Abstract
There is increasing recognition of the value added by integrating traditionally separate efforts to protect and promote worker safety and health. This paper presents an innovative conceptual model to guide research on determinants of worker safety and health and to inform the design, implementation and evaluation of integrated approaches to promoting and protecting worker health. This model is rooted in multiple theories and the premise that the conditions of work are important determinants of individual safety and health outcomes and behaviors, and outcomes important to enterprises such as absence and turnover. Integrated policies, programs and practices simultaneously address multiple conditions of work, including the physical work environment and the organization of work (e.g., psychosocial factors, job tasks and demands). Findings from two recent studies conducted in Boston and Minnesota (2009–2015) illustrate the application of this model to guide social epidemiological research. This paper focuses particular attention on the relationships of the conditions of work to worker health-related behaviors, musculoskeletal symptoms, and occupational injury; and to the design of integrated interventions in response to specific settings and conditions of work of small and medium size manufacturing businesses, based on a systematic assessment of priorities, needs, and resources within an organization. This model provides an organizing framework for both research and practice by specifying the causal pathways through which work may influence health outcomes, and for designing and testing interventions to improve worker safety and health that are meaningful for workers and employers, and responsive to that setting’s conditions of work.
Keywords: worker safety, occupational health and safety, health promotion, conceptual model, workplace health
INTRODUCTION
There is a paradigm shift underway in protection and promotion of worker health. Leading health organizations have recommended better integration of the traditionally separate efforts to address occupational safety and health, and worksite programs and policies intended to reduce chronic disease risk through worksite-based health promotion (Carnethon et al., 2009; European Network for Workplace Health Promotion, 1997; Hymel et al., 2011; Institute of Medicine Committee to Assess Worksite Preventive Health Program Needs for NASA Employees, 2005; International Association for Worksite Health Promotion (IAWHP), 2012; World Health Organization, 1997, 1999). Vanguard employers are demonstrating how this approach works in practice (Anderson and Stoltzfus, 2001; Dell Computer Corporation, 2014; Isaac and Flynn, 2001; Roberts, 2009; van de Ven; Whitehead, 2001). The concept of integration of protection and promotion efforts is not new: it was advanced several decades ago in multiple reports (DeJoy and Southern, 1993; Sorensen et al., 1995; Walsh et al., 1991). The recent trend toward adoption of this approach underscores the need for defining best practices and processes to ensure optimal results (Carnethon et al., 2009; Hammer and Sauter, 2013; Schulte and Vainio, 2010; Sorensen et al., 2011a).
These efforts have been bolstered by the National Institute for Occupational Safety and Health (NIOSH) through its Total Worker Health® (TWH) Initiative, (Schill and Chosewood, 2013, 2016) which has facilitated a broadening dialogue among researchers, practitioners, business leaders and organized labor representatives about testing, implementing and disseminating integrated approaches to health protection and health promotion. Attention to this emerging field of research was highlighted in a recent workshop co-sponsored by the National Institutes of Health (NIH) and NIOSH, which reviewed evidence and provided recommendations for research aimed at better understanding the effectiveness of integrated interventions (Bradley et al., 2016). This work builds on growing evidence about the potential benefits of integrated approaches for improvements in health behaviors (Bertera, 1990, 1993; Elliot et al., 2007; Maes et al., 1998; Okechukwu et al., 2009; Olson et al., 2009; Sorensen et al., 2005; Sorensen et al., 2007; Sorensen et al., 1998; Sorensen et al., 2002); enhanced rates of employee participation in programs (Hunt et al., 2005); potential reductions in pain, occupational injury and disability rates (Hlobil et al., 2007; Pronk et al., 2012; Robertson et al., 2013; Shaw et al., 2006; Shaw et al., 2003; Tsutsumi et al., 2009); strengthened health and safety programs (Goetzel et al., 2001; LaMontagne et al., 2004); potentially reduced costs (Goetzel et al., 2001); and support for market performance of companies (Fabius et al., 2016; Malan et al., 2009). These findings are supported by multiple reviews of integrated interventions (Anger et al., 2015; Cherniack, 2013; Cooklin et al., in press; Goetzel, 2012; Institute of Medicine Committee to Assess Worksite Preventive Health Program Needs for NASA Employees, 2005; National Institute for Occupational Safety and Health, 2012; Pronk, 2013; Sorensen et al., 2011a), although a recent systematic review concluded that while integrated interventions may improve health behaviors, there remains a significant need for further evidence on their impact on injuries and overall quality of life (Feltner et al., 2016).
Despite growing evidence, this field of inquiry is still in its infancy, needing further evaluation of the effectiveness of this approach. A common conceptual model can structure intervention research to elucidate the pathways through which occupational factors influence safety and chronic disease risk. Thus, a conceptual model is useful in making explicit the underlying assumptions of integrated interventions. The purpose of this manuscript is to present a conceptual model for worker health embedded within the work environment with a focus on the conditions of work, and to illustrate its application to both social epidemiological and intervention research.
METHODS
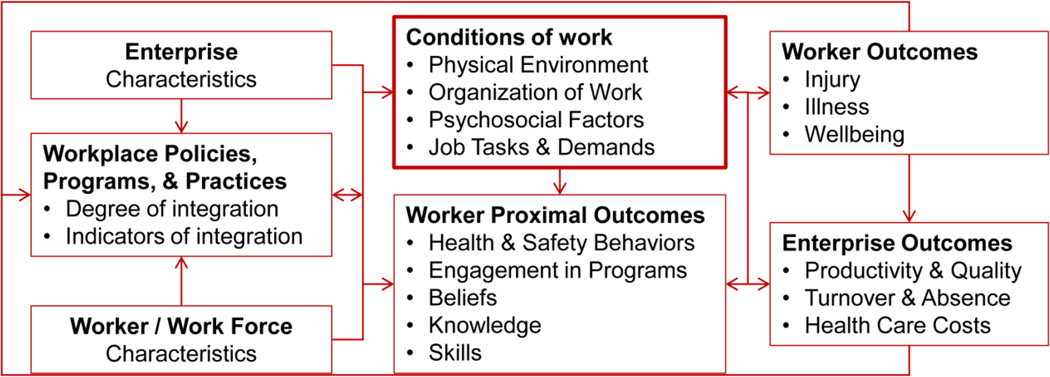
This conceptual model was developed by the Center for Work, Health and Well-being at the Harvard T.H. Chan School of Public Health, a Center for Excellence within NIOSH’s TWH Program. Based on the Center’s previous research and to guide future research, investigators developed and used this conceptual model to specify the causal pathways through which integrated policies, programs and practices are expected to influence worker safety and health outcomes (See Figure 1). The figure represents the evolution of this model based on revisions informed by the Center’s ongoing research. The research was approved by the Harvard Chan School’s Institutional Review Board.
Figure 1.
Conceptual model for integrated approaches to the protection and promotion of worker health and safety. Studies conducted in Boston and Minnesota (2009–2015).
Conceptual model for integrated approaches to protection and promotion of worker health
Our conceptual model is based on the premise that addressing multiple pathways in an integrated manner within the conditions of work will contribute to greater improvements in health outcomes than addressing each pathway separately. Policies, programs and practices may concurrently operate through many pathways affecting the conditions of work, including the physical work environment and the organization of work. Conditions of work are centrally located in the model as determinants of health and safety outcomes, also mediating the effects on health behaviors. Conditions of work are themselves influenced by enterprise and workforce characteristics, which are also likely to affect implementation of policies, programs and practices. These integrated policies, programs, and practices may contribute to improvements in enterprise outcomes such as turnover and health care costs. It is important to recognize, in addition, that these relationships occur within the context of labor market and economic trends, legal and political forces, and social mores, norms and influences.
Our conceptual model represents diverse theoretical perspectives, including the social ecological model (McLeroy et al., 1988; Stokols, 1996), social contextual model of health behavior change (Sorensen et al., 2004; Sorensen et al., 2003), hierarchy of controls (Levy et al., 2006; Office of Technology Assessment, 1985; Roelofs et al., 2003), organizational ergonomics (McLeroy et al., 1988; Stokols, 1996), participatory frameworks (Community-based participatory research for health: From process to outcomes, 2008; Punnett et al., 2009; Rivilis et al., 2008), job strain (Karasek, 1998; Karasek and Theorell, 1990), and socio-technical systems theory (Cooper and Foster, 1971; Murphy et al., 2014; Sauter et al., 2002). These theoretical foundations underscore the complex interplay of factors involving individual workers and the immediate work environment, characteristics of the larger contexts in which both the worker and the worksite are embedded, and proximal outcomes, such as individual health and safety behaviors and related factors of self-efficacy and risk perceptions that support improvements in these behaviors (Bandura, 1977; Walsh et al., 1991). Examples of feedback pathways are included in Figure 1, which underscore the complexity of the system and interrelationships across multiple dimensions. Each of the model’s components is presented below,.
Indicators of integrated workplace policies, programs and practices
Optimally, an integrated approach extends beyond simple summation of health protection and promotion to reflect a workplace culture that supports and protects worker safety, health and wellbeing. We consider four indicators of integration: (1) leadership commitment, (2) coordinated efforts, (3) supportive organizational policies and practices, and (4) comprehensive program content (Sorensen et al., 2013). We have operationalized these indicators in a measure of integrated approaches, which was validated in a limited number of settings. (See Williams et al for details on the measure; (Williams et al., 2015; Williams et al., 2016). We conceptualize implementation as operating on a continuum, recognizing that organizations may implement change in varying sequences, and may respond differently by industry sector, size of workplace, and extent of leadership and labor engagement (D. L. McLellan et al., 2015). These indicators include, first, organizational leadership and commitment, a necessary foundation for an integrated approach, reflecting the key role top management plays in articulating the vision for worker and worksite health and ensuring availability of resources (human, financial, physical) (Centers for Disease Control and Prevention, 2011; Institute of Medicine Committee to Assess Worksite Preventive Health Program Needs for NASA Employees, 2005). Second, rather than functioning independently, coordination among health protection, worksite health promotion and other workplace functions is needed to optimize benefits for worker safety and health (Institute of Medicine Committee to Assess Worksite Preventive Health Program Needs for NASA Employees, 2005; National Institute for Occupational Safety and Health, 2012). This indicator, for example, is measured by items that assess coordinated decision-making across departments; processes to coordinate interdepartmental budgets; and inclusion of both policies about the work environment and organization as well as programs for individual workers. Third, supportive organizational policies and practices can provide operational supports for worker safety and health. These include participatory approaches, which may take advantage of existing mechanisms for involving workers and managers in decision-making and planning concurrently for both health protection and promotion (Institute of Medicine Committee to Assess Worksite Preventive Health Program Needs for NASA Employees, 2005; McLellan et al., 2012). To ensure accountability, responsibility for an integrated approach can be built into job descriptions and performance metrics; skills for implementing this approach can be incorporated into training and capacity building plans (Kruse, 2009). Benefits and incentives may be instituted that protect and promote worker health and well-being (Blumenthal, 2006; Boden et al., 2012), and include attention to improvements in salary and overall benefits, which may present a barrier for some employers (Lax, 2016). Workplace programs, policies and practices can be monitored and evaluated for both occupational health exposures and health-related behaviors and the relationships of exposures and behaviors to health outcomes (Boden et al., 2012; Institute of Medicine Committee to Assess Worksite Preventive Health Program Needs for NASA Employees, 2005). Finally, the effectiveness of health protection and promotion messages for workers may be enhanced through comprehensive program content and coordinated messages that acknowledge and describe additive and sometimes synergistic effects of exposures to worksite hazards and individual health behaviors, such as the importance of controlling exposures to respiratory hazards at work while encouraging tobacco use cessation.
Conditions of work
We hypothesize and report below that these integrated policies, programs, and practices will influence worker health outcomes through several pathways based primarily within the conditions of work. First, integrated policies and practices have a direct impact on the physical work environment, including on potential exposures on the job. For example, policies may impact physical demands related to biomechanical sources of strain, or may include purchasing policies that influence selection of safer versus more hazardous chemicals or equipment used in some work processes. The work environment may also support healthy behaviors among workers, for example, through worksite tobacco control policies or availability of healthy foods in cafeterias and vending machines. Second, the organization ofwork has been consistently shown to influence worker health and safety outcomes (Amick et al., 2003; Eriksen et al., 2004; Lipscomb et al., 2004; Lipscomb et al., 2002; Tullar et al., 2010) as well as health behaviors (Albertsen et al., 2006; Brunner et al., 2007; Caruso et al., 2004; Choi et al., 2010; Jones et al., 2007; Kouvonen et al., 2006; Trinkoff et al., 2001). Psychosocial factors, part of the organization of work, broadly include job strain, psychological demands and control (Karasek and Theorell, 1990), rewards (Siegrist, 1996), social support, harassment and discrimination (National Institute for Occupational Safety and Health, 2008). For example, supervisor and co-worker support and social norms that support health and safety behaviors are associated with improved health behaviors (Belkic and Nedic, 2007; Choi et al., 2010; Hannerz et al., 2004; Kouvonen et al., 2007; Nishitani and Sakakibara, 2010; Siegrist and Rodel, 2006) and reduced risk of musculoskeletal disorders (MSDs) (Bongers et al., 2002; Macfarlane et al., 2009; Nahit et al., 2003). Job tasks and demands, including the extent to which high physical exertion is a requirement of the job, work hours and shift, and the pace of work, have been shown consistently to influence a range of safety and health outcomes (Heaney and Fujishiro, 2005; Karsh et al., 2005; Lipscomb et al., 2002; Trinkoff et al., 2001). Health and safety climate—workers’ shared perceptions about organization practices —is associated with work satisfaction, injury and accident risk, and enterprise outcomes (Beus et al., 2010; Christian et al., 2009; Hemingway and Smith, 1999; Hofmann and Mark, 2006; Huang et al., 2006; Law et al., 2011; Probst et al., 2008; Sparer et al., under re-review; Zohar and Polachek, 2014). Changes in the conditions of work may ultimately contribute to transformational change in the organization toward a culture of worker safety, health and wellbeing (Sorensen et al., 2013), by which we mean one that anticipates and mitigates potential workplace health risks, encourages worker identification and reporting of health and safety concerns without fear of reprisal, and provides health supportive programs, policies, and practices.
Enterprise characteristics
Enterprise characteristics, such as industry sector and size, influence the conditions of work and the types of exposures workers face, and are likely to play significant roles in the uptake of integrated approaches (Harris et al., 2014; Institute of Medicine and Committee on the Health and Safety Needs of Older Workers, 2004; Krieger, 2010). Employers also set pay scales and work hours, further shaping the resources and health outcomes workers experience (Baron et al., 2014; Krieger et al., 2008).
Work force/ worker characteristics
It is also important to understand, for example, the changing needs of an aging workforce, the potentially differing work-family intersections for men compared to women workers, and potential vulnerabilities of immigrant workers compared to US-born workers. Similarly, young workers are twice as likely as older workers to be injured on the job (Estes et al., 2010), and often lack sufficient training in workplace safety practices and legal rights on the job (Rohlman et al., 2013).
Outcomes
Both individual- and organization-level outcomes are included in the model. At the individual level, proximal outcomes include participation in programs, as well as health and safety behaviors that are associated with changes in risk of poor health and safety outcomes. The conditions of work contribute to health-related behaviors (e.g., job stress is associated with increased tobacco and alcohol use (Hammer and Sauter, 2013)) as well as increased risk of illness and injury. At the organizational level, enterprise outcomes can include financial and economic outcomes, such as absenteeism, turnover, employee expenditures on health care, and intervention return on investment (ROI). Given that worksite interventions require employer support and commitment of resources, consideration of enterprise outcomes can help make the business case for integrated interventions.
RESULTS
Findings from two recent studies illustrate the application of this model to social epidemiological and intervention research.
Understanding determinants of health and safety outcomes
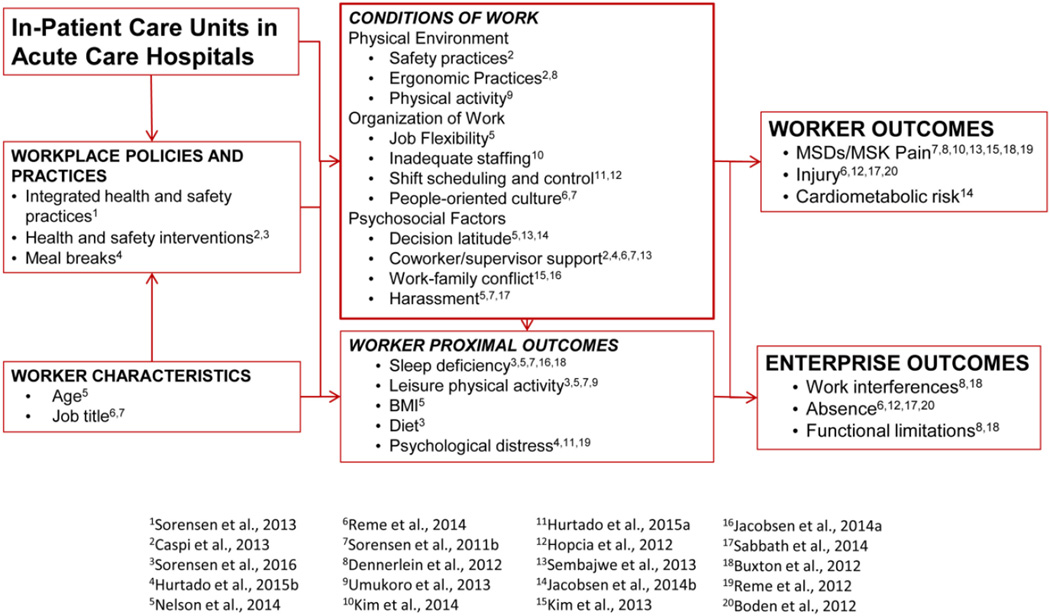
In a study of hospital patient care workers, we examined data from three surveys of patient care workers along with an integrated administrative database linking employees’ administrative records on outcomes such as injury with their survey responses. Three cross-cutting themes emerged from this body of work, with important implications for interventions (Figure 2).
Figure 2.
Application of the conceptual model. Studies conducted in Boston and Minnesota (2012–2015).
Theme 1: Injury, musculoskeletal pain, and health behaviors share diverse determinants within the work environment and vary by socioeconomic status of workers
Injury
Injury rates varied by both structural and social factors within work units. Compared to nurses, aides were more likely to have injuries, both those that required days away and those that did not result in lost days (Boden et al., 2012; Reme et al., 2014). We documented differences in injury rates by patient care unit, with higher rates in the operating room and emergency department, and lower rates in step-down and pediatric settings (Boden et al., 2012). We also found that several dimensions of the psychosocial work environment were associated with injury risk, including workplace harassment (both on an individual and unit level) (Sabbath et al., 2014) and supervisor support (Tveito et al., 2014), as well as organizational policies and practices (Reme et al., 2014; Tveito et al., 2014).
Pain
Worker perceptions of the overall work environment—particularly poor perceptions of organizational practices to reduce ergonomic strain (Dennerlein et al., 2012) and perceived staffing inadequacy (Kim et al., 2014) —were associated with increased risk of pain. The relationship between perceived inadequate staffing and pain was attenuated by work-related psychosocial factors, including stress and supervisor support, suggesting that these psychosocial factors may play an important role in this relationship.
Common Pathways to Health Behaviors, Pain, and Injury
We found that workplace culture reflected in policies and practices, such as effective ergonomic and other safety practices, jointly predicted lower back pain, improved sleep, and to a lesser extent, physical activity (Sorensen et al., 2011b). Although inadequate sleep and physical inactivity were associated, unexpectedly we did not find an association between these behaviors and low back pain.
Theme 2: The psychosocial work environment shapes safety and health behaviors and health outcomes
Supervisor Support
Supervisor support was associated with a range of health outcomes (Caspi et al., 2013; Hurtado et al., 2015b; Reme et al., 2014; Sembajwe et al., 2013; Sorensen et al., 2011b). We found lower injury rates in units where workers reported better supervisor support and more favorable organizational policies and practices (Tveito et al., 2014).
Work-family Conflict and Job Flexibility
Nurses working on units with more shift flexibility had relatively less depression and anxiety (Hurtado et al., 2015a). Higher levels of work-family conflict were also significantly associated with sleep deficiency in the short term and nearly two years later (HB Jacobsen et al., 2014), and with multiple types of musculoskeletal pain (Kim et al., 2013).
Harassment at Work
Being sworn at, screamed at, and receiving hostile or offensive gestures from patients, coworkers, or supervisors were associated with increased risk of chronic injury (Sabbath et al., 2014). Harassed workers were also more likely to be obese and have low levels of physical activity (Nelson et al., 2014; Sorensen et al., 2011b).
Decision Latitude and Job Demands
We found that higher job demands were associated with musculoskeletal pain (Sembajwe et al., 2013), that low decision latitude was associated with obesity (Nelson et al., 2014), and that job strain was associated with sleep deficiency and cardiometabolic risk (H.B. Jacobsen et al., 2014).
Individual and Organization-level Exposures
We found both contextual and compositional group-level exposures contribute to individual workers’ outcomes. For example, shift flexibility at the unit level translated to lower depression and anxiety at the individual level (Hurtado et al., 2016), and high levels of ambient harassment (regardless of individual harassment) were associated with greater injury risk (Sabbath et al., 2014).
Theme 3: Health behaviors are partially rooted in conditions of work, suggesting that conditions of work need to be addressed if health-related behaviors are to improve
Physical activity
Workers with low decision latitude and low job flexibility were less likely to meet guidelines for adequate physical activity (Nelson et al., 2014).
Sleep
We found especially strong evidence that sleep and sleep inadequacy were predicted by adverse conditions of work (Buxton et al., 2012; HB Jacobsen et al., 2014; H.B. Jacobsen et al., 2014; Nelson et al., 2014; Sorensen et al., 2011b). For example, sleep deficiency was associated with nearly all psychosocial exposures examined in Theme 2. Simultaneously, broader policies and practices within the work environment also predicted improved sleep, including people-oriented culture, ergonomic practices, and safety practices (Sorensen et al., 2011b).
Collectively, these findings underscore the need for a comprehensive approach to safety and health interventions, consistent with our integrated model.
Intervention design: A case study in small- to medium-sized businesses
We also used our conceptual model to design an integrated intervention in response to specific settings and conditions of work, based on a systematic assessment approach conducted within organizations (Pronk et al., 2016). We tested the feasibility of the intervention in three small- and medium-sized businesses (SMBs) in manufacturing in Minnesota.
As part of planning, we used the conceptual model to guide assessment of employee health indicators and the physical and organizational environment, and provided feedback on the assessments to the sites. Because back pain was prevalent, the intervention placed a high priority on reducing back pain and increasing safe movement at work and at home.
This program used four major strategies: (1) Worksite-wide events promoted changes in the conditions of work such as environmental supports for ergonomic and health promotion practices; for example, participating sites used technology to address ergonomic and physical hazards related to back pain, such as improved lifting or moving devices on factory floors and sit-to-stand devices in some office spaces. (2) A worksite-level intervention focused on consultation and training with mid-level and upper management and included committees comprised of those responsible for protecting and promoting worker health and safety. The management intervention was the primary intervention focus. (3) A learning collaborative convened company leaders, including the CEOs from the participating sites, to share their experiences with other executives (Pronk et al., 2015). (4) Although the intervention focused mostly on working conditions, telephone health coaching and web-based resources that included integrated messages on back pain and safe movement were available for employees as part of this comprehensive integrated program.
We identified factors critical to successful implementation of policies, programs and practices, including multi-level management support and articulation of that support throughout the enterprise; allocation of dedicated staff, budgets, and committees; collaborative organizational cultures that prioritized employee health and safety; existing organizational processes that could be leveraged for new approaches; and realistic implementation timelines to account for organizational changes (D. McLellan et al., 2015; Pember et al., 2015; Pronk et al., 2016). Results indicate that both employee-rated health culture and safety culture improved in two companies, self-reported back pain decreased in one company and remained the same in two; safety hazards were reduced in all companies; and organizational resources, as measured by the CDC Worksite Health Scorecard and related to organizational support, physical activity and nutrition, all improved across all companies (Pronk et al., 2016).
DISCUSSION
This model responds to the ongoing dialogue on the importance of a conceptual framework to guide research and intervention design related to worker health (Bradley et al., 2016; Punnett et al., 2009; Schulte and Vainio, 2010; Schulte et al., 2012). This conceptual model provides a framework for research and intervention by specifying how the conditions of work can shape worker safety and health. The model serves as a valuable and evidence-based guide for prioritizing research questions, framing a standard approach to interventions, and steering practical applications toward effective processes to protect and improve worker health. Specifying the pathways through which the intervention is intended to affect worker safety and health can clarify the priorities for both the intervention and evaluation. A conceptual model can also guide mediation analyses for testing specific pathways (Anger et al., 2015; MacKinnon, 2008).
This model highlights priorities for ongoing research that explores, for example, the extent to which integrated workplace policies, programs and practices determine safety and health outcomes; the ways in which these policies, programs and practices may shape physical and psychosocial work exposures; and the roles of worker and enterprise factors influencing these pathways. Research presented by other researchers further illustrates the applicability of this model. For example, Schulte and colleagues emphasized how shared pathways focusing on conditions of work could impact enterprise and worker outcomes such as occupational hazards and obesity. Although prior research has examined ways in which the conditions of work influence chronic disease and its behavioral antecedents (Johansson et al., 1991; Marchand, 2008) and risks associated with hazards on the job (Huang et al., 2003; Landsbergis et al., 2014), additional research is needed to examine the synergies and interactions in these relationships, as well as their associations with improved enterprise outcomes. In addition, few studies in this nascent field have successfully modified organizational factors; there is a significant need for systematic research directed at changes in the work organization (Lax, 2016). Responding to recommendations from a recent NIH-NIOSH workshop (Bradley et al., 2016), this model can also guide further development of measures to assess the effects of an integrated approach, inform the design and testing of future integrated approaches to worker health, and offer a framework for increased attention to organizational change, central to the TWH approach yet underrepresented within research findings reported to date (Lax, 2016; McLellan, 2016). Use of a common conceptual model offers a platform for bridging these diverse perspectives and suggests shared vocabularies for understanding the influences on worker health (Sorensen et al., 2004; Sorensen et al., 2003).
This model also informs translation from research to practice by outlining key components of effective implementation of TWH approaches. Although a growing array of guidelines and tools are available to support adoption of TWH approaches (Burton, 2010; Center for the Promotion of Health in the New England Workplace, 2013; International Labour Office, 2012; McLellan et al., 2012; Velazquez et al., 2010), implementation of these integrated policies, programs, and practices remains concentrated primarily among a select group of vanguard employers (Loeppke et al., 2015). There is an urgent need for effective dissemination of evidence-based best practices and resources to build capacity in worksites across size and sector to improve the conditions of work and transform the work organization, thus improving worker health. Our work has shown, however, that employers often turn first to providing programs for individual workers, rather than tackling system-level policies and practices, a tendency we have labeled “regression to the individual” (Cooklin A et al., 2013; D. L. McLellan et al., 2015; Sorensen et al., 2016). Effective implementation of TWH interventions requires that employers have the capacity to identify and modify features of the work organization that are a risk to worker health (DeJoy et al., 2010; Mellor and Webster, 2013). This conceptual model provides a framework for employers to identify, develop and implement interventions and strategies that will enable system-level changes in the conditions of work.
CONCLUSIONS
Traditionally, a focus on the conditions of work has been the domain of occupational safety and health; here, we aim to underscore the central role of the conditions of work, not only for classic occupational safety and health outcomes, but also for chronic disease risk. An increasing number of workplaces are adopting integrated approaches to worker health that should be carefully evaluated. We have proposed a conceptual model to guide this inquiry and to frame the focus on the conditions of work as central to building a culture of safety, health and wellbeing. This model further illustrates the potential for synergy in integrated approaches to worker health, offering opportunities for improvements in the conditions of work as well as for multiple worker health outcomes (Anger et al., 2015). Thus, this conceptual model may provide a valuable tool for future research aimed at testing the effectiveness of integrated approaches to worker health protection and health promotion, as well as a framework for translating research to practice.
HIGHLIGHTS.
Integrating health protection and promotion can benefit workers and employers.
Integrated efforts can improve the physical and organizational work environment.
Despite growing evidence, research on integrated approaches remains in its infancy.
A conceptual model can elucidate work-related pathways influencing worker health.
This model offers a tool to test the effectiveness of integrated approaches.
Acknowledgments
This work was supported by a grant from the National Institute for Occupational Safety and Health (U19 OH008861) for the Harvard T.H. Chan School of Public Health Center for Work, Health and Well-being and by a grant from the National Institutes of Health (K05 CA124415). The sponsors had no role or involvement in study design; in the collection, analysis and interpretation of data; in the writing of the report; or in the decision to submit the article for publication.
The authors would like to thank Steven Sauter for his input on the manuscript. We also appreciate the contributions of the co-investigators, staff and post-doctoral fellows in the Harvard T.H. Chan School of Public Health Center for Work, Health and Wellbeing, including Linnea Benson-Whelan, Leslie Boden, Orfeu Buxton, Alberto Caban-Martinez, Michael Grant, Dean Hashimoto, Karen Hopcia, Jeffrey Katz, Candace Nelson, Cassandra Okechukwu, Emily Sparer, Anne Stoddard, Julie Theron, Lorraine Wallace and Jessica Williams.
Footnotes
Publisher's Disclaimer: This is a PDF file of an unedited manuscript that has been accepted for publication. As a service to our customers we are providing this early version of the manuscript. The manuscript will undergo copyediting, typesetting, and review of the resulting proof before it is published in its final citable form. Please note that during the production process errors may be discovered which could affect the content, and all legal disclaimers that apply to the journal pertain.
Conflict of Interest Statement
The authors declare that there are no conflicts of interest.
References
- Albertsen K, Borg V, Oldenburg B. A systematic review of the impact of work environment on smoking cessation, relapse and amount smoked. Prev Med. 2006;43:291–305. doi: 10.1016/j.ypmed.2006.05.001. [DOI] [PubMed] [Google Scholar]
- Amick BC, 3rd, Robertson MM, DeRango K, Bazzani L, Moore A, Rooney T, Harrist R. Effect of office ergonomics intervention on reducing musculoskeletal symptoms. Spine. 2003;28:2706–2711. doi: 10.1097/01.BRS.0000099740.87791.F7. [DOI] [PubMed] [Google Scholar]
- Anderson MA, Stoltzfus JA. The 3M corporate experience: Health as a business strategy. Am J Health Promot. 2001;15:371–373. [PubMed] [Google Scholar]
- Anger WK, Elliot DL, Bodner T, Olson R, Rohlman DS, Truxillo DM, Kuehl KS, Hammer L, Montgomery D. Effectiveness of Total Worker Health interventions. J Occup Health Psychol. 2015;20:226–247. doi: 10.1037/a0038340. [DOI] [PubMed] [Google Scholar]
- Bandura A. Self-efficacy: Toward a unifying theory of behavioral change. Psychol Rev. 1977;84:191–215. doi: 10.1037//0033-295x.84.2.191. [DOI] [PubMed] [Google Scholar]
- Baron SL, Beard S, Davis LK, Delp L, Forst L, Kidd-Taylor A, Liebman AK, Linnan L, Punnett L, et al. Promoting integrated approaches to reducing health inequities among low-income workers: applying a social ecological framework. Am J Ind Med. 2014;57:539–556. doi: 10.1002/ajim.22174. PMC3843946. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Belkic K, Nedic O. Workplace stressors and lifestyle-related cancer risk factors among female physicians: assessment using the Occupational Stress Index. J Occup Health. 2007;49:61–71. doi: 10.1539/joh.49.61. [DOI] [PubMed] [Google Scholar]
- Bertera RL. The effects of workplace health promotion on absenteeism and employment costs in a large industrial population. Am J Public Health. 1990;80:1101–1105. doi: 10.2105/ajph.80.9.1101. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Bertera RL. Behavioral risk factor and illness day changes with workplace health promotion: two-year results. Am J Health Promot. 1993;7:365–373. doi: 10.4278/0890-1171-7.5.365. [DOI] [PubMed] [Google Scholar]
- Beus JM, SC P, Bergman ME, Arthur W., Jr Safety climate and injuries: an examination of theoretical and empirical relationships. J Appl Psychol. 2010;95:713. doi: 10.1037/a0019164. [DOI] [PubMed] [Google Scholar]
- Blumenthal D. Employer-sponsored health insurance in the United States--origins and implications. N Engl J Med. 2006;355:82–88. doi: 10.1056/NEJMhpr060703. [DOI] [PubMed] [Google Scholar]
- Boden LI, Sembajwe G, Tveito TH, Hashimoto D, Hopcia K, Kenwood C, Stoddard AM, Sorensen G. Occupational injuries among nurses and aides in a hospital setting. Am J Ind Med. 2012;55:117–126. doi: 10.1002/ajim.21018. [DOI] [PubMed] [Google Scholar]
- Bongers PM, Kremer AM, ter Laak J. Are psychosocial factors, risk factors for symptoms and signs of the shoulder, elbow, or hand/wrist?: A review of the epidemiological literature. Am J Ind Med. 2002;41:315–342. doi: 10.1002/ajim.10050. [DOI] [PubMed] [Google Scholar]
- Bradley CJ, Grossman DC, Hubbard RA, Ortega AN, Curry SJ. Integrated Interventions for Improving Total Worker Health: A Panel Report From the National Institutes of Health Pathways to Prevention Workshop: Total Worker Health-What's Work Got to Do With It? Ann Intern Med. 2016 doi: 10.7326/M16-0740. [DOI] [PubMed] [Google Scholar]
- Brunner EJ, Chandola T, Marmot MG. Prospective effect of job strain on general and central obesity in the Whitehall II Study. Am J Epidemiol. 2007;165:828–837. doi: 10.1093/aje/kwk058. [DOI] [PubMed] [Google Scholar]
- Burton J. WHO Healthy Workplace Framework and Model: Background and Supporting Literature and Practices. 2010 http://apps.who.int/iris/bitstream/10665/113144/1/9789241500241_eng.pdf?ua=1.
- Buxton OM, Hopcia K, Sembajwe G, Porter JH, Dennerlein JT, Kenwood C, Stoddard AM, Hashimoto D, Sorensen G. Relationship of sleep deficiency to perceived pain and functional limitations in hospital patient care workers. J Occup Environ Med. 2012;54:851–858. doi: 10.1097/JOM.0b013e31824e6913. PMCID3720240. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Carnethon M, Whitsel LP, Franklin BA, Kris-Etherton P, Milani R, Pratt CA, Wagner GR. Worksite wellness programs for cardiovascular disease prevention: a policy statement from the American Heart Association. Circulation. 2009;120:1725–1741. doi: 10.1161/CIRCULATIONAHA.109.192653. [DOI] [PubMed] [Google Scholar]
- Caruso C, Hitchcock E, Dick R, Russo J, Schmitt J. U.S. Department of Health and Human Services, Public Health Service, Centers for Disease Control and Prevention, National Institute for Occupational Safety and Health, DHHS (NIOSH); 2004. Overtime and extended work shifts: recent findings on illnesses injuries, and health behaviors; pp. 1–38. http://www.cdc.gov/niosh/docs/2004-143/default.html. [Google Scholar]
- Caspi CE, Dennerlein JT, Kenwood CAS, Hopcia K, Hashimoto D, Sorensen G. Results of a pilot intervention to improve health and safety for healthcare workers. J Occup Environ Med. 2013;55:1449–1455. doi: 10.1097/JOM.0b013e3182a7e65a. PMCID 3858503. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Center for the Promotion of Health in the New England Workplace. Intervention Design and Analysis Scorecard (IDEAS) CPH-NEW Intervention Planning Tool Facilitator’s Guide. Lowell: University of Massachusetts; 2013. http://www.uml.edu/docs/FGuide_Mar3_Website_tcm18-102071.pdf. [Google Scholar]
- Centers for Disease Control and Prevention. Workplace Health Program Development Checklist. 2011 www.cdc.gov/workplacehealthpromotion/pdfs/WHPChecklist.pdf.
- Cherniack M. Integrated health programs, health outcomes, and return on investment: measuring workplace health promotion and integrated program effectiveness. J Occup Environ Med. 2013;55:S38–S45. doi: 10.1097/JOM.0000000000000044. [DOI] [PubMed] [Google Scholar]
- Choi B, Schnall PL, Yang H, Dobson M, Landsbergis P, Israel L, Karasek R, Baker D. Psychosocial working conditions and active leisure-time physical activity in middle-aged us workers. Int J Occup Med Environ Health. 2010:1–15. doi: 10.2478/v10001-010-0029-0. [DOI] [PubMed] [Google Scholar]
- Christian MS, Bradley JC, Wallace JC, Burke MJ. Workplace safety: a meta-analysis of the roles of person and situation factors. J Appl Psychol. 2009;94:1103–1127. doi: 10.1037/a0016172. [DOI] [PubMed] [Google Scholar]
- Community-based participatory research for health: From process to outcomes. 2nd. San Francisco, CA: Jossey Bass; 2008. [Google Scholar]
- Cooklin A, Husser E, Joss NBO. Research report 1213-088-R1C. Melbourne, Australia: Monash Unversity; 2013. Integrated approaches to worker health, safety and well-being. [Google Scholar]
- Cooklin A, Joss N, Dupre-Husser E, Oldenburg B. Integrated approaches to occupational health and safety and health promotion: A systematic review. Am J Health Promot. doi: 10.4278/ajhp.141027-LIT-542. in press. [DOI] [PubMed] [Google Scholar]
- Cooper R, Foster M. Sociotechical systems. Am Psychol. 1971;26:467–474. [Google Scholar]
- DeJoy D, Southern D. An integrative perspective on worksite health promotion. J Med. 1993;35:1221–1230. [PubMed] [Google Scholar]
- DeJoy D, Wilson MG, Vandenberg RJ, McGrath-Higgins AL, Griffin-Blake CS. Assessing the impact of healthy work organization intervention. J Occup Organ Psychol. 2010;83:139–165. [Google Scholar]
- Dell Computer Corporation. Dell 2012 Corporate Responsibility Report. 2014 Available at http://i.dell.com/sites/content/corporate/corp-comm/en/Documents/dell-fy12-cr-report.pdf. [Google Scholar]
- Dennerlein JT, Hopcia K, Sembajwe G, Kenwood C, Stoddard AM, Tveito TH, Hashimoto DM, Sorensen G. Ergonomic practices within patient care units are associated with musculoskeletal pain and limitations. Am J Ind Med. 2012;55:107–116. doi: 10.1002/ajim.21036. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Elliot DL, Goldberg L, Kuehl KS, Moe EL, Breger RK, Pickering MA. The PHLAME (Promoting Healthy Lifestyles: Alternative Models' Effects) firefighter study: outcomes of two models of behavior change. J Occup Environ Med. 2007;49:204–213. doi: 10.1097/JOM.0b013e3180329a8d. [DOI] [PubMed] [Google Scholar]
- Eriksen W, Bruusgaard D, Knardahl S. Work factors as predictors of intense or disabling low back pain; a prospective study of nurses' aides. Occup Environ Med. 2004;61:398–404. doi: 10.1136/oem.2003.008482. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Estes CR, Jackson LL, Castillo DN. Occupational Injuries and Deaths Among Younger Workers - Unites States - 1998–2007. MMWR. Centers for Disease Control. 2010:449. www.cdc.gov/mmwr/preview/mmwrhtml/mm5915a2.htm. [PubMed]
- European Network for Workplace Health Promotion. The Luxembourg declaration on workplace health promotion in the European Union, European Network for Workplace Health Promotion Meeting. Luxembourg: European Network for Workplace Health Promotion; 1997. [Google Scholar]
- Fabius R, Loeppke RR, Hohn T, Fabius D, Eisenberg B, Konicki DL, Larson P. Tracking the Market Performance of Companies That Integrate a Culture of Health and Safety: An Assessment of Corporate Health Achievement Award Applicants. J Occup Environ Med. 2016;58:3–8. doi: 10.1097/JOM.0000000000000638. [DOI] [PubMed] [Google Scholar]
- Feltner C, Peterson K, Weber RP, Cluff L, Coker-Schwimmer E, Viswanathan M, Lohr KN. The Effectiveness of Total Worker Health Interventions: A Systematic Review for a National Institutes of Health Pathways to Prevention Workshop. Ann Intern Med. 2016 doi: 10.7326/M16-0626. [DOI] [PubMed] [Google Scholar]
- Goetzel RZ. Washington, DC: 2012. [Accessed November 2012]. Examining the value of integrating occupational health and safety and health promotion programs in the workplace, NIOSH 2012, Research Compendium: The NIOSH Total Worker Health Program: Seminal research papers 2012. Department of Health and Human Services, Public Health Service, Centers for Disease Control and Prevention, National Institute for Occupational Safety and Health, DHHS (NIOSH) Publication No. 2012-146. Available at http://www.cdc.gov/niosh/docs/2012-146/ [Google Scholar]
- Goetzel RZ, Guindon AM, Turshen IJ, Ozminkowski RJ. Health and productivity management: establishing key performance measures, benchmarks, and best practices. J Occup Environ Med. 2001;43:10–17. doi: 10.1097/00043764-200101000-00003. [DOI] [PubMed] [Google Scholar]
- Hammer LB, Sauter S. Total worker health and work-life stress. J Occup Environ Med. 2013;55:S25–S29. doi: 10.1097/JOM.0000000000000043. [DOI] [PubMed] [Google Scholar]
- Hannerz H, Albertsen K, Nielsen ML, Tuchsen F, Burr H. Occupational factors and 5-year weight change among men in a danish national cohort. Health Psychol. 2004;23:283–288. doi: 10.1037/0278-6133.23.3.283. [DOI] [PubMed] [Google Scholar]
- Harris JR, Hannon PA, Beresford SA, Linnan LA, McLellan DL. Health promotion in smaller workplaces in the United States. Annu Rev Public Health. 2014;35:327–342. doi: 10.1146/annurev-publhealth-032013-182416. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Heaney CA, Fujishiro K. Interventions to prevent work-related musculoskeletal disorders: Psychosocial characteristics of work as targets for change. In: Marras WS, Karwowski W, editors. Occupational ergonomics handbook. second. Boca Raton, FL: CRC Press; 2005. [Google Scholar]
- Hemingway MA, Smith CS. Organizational climate and occupational stressors as predictors of withdrawal behaviours and injuries in nurses. J Occup Organ Psychol. 1999;72:285–299. [Google Scholar]
- Hlobil H, Uegaki K, Staal JB, de Bruyne MC, Smid T, van Mechelen W. Substantial sick-leave costs savings due to a graded activity intervention for workers with non-specific sub-acute low back pain. Eur Spine J. 2007;16:919–924. doi: 10.1007/s00586-006-0283-9. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Hofmann DA, Mark B. An investigation of the relationship between safety climate and medication errors as well as other nurse and patient outcomes. Personnel Psychol. 2006;59:847–869. [Google Scholar]
- Huang GD, Feuerstein M, Kop WJ, Schor K, Arroyo F. Individual and combined impacts of biomechanical and work organization factors in work-related musculoskeletal symptoms. Am J Ind Med. 2003;43:495–506. doi: 10.1002/ajim.10212. [DOI] [PubMed] [Google Scholar]
- Huang Y-H, Ho M, Smith GS, Chen PY. Safety climate and self-reported injury: Assessing the mediating role of employee safety control. Accident; analysis and prevention. 2006;38:425–433. doi: 10.1016/j.aap.2005.07.002. [DOI] [PubMed] [Google Scholar]
- Hunt MK, Lederman R, Stoddard AM, LaMontagne AD, McLellan D, Combe C, Barbeau E, Sorensen G. Process evaluation of an integrated health promotion/occupational health model in WellWorks-2. Health Educ Behav. 2005;32:10–26. doi: 10.1177/1090198104264216. [DOI] [PubMed] [Google Scholar]
- Hurtado D, Glymour MM, Berkman LF, Hashimoto D, Reme SE, Sorensen G. Schedule control and mental health: the relevance of coworkers’ reports. Community Work Fam. 2015a;18:416–434. [Google Scholar]
- Hurtado D, Nelson CC, Hashimoto D, Sorensen G. Supervisors' support for nurses' meal breaks and mental health. Workplace health saf. 2015b;63:107–115. doi: 10.1177/2165079915571354. [DOI] [PubMed] [Google Scholar]
- Hurtado DA, Berkman LF, Buxton OM, Okechukwu CA. Schedule Control and Nursing Home Quality Exploratory Evidence of a Psychosocial Predictor of Resident Care. J Appl Gerontol. 2016;35:244–253. doi: 10.1177/0733464814546895. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Hymel PA, Loeppke RR, Baase CM, Burton WN, Hartenbaum NP, Hudson TW, McLellan RK, Mueller KL, Roberts MA, et al. Workplace health protection and promotion: a new pathway for a healthier--and safer--workforce. J Occup Environ Med. 2011;53:695–702. doi: 10.1097/JOM.0b013e31822005d0. [DOI] [PubMed] [Google Scholar]
- Institute of Medicine, Committee on the Health and Safety Needs of Older Workers. Health and safety needs of older workers. Washington, DC: National Academies Press; 2004. [Google Scholar]
- Institute of Medicine Committee to Assess Worksite Preventive Health Program Needs for NASA Employees, F.a.N.B. Integrating employee health: A model program for NASA. Washington, DC: Institute of Medicine, National Academies Press; 2005. [Google Scholar]
- International Association for Worksite Health Promotion (IAWHP) [Accessed August 9, 2013];IAWHP's Las Vegas Announcement on Worksite Health. 2012 Mar 27; 2012 http://www.acsmiawhp.org/files/public/Las%20Vegas%20Announcement%20on%20Worksite%20Health%20Promotion%202012_Final.pdf. [Google Scholar]
- International Labour Office. Stress prevention at work checkpoints: Practical improvements for stress prevention in the workplace. Geneva: 2012. http://www.ilo.org/wcmsp5/groups/public/@dgreports/@dcomm/@publ/documents/publication/wcms_168053.pdf. [Google Scholar]
- Isaac F, Flynn P. Johnson & Johnson LIVE FOR LIFE Program: Now and then. Am J Health Promot. 2001;15:365–367. [PubMed] [Google Scholar]
- Jacobsen H, Reme S, Sembajwe G, Hopcia K, Stoddard A, Kenwood C, Stiles T, Sorensen G, Buxton O. Work-family conflict, psychological distress, and sleep deficiency among patient care workers. Workplace Health Saf. 2014;62:282–291. doi: 10.3928/21650799-20140617-04. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Jacobsen HB, Reme SE, Sembajwe G, Hopcia K, Stiles TC, Sorensen G, Porter JH, Marino M, OM B. Work stress, sleep deficiency, and predicted 10-year cardiometabolic risk in a female patient care worker population. Am J Ind Med. 2014;57:940–949. doi: 10.1002/ajim.22340. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Johansson G, Johnson JV, Hall EM. Smoking and sedentary behavior as related to work organization. Soc Sci Med. 1991;32:837–846. doi: 10.1016/0277-9536(91)90310-9. [DOI] [PubMed] [Google Scholar]
- Jones F, O'Connor DB, Conner M, McMillan B, Ferguson E. Impact of daily mood, work hours, and iso-strain variables on self-reported health behaviors. J Appl Psychol. 2007;92:1731–1740. doi: 10.1037/0021-9010.92.6.1731. [DOI] [PubMed] [Google Scholar]
- Karasek R, Brisson C, Kawakami N, Houtman I, Bongers P, Amick B. The Job Content Questionnaire (JCQ): an instrument for internationally comparative assessments of psychosocial job characteristics. J Occup Health Psychol. 1998;3:322–355. doi: 10.1037//1076-8998.3.4.322. [DOI] [PubMed] [Google Scholar]
- Karasek R, Theorell T. Healthy work: Stress, productivity, and the reconstruction of working life. New York, NY: Basic Books; 1990. [Google Scholar]
- Karsh B, Booske BC, Sainfort F. Job and organizational determinants of nursing home employee commitment, job satisfaction and intent to turnover. Ergonomics. 2005;48:1260–1281. doi: 10.1080/00140130500197195. [DOI] [PubMed] [Google Scholar]
- Kim SS, Okechukwu CA, Buxton OM, Dennerlein JT, Boden LI, Hashimoto DM, Sorensen G. Association between work–family conflict and musculoskeletal pain among hospital patient care workers. Am J Ind Med. 2013;56:488–495. doi: 10.1002/ajim.22120. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Kim SS, Okechukwu CA, Dennerlein JT, Boden LI, Hopcia K, Hashimoto DM, Sorensen G. Association between perceived inadequate staffing and musculoskeletal pain among hospital patient care workers. Int Arch Occup Environ Health. 2014;87:323–330. doi: 10.1007/s00420-013-0864-y. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Kouvonen A, Kivimaki M, Vaananen A, Heponiemi T, Elovainio M, Ala-Mursula L, Virtanen M, Pentti J, Linna A, et al. Job strain and adverse health behaviors: the Finnish Public Sector Study. J Occup Environ Med. 2007;49:68–74. doi: 10.1097/JOM.0b013e31802db54a. [DOI] [PubMed] [Google Scholar]
- Kouvonen A, Kivimaki M, Virtanen M, Heponiemi T, Elovainio M, Pentti J, Linna A, Vahtera J. Effort-reward imbalance at work and the co-occurrence of lifestyle risk factors: cross-sectional survey in a sample of 36,127 public sector employees. BMC Public Health. 2006;6:24. doi: 10.1186/1471-2458-6-24. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Krieger N. Workers are people too: societal aspects of occupational health disparities--an ecosocial perspective. Am J Ind Med. 2010;53:104–115. doi: 10.1002/ajim.20759. [DOI] [PubMed] [Google Scholar]
- Krieger N, Chen JT, Waterman PD, Hartman C, Stoddard AM, Quinn MM, Sorensen G, Barbeau EM. The inverse hazard law: blood pressure, sexual harassment, racial discrimination, workplace abuse and occupational exposures in US low-income black, white and Latino workers. Soc Sci Med. 2008;67:1970–1981. doi: 10.1016/j.socscimed.2008.09.039. [DOI] [PubMed] [Google Scholar]
- Kruse MM. From the Basics to Comprehensive Programming. In: Pronk NP, editor. ACSM's Worksite Health Handbook. 2nd. Champaign, IL: Human Kinetics; 2009. pp. 296–307. [Google Scholar]
- LaMontagne AD, Youngstrom RA, Lewiton M, Stoddard AM, McLellan D, Wallace LM, Barbeau E, Sorensen G. Assessing and intervening on OSH programs: Effectiveness evaluation of the WellWorks-2 intervention in fifteen manufacturing worksites. Occup Environ Med. 2004;61:651–660. doi: 10.1136/oem.2003.011718. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Landsbergis PA, Grzywacz JG, LaMontagne AD. Work organization, job insecurity, and occupational health disparities. Am J Ind Med. 2014;57:495–515. doi: 10.1002/ajim.22126. [DOI] [PubMed] [Google Scholar]
- Law R, Dollard MF, Tuckey MR, Dormann C. Psychosocial safety climate as a lead indicator of workplace bullying and harassment, job resources, psychological health and employee engagement. Accident; analysis and prevention. 2011;43:1782–1793. doi: 10.1016/j.aap.2011.04.010. [DOI] [PubMed] [Google Scholar]
- Lax MB. The Perils of Integrating Wellness and Safety and Health and the Possibility of a Worker-Oriented Alternative. New Solut. 2016;26:11–39. doi: 10.1177/1048291116629489. [DOI] [PubMed] [Google Scholar]
- Levy BS, Wegman DH, Baron SL, Sokas RK. 5th. Philadelphia, PA: Lippincott Williams & Wilkins; 2006. Occupational and environmental health: Recognizing and preventing disease and injury. [Google Scholar]
- Lipscomb J, Trinkoff A, Brady B, Geiger-Brown J. Health care system changes and reported musculoskeletal disorders among registered nurses. Am J Public Health. 2004;94:1431–1435. doi: 10.2105/ajph.94.8.1431. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Lipscomb JA, Trinkoff AM, Geiger-Brown J, Brady B. Work-schedule characteristics and reported musculoskeletal disorders of registered nurses. Scand J Work Environ Health. 2002;28:394–401. doi: 10.5271/sjweh.691. [DOI] [PubMed] [Google Scholar]
- Loeppke RR, Hohn T, Baase C, Bunn WB, Burton WN, Eisenberg BS, Ennis T, Fabius R, Hawkins RJ, et al. Integrating health and safety in the workplace: how closely aligning health and safety strategies can yield measurable benefits. J Occup Environ Med. 2015;57:585–597. doi: 10.1097/JOM.0000000000000467. [DOI] [PubMed] [Google Scholar]
- Macfarlane GJ, Pallewatte N, Paudyal P, Blyth FM, Coggon D, Crombez G, Linton S, Leino-Arjas P, Silman AJ, et al. Evaluation of work-related psychosocial factors and regional musculoskeletal pain: results from a EULAR Task Force. Ann Rheum Dis. 2009;68:885–891. doi: 10.1136/ard.2008.090829. [DOI] [PubMed] [Google Scholar]
- MacKinnon D. Introduction to statistical mediation analysis. New York, NY: Lawrence Erlbaum Associates; 2008. [Google Scholar]
- Maes S, Verhoeven C, Kittel F, Scholten H. Effects of a Dutch worksite wellness-health program: The Brabantia project. Am J Public Health. 1998;88:1037–1041. doi: 10.2105/ajph.88.7.1037. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Malan D, Radjy S, Pronk N, Yach D. Reporting on Health: A Roadmap for Investors, Companies, and Reporting Platforms. 2009 Available at: www.thevitalityinstitute.org/healthreportingVitality Institute. [Google Scholar]
- Marchand A. Alcohol use and misuse: what are the contributions of occupation and work organization conditions? BMC Public Health. 2008;8:333. doi: 10.1186/1471-2458-8-333. [DOI] [PMC free article] [PubMed] [Google Scholar]
- McLellan D, Harden E, Markkanen P, Sorensen G. Version 2.0. Boston, MA: Dana-Farber Cancer Institute; 2012. SafeWell practice guidelines: An integrated approach to worker health. http://centerforworkhealth.sph.harvard.edu/sites/default/files/safewell_guidelines/SafeWellPracticeGuidelines_Complete.pdf. [Google Scholar]
- McLellan D, Pronk N, Pember M. The feasibility and acceptability of disseminating integrated health promotion and health protection interventions through a vendor in small- to medium-sized businesses. Accepted poster abstract Annual Meeting of the American Public Health Association. 2015 Nov [Google Scholar]
- McLellan DL, Caban-Martinez AJ, Nelson C, Pronk NP, Katz JN, Allen JD, Wagner GR, Davis K, Sorensen G. Organizational characteristics influence implementation of worksite health protection and promotion programs: Evidence from smaller businesses. J Occup Environ Med. 2015;57:1009–1016. doi: 10.1097/JOM.0000000000000517. [DOI] [PMC free article] [PubMed] [Google Scholar]
- McLellan RK. Total Worker Health: A Promising Approach to a Safer and Healthier Workforce. Ann Intern Med. 2016 doi: 10.7326/M16-0965. [DOI] [PubMed] [Google Scholar]
- McLeroy KR, Bibeau D, Steckler A, Glanz K. An ecological perspective on health promotion programs. Health Educ Q. 1988;15:351–377. doi: 10.1177/109019818801500401. [DOI] [PubMed] [Google Scholar]
- Mellor N, Webster J. Enablers and challenges in implementing a comprehensive workplace health and well-being approach. Int J Workplace Health Manag. 2013;6:129–142. [Google Scholar]
- Murphy LA, Robertson MM, Carayon P. The next generation of macroergonomics: integrating safety climate. Accident; analysis and prevention. 2014;68:16–24. doi: 10.1016/j.aap.2013.11.011. [DOI] [PubMed] [Google Scholar]
- Nahit ES, Hunt IM, Lunt M, Dunn G, Silman AJ, Macfarlane GJ. Effects of psychosocial and individual psychological factors on the onset of musculoskeletal pain: common and site-specific effects. Ann Rheum Dis. 2003;62:755–760. doi: 10.1136/ard.62.8.755. [DOI] [PMC free article] [PubMed] [Google Scholar]
- National Institute for Occupational Safety and Health. Expanding Our Understanding of the Psychosocial Work Environment: A Compendium of Measures of Discrimination, Harassment and Work-Family Issues. 2008 http://www.cdc.gov/niosh/docs/2008-104/pdfs/2008-104.pdf.
- National Institute for Occupational Safety and Health. Research Compendium: The NIOSH Total Worker HealthTM Program: Seminal Research Papers 2012. Washington DC: 2012. NIOSH 2012; pp. 1–214. http://www.cdc.gov/niosh/docs/2012-146/pdfs/2012-146.pdf. [Google Scholar]
- Nelson CC, Wagner GR, Caban-Martinez AJ, Buxton OM, Kenwood CT, Sabbath EL, Hashimoto DM, Hopcia K, Allen JD, et al. Physical activity and BMI: the contribution of age and workplace characteristics. Am J Prev Med. 2014;46:S42–S51. doi: 10.1016/j.amepre.2013.10.035. PMCID 4007484. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Nishitani N, Sakakibara H. Job stress factors, stress response, and social support in association with insomnia of Japanese male workers. Ind Health. 2010;48:178–184. doi: 10.2486/indhealth.48.178. [DOI] [PubMed] [Google Scholar]
- Office of Technology Assessment. Office of Technology Assessment, Congressional Board of the 99th Congress. Washington, DC: US Government Printing Office; 1985. Preventing illness and injury in the workplace. [Google Scholar]
- Okechukwu CA, Krieger N, Sorensen G, Li Y, Barbeau EM. MassBuilt: effectiveness of an apprenticeship site-based smoking cessation intervention for unionized building trades workers. Cancer Causes Control. 2009;20:887–894. doi: 10.1007/s10552-009-9324-0. PMCID2694320. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Olson R, Anger WK, Elliot DL, Wipfli B, Gray M. A new health promotion model for lone workers: results of the Safety & Health Involvement For Truckers (SHIFT) pilot study. J Occup Environ Med. 2009;51:1233–1246. doi: 10.1097/JOM.0b013e3181c1dc7a. [DOI] [PubMed] [Google Scholar]
- Pember M, McLellan D, Pronk N. Pember M, McLellan D, Pronk N. An integrated approach to worksite wellness, health & safety, delivered via a vendor: A qualitative evaluation. Accepted poster abstract Annual Meeting of the American Public Health Association. 2015 Nov [Google Scholar]
- Probst TM, Brubaker TL, Barsotti A. Organizational injury rate underreporting: The moderating effect of organizational safety climate. J appl Psychol. 2008;93:1147–1154. doi: 10.1037/0021-9010.93.5.1147. [DOI] [PubMed] [Google Scholar]
- Pronk N, McLellan D, McGrail M, Olson SK, Z M, Katz JN, Wagner GR, Sorensen G. Measurement Tools for Integrated Worker Health Protection and Promotion: Lessons Learned from the SafeWell Project. J Occup Environ Med. 2016 doi: 10.1097/JOM.0000000000000752. [DOI] [PubMed] [Google Scholar]
- Pronk NP. Integrated worker health protection and promotion programs: overview and perspectives on health and economic outcomes. J Occup Environ Med. 2013;55:S30–S37. doi: 10.1097/JOM.0000000000000031. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Pronk NP, Baase C, Noyce J, Stevens DE. Corporate America and community health: exploring the business case for investment. J Occup Environ Med. 2015;57:493–500. doi: 10.1097/JOM.0000000000000431. [DOI] [PubMed] [Google Scholar]
- Pronk NP, Katz AS, Lowry M, Payfer JR. Reducing occupational sitting time and improving worker health: the Take-a-Stand Project, 2011. Prev Chronic Dis. 2012;9:E154. doi: 10.5888/pcd9.110323. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Punnett L, Cherniack M, Henning R, Morse T, Faghri P. A conceptual framework for integrating workplace health promotion and occupational ergonomics programs. Public Health Rep. 2009;124(Suppl 1):16–25. doi: 10.1177/00333549091244S103. PMCID:PMC2708653. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Reme SE, Shaw WS, Boden LI, Tveito TH, O'Day ET, Dennerlein JT, Sorensen G. Worker assessments of organizational practices and psychosocial work environment are associated with musculoskeletal injuries in hospital patient care workers. Am J Ind Med. 2014;57:810–818. doi: 10.1002/ajim.22319. [DOI] [PubMed] [Google Scholar]
- Rivilis I, Van Eerd D, Cullen K, Cole DC, Irvin E, Tyson J, Mahood Q. Effectiveness of participatory ergonomic interventions on health outcomes: a systematic review. Appl Ergon. 2008;39:342–358. doi: 10.1016/j.apergo.2007.08.006. [DOI] [PubMed] [Google Scholar]
- Roberts D. The occupational athlete. Injury reduction and productivity enhancement in reforestation workers. In: Pronk N, editor. ACSM's Worksite Health Handbook. A Guide to Building Healthy and Productive Companies. 2nd. Champaign, IL: Human Kinetics; 2009. pp. 309–317. [Google Scholar]
- Robertson MM, Ciriello VM, Garabet AM. Office ergonomics training and a sit-stand workstation: effects on musculoskeletal and visual symptoms and performance of office workers. Appl Ergon. 2013;44:73–85. doi: 10.1016/j.apergo.2012.05.001. [DOI] [PubMed] [Google Scholar]
- Roelofs C, Barbeau E, Moure-Eraso R, Ellenbecker MJ. Prevention strategies in industrial hygiene: A critical literature review. Am J Ind Hygiene Assoc J. 2003;64:62–67. doi: 10.1080/15428110308984788. [DOI] [PubMed] [Google Scholar]
- Rohlman DS, Parish M, Elliot DL, Montgomery D, Hanson G. Characterizing the needs of a young working population: making the case for total worker health in an emerging workforce. J Occup Environ Med. 2013;55:S69–S72. doi: 10.1097/JOM.0000000000000039. [DOI] [PubMed] [Google Scholar]
- Sabbath EL, Hurtado DA, Okechukwu CA, Tamers SL, Nelson C, Kim SS, Wagner G, Sorenson G. Occupational injury among hospital patient-care workers: What is the association with workplace verbal abuse? Am J Ind Med. 2014;57:222–232. doi: 10.1002/ajim.22271. [DOI] [PubMed] [Google Scholar]
- Sauter S, Brightwell SW, Colligan MJ, et al. Department of Health and Human Services. Cincinnati, OH: National Institute for Occupational Health and Safety; 2002. The Changing Organization of Work and Safety and Health of Working People. [Google Scholar]
- Schill AL, Chosewood LC. The NIOSH Total Worker Health program: an overview. J Occup Environ Med. 2013;55:S8–S11. doi: 10.1097/JOM.0000000000000037. [DOI] [PubMed] [Google Scholar]
- Schill AL, Chosewood LC. Total Worker Health(R): More Implications for the Occupational Health Nurse. Workplace Health Saf. 2016;64:4–5. doi: 10.1177/2165079915612790. [DOI] [PubMed] [Google Scholar]
- Schulte P, Vainio H. Well-being at work--overview and perspective. Scand J Work Environ Health. 2010;36:422–429. doi: 10.5271/sjweh.3076. [DOI] [PubMed] [Google Scholar]
- Schulte PA, Pandalai S, Wulsin V, Chun H. Interaction of occupational and personal risk factors in workforce health and safety. Am J Public Health. 2012;102:434–448. doi: 10.2105/AJPH.2011.300249. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Sembajwe G, Tveito TH, Hopcia K, Kenwood C, O'Day ET, Stoddard AM, Dennerlein JT, Hashimoto D, Sorensen G. Psychosocial stress and multi-site musculoskeletal pain: a cross-sectional survey of patient care workers. Workplace Health Saf. 2013;61:117–125. doi: 10.1177/216507991306100304. [DOI] [PubMed] [Google Scholar]
- Shaw WS, Robertson MM, McLellan RK, Verma S, Pransky G. A controlled case study of supervisor training to optimize response to injury in the food processing industry. Work. 2006;26:107–114. [PubMed] [Google Scholar]
- Shaw WS, Robertson MM, Pransky G, McLellan RK. Employee perspectives on the role of supervisors to prevent workplace disability after injuries. J Occup Rehabil. 2003;13:129–142. doi: 10.1023/a:1024997000505. [DOI] [PubMed] [Google Scholar]
- Siegrist J. Adverse health effects of high-effort/low-reward conditions. J Occup Health Psychol. 1996;1:27–41. doi: 10.1037//1076-8998.1.1.27. [DOI] [PubMed] [Google Scholar]
- Siegrist J, Rodel A. Work stress and health risk behavior. Scand J Work Environ Health. 2006;32:473–481. doi: 10.5271/sjweh.1052. [DOI] [PubMed] [Google Scholar]
- Sorensen G, Barbeau E, Hunt MK, Emmons K. Reducing social disparities in tobacco use: A social contextual model for reducing tobacco use among blue-collar workers. Am J Public Health. 2004;94:230–239. doi: 10.2105/ajph.94.2.230. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Sorensen G, Barbeau E, Stoddard A, Hunt MK, Kaphingst K, Wallace L. Promoting behavior change among working-class, multi-ethnic workers: Results of the Healthy Directions Small Business Study. Am J Public Health. 2005;95:1389–1395. doi: 10.2105/AJPH.2004.038745. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Sorensen G, Barbeau E, Stoddard AM, Hunt MK, Goldman R, Smith A, Brennan AA. Tools for Health: The efficacy of a tailored intervention targeted for construction laborers. Cancer Cause Control. 2007;18:51–59. doi: 10.1007/s10552-006-0076-9. [DOI] [PubMed] [Google Scholar]
- Sorensen G, Emmons K, Hunt MK, Barbeau E, Goldman R, Peterson K, Kuntz K, Stoddard A, Berkman L. Model for incorporating social context in health behavior interventions: Applications for cancer prevention for working-class, multiethnic populations. Prev Med. 2003;37:188–197. doi: 10.1016/s0091-7435(03)00111-7. [DOI] [PubMed] [Google Scholar]
- Sorensen G, Himmelstein JS, Hunt MK, Youngstrom R, Hebert J, Hammond SK, Palombo R, Stoddard AM, Ockene J. A model for worksite cancer prevention: Integration of health protection and health promotion in the WellWorks project. Am J Health Promot. 1995;10:55–62. doi: 10.4278/0890-1171-10.1.55. [DOI] [PubMed] [Google Scholar]
- Sorensen G, Landsbergis P, Hammer L, Amick B, Linnan L, Yancey A, Welch L, Goetzel R, Flannery K, et al. Preventing Chronic Disease At the Workplace: A Workshop Report and Recommendations. Am J Public Health. 2011a;101(Suppl 1):S196–S207. doi: 10.2105/AJPH.2010.300075. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Sorensen G, McLellan D, Dennerlein J, Pronk N, Allen JD, Boden LI, Okechukwu CA, Hashimoto D, Stoddard A, et al. Integration of Health Protection and Health Promotion: Rationale, Indicators, and Metrics. J Occup Environ Med. 2013 Dec;55:S12–S18. doi: 10.1097/JOM.0000000000000032. PMCID 4184212. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Sorensen G, Nagler E, Hashimoto D, Dennerlein J, Theron J, Stoddard A, Buxton OM, Wallace L, Kenwood C, et al. Implementing an integrated health protection/health promotion intervention in the hospital setting: Lessons learned from the Be Well, Work Well Study. J Occup Environ Med. 2016;58:185–194. doi: 10.1097/JOM.0000000000000592. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Sorensen G, Stoddard A, Hunt MK, Herbert JR, Ockene JK, Spitz Avrunin J, Himmelstein JS, Hammond SK. The effects of a health promotion-health protection intervention on behavior change: The WellWorks Study. Am J Public Health. 1998;88:1685–1690. doi: 10.2105/ajph.88.11.1685. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Sorensen G, Stoddard A, LaMontagne A, Emmons K, Hunt M, Youngstrom R, McLellan D, Christiani D. A comprehensive worksite cancer prevention intervention: Behavior change results from a randomized controlled trial in manufacturing worksites (United States) Cancer Cause Control. 2002;13:493–502. doi: 10.1023/a:1016385001695. [DOI] [PubMed] [Google Scholar]
- Sorensen G, Stoddard AM, Stoffel S, Buxton O, Sembajwe G, Hashimoto D, Dennerlein JT, Hopcia K. The role of the work context in multiple wellness outcomes for hospital patient care workers. J Occup Environ Med. 2011b;53:899–910. doi: 10.1097/JOM.0b013e318226a74a. PMCID 3693572. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Sparer EH, Herrick RH, Catalano P, Dennerlein JT. Safety Climate Improved through a Safety Communication and Recognition Program for Construction: A Mixed Methods Study. Scan J. Work Environ Health. doi: 10.5271/sjweh.3569. under re-review. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Stokols D. Translating social ecological theory into guidelines for community health promotion. Am J Health Promot. 1996;10:282–298. doi: 10.4278/0890-1171-10.4.282. [DOI] [PubMed] [Google Scholar]
- Trinkoff AM, Storr CL, Lipscomb JA. Physically demanding work and inadequate sleep, pain medication use, and absenteeism in registered nurses. J Occup Environ Med. 2001;43:355–363. doi: 10.1097/00043764-200104000-00012. [DOI] [PubMed] [Google Scholar]
- Tsutsumi A, Nagami M, Yoshikawa T, Kogi K, Kawakami N. Participatory intervention for workplace improvements on mental health and job performance among blue-collar workers: a cluster randomized controlled trial. J Occup Environ Med. 2009;51:554–563. doi: 10.1097/JOM.0b013e3181a24d28. [DOI] [PubMed] [Google Scholar]
- Tullar JM, Brewer S, Amick BC, 3rd, Irvin E, Mahood Q, Pompeii LA, Wang A, Van Eerd D, Gimeno D, et al. Occupational safety and health interventions to reduce musculoskeletal symptoms in the health care sector. J Occup Rehabil. 2010;20:199–219. doi: 10.1007/s10926-010-9231-y. [DOI] [PubMed] [Google Scholar]
- Tveito T, Sembajwe G, Boden L, Dennerlein J, Wagner G, Kenwood C, Stoddard A, Reme S, Hopcia K, et al. Impact of organizational policies and practices on workplace injuries in a hospital setting. J Occup Environ Med. 2014;56:802–808. doi: 10.1097/JOM.0000000000000189. [DOI] [PubMed] [Google Scholar]
- van de Ven A. Theory in practice. Course materials; 2004. Dell Computer Corporation's rise to success. Available at http://www.learningace.com/doc/73248/7533e752bb370259a6fd678a65e90bad/vandeven-dell. [Google Scholar]
- Velazquez V, Baker R, Robin Dewey R, Andrews K, Stock L. Commission on Health and Safety and Workers’ Compensation, Department of Industrial Relations; 2010. The Whole Worker: Guidelines for Integrating Occupational Health and Safety with Workplace Wellness Programs. http://www.dir.ca.gov/chswc/WOSHTEP/Publications/WOSHTEP_TheWholeWorker.pdf. [Google Scholar]
- Walsh DC, Jennings SE, Mangione T, Merrigan DM. Health promotion versus health protection? Employees' perceptions and concerns. J Public Health Policy. 1991;12:148–164. [PubMed] [Google Scholar]
- Whitehead DA. A corporate perspective on health promotion: Reflections and advice from Chevron. Am J Health Promot. 2001;15:367–369. [PubMed] [Google Scholar]
- Williams J, Nelson C, Caban-Martinez AJ, Katz JN, Wagner GR, Pronk NP, Sorensen G, McLellan DL. Validation of a New Metric for Assessing Approaches Integrating Health Protection and Health Promotion. J Occup Environ Med. 2015;57:1017–1021. doi: 10.1097/JOM.0000000000000521. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Williams J, Schult T, Nelson C, Cabán-Martinez A, Katz J, Wagner G, Pronk N, Sorensen G, McLellan D. Validation and Dimensionality of the Integration Score in a Sample of Small and Medium Size Employer Groups and VA Medical Centers. J Occup Environ Med. 2016;58 doi: 10.1097/JOM.0000000000000732. [DOI] [PMC free article] [PubMed] [Google Scholar]
- World Health Organization. Jakarta, Indonesia: World Health Organization; 1997. Jakarta statement on healthy workplaces. [Google Scholar]
- World Health Organization. Shanghai: World Health Organization, Western Pacific Regional Office; 1999. Regional guidelines for the development of healthy workplaces; p. 66. [Google Scholar]
- Zohar D, Polachek T. Discourse-based intervention for modifying supervisory communication as leverage for safety climate and performance improvement: a randomized field study. J Appl Psychol. 2014;99:113–124. doi: 10.1037/a0034096. [DOI] [PubMed] [Google Scholar]