huge.” |
| No real use of interoperable systems | “Well, the [two major information systems] do not speak to each other, but they are two totally different things but they do work very well with other people's database; like electronic health records communicates with [one database] and we are able to see that. We don't have electronic medical records except for the [one] database and [the other] is communicable diseases and the other is vaccinations; they really have no real use to communicate with each other, no reason to do that.” |
Abbreviations: EMR, electronic medical record; IT, information technology; LHD, local health department.
Negative impacts due to lack of interoperability
There are 8 main themes depicting negative impacts. They included difficulty in coordination of care with other providers and within LHD clinics, data from state or federal level becoming less useful at local level, duplication of efforts in collecting data, delay in detecting outbreak of disease at local level, cumbersome log-on process, LHDs' inability to get data from hospitals in a timely manner, and IT systems not talking to each other. Thus, the incompatible IT systems at the local level resulted in difficulties in coordination of care/service both internally and externally, issues concerning timely data sharing, and duplication of efforts in collecting data.
Quantitative findings
Sample characteristics are presented in Table 2. About 41% of LHDs reported their IT systems are interoperable (some, most, or all systems). About 81.5% of LHDs in the sample had decentralized/local governance with respect to state authority. Roughly 40% of LHDs' survey participants rated their IT infrastructure excellent or good, but more than a quarter of them rated it as poor or fair. Twenty-four percent of LHDs created a strategic plan for their information systems, and 24% conducted business process analysis.
TABLE 2 •. Descriptive Statistics for the Variables in the Analyses, 2015.
| LHD Organizational Characteristics | Percent (Weighted) | Frequency (Unweighted) |
|---|---|---|
| Interoperability status of the information systems | 297 | |
| None of the systems interoperable/don't know/NA | 58.6 | |
| Some, most, or all systems are interoperable | 41.4 | |
| Decentralized governance (ie, shared or state governance) | 324 | |
| State or shared | 18.5 | |
| Local | 81.5 | |
| Self-rating of IT infrastructure | 318 | |
| Poor/fair | 26.1 | |
| Average | 34.0 | |
| Good/excellent | 39.9 | |
| In past 2 y, LHD reviewed current systems to determine if they need to be improved or replaced | 312 | |
| No | 28.9 | |
| Yes | 71.1 | |
| In 2 y, LHD created a strategic plan for information systems throughout your LHD | 312 | |
| No | 76.3 | |
| Yes | 23.7 | |
| LHD conducts business process analysis and redesign | 306 | |
| No | 76.0 | |
| Yes | 24.0 | |
| LHD provides project management | 306 | |
| No | 64.2 | |
| Yes | 35.8 | |
| LHD controls data management | 317 | |
| No | 37.4 | |
| Yes | 62.6 | |
| LHD controls data quality | 317 | |
| No | 68.1 | |
| Yes | 31.9 | |
| LHD controls IT budget allocation | 317 | |
| No | 41.7 | |
| Yes | 58.3 | |
| Support from leadership available | 277 | |
| Yes | 78.5 | |
| No, lack support | 21.5 | |
| LHD adequate access to technical support or expertise | 277 | |
| Yes | 62.7 | |
| No | 37.3 | |
| Mean | SE | |
| LHD jurisdiction population (log) | 10.6 | 0.027 |
| LHD jurisdiction population | 122 726 | 6,805 |
Abbreviations: IT, information technology; LHD, local health department.
Status of interoperability of LHDs' information systems
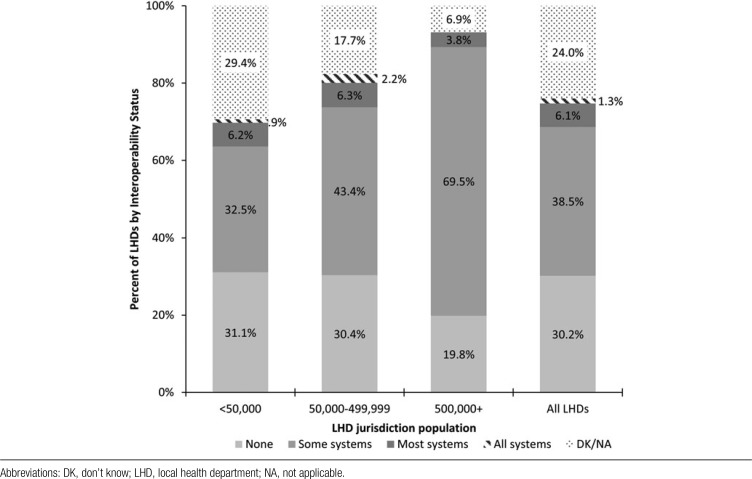
The Figure displays the status of IT system interoperability by jurisdiction population size. LHDs with jurisdictions with larger jurisdiction population seemed to have better interoperability, as 69.5% of LHDs with a jurisdiction population size of 500 000+ reported most of their IT systems were interoperable. In contrast, 32.5% of LHDs with a population size of less than 50 000 and 43.4% of LHDs with a population size of 50 000-499 999 reported having most systems interoperable (P < .01). The proportion of LHDs reporting “none of their IT was interoperable” was 31.1% in LHDs with a population size of less than 50 000 but 19.8% in LHDs with 500 000+ population.
FIGURE •.
Interoperability of Information Systems Used or Maintained by LHDs, by Size of Population in LHD Jurisdiction
Multiple logistic regression results
The multiple logistic regression model results showed that LHDs with larger jurisdiction population size were more likely to have an interoperable IT system than smaller LHDs (adjusted odds ratio [AOR] = 1.20; 95% CI, 1.11-1.29). LHDs with a state/shared governance structure (AOR = 1.75; 95% CI, 1.32-2.32) were more likely to have an interoperable IT system than LHDs with a local governance structure (Table 3).
TABLE 3 •. Logistic Regression of Interoperabilitya of LHD Informatics Systems, 2015b.
| LHD Organizational Characteristics | AOR | 95% CI for exp(B) | Pc | |
|---|---|---|---|---|
| Lower | Upper | |||
| LHD jurisdiction population (log) | 1.20 | 1.11 | 1.29 | <001 |
| Shared or state governance (vs local) | 1.75 | 1.32 | 2.32 | <001 |
| Self-rating of IT infrastructure (vs poor or fair) | <001 | |||
| Average | 1.50 | 1.16 | 1.93 | .002 |
| Good/excellent | 1.88 | 1.43 | 2.46 | <001 |
| In 2 y, reviewed current system to determine if they need to be improved or replaced (vs No) | 1.66 | 1.31 | 2.10 | <001 |
| In 2 y, LHD created a strategic plan for information systems throughout your LHD (vs No) | 1.92 | 1.51 | 2.43 | <001 |
| LHD conducts business process analysis and redesign | 1.49 | 1.17 | 1.90 | <001 |
| LHD provides project management | 2.14 | 1.71 | 2.66 | <001 |
| LHD controls data management | 2.31 | 1.57 | 3.40 | <001 |
| LHD controls data quality | 1.69 | 1.32 | 2.16 | <001 |
| LHD controls IT budget allocation | 2.48 | 1.68 | 3.67 | <001 |
| Support from leadership available (vs No) | 3.54 | 2.72 | 4.60 | <001 |
| LHD had adequate access to technical support or expertise (vs lacked accessed) | 1.39 | 1.11 | 1.73 | .004 |
Abbreviations: AOR, adjusted odds ratio; IT, information technology; LHD, local health department.
aInteroperability as the dependent variable was coded as follows: having all, most, or some systems interoperable = 1; no system interoperable or do not know = 0.
bAll of the variables in the table were included in the logistic regression simultaneously, resulting in the AORs presented in the table.
cP values in bold font indicate that AOR is significantly different than 1.
LHDs that had completed IT system review (AOR = 1.66; 95% CI, 1.31-2.10) or created an IT strategic plan (AOR = 1.92; 95% CI, 1.51-2.43) in the past 2 years were more likely to have an interoperable IT system. In addition, LHDs that provided project management (AOR = 2.14; 95% CI, 1.71-2.66) or conducted business process analysis and redesign (AOR = 1.49; 95% CI, 1.17-1.90) were more likely to have data management capacity (AOR = 2.31; 95% CI, 1.57-3.40) were more likely to have an interoperable system. LHDs that controlled their own data management (AOR = 2.31; 95% CI, 1.57-3.40), data quality (AOR = 1.69; 95% CI, 1.32-2.16), and IT budget allocation (AOR = 2.48; 95% CI, 1.68-3.67) were more likely to have an interoperable IT system. Finally, LHDs that had leadership support (AOR = 3.54; 95% CI, 2.72-4.60) or had adequate access to IT technical support (AOR = 1.39; 95% CI, 1.11-1.73) were more likely to have an interoperable IT system.
Discussion
The study results revealed several barriers and facilitators of interoperability of systems used or maintained by LHDs. Both qualitative and quantitative data highlighted the importance of leadership, both within the agency and potentially at the state. State health agencies can create information systems that link many LHDs to state data, as well as each other. This is especially the case in centralized, or shared governance model states and also potentially very useful in home-rule/decentralized states.47 Our findings about leadership support as the strongest facilitator of interoperability are consistent with the findings from a qualitative assessment in another study that revealed that leadership support was critical for LHD informatics.48 Interview participants reported significant financial, human, and technical difficulties preventing greater interoperability. A long history of project and LHD-specific databases and proprietary data formats have impacted interoperability of information systems. Because of such a lack of interoperability, many LHD information systems are incapable of interacting with outside organizations, as well as within their own agency.
Interoperability of information systems used by local public health agencies is in general poor, with roughly 4 in 10 LHDs reporting some, most, or all of their information systems being interoperable. Having informatics-savvy health departments is desirable across the spectrum of LHDs, as their capacities to exchange and manage information are critical in an era of health care reform.2,17,18 Although many LHDs do not provide clinical care directly, the absence of direct provision of clinical services does not diminish LHDs' need for health care information to guide their surveillance and assessment efforts. Regardless of clinical care needs, LHDs may want to engage in interorganizational information sharing with a large number of community partners in order to take advantage of data-driven decision making. Information sharing may also be essential for assessment and surveillance. Lack of interoperability may hamper LHDs' efforts to perform many essential public health functions. For instance, LHDs' inability to efficiently receive and use data will make it difficult to deal with the changing environment that requires evidence-based administrative and service delivery practices.
Factors related to the control of various aspects of LHD informatics were also significant factors for IT interoperability, including IT budget allocation, data management, and data quality control. This may imply that when LHDs may not control their own budget allocation, the system interoperability may not get priority. When LHD staff do not have control of budget allocation, those engaged in budgetary decisions may not be as aware of the benefits associated with having interoperable systems as the LHD staff.
Our findings also support the proposition that if LHD information systems or other informatics issues are not included in the list of high priority strategic issues and, in turn, do not become part of the strategic plan, LHD informatics cannot be strengthened.
The study results also indicated that LHDs that had reviewed their information systems to determine whether they need to be improved or replaced or those with strategic plans for information systems had better levels of interoperability of their information systems. This is consistent with the idea that assessment and strategic prioritization of informatics needs lead to better outcomes.45 Adequate availability of technical support was also a positive influence on interoperability of information systems.
Our study shows that LHD population size is a significant influence on interoperability levels of LHDs, suggesting that larger LHDs may have an edge due to economies of scope and scale. LHDs under state governance or in shared governance arrangements are also better off than those in decentralized governance structures. The favorable impact of state/shared governance indicates that unlike many other aspects of LHD informatics where locally governed LHDs have stronger informatics capacities,41 being centrally governed or having shared governance is beneficial for interoperability of the information systems.
Our study findings should be interpreted within the limitation that a definition of interoperability was not provided to the survey participants, leaving the meaning of the term to their interpretation. Although we examined level of interoperability, the type of interpretability (foundational, structural, semantic, etc)21 was not explored in this study.
Conclusion
Public health informatics is about both the infrastructure of health departments' information systems and the capacity to use data to further the public health enterprise. Data use capacity and IT infrastructure go hand in hand, and their inadequacy serves as the primary limiting factor in the field of public health. Leadership, financial support, assessment of existing IT systems, strategic prioritization, better LHD control over IT-related decision making, and technical know-how are key promoters of interoperability within LHDs nationwide. Local and state health department leadership have key roles to play in motivating informatics uptake, which itself holds the promise to transform the practice of public health. Interoperability may allow, not only, greater interaction and access to big data, but it can also facilitate greater cross-jurisdictional sharing of services and promote public transparency through improved data availability to all stakeholders. Interoperable systems may improve connectivity of LHDs with other community partners to support health improvement efforts with real-time visualization of health data. Despite all the potential benefits associated with informatics uptake, the majority of LHDs in this nation—especially those serving smaller jurisdictions—do not have systems that can talk to each other. Greater investment in LHDs' IT and human resource capacity will be necessary to move the field forward within public health.
Footnotes
The survey project analyzed in this manuscript received funding from the National Association of County and City Health Officials. The key informant interview project received funding from the de Beaumont Foundation.
No conflicts of interest declared.
REFERENCES
- 1.Laymon B, Shah G, Leep CJ, Elligers JJ, Kumar V. The proof's in the partnerships: are Affordable Care Act and local health department accreditation practices influencing collaborative partnerships in community health assessment and improvement planning? J Public Health Manag Pract. 2015;21(1):12–17. [DOI] [PubMed] [Google Scholar]
- 2.Leider JP, Castrucci BC, Russo P, Hearne S. Perceived impacts of health care reform on large urban health departments. J Public Health Manag Pract. 2015;21(suppl 1):S66–S75. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Bittle MJ. A new vision and leadership challenge: implementing the Affordable Care Act to improve the organization and delivery of health care services. J Public Health Manag Pract. 2015;21(1):59–61. [DOI] [PubMed] [Google Scholar]
- 4.Joseph S, Sow M, Furukawa MF, Posnack S, Chaffee MA. HITECH spurs EHR vendor competition and innovation, resulting in increased adoption. Am J Manag Care. 2014;20(9):734–740. [PubMed] [Google Scholar]
- 5.Shah GH, Madamala K. Knowing where public health is going: levels and determinants of workforce awareness of national public health trends. J Public Health Manag Pract. 2015;21:S102–S110. [DOI] [PubMed] [Google Scholar]
- 6.Borron SW. Checklists for hazardous materials emergency preparedness. Emerg Med Clin North Am. 2015;33(1):213–232. [DOI] [PubMed] [Google Scholar]
- 7.Tucker CA, Larkin SN, Akers TA. Food safety informatics: a public health imperative. Online J Public Health Inform. 2011;3(2):ojphi.v3i2.3832. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Shah GH, Williams K, Shah BG. Implementation of electronic disease reporting systems by local health departments. Front Public Health Serv Sys Res. 2015;4(4):13–20. [Google Scholar]
- 9.Savel TG, Foldy S. The role of public health informatics in enhancing public health surveillance. MMWR Surveill Summ. 2012;61(suppl):20–24. [PubMed] [Google Scholar]
- 10.Birkhead GS, Klompas M, Shah NR. Public health surveillance using electronic health records: rising potential to advance public health. Front Public Health Serv Sys Res. 2015;4(5):25–32. [Google Scholar]
- 11.Rabarison KM, Timsina L, Mays GP. Community health assessment and improved public health decision-making: a propensity score matching approach. Am J Public Health. 2015;105(12):2526–2533. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Shah GH, Sheahan JP. Local health departments' activities to address health disparities and inequities, are we moving in the right direction? Int J Environ Res Public Health. 2016;13(1)44. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Alberti P. Community health needs assessments: filling data gaps for population health research and management. EGEMS. 2015;2(4):1174. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Reams C, Powell M, Edwards R. State synergies and disease surveillance: creating an electronic health data communication model for cancer reporting and comparative effectiveness research in Kentucky. EGEMS. 2014;2(2):1064. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Harris JK, Erwin PC, Smith C, Brownson RC. The diffusion of evidence-based decision making among local health department practitioners in the United States. J Public Health Manag Pract. 2015;21(2):134–140. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Jacob RR, Baker EA, Allen P, Dodson EA, Duggan K, Fields R, et al. Training needs and supports for evidence-based decision making among the public health workforce in the United States. BMC Health Serv Res. 2014;14(1):564. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.LaVenture M, Brand B, Ross DA, Baker EL. Building an informatics-savvy health department, part I: vision and core strategies. J Public Health Manag Pract. 2014;20(6):667–669. [DOI] [PubMed] [Google Scholar]
- 18.LaVenture M, Brand B, Ross DA, Baker EL. Building an informatics-savvy health department, part II: operations and tactics. J Public Health Manag Pract. 2015;21(1):96–99. [DOI] [PubMed] [Google Scholar]
- 19.O'Carroll PW. Public Health Informatics and Information Systems. New York, NY: Springer; 2003. [Google Scholar]
- 20.Healthcare Information and Management Systems Society (HIMSS). What is interoperability? http://www.himss.org/library/interoperability-standards/what-is-interoperability. Accessed February 25, 2016.
- 21.Levy B. Health Language Blog. Understand the three levels of interoperability. http://blog.healthlanguage.com/understand-the-three-levels-of-interoperability. Published 2014. Accessed February 16, 2016.
- 22.Ola O, Sedig K. The challenge of big data in public health: an opportunity for visual analytics. Online J Public Health Inform. 2014;5(3):223. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23.Rudolph L, Caplan J, Mitchell C, Ben-Moshe K, Dillon L. Health in All Policies: Improving Health Through Intersectoral Collaboration. Washington, DC: National Academy of Sciences; 2013. [Google Scholar]
- 24.Vest JR, Kern LM, Silver MD, Kaushal R; HITEC Investigators. The potential for community-based health information exchange systems to reduce hospital readmissions. J Am Med Inform Assoc. 2015;22(2):435–442. [DOI] [PubMed] [Google Scholar]
- 25.Park H, Lee SI, Hwang H, et al. Can a health information exchange save healthcare costs? Evidence from a pilot program in South Korea. Int J Med Inform. 2015;84(9):658–666. [DOI] [PubMed] [Google Scholar]
- 26.Bowers K, Carradus B, Hinkeldey C, et al. Developing a statewide electronic public health care coordination tracking system. J Pediatric Nurs. 2014;30(2):416–420. [DOI] [PubMed] [Google Scholar]
- 27.Rosenstein BS, Capala J, Efstathiou JA, et al. How will big data improve clinical and basic research in radiation therapy? [published online ahead of print November 11, 2015]. Int J Radiat Oncol Biol Phys. 10.1016/j.ijrobp.2015.11.009. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 28.Khoury MJ, Ioannidis JP. Big data meets public health: human well-being could benefit from large-scale data if large-scale noise is minimized. Science. 2014;346(6213):1054–1055. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 29.Baker E. Open source data logger for low-cost environmental monitoring. Biodivers Data J. 2014;2:e1059. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 30.Coleman EW, Delea KC. The use of public health informatics to improve environmental health practice. J Environ Health. 2013;76(5):44–45. [PMC free article] [PubMed] [Google Scholar]
- 31.Janati A, Hosseiny M, Gouya MM, Moradi G, Ghaderi E. Communicable disease reporting systems in the world: a systematic review article. Iran J Public Health. 2015;44(11):1453–1465. [PMC free article] [PubMed] [Google Scholar]
- 32.Charles-Smith LE, Reynolds TL, Cameron MA, et al. Using social media for actionable disease surveillance and outbreak management: a systematic literature review. PLoS ONE. 2015;10(10):e0139701. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 33.Bernardo TM, Rajic A, Young I, Robiadek K, Pham MT, Funk JA. Scoping review on search queries and social media for disease surveillance: a chronology of innovation. J Med Internet Res. 2013;15:e147. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 34.Yom-Tov E, Borsa D, Cox IJ, McKendry RA. Detecting disease outbreaks in mass gatherings using Internet data. J Med Internet Res. 2014;16(6):e154. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 35.Li J, Shah GH, Hedber C. Complaint-based surveillance for food-borne illness in the united states: a survey of local health departments. J Food Prot. 2011;74(3):432–437. [DOI] [PubMed] [Google Scholar]
- 36.Kharrazi H, Weiner JP. IT-enabled community health interventions: challenges, opportunities, and future directions. EGEMS. 2014;2(3):1117. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 37.Plough A. Developing new systems of data to advance a culture of health. EGEMS. 2014;2(4):1180. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 38.Dixon BE, McGowan JJ, Grannis SJ. Electronic laboratory data quality and the value of a health information exchange to support public health reporting processes. AMIA Annu Symp Proc. 2011;2011:322–330. [PMC free article] [PubMed] [Google Scholar]
- 39.Dixon BE, Pina J, Kharrazi H, Gharghabi F, Richards J. What's past is prologue: a scoping review of recent public health and global health informatics literature. Online J Public Health Inform. 2015;7(2):e216. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 40.National Association of Local Health Departments. 2013 National Profile of Local Health Departments. Washington, DC: National Association of County & City Health Officials; 2014. http://nacchoprofilestudy.org/wp-content/uploads/2014/02/2013_National_Profile021014.pdf. Accessed February 16, 2016. [Google Scholar]
- 41.QSR International Pty Ltd (QSR). NVivo Qualitative Data Analysis Software. Version 10. Doncaster, Victoria, Australia: QSR International Pty Ltd; 2012. [Google Scholar]
- 42.Vest JR, Issel LM. Factors related to public health data sharing between local and state health departments. Health Serv Res. 2014;49(1, pt 2):373–391. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 43.Shah GH, Leider JP, Castrucci B, Williams K, Luo H. Characteristics of local health departments associated with their implementation of electronic health records and other informatics systems. Public Health Rep. 2016;131(2):272–282. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 44.McCullough JM, Zimmerman FJ, Bell DS, Rodriguez HP. Local public health department adoption and use of electronic health records. J Public Health Manag Pract. 2015;21(1):E20–E28. [DOI] [PubMed] [Google Scholar]
- 45.Cheatham M. Informatics works in local health departments NACCHO Exchange. 2013;12(1):1–2. [Google Scholar]
- 46.IBM Corp. IBM SPSS® Statistics: Version 23.0 for Windows. Armonk, NY: IBM Corp; 2015. [Google Scholar]
- 47.Riley WJ, Gearin KJ, Parrotta CD, Briggs J, Gyllstrom ME. Tax levy financing for local public health: fiscal allocation, effort, and capacity. Am J Prev Med. 2013;45(6):776–781. [DOI] [PubMed] [Google Scholar]
- 48.Lovelace K, Shah GH. An Iterative, Low-Cost Strategy to Building Information Systems Allows a Small Jurisdiction Local Health Department to Increase Efficiencies and Expand Services. J Public Health Manag Pract. 2016;22(suppl 6):S95–S100. [DOI] [PMC free article] [PubMed] [Google Scholar]