Abstract
Disturbances in circadian rhythms have been suggested as a possible cause of bipolar disorder (BD). Included in this study were 31 mood episodes of 26 BD patients, and 18 controls. Circadian rhythms of BD were evaluated at admission, at 2-week intervals during hospitalization, and at discharge. All participants wore wrist actigraphs during the studies. Saliva and buccal cells were obtained at 8:00, 11:00, 15:00, 19:00, and 23:00 for two consecutive days. Collected saliva and buccal cells were used for analysis of the cortisol and gene circadian rhythm, respectively. Circadian rhythms had different phases during acute mood episodes of BD compared to recovered states. In 23 acute manic episodes, circadian phases were ~ 7 hour advanced (equivalent to ~ 17 hour delayed). Phases of 21 out of these 23 cases returned to normal by ~ 7 hour delay along with treatment, but two out of 23 cases returned to normal by ~ 17 hour advance. In three cases of mixed manic episodes, the phases were ~ 6–7 hour delayed. For five cases of depressive episodes, circadian rhythms phases were ~ 4–5 hour delayed. After treatment, circadian phases resembled those of healthy controls. Circadian misalignment due to circadian rhythm phase shifts might be a pathophysiological mechanism of BD.
Keywords: Circadian rhythm, Bipolar disorders, Phase shift, Circadian dysregulation
Highlights
-
•
Bipolar disorder in acute mood episodes showed circadian dysregulation due to phase shifts which returned to normal after treatment.
-
•
Acute manias were ~ 7 h circadian phase advanced, mixed manias were > 6 h delayed, whereas depressions were 4-5 h delayed compared to the controls.
-
•
Circadian dysregulation due circadian rhythm phase shifts might be a pathophysiological mechanism of bipolar disorder.
Bipolar disorder is a common mental disorder characterized by mood disturbances with alternating episodes of mania and depression. Circadian rhythms are rhythms of about 24 h found in many body functions. We repeatedly measured circadian rhythms in bipolar disorder patients during hospitalization. Acute manic episodes were associated with circadian dysregulation of ~ 7 hour phase advances, mixed manias were > 6 hour delayed, whereas bipolar depression was associated with 4–5 hour phase delays compared to the controls. After treatment, the shifted rhythms recovered to the normal range. This study suggests that novel chronotherapy approaches based on our findings might be found useful for the prevention and treatment of bipolar disorder.
1. Introduction
Bipolar disorder (BD) is a common mental disorder characterized by episodic mood symptoms of mania or depression. Episodic relapses of BD are very common, and therefore BD is one of the major leading causes of disability around the world (Goldberg and Harrow, 2004). Numerous etiologies for BD have been proposed, but there is no conclusive evidence.
Humans exhibit an orchestration of circadian rhythmicity with respect to the light-dark cycle (Reppert and Weaver, 2002), involving regulation of physiological processes such as the autonomic nervous system, hormone secretion, and sleep-wake cycles (Dijk and Czeisler, 1995). Circadian rhythms can be entrained by both photic and nonphotic stimuli, however light plays the primary role in the entrainment of the human circadian pacemaker to the environment (Lavie, 2001). The hypothalamic suprachiasmatic nuclei (SCN) are a master clock for the orchestration of circadian rhythmicity. The SCN synchronize peripheral oscillators to ensure temporally coordinated physiology, while the peripheral oscillators interact among themselves and communicate back to the SCN (Schibler and Sassone-Corsi, 2002). The endogenous circadian rhythmicity affects timing for sleep-wake cycles and biochemical rhythms. The circadian regulation of the sleep-wake cycle is thought to be mediated by multisynaptic projections from the SCN to sleep-wake centers of the brain (Deurveilher and Semba, 2005, Saper et al., 2005). Biochemical rhythms such as cortisol concentrations are also thought to be affected by endogenous circadian timing systems (Bremner et al., 1983). Time coordination of functions affected by endogenous circadian rhythmicity may result from predictive regulation of function rather than being entirely reactive, for example, body temperature and plasma cortisol increase prior to waking from sleep (Fuller et al., 2006).
Disruptions of circadian rhythms have long been proposed as a fundamental cause of BD (Gonzalez, 2014). Some research has suggested that the intrinsic circadian pacemaker of BD was shorter than a close-to-24-hour period (Wehr et al., 1985). Other hypotheses emphasized phase shifts as the primary circadian rhythm disturbances in BD (Salvatore et al., 2008, Wood et al., 2009). Another formulation suggested that instability in the behaviors of BD patients were keys to disruption of circadian rhythms (Lee et al., 2013). There are many studies suggesting an association between variations in circadian genes and BD as well as specific clinical subphenotypes (Maciukiewicz et al., 2014). Both lithium and valproic acid, used to treat BD, have been shown to influence the rhythmic expression of circadian genes and the rhythmic properties of molecular clocks, especially via inhibition of glycogen synthase kinase-3β (GSK-3β) (Li et al., 2002). There are a wide diversity of reported circadian abnormalities and many unresolved questions.
First, are there characteristic sequential changes in circadian rhythms related to the exacerbation of BD symptoms? So far, studies about the disturbances of circadian rhythms related to BD have been almost entirely cross-sectional (Nurnberger et al., 2000, Wood et al., 2009). If we identify sequential changes of circadian rhythms with the clinical transitions from severe mood states (such as mania or depression or mixed states) to euthymic states, it will provide a deeper understanding of circadian rhythms associated with BD.
Second, how should we interpret the variations of circadian rhythm shifts within studies of BD (Nurnberger et al., 2000, Salvatore et al., 2008)? As highlighted by the subphenotypes in genetic studies of BD (Craddock and Sklar, 2009), we speculate that there could be several subphenotypes correlated with distinctive changes of circadian rhythms within BD.
Third, are there inconsistencies in disorders when measuring circadian rhythm variables of different body systems at the same time, so-called internal desynchronization? Most of the studies have been analyses of independent variables such as hormonal, genetic, or physical activity (Nurnberger et al., 2000, Salvatore et al., 2008). However, these variables may differ in sensitivity to reflect aspects of human circadian rhythm systems. If we compare several circadian rhythm variables of different systems at the same time, it might distinguish dysregulation of circadian coordination in these systems.
To clarify the questions mentioned above, we serially measured behavior and biochemical circadian rhythms in BD during hospitalization from severe states at admission to euthymic states at discharge, and compared them with those of healthy controls.
2. Materials & Methods
2.1. Participants
The patients with BD were recruited from inpatients at the Department of Psychiatry, Korea University Anam Hospital, Seoul, Republic of Korea. Included in the study were 26 manic episodes of 22 Bipolar I disorder (BD-I) patients (12 male and 10 female) who were hospitalized from May 2012 to June 2014, 5 depressive episodes of 5 BD patients (2 male and 3 female, 2 BD-I and 3 BD-II) who were hospitalized from June 2014 to March 2015, and 18 healthy subjects (11 male and 7 female) were assessed from September 2012 to November 2012. The ages of the participants [mean ± SD] were 30.42 ± 10.88 years for patients and 23.00 ± 3.57 years for healthy controls. One BD patient was observed in both manic and depressed episodes during different hospitalizations. In sum, 31 mood episodes requiring hospitalization of 26 BD patients were analyzed. There were no significant differences with respect to characteristics including age and sex among groups (Table 1).
Table 1.
Demographic data of study population.
| Patients with bipolar disorder | Healthy controls | P value | |
|---|---|---|---|
| Number of subjects | 26 | 18 | – |
| Age (mean ± SD), years | 30.42 ± 10.88 | 23.00 ± 3.57 | 0.083 |
| Sex (M/F), N | 13/13 | 10/8 | 0.717 |
| Bipolar type (I/II), N | 23/3 | N/A | – |
| Education (mean ± SD), years | 13.85 ± 1.95 | 14.39 ± 2.33 | 0.407 |
| Age of onset (mean ± SD), years | 21.19 ± 7.68 | N/A | – |
| Total number of mood episodes (mean ± SD) | 7.62 ± 5.87 | 0 | – |
| Family loading of mood disorder, % | 57.7 | 0 | – |
| Total number of psychiatric hospitalizations (mean ± SD) | 3.62 ± 2.43 | 0 | – |
N, number of subjects.
Diagnoses were determined by two psychiatrists (H.-J.L and C.-H.C) according to DSM-IV-TR criteria using the Korean version of the Mini International Neuropsychiatric Interview (Yoo et al., 2006). Patients with BD who needed to be hospitalized because of the aggravation of mood symptoms, were recruited for the study. Inclusion criteria of the participants were: 1) Diagnosis of BD according to DSM-IV-TR criteria and 2) Acute mood episode requiring hospitalization for intensive psychiatric treatment. Patients or controls with intellectual disability, organic brain injury, or other major psychiatric disorders were excluded from the present study. All participants underwent screening to exclude past or present major medical disorders such as cardiovascular disease, metabolic disease (including diabetes mellitus), hormonal disease (including thyroid disease), and cancer. Clinical symptoms were evaluated with the Young Mania Rating Scale (YMRS) (Young et al., 1978), the 17-item Hamilton Depression Rating Scale (HAMD) (Hamilton, 1980), and the Clinical Global Impression-Bipolar Version (CGI-BP) (Spearing et al., 1997).
Through in-depth interviews by a psychiatrist (H.-J.L) with all volunteers, we confirmed that controls had no personal or familial psychiatric history. All participants completed questionnaires regarding their sleep conditions to exclude controls who had irregular or disturbed sleep/wake patterns. Controls were excluded if working night shifts or reporting sleep patterns suggestive of circadian rhythm phase disorders. The mood disorder questionnaire (MDQ) was used to assess subthreshold bipolarity (Hirschfeld et al., 2000). Only those with MDQ scores < 7 were included in the control group.
Participants were informed about the purpose and procedures of the study and all participants provided informed written consent prior to enrollment after a full explanation and thorough understanding of this study. The study protocol was approved by the Institutional Review Board of Korea University Anam Hospital and was conducted in accordance with the Declaration of Helsinki.
2.2. Protocol
Patients were hospitalized during treatment and wore Actiwatch-L activity recorders on a non-dominant wrist (Philips Respironics, Bend, OR, USA). The sleep habits of hospitalized subjects were controlled by the regular ward routine, i.e., they went to bed at 22:00 h and were awakened at 06:00 h. Light exposure was also controlled by the ward routine, i.e., the lights were turned off from 22:00 h to 06:00 h and turned on from 06:00 h to 22:00 h. All BD patients had free access to natural daylight through the window during the day, and provided saliva (≥ 1 mL) directly into Salivettes (Sarstedt AG & Co., Nümbrecht, Germany). Buccal epithelial cells were collected and immediately placed into RNAlater (Sigma-Aldrich, St. Louis, MO, USA). Sample collection was begun with the start of hospitalization and continued at 08:00, 11:00, 15:00, 19:00, and 23:00 for two consecutive days and then repeated at 2-week intervals during hospitalization and then right before discharge. The nighttime sample collections (at 23:00) were performed by well-trained experimental staff without additional light exposure, under light as dim as possible, but these collections did require brief awakenings, and it is known that patients with acute psychiatric illnesses usually have disturbed sleep.
Each control subject participated in the study for one week and wore an Actiwatch-L. Controls lived near the hospital and were asked to maintain same sleep-wake schedules as hospitalized BD patients. Their sleep-wake times were checked by actigraphy data. Controls entered the hospital for the last two days of their participation, and the sampling was performed in the same conditions as with patients.
2.3. Measurement of Physical and Sleep-Wake Activity
Circadian rhythms of physical activity were analyzed using the Actiwatch-L and Cosinor software (Circadian Rhythm Laboratory of Boise State University, Boise, ID, USA). The software estimates the phase of a circadian rhythm by determining its acrophase, which is the time of the peak of the best-fitting sine curve, as illustrated in several figures. Non-parametric circadian rhythm analysis was also performed as described previously (Rock et al., 2014). “M10” and “L5” were denoted as intervals of the 10 most active hours and the 5 least active hours, respectively. “M10 activity” and “L5 activity” were defined as the levels of Actiwatch-L activity during “M10” and “L5”, respectively. “Relative amplitude” was calculated as follows: (“M10 activity” − “L5 activity”)/(“M10 activity” + “L5 activity”).
Circadian rhythms of sleep-wake activity were analyzed using the Actiwatch-L and Philips Respironics Actiware software (Philips Respironics, Bend, OR, USA). “Sleep onset time” and “final wake time” were estimated by the algorithms of the software. “Total sleep period” was defined as a length of time from “sleep onset time” to “final wake time”, and the total sleep period included “wake time” within sleep, which was defined as minutes of activity by the algorithm. “Total sleep time” was defined as “total sleep period,” subtracting “wake time”. “Sleep onset latency” was defined as a length of time from “bedtime” to “sleep onset time”. “Sleep efficiency” was denoted as percentage of “total sleep time”/“total sleep period”.
2.4. Measurement of Salivary Cortisol
Coat-A-Count Cortisol (Siemens Healthcare Diagnostics Inc., Los Angeles, USA) was used for salivary cortisol assays. The analytical sensitivity was 0.01 μg/dL. The intra-assay coefficient of variation was 3% for samples of 0.19 ± 0.10 μg/dL and 4% for samples of 0.24 ± 0.02 μg/dL. The inter-assay coefficient of variation was 12% for samples of 1.85 ± 0.10 μg/dL and 14% for samples of 0.24 ± 0.02 μg/dL.
2.5. Measurement of Circadian Gene Expression
To observe circadian rhythms of gene expression, we tested five circadian clock genes (ARNTL, PER1, PER2, PER3, and NR1D1) extracted from buccal epithelial cells, and observed more relevant circadian rhythms of ARNTL and PER1 than in the other genes. The circadian rhythms of ARNTL and PER1 were inverse in phase to each other, in agreement with previous studies of circadian oscillation (Akashi et al., 2010, Chung et al., 2014, Guo et al., 2006, Novakova et al., 2015, Son et al., 2008). Accordingly, to obtain the most distinguishable circadian rhythms, we investigated the relative gene expression of ARNTL and PER1, as performed and validated in a previous study (Cho et al., 2016, Guo et al., 2006). Briefly put, circadian gene expression levels of PER1 and ARNTL were determined by RT-qPCR: then their ratios of PER1/ARNTL at each sampling time were used to describe circadian rhythms. Total RNA was isolated using RNeasy Micro Kit (Qiagen Inc., Valencia, CA, USA) from buccal epithelial cells, and only RNA samples concentrated to > 200 ng/μL were subjected to next step. The whole RNA sample was reverse-transcribed using the Sensiscript Reverse Transcription Kit (Qiagen). Then, cDNA was subjected to the Taqman PCR reaction using an Applied Biosystems StepOnePlus Real-Time PCR Systems (ThermoFisher Scientific, Foster City, CA, USA). The primers and Taqman probes used in this experiment are as follows; PER1 (NM_002616): forward 5′-CTCACACAGCTCCTCCTCAG-3′, reverse 5′-TTTGTGCTCTTGCTGCTCTC-3′, probe 5′FAM-CGGCAAGGACTCAGCCCTGC-3′BHQ1; ARNTL (NM_001030272): forward 5′-TGCCTCGTCGCAATTGG-3′, reverse 5′-ACCCTGATTTCCCCGTTCA-3′, probe 5’FAM-CGACTGCATTCTCATGTAGTTCCACAACCA-3′BHQ1.
2.6. Sine Regression Analysis
Biochemical rhythms were fitted with sine curves using SigmaPlot software (Systat Software Inc., San Jose, CA, USA).
2.7. Statistical Analysis
Collected data were summarized using mean ± SD and frequencies for continuous variables and categorical variables, respectively. We conducted Fisher's exact tests and Wilcoxon rank sum tests in order to compare general characteristics of categorical and continuous variables among groups, respectively. For the analyses of physical, sleep-wake activity, cortisol and gene expression, we used marginal models with unstructured variance-covariance to compare groups and times accounting for within subject correlation. In addition, we also considered the within-episode correlations, since episodes are nested within subjects in these models. Post-hoc tests were applied if needed using Tukey-Kramer tests which were proper for repeated measures data. All analyses were implemented by SAS version 9.4 for Windows (SAS Institute Inc., Cary, NC, USA).
2.8. Role of the Funding Source
The funder of the study had no role in study design, data collection, data analysis, data interpretation, or writing of the report. The corresponding author had full access to all the data in the study and had final responsibility for the decision to submit for publication.
3. Results
3.1. Circadian Rhythms of Physical and Sleep-Wake Activity
Patients did not show significant differences in any parameters for physical activity when compared to healthy controls, neither in recovered nor during acute mood exacerbations (Table 2).
Table 2.
Circadian rhythms of physical activity in bipolar disorder patients with manic and depressive episodes and healthy controls.
| Manic episodes, N = 26 |
Depressive episodes, N = 5 |
Healthy controls, N = 18 | P value | |||
|---|---|---|---|---|---|---|
| Acute state | Recovered state | Acute state | Recovered state | |||
| Period, h | 23.92 ± 0.59 | 24.02 ± 0.44 | 24.16 ± 0.23 | 24.04 ± 0.24 | 24.02 ± 0.66 | 0.859 |
| Robustness, % | 22.83 ± 9.1 | 22.93 ± 7.89 | 23.07 ± 3.55 | 23.08 ± 1.74 | 23.08 ± 5.03 | 0.993 |
| Mesor | 247.57 ± 72.12 | 245.76 ± 89.72 | 242.28 ± 33.29 | 244.26 ± 38.51 | 246 ± 46.2 | 0.986 |
| Amplitude | 169.88 ± 62.75 | 168.62 ± 48.82 | 162.54 ± 15.84 | 165.96 ± 22.4 | 168.58 ± 71.09 | 0.974 |
| Acrophase, h | 14.99 ± 1.32 | 15.38 ± 1.12 | 16.22 ± 1.06 | 15.88 ± 0.96 | 15.33 ± 2.12 | 0.324 |
| M10 onset time, hh:mma | 11:12 ± 01:03 | 11:13 ± 01:01 | 11:15 ± 00:49 | 11:12 ± 01:01 | 11:13 ± 01:05 | 0.998 |
| M10 activityb | 24,726 ± 5431 | 24,661 ± 2798 | 23,027 ± 3133 | 24,131.4 ± 6393 | 24,692 ± 4527 | 0.708 |
| L5 onset time, hh:mmc | 02:13 ± 01:04 | 02:16 ± 01:03 | 02:15 ± 01:16 | 02:12 ± 00:44 | 02:14 ± 01:03 | 0.998 |
| L5 activityd | 1518 ± 280 | 1444 ± 416 | 1351 ± 309 | 1407.6 ± 385 | 1467.61 ± 267 | 0.511 |
| Relative amplitudee | 0.87 ± 0.1 | 0.89 ± 0.03 | 0.89 ± 0.02 | 0.89 ± 0.03 | 0.89 ± 0.03 | 0.765 |
Values are mean ± SD.
P values are for differences among three group means corrected for time effects (manic episodes versus depressive episodes versus healthy controls).
N, number of episodes in BD patients and number of subjects in healthy controls; h, hour; M10, period of the 10 most active hours; and L5, period of the 5 least active hours. 26 manic episodes include 3 mixed manic episodes.
The onset time of periods for the 10 most active hours.
The levels of activity during the 10 most active hours.
The onset time of periods for the 5 least active hours.
The levels of activity during the 5 least active hours.
The difference between “M10 activity” and “L5 activity” and calculated as follows: (“M10 activity” − “L5 activity”)/(“M10 activity” + “L5 activity”).
Analyses of sleep parameters of manic episodes found significant changes over time in group means for final wake time and sleep efficiency (Table 3). The final wake time was delayed about 1 h and the sleep efficiency was increased about 4% during hospitalization from admission to recovery. In contrast, analyses of depressive episodes found no significant differences over time for any sleep parameters.
Table 3.
Circadian rhythms of sleep-wake activity in bipolar disorder patients with manic and depressive episodes.
| Manic episodes, N = 26 |
Depressive episodes, N = 5 |
Healthy controls, N = 18 | ||||||||
|---|---|---|---|---|---|---|---|---|---|---|
| Course of hospitalization |
P value | Course of hospitalization |
P value | |||||||
| Manic | 2 weeks after | 4 weeks after | Recovered | Depressive | 2 weeks after | Recovered | ||||
| Sleep oneset time, hh:mm | 21:56 ± 1:11 | 21:58 ± 0:52 | 21:39 ± 0:20 | 21:49 ± 0:53 | 0.763 | 21:42 ± 0:21 | 22:42 ± 1:43 | 22:36 ± 1:00 | 0.264 | 23:09 ± 1:41 |
| Final wake time, hh:mm | 6:35 ± 0:54 | 6:44 ± 1:00 | 6:35 ± 1:15 | 7:36 ± 4:54 | 0.001⁎⁎ | 7:43 ± 0:53 | 6:43 ± 0:48 | 7:08 ± 0:51 | 0.449 | 7:01 ± 0:53 |
| Total sleep period, hh:mm | 9:07 ± 1:27 | 9:11 ± 1:48 | 9:04 ± 0:46 | 8:58 ± 1:34 | 0.862 | 11:17 ± 1:27 | 8:55 ± 2:20 | 9:03 ± 1:16 | 0.063 | 8:11 ± 0:47 |
| Total sleep time, hh:mm | 7:33 ± 1:30 | 7:30 ± 1:36 | 7:38 ± 1:09 | 7:35 ± 1:24 | 0.450 | 8:31 ± 1:58 | 7:13 ± 1:25 | 7:08 ± 0:43 | 0.363 | 7:38 ± 0:49 |
| Sleep onset latency, m | 18.15 ± 15.19 | 19.35 ± 21.20 | 11.33 ± 13.76 | 9.96 ± 13.43 | 0.146 | 17.80 ± 13.86 | 7.00 ± 1.41 | 13.60 ± 10.36 | 0.767 | 6.72 ± 9.56 |
| Sleep efficiency, % | 79.97 ± 10.31 | 80.44 ± 9.15 | 83.58 ± 8.93 | 83.75 ± 9.51 | 0.048⁎ | 74.78 ± 7.41 | 81.68 ± 5.48 | 81.85 ± 6.15 | 0.293 | 84.44 ± 7.48 |
| Wake-time after sleep onset , m | 78.77 ± 51.27 | 64.75 ± 47.89 | 55.00 ± 32.94 | 54.73 ± 45.45 | 0.238 | 91.20 ± 58.70 | 83.50 ± 51.62 | 62.20 ± 33.95 | 0.525 | 41.11 ± 36.17 |
Values are mean ± SD.
P values are for differences among successive time points for each group of manic and depressive episodes.
N, number of episodes; and m, minutes.
P < 0.05.
P < 0.01.
3.2. Biochemical Circadian Rhythms
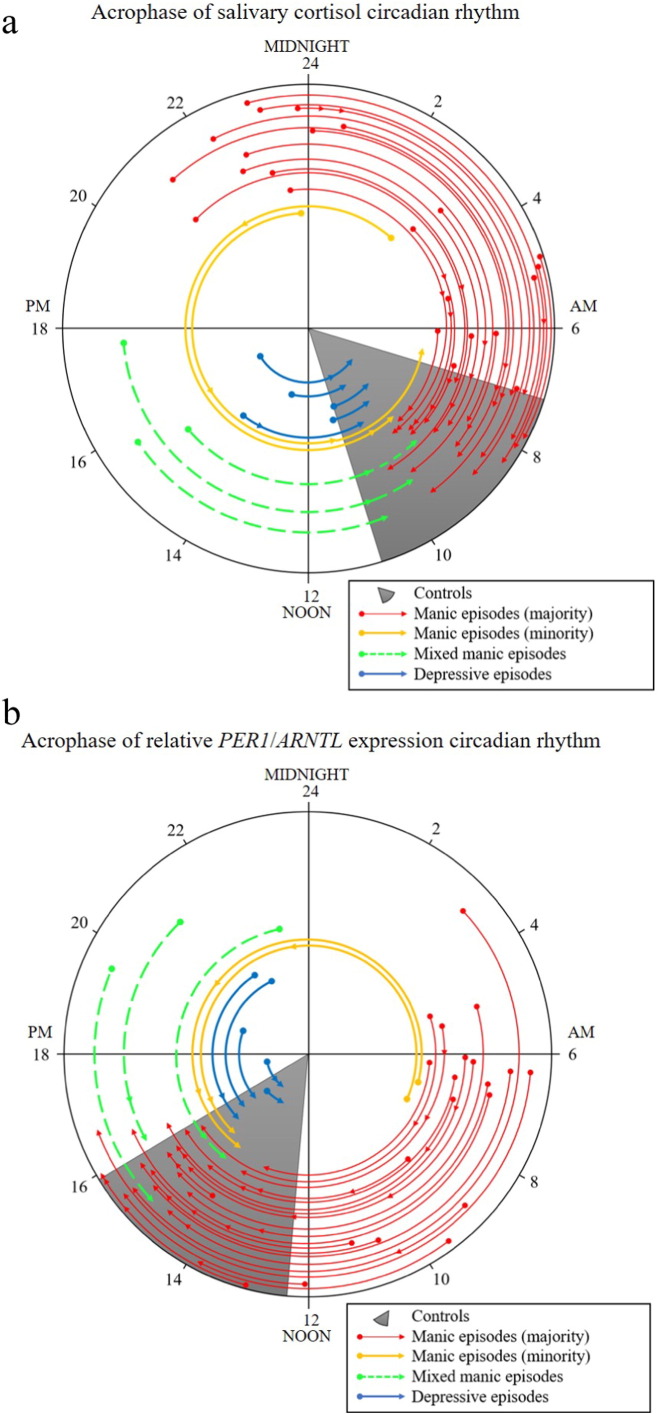
Changes in biochemical circadian rhythms from acute to recovery states of BD were observed (Fig. 1). Biochemical circadian rhythms of acute mood episodes commenced with different phases compared to those of the recovered states.
Fig. 1.
The shifting of acrophases of circadian rhythms in bipolar disorder patients. Note that the acrophase is the timing of the peak of the best-fitting sine curve. (a) The acrophase transitions of salivary cortisol circadian rhythms in bipolar patients compared to controls as the circadian peaks shifted in timing. (b) The acrophase transitions of the relative PER1/ARNTL expression circadian rhythms in bipolar patients compared to controls. The outer circular axis indicates the clock time of each acrophase assessment for each patient. Acrophases of circadian rhythms of bipolar patients were observed over the course of hospitalization. Evaluation was performed at acute states (near start of hospitalization), and every two weeks into recovery states (at the end of hospitalization). The arrow presents the direction of change in acrophase of the circadian rhythm from the acute state to the recovery state of each patient. If the duration of hospitalization was no longer than 2 weeks, there were only initial and final assessments, so the acrophase arc is an arrow that has a solid circle at the time of the first acute acrophase assessment and the head of the arrow pointing to the recovery acrophase. If the duration of hospitalization was longer than 2 weeks, there were sometimes intermediate and final assessments, with acrophases illustrated as two or three arrow heads along the arc. Red and orange arrows indicate the shifting of acrophase of circadian rhythms in manic episodes, green arrows indicate that of mixed episodes, and blue arrows indicate that of depressive episodes. The gray sector indicates the range of acrophases for the healthy controls. The radius of each arc was arbitrarily chosen to contrast the different groups of participants, and does not represent the amplitudes of the circadian rhythms.
Fig. 1 and Table 4 clearly show that the biochemical circadian rhythms of acute manic and depressive episodes were different from those of controls. Notably, the biochemical circadian rhythms in salivary cortisol concentrations and PER1/ARNTL expression ratios had contrasting initial phases during the acute mood episodes, but transitioned by comparable phase shifts during recovery, almost entirely arriving within the normal control ranges.
Table 4.
Biochemical circadian rhythms in bipolar disorder patients with manic and depressive episodes and healthy controls.
| Manic episodes (N = 26) |
|||||||||||||||
|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|
| Manic episodes (majority) |
Manic episodes (minority) |
Mixed manic episodes |
Depressive episodes (N = 5) |
||||||||||||
| Manic N = 21 | 2 weeks after N = 16 | 4 weeks after N = 4 | Recovered N = 21 | Manic N = 2 |
2 weeks after N = 2 |
4 weeks after N = 2 |
Recovered N = 2 |
Mixed N = 3 |
2 weeks after N = 2 |
Recovered N = 3 |
Depressive N = 5 |
2 weeks after N = 2 |
Recovered N = 5 |
Healthy controls (N = 18) |
|
| Cortisol | |||||||||||||||
| Acrophase, h | 2.03 ± 3.41⁎⁎⁎ | 6.18 ± 2.13⁎⁎ | 6.61 ± 3.87 | 8.53 ± 0.88 | 0.98 ± 1.7⁎⁎⁎ | 18.37 ± 3.86⁎⁎⁎ | 10.52 ± 0.41 | 7.71 ± 2.12 | 16.34 ± 1.5⁎⁎ | 10.47 ± 0.03 | 9.64 ± 0.88 | 13.83 ± 2.78⁎⁎ | 12.68 ± 2.87 | 9.15 ± 0.72 | 8.44 ± 0.92 |
| Amplitude, μg/dL | 0.19 ± 0.1 | 0.18 ± 0.09 | 0.24 ± 0.07 | 0.21 ± 0.06 | 0.35 ± 0.12 | 0.23 ± 0.1 | 0.18 ± 0.15 | 0.21 ± 0.05 | 0.26 ± 0.1 | 0.19 ± 0.04 | 0.23 ± 0.01 | 0.19 ± 0.03 | 0.20 ± 0.03 | 0.19 ± 0.02 | 0.19 ± 0.08 |
| PER1/ARNTL | |||||||||||||||
| Acrophase, h | 7.78 ± 2.92⁎⁎⁎ | 11.85 ± 2.95⁎⁎⁎ | 12.17 ± 3.24 | 15.34 ± 0.81 | 7.21 ± 0.75⁎⁎⁎ | 22.05 ± 2.24⁎⁎ | 16.57 ± 0.15 | 14.66 ± 0.75 | 21.41 ± 1.77⁎⁎⁎ | 16.40 ± 1.12 | 14.97 ± 1.01 | 19.21 ± 2.87⁎⁎ | 15.38 ± 0.77 | 14.82 ± 0.57 | 14.85 ± 0.76 |
| Amplitude | 19.24 ± 8.15⁎⁎ | 20.1 ± 5.62⁎ | 24.07 ± 3.03⁎⁎ | 27.26 ± 4.74 | 21.03 ± 5.41 | 22.61 ± 3.24 | 26.57 ± 9.26 | 22.03 ± 10.92 | 17.95 ± 7.33 | 25.60 ± 0.47 | 24.14 ± 5.97 | 19.41 ± 10.07 | 19.78 ± 9.71 | 25.83 ± 6.78 | 26.58 ± 5.17 |
Values are mean ± SD.
Significantly different from recovered state.
N; number of episodes in BD patients and number of subjects in healthy controls; and h, hour.
P < 0.05.
P < 0.01.
P < 0.001.
3.3. Healthy Controls
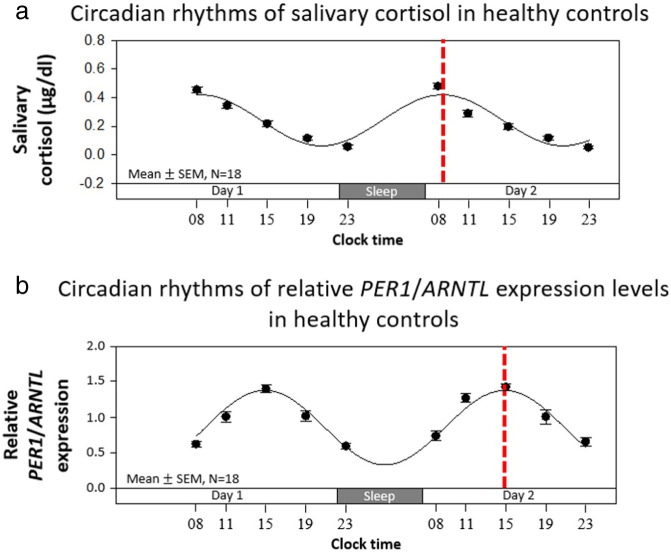
The biochemical circadian rhythms in control subjects are depicted in Table 4 and Fig. 2.
Fig. 2.
Mean biochemical circadian rhythms in healthy controls (N = 18). (a) Circadian rhythms of salivary cortisol in healthy controls. (b) Circadian rhythms of relative PER1/ARNTL expression levels in healthy controls. Black dots indicate mean ± SEM, curved black lines indicate the fitted sine curves of mean values, and broken red lines indicate the timing of the acrophases of each circadian rhythm.
3.4. Manic Episodes
Of 26 manic episodes, 21 episodes showed similar phase shifts of the biochemical circadian rhythms during hospitalization (Fig. 1, Fig. 3). Significant differences of acrophase of cortisol circadian rhythms were observed in acute manic states and after 2 weeks of hospitalization when compared with recovered states (Table 4). Similarly, acrophases of gene expression circadian rhythms also showed significant differences between acute manic states and after 2 weeks of hospitalization when compared with recovered states (Table 4). In sum, at admission, most of the manic episodes showed about 7 hour advanced biochemical circadian acrophases in acute states (equivalent to 17 hour delayed), and recovered through delays (clockwise), returning to the normal range of the control group. Moreover, a significant increase in the PER1/ARNTL circadian amplitude accompanying recovery from mania was observed in these manic episodes (Table 4). Circadian rhythms of each patient recovering from the majority of manic episodes are illustrated in the Supplemental Figs. S1 and S2 for cortisol and gene expression, respectively.
Fig. 3.
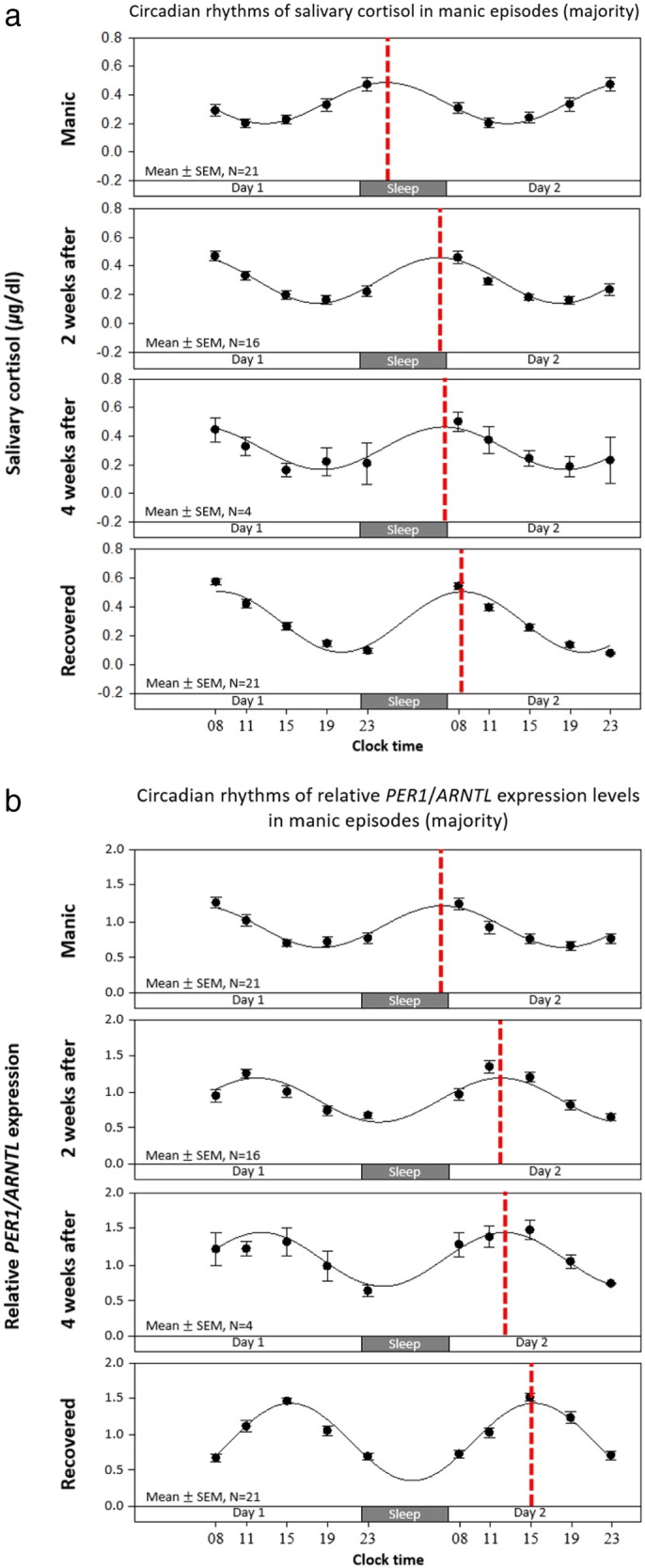
Mean biochemical circadian rhythms in manic episodes (majority, N = 21 episodes). (a) Circadian rhythms of salivary cortisol in manic episodes (majority). (b) Circadian rhythms of relative PER1/ARNTL expression levels in manic episodes (majority). Black dots indicate mean ± SEM, curved black lines indicate the fitted sine curves of mean values, and broken red lines indicate acrophases of each circadian rhythms.
However, two out of 26 manic episodes had a pattern of circadian phase shifts different from those of the majority during recovery (Fig. 1, Fig. 4). The admission biochemical circadian rhythms in the minority manic states of the two cases were similar to the majority of manic episodes (about 7 hour advanced as compared to recovered states), but the recovery directions of the minor two cases were counterclockwise advances, opposite to those of majority. In other words, two cases out of 26 manic episodes showed recovery shifting of about 17 hour advancing. Circadian rhythms of each subject in the minority two cases of manic episodes are detailed in Supplemental Figs. S3 and S4 for cortisol and gene expression, respectively.
Fig. 4.
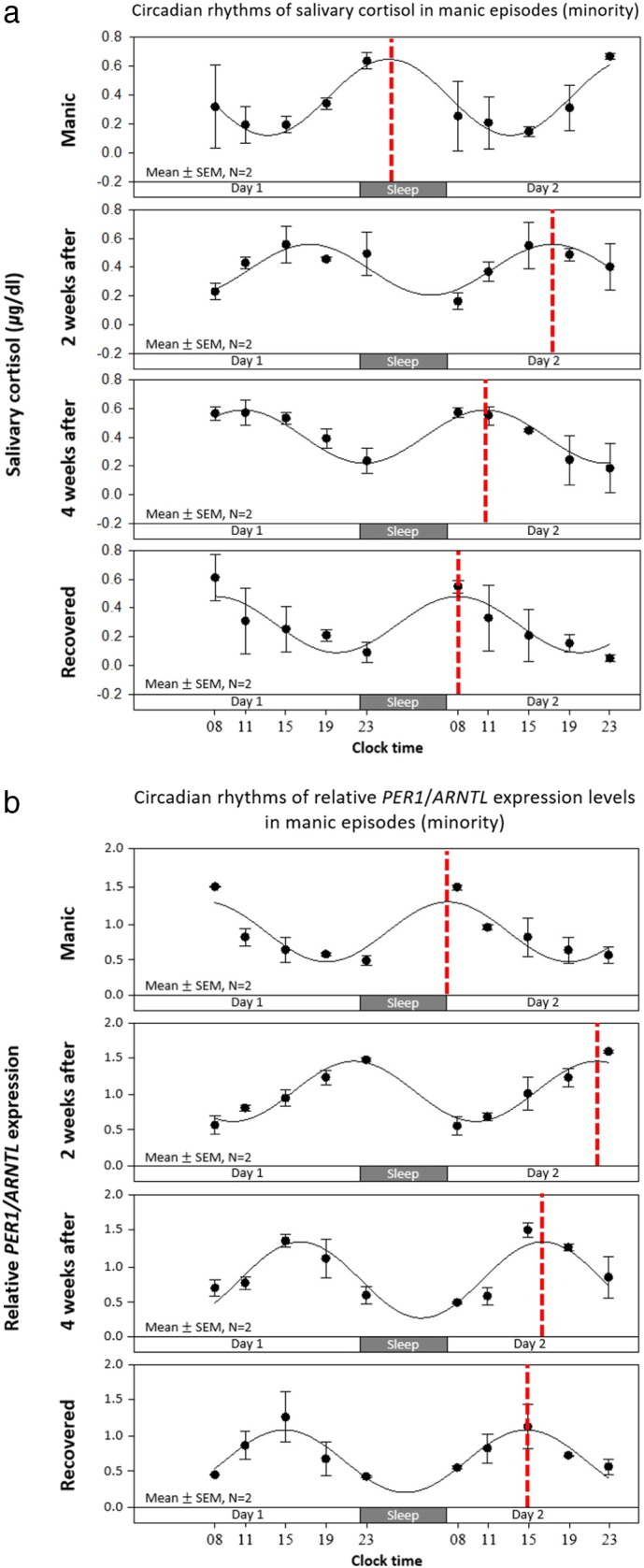
Mean biochemical circadian rhythms in manic episodes (minority, N = 2 episodes). (a) Circadian rhythms of salivary cortisol in manic episodes (minority). (b) Circadian rhythms of relative PER1/ARNTL expression levels in manic episodes (minority). Black dots indicate mean ± SEM, curved black lines indicate the fitted sine curves of mean values, and broken red lines indicate acrophases of each circadian rhythms.
3.5. Mixed Manic Episodes
Three out of 26 manic episodes were in mixed episodes displaying manic symptoms and moderate depressive symptoms simultaneously. These three mixed manic episodes showed a pattern of circadian phase shifts different from those of other manic episodes during hospitalization (Fig. 1, Fig. 5). Significant differences of cortisol and gene expression circadian rhythms were seen in the acute mixed states when compared with those of recovered states (Table 4). In sum, patients in mixed states recovered from manic episodes by about 6–7 h phase advances (counterclockwise). Circadian rhythms of each subject in the mixed manic episodes are in Supplemental Figs. S5 and S6 for cortisol and gene expression, respectively.
Fig. 5.
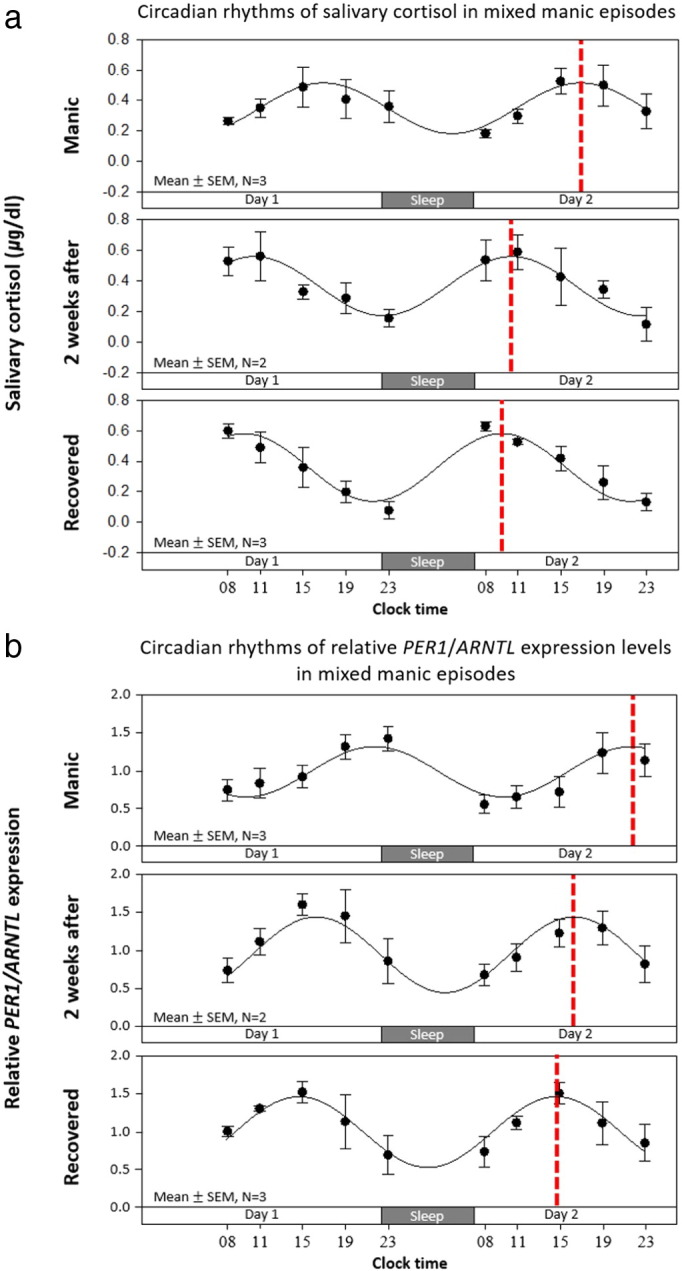
Mean biochemical circadian rhythms in mixed manic episodes (N = 3 episodes). (a) Circadian rhythms of salivary cortisol in mixed manic episodes. (b) Circadian rhythms of relative PER1/ARNTL expression levels in mixed manic episodes. Black dots indicate mean ± SEM, curved black lines indicate the fitted sine curves of mean values, and broken red lines indicate acrophases of each circadian rhythms.
3.6. Depressive Episodes
Patients with depressive episodes showed about 4–5 hour delayed biochemical circadian acrophases at the start of hospitalization, and then recovered through advances to the normal ranges of the control group (Fig. 1, Fig. 6). Significant differences of cortisol and gene expression circadian rhythms were seen in the acute depressive states when compared with those of recovered states (Table 4). Circadian rhythms of each subject with depressive episodes are detailed in Supplemental Figs. S7 and S8 for cortisol and gene expression, respectively.
Fig. 6.
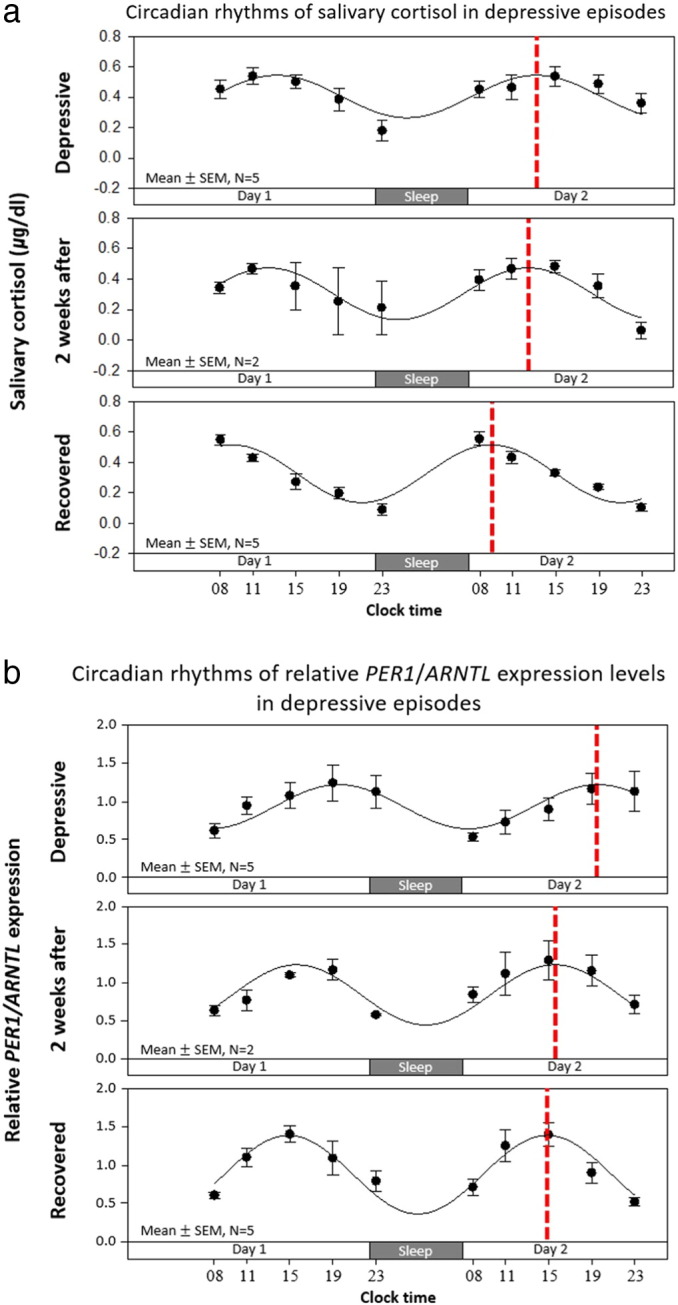
Mean biochemical circadian rhythms in depressive episodes (N = 5 episodes). (a) Circadian rhythms of salivary cortisol in depressive episodes. (b) Circadian rhythms of relative PER1/ARNTL expression levels in depressive episodes. Black dots indicate mean ± SEM, curved black lines indicate the fitted sine curves of mean values, and broken red lines indicate acrophases of each circadian rhythms.
3.7. Clinical Symptoms
Clinical symptoms of patients with BD had been reduced during treatment in all groups (Supplemental Figs. S9 and Table S1).
4. Discussion
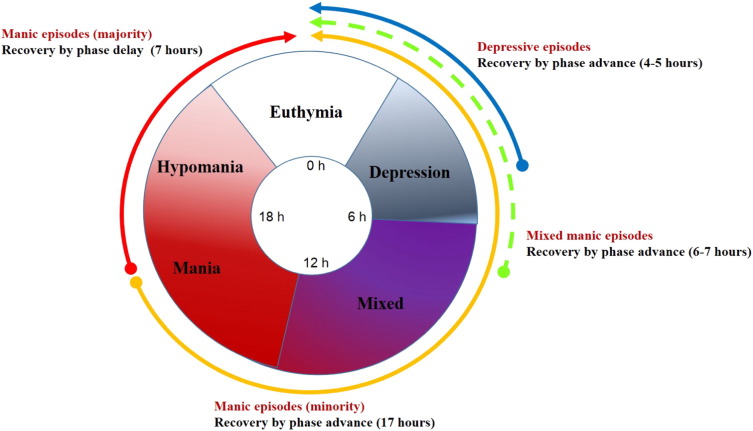
This study suggests that acute mood episodes are related to circadian misalignment between the individual's endogenous circadian rhythms and the individual's physical environment. Acute manic episodes were usually associated with biochemical circadian rhythm acrophases averaging 7 hour more advanced (earlier) than those of controls, though these acrophases could perhaps have resulted from an average of 17 hour clockwise delays. Mixed manias were > 6 hour delayed, whereas bipolar depression was associated with 4–5 hour phase delays compared to the controls. Interestingly, findings of advanced phase in mania and delayed phase in depression are parallel to studies of jetlag effects on BD that traveling east precipitate manic episode while traveling west induces depressive episode (Inder et al., 2016).
Previous studies suggested that disturbance of circadian rhythms is a possible mechanism of BD (Duarte Faria et al., 2015, Gonzalez, 2014, Kripke et al., 2015, McClung, 2007, Wirz-Justice, 2006). However, there has been no monitoring of circadian rhythms at the biochemical level tracking the healing from an acute mood episode to euthymia. This study provides novel observations of resolution of circadian phase abnormalities accompanying resolution of mood disturbances.
When biochemical circadian rhythms were observed in manic episodes, most (21 of 26) episodes showed one pattern of phase shift. Two cases of manic episodes showed similar acrophases in acute states but different recovery directions to those of the majority of manic episodes. Our data do not disclose the direction of phase shifting during the development of mania, though some phase aberrations resolved in opposite directions during recovery. Because these two different recovery directions could be related to medication effects, we compared the medications between groups. However, there were no evident differences in medication between the minority and majority of manic episodes (Supplemental Table S2).
Three of 26 manic episodes arose in mixed states and showed a pattern of circadian shifts distinct from other manic episodes. During the acute mixed states, patients showed about 6–7 hour delayed phases compared to those in recovered states. Interestingly, when biochemical circadian rhythms were observed in depressive episodes, the result showed about 4–5 h delayed circadian phases in acute depressive states compared to recovered states. Thus, the phase orientation of the biochemical rhythms of the mixed manic-depressives during the acute episodes were intermediate between the phases of pure manic and the depressive episodes, seemingly corresponding to the intermediate phenotype of mixed mania and depression. Both mixed manics and depressives corrected the phase delay during the acute mood episode by phase advance during recovery.
Mixed mania, also known as dysphoric mania or mixed features, is a condition during which features of mania and depression occur almost simultaneously. However, the pathophysiology of mixed mania was not well established. Transitions between manic or depressive states are common as demonstrated in a longitudinal study (Kotin and Goodwin, 1972). Polyphasic episodes, in which state changes occur without a euthymic mood period, resemble mixed states (Turvey et al., 1999). Furthermore, Sit et al. reported that the mixed states were induced by morning bright light treatment in women with bipolar depression and midday light therapy did not (Sit et al., 2007), which suggest that abrupt phase shifts by light may be a cause of mixed states. It is possible that morning light therapy for bipolar depressive patients induce further circadian delays because morning times may lie in the delay zone in the phase response curve for light during bipolar depression (Khalsa et al., 2003). Furthermore, hypersensitivity of circadian rhythm shifts to bright light has been suggested to be a possible biological marker for sub-threshold bipolarity and BD (Cho et al., 2016, Lewy et al., 1985).
One of the interesting aspects of the findings in this study is the dissociation between the large phase advances/delays observed in the biochemical rhythms and the much more moderate changes in the sleep/wake cycle. We believe that this discrepancy mainly derives from the environmental/behavioral constraints placed on sleep/wake behavior with hospitalization and medications. From initial stage of hospitalization, behavioral problems, especially sleep problems, were intensively treated. If the patients had not been treated, we assume that perhaps the discrepancies would not appear so great. Like adjustments for jet lags, after environmental circadian realignment, it takes time to be adjusted in alignment of the endogenous circadian rhythm. We suggested that BD patients tend to be easily circadian phase shifted by the disturbance of sleep wake cycles and some disordered Zeitgeber (e.g., inappropriate artificial light). We observed that delays of the circadian rhythm of salivary cortisol to bright light exposure before bedtime is related to subthreshold bipolarity (Cho et al., 2016).
From these findings, we suggest a new circadian rhythm shift model of BD (Fig. 7). Our observations indicate that the biochemical circadian phase orientations had distinct abnormalities in acute manic episodes versus mixed episodes versus depressive episodes, and that some phase disturbances resolved through advance and others through delay to recover the normal phase orientation. However, since we have no observations of the development of these abnormal states, we cannot infer with certainty whether some developed through advance or others through delay. It has been hypothesized that both bipolar depression and mania result from a tendency towards phase delay, but mania occurs when the delay is more extreme than in depression and may perhaps exceed 12 h, leading to resolution by a 360 degree delay rotation of phase (Kripke et al., 2015). Moreover, differing phase excursions of distinct cell groups within the SCN may be involved, contributing to internal desynchronization of peripheral circadian rhythms. Indeed, bifurcation of circadian secretion of melatonin suggesting bifurcation of SCN circadian systems has been hypothesized (Kripke et al., 2015, Novakova et al., 2015). In this regard, we have not noted any suggestion of bifurcation of individual circadian rhythms we have observed in bipolar patients, but it is possible that some dysregulation resembling pacemaker bifurcation might be suggested by dramatic phase abnormalities in cortisol and RNA expression contrasted to no significant phase changes in sleep and gross activity.
Fig. 7.
Hypothesis on circadian rhythm shift model of bipolar disorder. Circadian phase orientations had distinct abnormalities in acute manic episodes versus mixed episodes versus depressive episodes. The phase disturbances resolved through advance or delay to recover the normal phase orientation after treatment.
Despite sequential observation of biochemical circadian rhythm shifts during hospitalization in BD patients, we are aware of several limitations. First, the sample size in this study was relatively small. Considering the difficult study design, there were rather consistent results despite the small sample sizes. Second, this study observed transitions of biochemical circadian rhythms over two weeks intervals. We cannot sure what really happened in the initial two weeks of acute manic and depressive episodes. Some portion of manic patients showed normalized circadian shifts in the two weeks. To overcome of these limitations, future studies would be desirable with daily observation in the early stages of mood episodes, especially manic episodes.
In conclusion, biochemical circadian rhythms in manic episodes of bipolar patients were significantly advanced compared to controls. Mixed manic episodes and depressive episodes were associated with phase delays. After the treatment, the shifted rhythm recovered to normal. These findings provide a means for our understanding of the mechanisms of the circadian rhythm of bipolar mood episodes. The possibility of using circadian rhythms as a novel biomarker for diagnosis and treatment monitoring in bipolar disorder is suggested by these observations.
Conflict of Interests
All authors declare no competing interests.
Author Contributions
J.H.M., C.H.C., G.H.S., D.G., S.C., H.K., S.G.K., Y.M.P., H.K.Y., L.K., and H.J.L. designed the experiment. J.H.M., C.H.C., G.H.S., D.G., S.C., and H.J.L. performed the experiment. J.H.M., C.H.C., G.H.S., D.G., S.C., H.J.J, H.A., D.F.K., and H.J.L. analyzed the data. J.H.M., C.H.C., H.J. J, H.A., D.F.K., and H.J.L. wrote the manuscript. All authors reviewed, commented on, and approved the report.
Acknowledgements and Funding Sources
This study was supported by the Korea Health 21 R&D Project funded by the Ministry of Health & Welfare, Republic of Korea (HI14C3212 and HM14C2606) and by Ministry of Science, ICT and Future Planning, Republic of Korea (NRF-2012M3A9C7050135).
Footnotes
Supplementary data to this article can be found online at http://dx.doi.org/10.1016/j.ebiom.2016.08.019.
Appendix A. Supplementary Data
Supplementary material.
References
- Akashi M., Soma H., Yamamoto T., Tsugitomi A., Yamashita S., Yamamoto T., Nishida E., Yasuda A., Liao J.K., Node K. Noninvasive method for assessing the human circadian clock using hair follicle cells. Proc. Natl. Acad. Sci. U. S. A. 2010;107:15643–15648. doi: 10.1073/pnas.1003878107. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Bremner W.J., Vitiello M.V., Prinz P.N. Loss of circadian rhythmicity in blood testosterone levels with aging in normal men. J. Clin. Endocrinol. Metab. 1983;56:1278–1281. doi: 10.1210/jcem-56-6-1278. [DOI] [PubMed] [Google Scholar]
- Cho C.H., Moon J.H., Yoon H.K., Kang S.G., Geum D., Son G.H., Lim J.M., Kim L., Lee E.I., Lee H.J. Molecular circadian rhythm shift due to bright light exposure before bedtime is related to subthreshold bipolarity. Sci. Rep. 2016;6:31846. doi: 10.1038/srep31846. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Chung S., Lee E.J., Yun S., Choe H.K., Park S.B., Son H.J., Kim K.S., Dluzen D.E., Lee I., Hwang O., Son G.H., Kim K. Impact of circadian nuclear receptor REV-ERBalpha on midbrain dopamine production and mood regulation. Cell. 2014;157:858–868. doi: 10.1016/j.cell.2014.03.039. [DOI] [PubMed] [Google Scholar]
- Craddock N., Sklar P. Genetics of bipolar disorder: successful start to a long journey. Trends Genet. 2009;25:99–105. doi: 10.1016/j.tig.2008.12.002. [DOI] [PubMed] [Google Scholar]
- Deurveilher S., Semba K. Indirect projections from the suprachiasmatic nucleus to major arousal-promoting cell groups in rat: implications for the circadian control of behavioural state. Neuroscience. 2005;130:165–183. doi: 10.1016/j.neuroscience.2004.08.030. [DOI] [PubMed] [Google Scholar]
- Dijk D.J., Czeisler C.A. Contribution of the circadian pacemaker and the sleep homeostat to sleep propensity, sleep structure, electroencephalographic slow waves, and sleep spindle activity in humans. J. Neurosci. 1995;15:3526–3538. doi: 10.1523/JNEUROSCI.15-05-03526.1995. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Duarte Faria A., Cardoso Tde A., Campos Mondin T., Souza L.D., Magalhaes P.V., Patrick Zeni C., Silva R.A., Kapczinski F., Jansen K. Biological rhythms in bipolar and depressive disorders: a community study with drug-naive young adults. J. Affect. Disord. 2015;186:145–148. doi: 10.1016/j.jad.2015.07.004. [DOI] [PubMed] [Google Scholar]
- Fuller P.M., Gooley J.J., Saper C.B. Neurobiology of the sleep-wake cycle: sleep architecture, circadian regulation, and regulatory feedback. J. Biol. Rhythm. 2006;21:482–493. doi: 10.1177/0748730406294627. [DOI] [PubMed] [Google Scholar]
- Goldberg J.F., Harrow M. Consistency of remission and outcome in bipolar and unipolar mood disorders: a 10-year prospective follow-up. J. Affect. Disord. 2004;81:123–131. doi: 10.1016/S0165-0327(03)00161-7. [DOI] [PubMed] [Google Scholar]
- Gonzalez R. The relationship between bipolar disorder and biological rhythms. J. Clin. Psychiatry. 2014;75:e323–e331. doi: 10.4088/JCP.13r08507. [DOI] [PubMed] [Google Scholar]
- Guo H., Brewer J.M., Lehman M.N., Bittman E.L. Suprachiasmatic regulation of circadian rhythms of gene expression in hamster peripheral organs: effects of transplanting the pacemaker. J. Neurosci. 2006;26:6406–6412. doi: 10.1523/JNEUROSCI.4676-05.2006. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Hamilton M. Rating depressive patients. J. Clin. Psychiatry. 1980;41:21–24. [PubMed] [Google Scholar]
- Hirschfeld R.M., Williams J.B., Spitzer R.L., Calabrese J.R., Flynn L., Keck P.E., Jr., Lewis L., McElroy S.L., Post R.M., Rapport D.J., Russell J.M., Sachs G.S., Zajecka J. Development and validation of a screening instrument for bipolar spectrum disorder: the mood disorder questionnaire. Am. J. Psychiatry. 2000;157:1873–1875. doi: 10.1176/appi.ajp.157.11.1873. [DOI] [PubMed] [Google Scholar]
- Inder M.L., Crowe M.T., Porter R. Effect of transmeridian travel and jetlag on mood disorders: evidence and implications. Aust. N. Z. J. Psychiatry. 2016;50:220–227. doi: 10.1177/0004867415598844. [DOI] [PubMed] [Google Scholar]
- Khalsa S.B., Jewett M.E., Cajochen C., Czeisler C.A. A phase response curve to single bright light pulses in human subjects. J. Physiol. Lond. 2003;549:945–952. doi: 10.1113/jphysiol.2003.040477. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Kotin J., Goodwin F.K. Depression during mania: clinical observations and theoretical implications. Am. J. Psychiatry. 1972;129:679–686. doi: 10.1176/ajp.129.6.679. [DOI] [PubMed] [Google Scholar]
- Kripke D.F., Elliott J.A., Welsh D.K., Youngstedt S.D. Vol. 4. 2015. Photoperiodic and Circadian Bifurcation Theories of Depression and Mania. F1000Res. p. 107. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Lavie P. Sleep-wake as a biological rhythm. Annu. Rev. Psychol. 2001;52:277–303. doi: 10.1146/annurev.psych.52.1.277. [DOI] [PubMed] [Google Scholar]
- Lee H.J., Son G.H., Geum D. Circadian rhythm hypotheses of mixed features, antidepressant treatment resistance, and manic switching in bipolar disorder. Psychiatry Investig. 2013;10:225–232. doi: 10.4306/pi.2013.10.3.225. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Lewy A.J., Nurnberger J.I., Jr., Wehr T.A., Pack D., Becker L.E., Powell R.L., Newsome D.A. Supersensitivity to light: possible trait marker for manic-depressive illness. Am. J. Psychiatry. 1985;142:725–727. doi: 10.1176/ajp.142.6.725. [DOI] [PubMed] [Google Scholar]
- Li X., Bijur G.N., Jope R.S. Glycogen synthase kinase-3beta, mood stabilizers, and neuroprotection. Bipolar Disord. 2002;4:137–144. doi: 10.1034/j.1399-5618.2002.40201.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Maciukiewicz M., Dmitrzak-Weglarz M., Pawlak J., Leszczynska-Rodziewicz A., Zaremba D., Skibinska M., Hauser J. Analysis of genetic association and epistasis interactions between circadian clock genes and symptom dimensions of bipolar affective disorder. Chronobiol. Int. 2014;31:770–778. doi: 10.3109/07420528.2014.899244. [DOI] [PubMed] [Google Scholar]
- McClung C.A. Circadian genes, rhythms and the biology of mood disorders. Pharmacol. Ther. 2007;114:222–232. doi: 10.1016/j.pharmthera.2007.02.003. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Novakova M., Prasko J., Latalova K., Sladek M., Sumova A. The circadian system of patients with bipolar disorder differs in episodes of mania and depression. Bipolar Disord. 2015;17:303–314. doi: 10.1111/bdi.12270. [DOI] [PubMed] [Google Scholar]
- Nurnberger J.I., Jr., Adkins S., Lahiri D.K., Mayeda A., Hu K., Lewy A., Miller A., Bowman E.S., Miller M.J., Rau L., Smiley C., Davis-Singh D. Melatonin suppression by light in euthymic bipolar and unipolar patients. Arch. Gen. Psychiatry. 2000;57:572–579. doi: 10.1001/archpsyc.57.6.572. [DOI] [PubMed] [Google Scholar]
- Reppert S.M., Weaver D.R. Coordination of circadian timing in mammals. Nature. 2002;418:935–941. doi: 10.1038/nature00965. [DOI] [PubMed] [Google Scholar]
- Rock P., Goodwin G., Harmer C., Wulff K. Daily rest-activity patterns in the bipolar phenotype: a controlled actigraphy study. Chronobiol. Int. 2014;31:290–296. doi: 10.3109/07420528.2013.843542. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Salvatore P., Ghidini S., Zita G., De Panfilis C., Lambertino S., Maggini C., Baldessarini R.J. Circadian activity rhythm abnormalities in ill and recovered bipolar I disorder patients. Bipolar Disord. 2008;10:256–265. doi: 10.1111/j.1399-5618.2007.00505.x. [DOI] [PubMed] [Google Scholar]
- Saper C.B., Scammell T.E., Lu J. Hypothalamic regulation of sleep and circadian rhythms. Nature. 2005;437:1257–1263. doi: 10.1038/nature04284. [DOI] [PubMed] [Google Scholar]
- Schibler U., Sassone-Corsi P. A web of circadian pacemakers. Cell. 2002;111:919–922. doi: 10.1016/s0092-8674(02)01225-4. [DOI] [PubMed] [Google Scholar]
- Sit D., Wisner K.L., Hanusa B.H., Stull S., Terman M. Light therapy for bipolar disorder: a case series in women. Bipolar Disord. 2007;9:918–927. doi: 10.1111/j.1399-5618.2007.00451.x. [DOI] [PubMed] [Google Scholar]
- Son G.H., Chung S., Choe H.K., Kim H.D., Baik S.M., Lee H., Lee H.W., Choi S., Sun W., Kim H., Cho S., Lee K.H., Kim K. Adrenal peripheral clock controls the autonomous circadian rhythm of glucocorticoid by causing rhythmic steroid production. Proc. Natl. Acad. Sci. U. S. A. 2008;105:20970–20975. doi: 10.1073/pnas.0806962106. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Spearing M.K., Post R.M., Leverich G.S., Brandt D., Nolen W. Modification of the clinical global impressions (CGI) scale for use in bipolar illness (BP): the CGI-BP. Psychiatry Res. 1997;73:159–171. doi: 10.1016/s0165-1781(97)00123-6. [DOI] [PubMed] [Google Scholar]
- Turvey C.L., Coryell W.H., Solomon D.A., Leon A.C., Endicott J., Keller M.B., Akiskal H. Long-term prognosis of bipolar I disorder. Acta Psychiatr. Scand. 1999;99:110–119. doi: 10.1111/j.1600-0447.1999.tb07208.x. [DOI] [PubMed] [Google Scholar]
- Wehr T.A., Sack D.A., Duncan W.C., Mendelson W.B., Rosenthal N.E., Gillin J.C., Goodwin F.K. Sleep and circadian rhythms in affective patients isolated from external time cues. Psychiatry Res. 1985;15:327–339. doi: 10.1016/0165-1781(85)90070-8. [DOI] [PubMed] [Google Scholar]
- Wirz-Justice A. Biological rhythm disturbances in mood disorders. Int. Clin. Psychopharmacol. 2006;21(Suppl 1):S11–S15. doi: 10.1097/01.yic.0000195660.37267.cf. [DOI] [PubMed] [Google Scholar]
- Wood J., Birmaher B., Axelson D., Ehmann M., Kalas C., Monk K., Turkin S., Kupfer D.J., Brent D., Monk T.H., Nimgainkar V.L. Replicable differences in preferred circadian phase between bipolar disorder patients and control individuals. Psychiatry Res. 2009;166:201–209. doi: 10.1016/j.psychres.2008.03.003. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Yoo S., Kim Y., Noh J., Oh K., Kim C., Namkoong K., Chae J., Lee G., Jeon S., Min K. Validity of Korean version of the mini-international neuropsychiatric interview. Anxiety Mood. 2006;2:50–55. [Google Scholar]
- Young R.C., Biggs J.T., Ziegler V.E., Meyer D.A. A rating scale for mania: reliability, validity and sensitivity. Br. J. Psychiatry. 1978;133:429–435. doi: 10.1192/bjp.133.5.429. [DOI] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Supplementary Materials
Supplementary material.