Abstract
This study examines black-white and other sociodemographic differences in young women’s sexual and contraceptive behaviors, using new longitudinal data from a weekly journal-based study of 1,003 18- to 19-year-old women spanning 2.5 years. We investigate hypotheses about dynamic processes in these behaviors during early adulthood in order to shed light on persisting racial differences in rates of unintended pregnancies in the United States. We find that net of other sociodemographic characteristics and adolescent experiences with sex and pregnancy, black women spent less time in relationships and had sex less frequently in their relationships than white women, but did not differ in the number of relationships they formed or in their frequency or consistency of contraceptive use within relationships. Black women were more likely to use less effective methods for pregnancy prevention (e.g., condoms) than white women, who tended to use more effective methods (e.g., oral contraceptives). And although the most effective method for pregnancy prevention—long-acting reversible contraception (LARC)—was used more often by black women than white women, LARC use was low in both groups. In addition, black women did not differ from white women in their number of discontinuations or different methods used and had fewer contraceptive method switches. Further, we find that net of race and adolescent experiences with sex and pregnancy, women from more-disadvantaged backgrounds had fewer and longer (and thus potentially more serious) relationships, used contraception less frequently (but not less consistently), and used less effective methods (condoms) than women from more-advantaged backgrounds.
Keywords: Sex, Contraceptive use, Pregnancy, Race, Sociodemographic, RDSL
Introduction
Black-white differences in pregnancy behaviors persist in the United States. On average, black women have their first baby much earlier than white women (at age 20.9 versus age 24.1) and have more children than white women (2.4 versus 2.2) (Martinez et al. 2012). Although teen pregnancy rates have declined dramatically among all racial and ethnic groups in the United States since their peak in the early 1990s (Kost and Henshaw 2012), black teens have a pregnancy rate that is nearly three times higher than that of white teens (Martinez et al. 2011) as well as an abortion rate four times higher (Kost and Henshaw 2012). Among women of all ages, the unintended pregnancy rate for blacks is more than twice that of whites (Finer and Zolna 2011), as is the percentage of unintended births (Mosher et al. 2012). In this study, we investigate the role of two important proximate determinants of pregnancy—sex and contraceptive use—in producing these black-white differences.
We focus on the beginning of the transition to adulthood, from age 18 or 19 through age 20 or 21, which spans a particularly important period of the life course. Although overall pregnancy rates are higher at older ages, unintended pregnancies—which have been targeted for reduction by Healthy People goals in 2000, 2010, and 20201—peak at these ages (Finer and Zolna 2011). Further, developmental researchers have emphasized the importance of this transition as a period in which young people’s experiences begin to diverge sharply—for instance, as a result of the shift from mandatory, publically funded secondary education to voluntary, mainly privately funded postsecondary school. Accordingly, we draw on the life course perspective to conceptualize the links among race, other sociodemographic characteristics, and sexual and contraceptive behaviors. The life course perspective emphasizes the importance of the timing and sequencing of experiences across the lifespan and proposes that individuals make choices conditional on these experiences and within the constraints and opportunities available to them (Elder 1995; Mayer 2004). Thus, young women’s decisions about sex and contraception during the transition to adulthood depend on their life experiences, which are partly a function of race and other sociodemographic characteristics. These behaviors then set the stage for future behavior in adulthood.
We use unique data from the Relationship Dynamics and Social Life (RDSL) study, which collected weekly information about young women’s relationships, sex, and contraceptive behaviors. Existing longitudinal studies, such as National Longitudinal Study of Adolescent to Adult Health (Add Health), the Fragile Families and Child Wellbeing Study (Fragile Families), and the National Survey of Families and Households (NSFH), as well as the nationally representative cross-sectional National Survey of Family Growth (NSFG), have facilitated important research on sex and contraceptive use. However, hypotheses about how sex and contraceptive use change over time are more plentiful than evidence that can actually speak to these questions. For example, researchers have posited that poor women have more serious relationships at younger ages, which contributes to their higher risk of early pregnancy (Edin and Kefalas 2005), and that black women discontinue their contraceptive methods more frequently than other women (Hammerslough 1984; Trussell and Vaughan 1999). Empirically testing these and other similar hypotheses requires dynamic data on sex and contraception use over time.
Sex and contraception are key proximate determinants of fertility (Bongaarts 1978); all other factors must affect pregnancy via sex and/or contraception. Risk of pregnancy increases with more sex and/or less contraception. The present study contributes to our understanding of these proximate determinants of pregnancy among young women in two important ways. First, we developed a rich set of measures integrating the relationships, sexual intercourse experiences, and contraceptive use of 18- to 19-year-old women over the first year of the RDSL study. Second, because data were collected weekly, we are able to examine changes in sexual and contraceptive behaviors over partners, across relationship length, and by contraceptive method and consistency.
This rich set of data allows, for the first time, an investigation of how race and other sociodemographic characteristics—both separately and in tandem—are related to dynamic pregnancy-related behaviors. This research capability is important because sex and contraceptive use vary substantially across other sociodemographic factors (e.g., by income), and black-white differences in these factors may produce what appear to be—but may not be—variation by race.
Background
Adolescence and the transition to adulthood is a time of many persisting black-white differences in sex and contraceptive behaviors. Black young people [are more likely to have had sexual intercourse, to have initiated sexual activity at earlier ages, and to have had multiple sexual partners in their lifetime than white young people (Cavazos-Rehg et al. 2009; Martinez et al. 2011). Contraceptive non-use is higher among black young people than white young people; and among users, black young people are less likely to report highly effective methods (e.g., oral contraceptives) and more likely to report less effective2 methods (e.g., condoms) (CDC 2012; Shih et al. 2011; Welti et al. 2011).
We hypothesize that three broad sets of factors may lead to these black-white differences in sex and contraceptive use: (1) family and early-life experiences, (2) economic opportunity and attainment, and (3) the legacy of eugenics.
Family and Early-Life Experiences
Compared with their more-advantaged counterparts, young women from disadvantaged backgrounds (e.g., who have teen or single mothers, or who live in poverty) tend to have earlier sex, have a more casual relationship with their first sexual partner, use contraception less frequently in their first sexual experience, experience more forced sex, and have older sexual partners (Browning et al. 2004; Martinez et al. 2011; Sprecher 2013). The research literature has suggested that (1) young women see their mothers or women in their neighborhoods as role models and imitate their behavior (Axinn and Thornton 1996; Brewster 1994; Newcomer and Udry 1984; Thornton and Camburn 1987); (2) the often lower levels of parental supervision in disadvantaged households permit earlier and riskier sexual behavior (Meade et al. 2008); and conversely, (3) parental closeness and authoritative parenting styles in more-advantaged households discourage these behaviors (Kirby 2002; Longmore et al. 2009; McBride et al. 2003; Pearson et al. 2006). Black women are more likely than their white peers to experience these sociodemographic disadvantages given that they are more likely to grow up with younger mothers, more family instability, and lower family income (Browning and Barrington 2006).
In addition, the high proportions of unemployed and incarcerated young black men (Lopoo and Western 2005; Wilson and Neckerman 1986) may disproportionately raise the attractiveness of more available and economically viable black men as sexual partners, thus increasing black women’s willingness to have sex and forgo condom use. This notion is supported by an empirical study of young black women who themselves said that gender imbalance was a reason they tolerated refusal to use condoms and nonmonogamous sexual behavior in their male partners (Ferguson et al. 2006). Also, some evidence has suggested that even though black women have sex earlier than their peers, they have more negative attitudes about sex (Barber et al. 2015; Martinez et al. 2011), which may indicate they feel pressured by their circumstances into early and/or unprotected sex.
Black young people are at a much higher risk of acquiring a sexually transmitted infection (STI) than their white peers (CDC 2014), partly because of higher rates of concurrency and more assortative mating than other racial groups (Hamilton and Morris 2015; Laumann and Youm 1999). The higher rate of STIs among black young men and women (CDC 2014; Owusu-Edusei et al. 2013), coupled with gender distrust among low-income black women (Edin and Kefalas 2005; Whitehead 1997), may result in a greater use of condoms, which protect against STIs but are a less effective method of pregnancy prevention.
Religiosity may have a differential racial impact on both young sex and contraceptive use. In the United States, black young people grow up in more religious families than their white counterparts, with the vast majority attending historically black churches (e.g., Baptist) or evangelical churches (Chatters et al. 2009). Religious doctrine generally opposes premarital sex, and religious young people are more likely than those who are not religious to delay first sex, avoid premarital sex, and have fewer sexual partners (Manlove et al. 2006, 2008). Religious doctrine also tends to be negative toward contraception, but evidence is mixed about whether religiosity affects contraceptive use among those young people who have sex (Manlove et al. 2006, 2008).
Economic Opportunity and Attainment
Because of higher rates of poverty, lower-quality early education, greater labor market discrimination, and residence in more-disadvantaged neighborhoods, black women tend to have less education, lower employment rates, and fewer opportunities for economic attainment than white women (Avery and Rendall 2002; Conley 1999; Isaacs 2007; Oliver and Shapiro 2006; Orr 2003; Proctor and Dalaker 2002). The uncertainty and instability endemic to concentrated poverty (Gottschalk and Moffitt 2009; Western et al. 2012) mean that poor women can expect to see their relationships, cohabitations, and marriages dissolve at higher rates (Copen et al. 2012); to experience more intimate partner violence (Jewkes 2002); to make more residential moves (Pavao et al. 2007); to have more health problems (Mirowsky et al. 2000; Robert and House 2000; Williams and Collins 1995); and to live in poorer-quality environments (Kirby 2008; Wilson 1987). Young women with these experiences may seek out romantic relationships as an escape from a harsh life (Cavanagh et al. 2008; Meadows-Oliver 2006). Edin and Kefalas (2005) described poor young women who perceive potential stability in a path of early sex, lack of contraception, and early parenthood. And Burton and Tucker (2009) described this unreliability and insecurity in the lives of poor African American women—intermittent, low-wage employment, and few alternatives (e.g., men who can support them)—with babies serving as a visible and accessible aspect of stability in otherwise uncertain futures.
Poverty-related structural disadvantages in black neighborhoods—such as lower-quality schools, fewer churches, fewer community centers or associations, and generally less-cohesive local networks—may contribute to so-called ghetto-related behaviors, including teen and nonmarital pregnancy, among residents (Anderson 1990; Wilson 1996). Neighborhood economic conditions of blacks explain a substantial amount of race-based variance in nonmarital pregnancy (South and Baumer 2000) and attitudes related to early sex (Browning and Burrington 2006).
Poor women may also perceive lower potential for education and careers, which would reduce their opportunity costs for having early sex and unprotected sex. An in-depth study of class and sexual behavior among college women found that young women from more-advantaged social backgrounds, who also had higher academic aspirations, delayed serious relationships and pregnancy in explicit recognition that their opportunity costs were high (Armstrong and Hamilton 2013). These strong preferences for delaying childbearing and marriage translate to contraceptive vigilance, given that the vast majority of young women have had sex by their early 20s (Finer and Philbin 2013).
Legacy of Eugenics
Although poverty may affect contraceptive use, given that poor women are less likely to have insurance3 (Ebrahim et al. 2009), the significance of race may extend beyond its connection to family or socioeconomic experiences. Previous research has uncovered significant race differences that are not fully explained by economic factors (e.g., Browning and Burrington 2006; South and Baumer 2000), suggesting the importance of other factors.
At its inception, the U.S. birth control movement drew heavily on the arguments of the eugenics movement (Chesler 2007), popular in the United States in the late nineteenth and early twentieth centuries, the goal of which was to “improve the inborn qualities of a race” (Galton 1904; Osborn 1937) through selective breeding and sterilization. To eugenicists, race and socioeconomic class signaled “fitness” to reproduce (Stubblefield 2007). The massive forced sterilization of Puerto Rican women between 1930 and 1970 was funded by a U.S. federal law, targeting the “unfit” in response to a depressed economy (Gibson-Rosado 1993; Gutiérrez 2008; Presser 1969). The involuntary sterilization of women receiving public assistance in the United States has been publically documented as recently as the 1970s (Boonstra et al. 2000; Malat 2000; Reilly 1991; Roberts 2000; Stern 2005). Many studies in the 1970s documented black men and women’s wariness about contraception—for example, the belief that public funding of birth control is a government plot to keep black fertility rates low (e.g., Darity and Turner 1972; Farrell and Dawkins 1979). More recent studies have also documented the persistence of these ideas (Thorburn and Bogart 2005). Recent nationally representative data demonstrate strong racial/ethnic differences in these perceptions (Rocca and Harper 2012).
The question of whether poor women should bear children is at the heart of some ongoing welfare debates (e.g., see Jencks and Edin 1995); this stance may be particularly distressing to minorities, who disproportionately receive public assistance, and may influence health care providers’ perceptions of the contraceptive methods most appropriate for certain groups of women. Provider bias in contraceptive counseling (Dehlendorf et al. 2010) and other experiences of discrimination within the health care system (Smedley et al. 2006), as well as women’s reactions to these experiences, may affect use of specific contraceptive methods. We expect these beliefs and experiences to translate to lower rates of contraceptive use among black women and also translate to particular avoidance of methods that require interaction with a health care provider (e.g., intrauterine device (IUD), oral contraceptives, or other hormonal birth control methods).
Hypotheses
There are multiple aspects of sex and contraceptive use. Sexual behavior encompasses the number of distinct sexual partners and frequency of sexual intercourse. Contraceptive behavior includes use of any method, consistent use, and the effectiveness of the specific method used (Kirby 2007). Because black women and/or disadvantaged women experience higher rates of pregnancy, we examine whether the following sexual and contraceptive behaviors are more prevalent among them compared with white and/or more-advantaged women, respectively:
Hypothesis 1 (Relationships and Sex): More serious (fewer and longer) relationships and more frequent sex within relationships.
Hypothesis 2 (Contraceptive Use): Less frequent and less consistent contraceptive use.
Hypothesis 3 (Contraceptive Method): Less use of highly effective contraceptive methods.
Hypothesis 4 (Contraceptive Use and Method Instability): More discontinuation of contraceptive use, a greater number of different contraceptive methods used, and more method switches.
Data and Methods
Data
The RDSL study began with a representative random, population-based sample of 1,003 young women, ages 18–19, residing in a single Michigan county. The sampling frame was the Michigan Department of State driver’s license and Personal Identification Card (PID) database.
The first component of data collection was a face-to-face baseline interview conducted between March 2008 and July 2009, assessing sociodemographic characteristics, attitudes, relationship characteristics and history, contraceptive use, and pregnancy history. The most innovative aspect of the RDSL study design was the second component of data collection—dynamic measurement of current pregnancy desires and pregnancy status, as well as characteristics of current relationships (such as commitment level, sexual involvement, and contraceptive use)—collected in weekly five-minute surveys over the following 30 months. We refer to these short weekly surveys as “journals” and to the period between journals as a “week,” although this interval varied from 5 to 13 days, with a mode of 8 days. Respondents were paid $1 per weekly journal, with $5 bonuses for on-time completion of five in a row.
The journal component of the survey concluded in January 2012, resulting in 57,602 weekly interviews. Of the 1,003 women who completed the baseline interview, 953 (95 %) participated in the weekly journal. Among these, 84 % participated for at least six months; 79 %, for at least 12 months; and 75 %, for at least 18 months.
We restrict our analyses to the first 12 months of the study, when response rates were highest. Seven respondents were not included in our analytic sample because they completed only one journal in the first 12 months of the study. Because our study investigates black-white differences, we also excluded 97 respondents who did not identify as non-Hispanic black or non-Hispanic white (see description of race in Measures section). This left 849 respondents who contributed 25,131 weekly interviews in total.
One major contribution of the RDSL data is that we measure sexual and contraceptive behaviors in much more detail than did past surveys, allowing us to better understand which particular facet of these behaviors may explain race differences in unintended pregnancy: not only whether respondents were having sex, but also their sexual frequency, number of sexual partners, and relationship length. Similarly, we consider not only whether any contraception is used but also the method, method switches, method discontinuation, and so on. Because we investigate multiple outcomes, the analytic sample varies by outcome. For instance, respondents are at risk of using contraception to prevent pregnancy only if they are having sex. The specific analytic sample for each outcome is described in more detail in the next section.
Measures
Individual Characteristics
Table 1 presents the distributions of race and other sociodemographic characteristics included in the models, among the full sample and separately by race. Race was measured with the following question: “Which groups describe your racial background? Please select one or more groups: American Indian or Alaska Native, Asian, Native Hawaiian or Other Pacific Islander, Black or African American, or White.” If a respondent selected more than one group, she was asked, “Which of these groups, would you say best describes your racial background?” We excluded 77 respondents who answered affirmatively to a preceding question about Hispanic ethnicity, and we excluded the remaining non-Hispanic groups (n = 20), yielding an analytic sample of n = 849. (The results presented in this article were comparable with those that included the remaining non-Hispanic groups either with whites or as a separate category.) Overall, 35 % of the sample identified as black or African American. We recognize that race is more complex than this dichotomous variable, and we hope that future research will examine how sex and contraceptive behavior differ within racial groups or across racial/ethnic identities, which may be highly contextualized across history and geography.
Table 1.
Descriptive statistics of measures used in the analyses (N = 849; 25,131 weeks; except where noted)
| Total Population | White (n = 556) | Black (n = 293) |
|||||||
|---|---|---|---|---|---|---|---|---|---|
|
|
|||||||||
| Proportion /Mean |
SD | Min. | Max. | Proportion /Mean |
SD | Proportion /Mean |
SD | p Value | |
| Race | |||||||||
| Black | 0.35 | 0 | 1 | ||||||
| White | 0.65 | 0 | 1 | ||||||
| Sociodemographic Characteristics | |||||||||
| High religious importance | 0.58 | 0 | 1 | 0.44 | 0.84 | *** | |||
| Biological mother <20 years old at first birth | 0.36 | 0 | 1 | 0.27 | 0.54 | *** | |||
| Biological mother high school graduate or less | 0.43 | 0 | 1 | 0.40 | 0.49 | *** | |||
| Grew up with both biological parents | 0.45 | 0 | 1 | 0.57 | 0.23 | *** | |||
| Childhood public assistance | 0.36 | 0 | 1 | 0.27 | 0.53 | *** | |||
| Receiving public assistance at age 18–19 | 0.26 | 0 | 1 | 0.18 | 0.43 | *** | |||
| Enrolled in postsecondary education at age 18–19 | 0.57 | 0 | 1 | 0.58 | 0.54 | ||||
| Employed at age 18–19 | 0.49 | 0 | 1 | 0.56 | 0.38 | *** | |||
| Adolescent Experiences With Sex and Pregnancy | |||||||||
| Age at first sex ≤16 years | 0.52 | 0 | 1 | 0.47 | 0.63 | *** | |||
| Two or more sex partners by age 18–19 | 0.60 | 0 | 1 | 0.54 | 0.70 | *** | |||
| Had sex without birth control by age 18–19 | 0.48 | 0 | 1 | 0.41 | 0.60 | *** | |||
| At least one pregnancy by age 18–19 | 0.26 | 0 | 1 | 0.19 | 0.39 | *** | |||
| Relationships and Sex | |||||||||
| Proportion of partnered weeks | 0.67 | 0.37 | 0 | 1 | 0.68 | 0.38 | 0.64 | 0.35 | † |
| Proportion of weeks in an exclusive partnershipa | 0.62 | 0.37 | 0 | 1 | 0.65 | 0.37 | 0.56 | 0.36 | *** |
| Proportion of weeks in which sex occurreda | 0.52 | 0.36 | 0 | 1 | 0.55 | 0.37 | 0.46 | 0.34 | *** |
| Number of partnersa | 2.12 | 1.73 | 1 | 14 | 2.11 | 1.76 | 2.13 | 1.68 | |
| Average length (months) of partnershipsa | 15.86 | 17.77 | 0.23 | 115.15 | 15.27 | 16.06 | 16.93 | 20.51 | |
| Contraceptive Use | |||||||||
| Proportion of weeks any contraception was usedb | 0.89 | 0.24 | 0 | 1 | 0.90 | 0.23 | 0.89 | 0.24 | |
| Proportion of weeks contraception was used consistentlyc | 0.75 | 0.33 | 0 | 1 | 0.77 | 0.32 | 0.69 | 0.35 | ** |
| Contraceptive Method Use | |||||||||
| Proportion of weeks using LARCc | 0.09 | 0.25 | 0 | 1 | 0.07 | 0.22 | 0.13 | 0.29 | ** |
| Among only those who ever used LARC (N = 91) | 0.59 | 0.34 | 0.05 | 1 | 0.58 | 0.35 | 0.59 | 0.33 | |
| Proportion of weeks using the Pillc | 0.38 | 0.42 | 0 | 1 | 0.45 | 0.42 | 0.25 | 0.38 | *** |
| Among only those who ever used the Pill (N = 328) | 0.69 | 0.32 | 0.03 | 1 | 0.70 | 0.32 | 0.65 | 0.33 | |
| Proportion of weeks using a condomc | 0.36 | 0.39 | 0 | 1 | 0.30 | 0.37 | 0.47 | 0.42 | *** |
| Among only those who ever used a condom (N = 367) | 0.58 | 0.35 | 0.02 | 1 | 0.52 | 0.35 | 0.67 | 0.33 | *** |
| Proportion of weeks using withdrawalc | 0.17 | 0.29 | 0 | 1 | 0.18 | 0.30 | 0.15 | 0.27 | † |
| Among only those who ever used withdrawal (N = 234) | 0.43 | 0.33 | 0.02 | 1 | 0.44 | 0.33 | 0.41 | 0.32 | |
| Proportion of weeks using a dual methodc | 0.23 | 0.33 | 0 | 1 | 0.25 | 0.35 | 0.19 | 0.31 | * |
| Among only those who ever used a dual method (N = 291) | 0.47 | 0.34 | 0.02 | 1 | 0.47 | 0.35 | 0.47 | 0.31 | |
| Instability in Contraceptive Use and Method | |||||||||
| Number of discontinuationsc | 0.28 | 0.73 | 0 | 5 | 0.30 | 0.75 | 0.26 | 0.70 | |
| Number of different contraceptive methodsc | 1.76 | 0.82 | 1 | 4 | 1.79 | 0.80 | 1.70 | 0.85 | |
| Number of contraceptive method switchesc | 1.56 | 2.19 | 0 | 15 | 1.64 | 2.18 | 1.40 | 2.21 | |
Notes: LARC includes IUD, implant, or injectable (Depo-Provera). Pill includes the Pill, patch, or vaginal ring (NuvaRing). Dual method use includes LARC or the Pill and condom.
Computed only among weeks in which a partner was reported (N = 786 women; 15,785 weeks).
Computed only among weeks in which sex occurred (N = 611; 7,796 weeks).
Computed only among weeks in which any contraception was used and not missing on specific type of method used (N = 593; 6,873 weeks).
p < .10;
p < .05;
p < .01;
p < .001 (one-tailed tests)
Religious importance was measured with the question, “How important if at all is your religious faith to you?” Response choices ranged from 1 (not at all important) to 4 (more important than anything else). Almost one-half (42 %) chose “not at all” or “somewhat important,” and more than one-half (58 %) chose “very important” or “more important than anything else.” More than one-third (36 %) of respondents reported that their mother was a teen when she had her first child. In answer to the question, “What is the highest level of education your mother completed?,” 43 % reported high school or less, and 57 % reported at least some college. In response to a question about primary childhood residence, 45 % of respondents reported growing up with both biological parents, and 55 % reported growing up with some other family arrangement. More than one-third (36%) reported that their family received public assistance during childhood.
Respondents used a laptop-based computer-assisted self-interview (CASI) program in the baseline interview to report current receipt of public assistance, including Women, Infants, and Children (WIC) program, Family Independence Program (FIP), cash welfare, or food stamps. Approximately one-quarter (26 %) reported receiving assistance from at least one source. Because respondents were age 18 or 19 at the baseline, many were still in high school, although a little more than one-half (57 %) reported being enrolled in a two- or four-year college or a vocational, technical, or other postsecondary school.4 Almost one-half (49 %) reported working either part-time or full-time.5 Black women demonstrated more disadvantage on all these variables than white women (see Table 1). These race differences are substantial and statistically significant except for enrollment in postsecondary education.
Our analyses control for four baseline measures of adolescent experiences with sex and pregnancy prior to the baseline survey: (1) sexual intercourse at age 16 or before, (2) two or more lifetime sexual partners, (3) any sexual intercourse without birth control, and (4) any prior pregnancies. As shown in Table 1, black women in the sample had riskier sexual experiences in their adolescence and higher rates of teen pregnancy than white women—findings that are consistent with the literature (Manlove and Terry-Humen 2007; Martinez et al. 2011).
Relationships, Sex, and Contraception
In every weekly interview, respondents answered a variety of questions about relationships, sexual behavior, and contraceptive use in the prior week. Table 1 presents the distributions of these outcomes for the full sample and separately by race. Respondents were asked to identify their most important partner during the prior week—defined as someone the respondent considered “special” or “romantic,” and/or had sexual contact with during the prior week—which could range from a one-night stand to a fiancée, or anything in-between. Respondents provided initials for a new partner or chose a prior partner from a list. Thus, the data include a continuous record of each respondent’s relationship history during the study period. (If respondents reported more than one partner, we asked them, “Think about the most serious of those partners. If you can’t choose one partner as most serious, then please think about the partner you have been with most recently.”)
Proportion of partnered weeks was calculated by dividing the number of weekly journals in which the respondent identified a partner by her total number of journals. On average, white women were partnered slightly more than two-thirds of the year (mean = 0.68), and black women were partnered slightly less (mean = 0.64; p < .10).
Proportion of weeks in an exclusive partnership is calculated by dividing the number of journals in which the respondent reported being in an exclusive partnership by her total number of journals. On average, white women spent more time in exclusive partnerships (mean = 0.65), and black women spent less time in exclusive partnerships (mean = 0.56; p < .001). (This particular measure is a control in the models, not an outcome of interest.)
In each partnered week, the respondent was asked whether she had sexual intercourse: “Did you have sexual intercourse with [Partner Name]? By sexual intercourse, we mean when a man puts his penis into a woman’s vagina.” We compute the proportion of weeks in which sex occurred among only those weeks when a respondent identified a partner. On average, white women had sex in slightly more than one-half of partnered weeks (mean = 0.55), and black women had sex fewer than one-half of partnered weeks (mean = 0.46; p < .001).
Number of partners was calculated by counting the number of unique partners reported. On average, respondents had two partners during the year (mean = 2.12); this did not significantly differ by race.
Average length of partnerships (in months) was calculated by summing the number of days with each unique partner, converting this to months, and dividing by the number of partners. (This includes the period prior to the beginning of the study for partnerships that were ongoing at baseline; therefore, length can exceed 12 months.) On average, partnerships lasted more than a year (mean = 15.86); this did not significantly differ by race.
Each week, respondents were asked whether they had used any form of birth control in the prior week, regardless of whether they had sex or were trying to prevent pregnancy. Contraceptive users were also asked a series of questions about their use of specific methods as well as a question about consistent contraceptive use: “Did you or your partner use some method of birth control every time you had intercourse (even if you are not trying to prevent pregnancy)?” Based on responses to these survey items, we construct the contraceptive outcomes.
Proportion of weeks any contraception was used was calculated only for the weeks in which sex occurred because some of the methods are used only during sex (e.g., condoms, withdrawal).6 On average, both black and white women reported using some type of contraception about 90 % of the weeks in which they reported having sex (mean = 0.89).
Proportion of weeks contraception was used consistently was calculated only in weeks that any contraception was used. On average, white contraceptors reported consistent use 77 % of the time compared with 69 % for black contraceptors (p < .001).
We grouped contraceptive use weeks into four mutually exclusive categories: (1) IUD, implant, or contraceptive injection (e.g., Depo-Provera), referred to collectively as LARC; (2) oral contraceptives, contraceptive transdermal patch, or vaginal rings (e.g., NuvaRing), referred to collectively as Pill (because this category is dominated by Pill use); (3) condom (male or female); and (4) withdrawal.7 Weeks in which multiple methods were used are coded according to the more effective method. For example, weeks of using both a condom and oral contraceptives (the Pill) are coded as Pill; and weeks coded as Condom refer to use of a condom only or a condom along with a less effective method.
Proportion of weeks using each method was calculated by dividing the number of weeks in which that method was used by the total number of weeks in which any method was used. We also calculate the frequency of use, for each method, for all women who ever used that method.
On average, contraceptors used a LARC method about 10 % of the time (mean = 0.09); and among those who ever used LARC, they did so about 60 % of the time (mean = 0.59). Black contraceptors used LARC slightly more than white contraceptors (mean = 0.13 and 0.07, respectively), but there was no race difference in how long LARC users used that method.
Among white contraceptors, the Pill was the most frequently used method, at nearly one-half of the time (mean = 0.45), and black contraceptors used the Pill only one-quarter of the time (mean = 0.25; p < .001). We found no race difference in how frequently Pill users used that method.
Among black women, condoms were used more than any other method: about one-half of the time (mean = 0.47) for all contraceptors, and more than two-thirds of the time (mean = 0.67) for condom-only users. This usage rate compares with proportions of 30 % and 52 %, respectively, for white contraceptors (p < .001).
Contraceptors in this age group relied on withdrawal relatively infrequently: less than 20 % of all contraception-use weeks among both white and black women. Even those who had ever used withdrawal relied on this method relatively infrequently (mean = 0.43). Black contraceptors relied solely on withdrawal marginally less frequently than white contraceptors (means = 0.15 and 0.18, respectively; p < .10), with no significant race difference among withdrawal users.
Additionally, we coded a separate category, which overlaps with the aforementioned categories: dual method use, defined as weeks in which respondents reported using a LARC or Pill and a condom. Although STIs are not our focus in this article, dual method use is important because it combines the most effective contraceptive method for preventing pregnancy (e.g.., LARC methods) with the most effective method for preventing STIs (e.g., condoms). On average, contraceptors used a dual method almost one-quarter of the time (mean = 0.23), with contraceptors who had ever used a dual method doing so almost one-half of the time (mean = 0.47). Black contraceptors used dual methods less frequently than white contraceptors (mean = 0.19 and 0.25, respectively; p < .05), but there was no race difference in frequency among dual method users.
Number of discontinuations of contraceptive use is a count of distinct periods of non-use. For example, if a respondent reported using condoms, then reported no use of contraception, then used the Pill, then quit all use, and then used condoms again, she would have two discontinuations. On average, all contraceptors had 0.28 periods of discontinuation—a number that did not significantly differ by race.
Number of different methods refers to the total number of unique contraceptive methods ever used. On average, contraceptors used 1.76 methods, with no significant differences by race.
Number of method switches combines these two concepts. For instance, four periods of use consisting of pills, condoms, pills, and condoms, is two methods but three method switches. On average, contraceptors switched methods 1.56 times; number of method switches did not differ by race.
Analytic Strategy
We estimated a series of ordinary least squares (OLS) or Poisson regression models for each outcome using Stata/SE 13.1. We initially used a model-building strategy to examine the extent of race differences in sex and contraceptive use net of other sociodemographic differences. We ran a model that included race only, followed by additions of childhood sociodemographic characteristics, current sociodemographic characteristics, adolescent experiences with sex and pregnancy, and finally proportion of weeks in an exclusive partnership. We also ran models excluding race to examine the extent to which these other sociodemographic differences were net of race differences. In these race-excluded models, the coefficients for the other sociodemographic characteristics remained quite stable, regardless of what additional variables were included in the model. In the race-included models, however, the coefficient for race varied dramatically depending on whether the other characteristics were included. Thus, here, we present two models for each outcome: Model 1 includes race only, and Model 2 adds the other sociodemographic characteristics, measures for adolescent experiences with sex and pregnancy, and a control for proportion of weeks in an exclusive partnership. The latter is not included in the first outcome (proportion of partnered weeks) because a respondent needs to be in a relationship for it to be exclusive or not.8
Results
Table 2 presents the results from OLS or Poisson regression models of relationships and sex (Hypothesis 1). We found that net of other variables, black women spent significantly less time in a relationship than did white women. Among women who spent any time in a relationship, blacks had significantly less frequent sex. These differences are net of other sociodemographic characteristics and of sex and pregnancy during adolescence.9 Black women, however, did not significantly differ from white women during this period in terms of number of partners during the year, regardless of whether we consider other sociodemographic characteristics and/or adolescent experiences. In other words, although they had experienced earlier sex and partnerships during adolescence, these differences were not in evidence during the study period of young adulthood. After we controlled for other sociodemographic characteristics, adolescent experiences with sex and pregnancy, and/or proportion of weeks in an exclusive partnership, black women did have significantly longer partnerships than white women.
Table 2.
OLS or Poisson regression results of relationships and sex on race and sociodemographic characteristics
| Total | Respondents With a Partner | |||||||
|---|---|---|---|---|---|---|---|---|
|
|
||||||||
| Proportion of Partnered Weeks | Proportion of Weeks in Which Sex Occurred |
Number of Partners | Average Length of Partnerships |
|||||
|
|
||||||||
| M1 | M2 | M1 | M2 | M1 | M2 | M1 | M2 | |
| Race | ||||||||
| Black (ref. = white) | −0.04 † (0.03) |
−0.08 ** (0.03) |
−0.09 *** (0.03) |
−0.07 ** (0.03) |
0.01 (0.05) |
0.00 (0.06) |
1.66 (1.32) |
3.98 ** (1.38) |
| Sociodemographic Characteristics | ||||||||
| High religious importance | 0.00 (0.03) |
−0.07 ** (0.02) |
−0.08 † (0.05) |
−1.61 † (1.21) |
||||
| Biological mother <20 years old at first birth | 0.00 (0.03) |
0.00 (0.02) |
0.00 (0.06) |
−0.50 (1.23) |
||||
| Biological mother high school graduate or less | 0.03 (0.03) |
0.03 † (0.02) |
−0.06 (0.05) |
0.90 (1.15) |
||||
| Grew up with both biological parents | 0.00 (0.03) |
−0.01 (0.02) |
−0.02 (0.06) |
2.59 * (1.24) |
||||
| Childhood public assistance | −0.05 * (0.03) |
0.00 (0.02) |
−0.10 * (0.06) |
1.32 (1.26) |
||||
| Receiving public assistance at age 18–19 | 0.00 (0.03) |
−0.04 † (0.03) |
−0.14 * (0.07) |
3.63 ** (1.54) |
||||
| Enrolled in postsecondary education at age 18–19 | 0.01 (0.03) |
−0.02 (0.02) |
0.06 (0.05) |
0.55 (1.17) |
||||
| Employed at age 18–19 | 0.04 † (0.02) |
−0.01 (0.02) |
−0.09 * (0.05) |
1.90 * (1.14) |
||||
| Adolescent Experiences With Sex and Pregnancy | ||||||||
| Age at first sex ≤16 years | 0.07 * (0.03) |
0.11 *** (0.03) |
0.07 (0.07) |
4.52 *** (1.44) |
||||
| Two or more sex partners by age 18–19 | 0.10 *** (0.03) |
0.19 *** (0.03) |
0.21 ** (0.07) |
−7.14 *** (1.47) |
||||
| Had sex without birth control by age 18–19 | 0.14 *** (0.03) |
0.09 *** (0.03) |
0.02 (0.06) |
0.75 (1.35) |
||||
| At least one pregnancy by age 18–19 | 0.04 (0.03) |
−0.07 * (0.03) |
−0.13 * (0.07) |
3.62 ** (1.53) |
||||
| Young Adult Relationship Status | ||||||||
| Proportion of weeks in an exclusive partnership | — | 0.32 *** (0.03) |
−0.73 *** (0.07) |
21.97 *** (1.52) |
||||
| Constant | 0.68 *** (0.02) |
0.14 *** (0.02) |
0.55 *** (0.02) |
0.19 *** (0.04) |
0.75 *** (0.03) |
1.18 *** (0.09) |
15.27 *** (0.79) |
−1.70 (2.02) |
| N | 849 | 786 | 786 | 786 | ||||
Notes: Standard errors are shown in parentheses. A Poisson regression was used for number of partners, and an OLS regression was used for the other outcomes.
p < .10;
p < .05;
p < .01;
p < .001 (one-tailed tests)
Sociodemographic characteristics other than race also were related to relationship formation and sex. Highly religious women had less frequent sex in their relationships than their less religious peers but did not spend less time in relationships and had only marginally fewer partners during the year and marginally shorter relationships. Women who were currently receiving public assistance had significantly fewer and longer relationships. Women who were employed spent more time in relationships than those who were not employed, and they also had fewer and longer (and thus potentially more serious) relationships.
For the most part, as expected, women with more sex and pregnancy experiences during adolescence (sex at an earlier age, more sexual partners, sex without birth control, and pregnancy) had more partners during the first year of the study and had more serious relationships (more time in relationships, more frequent sex, and longer relationships.) The one exception is that young women who reported two or more sexual partners during adolescence had shorter relationships than their counterparts.
Overall, these models suggest substantial black-white differences in time spent in relationships and frequency of sex, but the direction of these differences puts black women at lower risk of pregnancy. Black women had slightly longer relationships, which could increase exposure to sex and thus the risk of pregnancy, but they are less likely to have sex in their relationships. Other sociodemographic characteristics are more closely related to the number of partners and the average length of partnerships during the study: greater disadvantage (public assistance and employed at age 18–19) is associated with fewer partners and longer relationships. Finally, adolescent experiences with sex and pregnancy are strongly related to the subsequent amount of time spent in relationships, frequency of sex, number of partners, and average partnership length, with risky adolescent behavior associated with more time in more serious (longer) relationships (with the exception, noted earlier, that having had two or more sexual partners during adolescence is associated with shorter relationships).
Table 3 presents the results from OLS regression models of contraceptive use: the proportion of weeks any contraception was used and the proportion of weeks contraception was used consistently (Hypothesis 2). Black women did not use contraception less often than their white peers, regardless of whether other sociodemographic characteristics and/or adolescent experiences with sex and pregnancy are included in the models. Among contraceptive users, black women used it less consistently than whites. However, this apparent race difference in consistency is actually due in large part to differences in other sociodemographic characteristics and adolescent experiences with sex and pregnancy.10 Overall, women from more-disadvantaged backgrounds (nonintact family, public assistance during childhood) used contraception less frequently, but if they did use contraception, this use was not necessarily less consistent. Women who were enrolled in postsecondary education used contraception more frequently but only marginally more consistently, while women who were employed used contraception more consistently but only marginally more frequently. Young women with risky sexual experiences and pregnancy in adolescence used contraception less consistently, but not less frequently, than did their counterparts.
Table 3.
OLS regression results of contraceptive use on race and sociodemographic characteristics
| Respondents Who Had Sex: Proportion of Weeks Any Contraception Was Used |
Respondents Who Used Contraception: Proportion of Weeks Contraception Was Used Consistently |
|||
|---|---|---|---|---|
|
|
||||
| M1 | M2 | M1 | M2 | |
| Race | ||||
| Black (ref. = white) | −0.01 (0.02) |
0.03 (0.02) |
−0.08 ** (0.03) |
−0.01 (0.03) |
| Sociodemographic Characteristics | ||||
| High religious importance | −0.01 (0.02) |
−0.03 (0.03) |
||
| Biological mother <20 years old at first birth | 0.02 (0.02) |
−0.02 (0.03) |
||
| Biological mother high school graduate or less | −0.01 (0.02) |
−0.02 (0.03) |
||
| Grew up with both biological parents | 0.04 * (0.02) |
0.01 (0.03) |
||
| Childhood public assistance | −0.04 * (0.02) |
0.01 (0.03) |
||
| Receiving public assistance at age 18–19 | −0.03 (0.03) |
0.01 (0.04) |
||
| Enrolled in postsecondary education at age 18– 19 |
0.05 ** (0.02) |
0.04 † (0.03) |
||
| Employed at age 18–19 | 0.03 † (0.02) |
0.07 ** (0.03) |
||
| Adolescent Experiences With Sex and Pregnancy | ||||
| Age at first sex ≤16 years | 0.02 (0.02) |
0.03 (0.03) |
||
| Two or more sex partners by age 18–19 | −0.02 (0.03) |
−0.09 ** (0.03) |
||
| Had sex without birth control by age 18–19 | −0.03 † (0.02) |
−0.13 *** (0.03) |
||
| At least one pregnancy by age 18–19 | −0.01 (0.03) |
−0.05 † (0.04) |
||
| Young Adult Relationship Status | ||||
| Proportion of weeks in an exclusive partnership | −0.05 * (0.03) |
0.09 * (0.04) |
||
| Constant | 0.90 *** (0.01) |
0.92 *** (0.04) |
0.77 *** (0.02) |
0.79 *** (0.05) |
| N | 611 | 593 | ||
Note: Standard errors are shown in parentheses.
p < .10;
p < .05;
p < .01;
p < .001 (one-tailed tests)
Table 4 presents the results from OLS regression models of the specific contraceptive method used (LARC, Pill, condom, or withdrawal, dual method) (Hypothesis 3). Compared with white women, black women used LARC and condoms more frequently, and the Pill, withdrawal, and a dual method less frequently. Each of these differences is only partially explained by other sociodemographic characteristics and/or adolescent experiences with sex and pregnancy; the exception is dual method use, which is fully explained by the other factors. Women from more-advantaged backgrounds (intact family, and mother not a teen mother) more frequently used oral contraceptives or a combination of condoms and a hormonal method (dual method use), while women from less-advantaged backgrounds more frequently used LARC and condoms. Women who were enrolled in postsecondary education used oral contraceptives more frequently and condoms less frequently than women who were not enrolled. Employed women used LARC less frequently and used oral contraceptives or a combination of condoms and a hormonal method (dual method use) more frequently than unemployed women. Those with multiple partners during adolescence more frequently used LARC and less frequently used condoms; those who previously had sex without birth control used all methods less frequently except condoms and withdrawal; and those with prior pregnancies more frequently used LARC and less frequently used oral contraceptives.
Table 4.
OLS regression results of contraceptive method use on race and sociodemographic characteristics
| Proportion of LARC Weeks | Proportion of Pill Weeks | Proportion of Condom Weeks | Proportion of Withdrawal Weeks |
Proportion of Dual Method Use Weeks |
||||||
|---|---|---|---|---|---|---|---|---|---|---|
|
|
||||||||||
| M1 | M2 | M1 | M2 | M1 | M2 | M1 | M2 | M1 | M2 | |
| Race | ||||||||||
| Black (ref. = white) | 0.06 ** (0.02) |
0.05 * (0.03) |
−0.20 *** (0.04) |
−0.10 ** (0.04) |
0.18 *** (0.03) |
0.13 *** (0.04) |
−0.04 † (0.03) |
−0.07 ** (0.03) |
−0.06 * (0.03) |
−0.04 (0.03) |
| Sociodemographic Characteristics | ||||||||||
| High religious importance | −0.01 (0.02) |
0.01 (0.04) |
−0.02 (0.03) |
0.03 (0.03) |
0.02 (0.03) |
|||||
| Biological mother <20 years old at first birth |
−0.02 (0.02) |
−0.06 * (0.04) |
0.09 ** (0.03) |
−0.01 (0.03) |
−0.05 * (0.03) |
|||||
| Biological mother high school graduate or less |
0.03 † (0.02) |
−0.05 † (0.03) |
0.02 (0.03) |
0.00 (0.02) |
−0.01 (0.03) |
|||||
| Grew up with both biological parents |
0.02 (0.02) |
0.07 * (0.04) |
−0.06 * (0.03) |
−0.03 (0.03) |
0.02 (0.03) |
|||||
| Childhood public assistance | 0.04 * (0.02) |
0.00 (0.04) |
−0.03 (0.04) |
−0.02 (0.03) |
0.05 * (0.03) |
|||||
| Receiving public assistance at age 18–19 |
0.02 (0.03) |
−0.01 (0.05) |
0.04 (0.04) |
−0.05 † (0.03) |
0.05 (0.04) |
|||||
| Enrolled in postsecondary education at age 18–19 |
0.02 (0.02) |
0.06 * (0.03) |
−0.06 * (0.03) |
−0.02 (0.03) |
0.00 (0.03) |
|||||
| Employed at age 18–19 | −0.04 * (0.02) |
0.09 ** (0.03) |
−0.03 (0.03) |
−0.02 (0.02) |
0.06 * (0.03) |
|||||
| Adolescent Experiences With Sex and Pregnancy | ||||||||||
| Age at first sex ≤16 years | 0.01 (0.03) |
0.07 † (0.04) |
−0.06 † (0.04) |
−0.01 (0.03) |
−0.02 (0.03) |
|||||
| Two or more sex partners by age 18–19 |
0.06 * (0.03) |
0.00 (0.04) |
−0.08 * (0.04) |
0.02 (0.03) |
0.04 (0.04) |
|||||
| Had sex without birth control by age 18–19 |
−0.06 ** (0.02) |
−0.13 *** (0.04) |
0.04 (0.04) |
0.15 *** (0.03) |
−0.18 *** (0.03) |
|||||
| At least one pregnancy by age 18–19 |
0.09 *** (0.03) |
−0.10 * (0.04) |
−0.01 (0.04) |
0.01 (0.03) |
0.02 (0.04) |
|||||
| Young Adult Relationship Status | ||||||||||
| Proportion of weeks in an exclusive partnership |
0.04 (0.03) |
0.12 ** (0.05) |
−0.12 ** (0.05) |
−0.04 (0.04) |
−0.02 (0.04) |
|||||
| Constant | 0.07 *** (0.01) |
−0.01 (0.04) |
0.45 *** (0.02) |
0.33 *** (0.06) |
0.30 *** (0.02) |
0.51 *** (0.06) |
0.18 *** (0.01) |
0.17 *** (0.05) |
0.25 *** (0.02) |
0.29 *** (0.05) |
| N | 593 | 593 | 593 | 593 | 593 | |||||
Notes: Standard errors are shown in parentheses. LARC includes IUD, implant, or injectable (Depo-Provera). Pill includes the Pill, patch, or vaginal ring (NuvaRing). Dual method use includes LARC or the Pill and condom.
p < .10;
p < .05;
p < .01;
p < .001 (one-tailed tests)
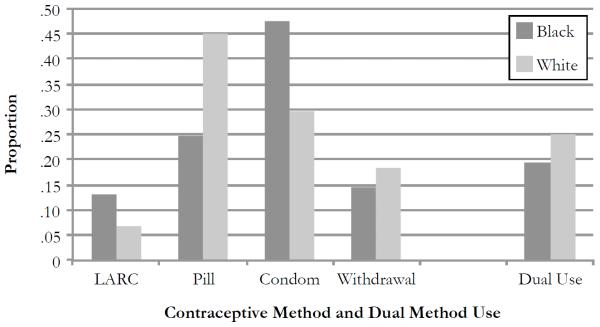
Because the frequency with which these methods were used varies widely, we also present, in Fig. 1, model-based predicted proportions of weeks using each method, by race. On average, the proportion of weeks that black women used LARC was somewhat higher than the proportion for white women; even for black women, however, the average proportion was only about 13 %. Pills and condoms were the most frequently used methods for all women, but whites used pills nearly twice as much as blacks, and blacks used condoms over 1.5 times more than whites. Withdrawal was used less often than pills or condoms but more than LARC, with white women depending on withdrawal slightly more than black women. Dual method use did not differ for black and white women.
Fig. 1.
Model-based predicted proportions of weeks used each contraceptive method and dual method use by race. *p < .05
Table 5 presents the results from Poisson regression models of instability in contraceptive use and method (Hypothesis 4). At the bivariate level, black women did not have more periods of discontinuation or use more different methods, and they had significantly fewer method switches than their white peers. After we accounted for sociodemographic characteristics and adolescent experience variables, race differences in the number of switches remained significant and became slightly more negative. This is because unemployment and adolescent experiences of having more partners, sex without birth control, and prior pregnancies are associated with more method switches—all of which are more commonly experienced by black women. In other words, given their adolescent experiences with sex and pregnancy and lower employment rates, black women switched methods less frequently than would be expected. Women who were enrolled in postsecondary education had fewer periods of discontinuation than those who were not enrolled. Employed women had fewer method switches than unemployed women. Finally, an earlier age at first sex predicted more periods of discontinuation, and previous sex without birth control was associated with more periods of discontinuation and more method switches.
Table 5.
Poisson regression results of instability in contraceptive use and method on race and sociodemographic characteristics
| Number of Discontinuations | Number of Different Methods | Number of Method Switches | ||||
|---|---|---|---|---|---|---|
|
|
||||||
| M1 | M2 | M1 | M2 | M1 | M2 | |
| Race | ||||||
| Black (ref. = white) | −0.15 (0.17) |
−0.14 (0.19) |
−0.05 (0.07) |
−0.06 (0.08) |
−0.16 * (0.07) |
−0.18 * (0.08) |
| Sociodemographic Characteristics | ||||||
| High religious importance | −0.07 (0.17) |
−0.05 (0.07) |
−0.08 (0.07) |
|||
| Biological mother <20 years old at first birth | −0.20 (0.17) |
0.00 (0.07) |
0.11 † (0.07) |
|||
| Biological mother high school graduate or less | −0.03 (0.16) |
0.01 (0.07) |
−0.11 † (0.07) |
|||
| Grew up with both biological parents | −0.25 † (0.18) |
−0.04 (0.07) |
−0.09 (0.08) |
|||
| Childhood public assistance | 0.33 * (0.17) |
0.04 (0.07) |
0.09 (0.08) |
|||
| Receiving public assistance at age 18–19 | −0.38 * (0.21) |
−0.05 (0.09) |
−0.15 † (0.09) |
|||
| Enrolled in postsecondary education at age 18–19 | −0.36 * (0.16) |
0.05 (0.07) |
0.06 (0.07) |
|||
| Employed at age 18–19 | 0.22 † (0.16) |
−0.04 (0.07) |
−0.23 *** (0.07) |
|||
| Adolescent Experiences With Sex and Pregnancy | ||||||
| Age at first sex ≤16 years | 0.56 ** (0.22) |
0.02 (0.08) |
0.02 (0.09) |
|||
| Two or more sex partners by age 18–19 | 0.30 (0.24) |
0.02 (0.08) |
0.12 † (0.09) |
|||
| Had sex without birth control by age 18–19 | 0.54 ** (0.20) |
0.07 (0.07) |
0.17 * (0.08) |
|||
| At least one pregnancy by age 18–19 | −0.10 (0.20) |
0.07 (0.08) |
−0.01 (0.09) |
|||
| Young Adult Relationship Status | ||||||
| Proportion of weeks in an exclusive partnership | 0.82 ** (0.27) |
0.18 * (0.10) |
0.72 *** (0.11) |
|||
| Constant | −1.20 *** (0.09) |
−2.54 *** (0.36) |
0.58 *** (0.04) |
0.40 *** (0.13) |
0.50 *** (0.04) |
−0.04 (0.14) |
| N | 593 | 593 | 593 | |||
Note: Standard errors are shown in parentheses.
p < .10;
p < .05;
p < .01;
p < .001 (one-tailed tests)
We also investigated whether the effect of disadvantage on the outcomes differed by race (results not shown). Although the overall patterns were less clear, we did find a specific few examples where the effect of disadvantage was more evident for whites compared with blacks. For instance, the negative effects of having a mother with a high school diploma or less or of receiving public assistance during childhood or at age 18–19 on consistency of contraceptive use were greater for whites than blacks. In addition, the negative effect of having a mother who was a teen mother or had a high school diploma or less, or of receiving public assistance at age 18–19, on pill use was greater for whites than blacks. Finally, the positive effect of having a mother who was a teen mother on number of discontinuations and of having a mother with a high school diploma or less on number of method switches was greater for whites than blacks.
Discussion
In their now-famous portrait of young disadvantaged mothers, both black and white, Edin and Kefalas (2005) argued that when relationships become serious, contraceptive use ceases. Elijah Anderson (1990) and others have argued that unstable, “messy” relationships among blacks produce pregnancies because young black men are not committed to the mothers. To be thoroughly tested, these and other similar hypotheses must be investigated with dynamic data that capture the interaction of sex, contraception, and relationship experiences with the influence of other sociodemographic characteristics during the transition to adulthood.
According to the proximate determinants of fertility framework (Bongaarts 1978), black women’s higher rates of teen and/or unintended pregnancy would be due to having more sex and/or using less contraception than white women. However, we found that 18- and 19-year-old black women engage in sex and use contraception during the transition to adulthood about as frequently as their white counterparts. And although they use contraception less consistently than white women, this difference largely disappears after other sociodemographic characteristics are included in the models. Net of other variables, the most striking difference is in the method of contraception, with black women using the Pill at significantly lower rates and condoms at significantly higher rates than white women. Although other researchers have posited that black women’s higher pregnancy and unintended pregnancy rates are due to discontinuation and/or method switching (Hammerslough 1984; Trussell and Vaughan 1999), we find no such evidence. Black women in our study did not discontinue contraceptive use more than white women and actually switched methods less frequently, which is consistent with our finding that black women use condoms more frequently and use the Pill less frequently than white women. Discontinuation of condom use is more often followed by resumed use of condoms, whereas discontinuation of the Pill is often followed by a change in method (Vaughan et al. 2008).
Other research has demonstrated that black women are more negative than white women about contraception, especially oral contraceptive pills (Barber et al. 2015; Gilliam et al. 2009). They perceive more side effects of hormonal contraception (Guzzo and Hayford 2012; Kaye et al. 2009). We speculate that these negative attitudes may reflect mistrust of healthcare providers partly because of the historical association between the family planning movement and eugenics, unethical medical testing on vulnerable populations, and forced sterilization, although these mechanisms are difficult to test. In addition, because black women are more negative than white women about sex, and have lower expectation for sex in the near future (Barber et al. 2015), they may eschew methods that require a great deal of advance planning, such as oral contraceptives, in favor of methods that can be provided by men or procured at the last minute (e.g., condoms). Black women also face a high risk of STIs (CDC 2014), and condoms are highly effective for STI prevention. Nevertheless, black women’s reliance on condoms likely contributes to their risk of unintended pregnancy.
Similarly, the proximate determinants of fertility framework (Bongaarts 1978) would posit that disadvantaged women’s higher rates of teen and/or unintended pregnancy are associated with their tendency to have more sex and/or use less contraception than more-advantaged women. Overall, we find support for these linkages. For instance, young women who receive public assistance tend to have fewer and longer relationships, potentially signifying more serious relationships, and thus a higher risk of pregnancy. These are the types of relationships that Edin and Kefalas (2005) highlighted as being at risk of pregnancy as contraception ceases with increased seriousness. The findings from our study extend this finding in that we also have a comparison group of more-advantaged women and find that disadvantaged women form more serious relationships. We also find that young women from disadvantaged backgrounds use contraception less frequently. On the other hand, these young women are not necessarily using contraception less consistently. We do find differences in terms of the type of contraceptive method used, with disadvantaged young women using less effective methods (condoms) more frequently and using more effective methods (oral contraceptives) less frequently. In summary, among our sample of 18- to 19-year olds, women from more-disadvantaged backgrounds formed fewer, longer, and thus possibly more serious relationships than women from more-advantaged backgrounds, and used less effective contraceptive methods within these relationships.
In addition, we find that women who were employed had fewer and longer relationships, and thus possibly more serious ones, which could increase their risk of pregnancy (Edin and Kefalas 2005). This finding is consistent with the idea that employment may detract from school and other activities that could reduce the incidence of risky relationship behaviors (Bauermeister et al. 2009). Employment during the transition to adulthood may also indicate lower investment in a future career, which may translate into less desire to avoid pregnancy, especially if employment improves the affordability of having a baby. However, we also find that women who were employed used contraception more consistently and used more effective methods. This finding is more consistent with the idea that employment promotes young people’s sense of responsibility and independence, and exposes them to more adult-like roles and expectations (Bauermeister et al. 2009). Further, and perhaps more importantly in the case of contraceptive behaviors, employment provides greater resources to both purchase health care and birth control and may also increase the opportunity costs of becoming pregnant. This perspective would suggest that employed young women would be less likely to engage in behaviors that would increase their risk of pregnancy.
The present study has important limitations, perhaps most notably the narrow geographic focus (a single county in Michigan) of the RDSL data. However, Michigan falls around the national median in measures of cohabitation, marriage, age at first birth, completed family size, nonmarital childbearing, and teenage childbearing (see Lesthaeghe and Neidert 2006). Also, because the geographic area is the same for all respondents, observed race differences cannot be attributed to well-known, black-white regional variation in the variables of interest. Furthermore, the county sample has a good deal of variation in sociodemographic characteristics within each race group. On the other hand, the RDSL sample includes only a small number of Latinas—a limitation that we hope motivates future researchers to implement similar studies on larger and more diverse populations. We also recognize that race and other sociodemographic characteristics are nuanced. For instance, race is not a simple dichotomous variable that can explain black women’s low oral contraceptive usage or reliance on condoms. Understanding race differences in method use requires a more comprehensive portrait of which women within the black community are choosing to use the Pill and which women are not. Finally, further exploration of relationship characteristics may provide insights into early and unintended pregnancy rates. Although black women in our sample had fewer relationships and less sex than white women, unobserved characteristics of their relationships may lead to differential risks of pregnancy.
In this study, we use detailed dynamic data to investigate hypotheses about the dynamic processes in pregnancy-related behavior behaviors during early adulthood in order to shed light on persisting racial differences in rates of unintended pregnancies in the United States. We find many similarities in sex and contraceptive use between black and white young women, and some of the observed differences—such as black women’s less consistent contraceptive use—are attributable mainly to other sociodemographic factors. We find striking black-white differences in contraceptive method: black women use the Pill less often and rely on condoms more often than white women. These differences are not explained by relative disadvantage and may contribute to black women’s higher risk of unintended pregnancy. Socioeconomic disadvantage is an independent predictor of more serious relationships, less-frequent contraception, and greater reliance on less effective contraceptive methods, all of which are behaviors that put disadvantaged women at greater risk of unintended pregnancy than their more affluent peers.
Acknowledgments
This research was supported by two research grants from the National Institute of Child Health and Human Development (R01 HD050329, R01 HD050329-S1, PI Barber), a research grant from the National Institute on Drug Abuse (R21 DA024186, PI Axinn), and a population center grant (R24 HD041028) and training grant (T32 HD007339) from the National Institute of Child Health and Human Development to the University of Michigan Population Studies Center. The authors gratefully acknowledge the Survey Research Operations (SRO) unit at the Survey Research Center of the Institute for Social Research for their help with the data collection, particularly Vivienne Outlaw, Sharon Parker, and Meg Stephenson. The authors also gratefully acknowledge the intellectual contributions of the other members of the original RDSL project team (William Axinn, Mick Couper, Steven Heeringa, Heather Gatny), and the National Advisory Committee for the project (Larry Bumpass, Elizabeth Cooksey, Kathie Harris, and Linda Waite).
Footnotes
More information about the National Center for Health Statistics Healthy People goals can be found online (http://www.cdc.gov/nchs/healthy_people/index.htm).
Throughout this article, the “effectiveness” of contraceptive methods refers specifically to pregnancy prevention. We recognize that condoms are highly effective at sexually transmitted infection (STI) prevention.
RDSL data collection preceded the Affordable Care Act (ACA), which eliminates co-pays for contraception.
Preliminary analyses included separate categories for two-year college, vocational, technical, or other school versus four-year college, but the results did not differ for the two categories. They are combined for parsimony.
Preliminary analyses included separate categories for full-time versus part-time employment, but the results did not differ for the two categories. They are combined for parsimony.
In all analyses of contraceptive use, we eliminate the small number of weeks in which the respondents were pregnant—less than 1 % of the weeks (N = 895 weeks). Fourteen respondents were excluded entirely because they were pregnant during all the weeks they completed interviews during the first 12 months.
Preliminary analyses included separate categories for each method type, but the results did not differ for the methods included in LARC or for those included in Pill; therefore, they were combined for the sake of parsimony. Weeks in which only an “other” method was reported (e.g., spermicide only) or the respondent did not report the specific method used were excluded from this set of analyses because of small sample sizes (less than 1 % of weeks where any contraception was used (n = 46 weeks)).
We also conducted sensitivity analyses for all contraception models (Tables 3–5) that excluded weeks in which the respondent had a strong desire to become pregnant (and no desire to avoid pregnancy). The results did not differ from those presented.
Race differences were larger after we controlled for adolescent experiences with sex and pregnancy, indicating that black women experience even less sex and partnerships than we would expect, given their adolescent experiences with sex and pregnancy.
There were no differences in the race coefficient between models that did not include adolescent experiences with sex and pregnancy and models that did.
References
- Anderson E. Streetwise: Race, class, and change in an urban community. University of Chicago Press; Chicago, IL: 1990. [Google Scholar]
- Armstrong EA, Hamilton LT. Paying for the party: How college maintains inequality. Harvard University Press; Cambridge, MA: 2013. [Google Scholar]
- Avery RB, Rendall MS. Lifetime inheritances of three generations of whites and blacks. American Journal of Sociology. 2002;107:1300–1346. [Google Scholar]
- Axinn WG, Thornton A. The influence of parents’ marital dissolutions on children’s attitudes toward family formation. Demography. 1996;33:66–81. [PubMed] [Google Scholar]
- Barber JS, Eckerman Yarger J, Gatny HH. Black-white differences in attitudes related to pregnancy among young women. Demography. 2015;52:751–786. doi: 10.1007/s13524-015-0391-4. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Bauermeister JA, Zimmerman MA, Gee GC, Caldwell C, Xue Y. Work and sexual trajectories among African American youth. Journal of Sex Research. 2009;46:290–300. doi: 10.1080/00224490802666241. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Bongaarts J. A framework for analyzing the proximate determinants of fertility. Population and Developmental Review. 1978;4:105–132. [Google Scholar]
- Boonstra H, Duran V, Gamble VN, Blumenthal P, Dominguez L, Pies C. The “boom and bust phenomenon”: The hopes, dreams, and broken promises of the contraceptive revolution. Contraception. 2000;61:9–25. doi: 10.1016/s0010-7824(99)00121-3. [DOI] [PubMed] [Google Scholar]
- Brewster KL. Neighborhood context and the transition to sexual activity among young black women. Demography. 1994;31:603–614. [PubMed] [Google Scholar]
- Browning CR, Burrington LA. Racial differences in sexual and fertility attitudes in an urban setting. Journal of Marriage and Family. 2006;68:236–251. [Google Scholar]
- Browning CR, Leventhal T, Brooks-Gunn J. Neighborhood context and racial differences in early adolescent sexual activity. Demography. 2004;41:697–720. doi: 10.1353/dem.2004.0029. [DOI] [PubMed] [Google Scholar]
- Burton LM, Tucker MB. Romantic unions in an era of uncertainty: A post-Moynihan perspective on African American women and marriage. ANNALS of the American Academy of Political and Social Science. 2009;621:132–148. [Google Scholar]
- Cavanagh SE, Crissey SR, Raley RK. Family structure history and adolescent romance. Journal of Marriage and Family. 2008;70:698–714. [Google Scholar]
- Cavazos-Rehg PA, Kraussb MJ, Spitznagelc EL, Schootmand M, Bucholza KK, Peiperte JF, Bierut LJ. Age of sexual debut among US adolescents. Contraception. 2009;80:158–162. doi: 10.1016/j.contraception.2009.02.014. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Centers for Disease Control and Prevention (CDC) Sexual experience and contraceptive use among female teens—United States, 1995, 2002, and 2006–2010. Morbidity and Mortality Weekly Report (MMWR) 2012;61:297–301. [PubMed] [Google Scholar]
- Centers for Disease Control and Prevention (CDC) Sexually transmitted disease surveillance 2013. U.S. Department of Health and Human Services; Atlanta, GA: 2014. (Division of STD Prevention Report, December 2014) [Google Scholar]
- Chatters LM, Taylor RJ, Bullard KM, Jackson JS. Race and ethnic differences in religious involvement: African Americans, Caribbean blacks and non-Hispanic whites. Ethnic and Racial Studies. 2009;32:1143–1163. doi: 10.1080/01419870802334531. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Chesler E. Woman of valor: Margaret Sanger and the birth control movement in America. Simon & Schuster; New York, NY: 2007. [Google Scholar]
- Conley D. Being black, living in the red: Race, wealth, and social policy in America. University of California Press; Berkeley: 1999. [Google Scholar]
- Copen CE, Daniels K, Vespa J, Mosher WD. First marriages in the United States: Data from the 2006–2010 National Survey of Family Growth. National Center for Health Statistics; Hyattsville, MD: 2012. (National Health Statistics Reports, No. 49) [PubMed] [Google Scholar]
- Darity WA, Turner CB. Family planning, race consciousness and the fear of race genocide. American Journal of Public Health. 1972;62:1455–1459. doi: 10.2105/ajph.62.11.1454. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Dehlendorf C, Ruskin R, Grumbach K, Vittinghoff E, Bibbins-Domingo K, Schillinger D, Steinauer J. Recommendations for intrauterine contraception: A randomized trial of the effects of patients’ race/ethnicity and socioeconomic status. American Journal of Obstetrics & Gynecology. 2010;203:319e1–319e8. doi: 10.1016/j.ajog.2010.05.009. doi: http://dx.doi.org/10.1016/j.ajog.2010.05.009. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Ebrahim SH, Anderson JE, Correa-de-Araujo R, Posner SF, Atrash HK. Overcoming social and health inequalities among US women of reproductive age—Challenges to the nation’s health in the 21st century. Health Policy. 2009;90:196–205. doi: 10.1016/j.healthpol.2008.09.011. [DOI] [PubMed] [Google Scholar]
- Edin K, Kefalas M. Promises I can keep. University of California Press; Berkeley: 2005. [Google Scholar]
- Elder GH. The life course paradigm: Social change and individual development. In: Moen P, Elder GH, Lüscher K, editors. Examining lives in context: Perspectives on the ecology of human development. American Psychological Association; Washington, DC: 1995. pp. 101–139. [Google Scholar]
- Farrell WC, Dawkins MP. Determinants of genocide fear in a rural Texas community: A research note. American Journal of Public Health. 1979;69:605–607. doi: 10.2105/ajph.69.6.605. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Ferguson YO, Quinn SC, Eng E, Sandelowski M. The gender ratio imbalance and its relationship to risk of HIV/AIDS among African American women at historically black colleges and universities. AIDS Care. 2006;18:323–331. doi: 10.1080/09540120500162122. [DOI] [PubMed] [Google Scholar]
- Finer LB, Philbin JM. Sexual initiation, contraceptive use, and pregnancy among young adolescents. Pediatrics. 2013;131(5):1–8. doi: 10.1542/peds.2012-3495. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Finer LB, Zolna MR. Unintended pregnancy in the United States: Incidence and disparities, 2006. Contraception. 2011;84:478–485. doi: 10.1016/j.contraception.2011.07.013. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Galton F. Eugenics: Its definition, scope, and aims. American Journal of Sociology. 1904;10:1–25. [Google Scholar]
- Gibson-Rosado EM. The sterilization of women in Puerto Rico under the cloak of colonial policy: A case study on the role of perception in U.S. foreign policy and population control. Johns Hopkins University; Baltimore, MD: 1993. [Google Scholar]
- Gilliam ML, Davis SD, Neustadt AB, Levey EJ. Contraceptive attitudes among inner-city African American female adolescents: Barriers to effective hormonal contraceptive use. Journal of Pediatric and Adolescent Gynecology. 2009;22:97–104. doi: 10.1016/j.jpag.2008.05.008. [DOI] [PubMed] [Google Scholar]
- Gottschalk P, Moffitt R. The rising instability of US earnings. Journal of Economic Perspectives. 2009;23(4):3–24. [Google Scholar]
- Gutiérrez ER. The politics of Mexican-origin women’s reproduction. University of Texas Press; Austin: 2008. [Google Scholar]
- Guzzo KB, Hayford S. Race-ethnic differences in sexual health knowledge. Race and Social Problems. 2012;4:158–170. doi: 10.1007/s12552-012-9076-4. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Hamilton DT, Morris M. The racial disparities in STI in the U. S.: Concurrency, STI prevalence, and heterogeneity in partner selection. Epidemics. 2015;11:56–61. doi: 10.1016/j.epidem.2015.02.003. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Hammerslough CR. Characteristics of women who stop using contraceptives. Family Planning Perspectives. 1984;16:14–15. 18. [PubMed] [Google Scholar]
- Isaacs J. Economic mobility of black and white families (Economic Mobility Project report) Pew Charitable Trusts; Washington, DC: 2007. [Google Scholar]
- Jencks C, Edin K. Do poor women have a right to bear children? American Prospect. 1995;20:43–52. [Google Scholar]
- Jewkes R. Intimate partner violence: Causes and prevention. Lancet. 2002;359:1423–1429. doi: 10.1016/S0140-6736(02)08357-5. [DOI] [PubMed] [Google Scholar]
- Kaye K, Suellentrop K, Sloup C. The fog zone: How misperceptions, magical thinking, and ambivalence put young adults at risk for unplanned pregnancy (report) The National Campaign to Prevent Teen and Unplanned Pregnancy; Washington, DC: 2009. Retrieved from https://thenationalcampaign.org/sites/default/files/resource-primary-download/FogZone.pdf. [Google Scholar]
- Kirby D. Antecedents of adolescent initiation of sex, contraceptive use, and pregnancy. American Journal of Health Behavior. 2002;26:473–485. doi: 10.5993/ajhb.26.6.8. [DOI] [PubMed] [Google Scholar]
- Kirby D. Emerging answers, 2007: Research findings on programs to reduce teen pregnancy and sexually transmitted diseases (report) National Campaign to Prevent Teen and Unplanned Pregnancy; Washington, DC: 2007. [Google Scholar]
- Kirby JB. Poor people, poor places and access to health care in the United States. Social Forces. 2008;87:325–355. [Google Scholar]
- Kost K, Henshaw S. U.S. teenage pregnancies, births and abortions, 2008: National trends by age, race and ethnicity (report) Guttmacher Institute; New York, NY: 2012. Retrieved from https://www.guttmacher.org/pubs/USTPtrendsState08.pdf. [Google Scholar]
- Laumann EO, Youm Y. Racial/ethnic group differences in the prevalence of sexually transmitted diseases in the United States: A network explanation. Sexually Transmitted Diseases. 1999;23:250–261. doi: 10.1097/00007435-199905000-00003. [DOI] [PubMed] [Google Scholar]
- Lesthaeghe RJ, Neidert L. The second demographic transition in the United States: Exception or textbook example? Population and Development Review. 2006;32:669–698. [Google Scholar]
- Longmore MA, Eng AL, Giordano PC, Manning WD. Parenting and adolescents’ sexual initiation. Journal of Marriage and Family. 2009;71:969–982. doi: 10.1111/j.1741-3737.2009.00647.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Lopoo LM, Western B. Incarceration and the formation and stability of marital unions. Journal of Marriage and Family. 2005;67:721–734. [Google Scholar]
- Malat J. Racial differences in Norplant use in the United States. Social Science & Medicine. 2000;50:1297–1308. doi: 10.1016/s0277-9536(99)00377-9. [DOI] [PubMed] [Google Scholar]
- Manlove J, Logan C, Moore KA, Ikramullah E. Pathways from family religiosity to adolescent sexual activity and contraceptive use. Perspectives on Sexual and Reproductive Health. 2008;40:105–117. doi: 10.1363/4010508. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Manlove J, Terry-Humen E. Contraceptive use patterns within females’ first sexual relationships: The role of relationships, partners, and methods. Journal of Sex Research. 2007;44:3–16. doi: 10.1080/00224490709336788. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Manlove JS, Terry-Humen E, Ikramullah EN, Moore KA. The role of parent religiosity in teens’ transitions to sex and contraception. Journal of Adolescent Health. 2006;39:578–587. doi: 10.1016/j.jadohealth.2006.03.008. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Martinez G, Copen CE, Abma JC. Teenagers in the United States: Sexual activity, contraceptive use, and childbearing, 2006–2010 National Survey of Family Growth. National Center for Health Statistics; Washington, DC: 2011. (Vital and Health Statistics Report Series 23, No. 31) [PubMed] [Google Scholar]
- Martinez G, Daniels K, Chandra A. Fertility of men and women aged 15–44 years in the United States: National Survey of Family Growth, 2006–2010. National Center for Health Statistics; Hyattsville, MD: 2012. (National Health Statistics Reports, No. 51) [PubMed] [Google Scholar]
- Mayer KU. Whose lives? How history, societies, and institutions define and shape life courses. Research in Human Development. 2004;1:161–187. [Google Scholar]
- McBride CK, Paikoff RL, Holmbeck GN. Individual and familial influences on the onset of sexual intercourse among urban African American adolescents. Journal of Consulting and Clinical Psychology. 2003;71:159–167. doi: 10.1037//0022-006x.71.1.159. [DOI] [PubMed] [Google Scholar]
- Meade CS, Kershaw TS, Ickovics JR. The intergenerational cycle of teenage motherhood: An ecological approach. Health Psychology. 2008;27:419–429. doi: 10.1037/0278-6133.27.4.419. [DOI] [PubMed] [Google Scholar]
- Meadows-Oliver M. Homeless adolescent mothers: A metasynthesis of their life experiences. Journal of Pediatric Nursing. 2006;21:340–349. doi: 10.1016/j.pedn.2006.02.004. [DOI] [PubMed] [Google Scholar]
- Mirowsky J, Ross CE, Reynolds J. Links between social status and health status. In: Bird CE, Conrad P, Fremont AM, editors. Handbook of medical sociology. 5th ed Prentice Hall; Upper Saddle River, NJ: 2000. pp. 47–67. [Google Scholar]
- Mosher WD, Jones J, Abma JC. Intended and unintended births in the United States: 1982–2010. National Center for Health Statistics; Hyattsville, MD: 2012. (National Health Statistics Reports, No. 55) Retrieved from http://198.246.124.22/nchs/data/nhsr/nhsr055.pdf. [PubMed] [Google Scholar]
- Newcomer SF, Udry JR. Mother’s influence on the sexual behavior of their teenage children. Journal of Marriage and the Family. 1984;46:477–485. [Google Scholar]
- Oliver ML, Shapiro TM. Black wealth, white wealth: A new perspective on racial inequality. 2nd ed Routledge; New York, NY: 2006. [Google Scholar]
- Orr AJ. Black-white differences in achievement: The importance of wealth. Sociology of Education. 2003;76:281–304. [Google Scholar]
- Osborn F. Development of a eugenic philosophy. American Sociological Review. 1937;2:389–397. [Google Scholar]
- Owusu-Edusei K, Jr., Chesson HW, Leichliter JS, Kent CK, Aral SO. The association between racial disparity in income and reported sexually transmitted infections. American Journal of Public Health. 2013;103:910–916. doi: 10.2105/AJPH.2012.301015. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Pavao J, Alvarez J, Baumrind N, Induni M, Kimerling R. Intimate partner violence and housing instability. American Journal of Preventive Medicine. 2007;32:143–146. doi: 10.1016/j.amepre.2006.10.008. [DOI] [PubMed] [Google Scholar]
- Pearson J, Muller C, Frisco ML. Parental involvement, family structure, and adolescent sexual decision making. Sociological Perspectives. 2006;49:67–90. [Google Scholar]
- Presser HB. The role of sterilization in controlling Puerto Rican fertility. Population Studies. 1969;23:343–361. doi: 10.1080/00324728.1969.10405290. [DOI] [PubMed] [Google Scholar]
- Proctor BD, Dalaker J. Poverty in the United States: 2001. U.S. Government Printing Office; Washington, DC: 2002. (Current Population Reports, No. P60-219) [Google Scholar]
- Reilly PP. The surgical solution: A history of involuntary sterilization in the United States. Johns Hopkins University Press; Baltimore, MD: 1991. [Google Scholar]
- Robert SA, House JS. Socioeconomic inequalities in health: Integrating individual-, community-, and societal-level theory and research. In: Albrecht G, Fitzpatrick R, Scrimshaw S, editors. Handbook of social studies in health and medicine. Sage; London, UK: 2000. pp. 115–136. [Google Scholar]
- Roberts DE. Forum: Black women and the Pill. Family Planning Perspectives. 2000;32:89–90. [PubMed] [Google Scholar]
- Rocca CH, Harper CC. Do racial and ethnic differences in contraceptive attitudes and knowledge explain disparities in method use? Perspectives on Sexual and Reproductive Health. 2012;44:150–158. doi: 10.1363/4415012. [DOI] [PubMed] [Google Scholar]
- Shih G, Vittinghoff E, Steinauer J, Dehlendorf C. Racial and ethnic disparities in contraceptive method choice in California. Perspectives on Sexual and Reproductive Health. 2011;43:173–180. doi: 10.1363/4317311. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Smedley BD, Stith AY, Nelson AR, editors. Unequal treatment: Confronting racial and ethnic disparities in health care. National Academies Press; Washington, DC: 2006. Retrieved from http://www.iom.edu/Reports/2002/Unequal-Treatment-Confronting-Racial-and-Ethnic-Disparities-in-Health-Care.aspx. [PubMed] [Google Scholar]
- South SJ, Baumer EP. Deciphering community and race effects on adolescent premarital childbearing. Social Forces. 2000;78:1379–1407. [Google Scholar]
- Sprecher S. Predictors of condom use in first sexual intercourse: A consideration of individual, situational, relational, and cohort effects. Journal of Applied Social Psychology. 2013;43:E71–E84. [Google Scholar]
- Stern AM. Sterilized in the name of public health: Race, immigration, and reproductive control in modern California. American Journal of Public Health. 2005;95:1128–1138. doi: 10.2105/AJPH.2004.041608. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Stubblefield A. “Beyond the pale”: Tainted whiteness, cognitive disability, and eugenic sterilization. Hypatia. 2007;22(2):162–181. [Google Scholar]
- Thorburn S, Bogart LM. Conspiracy beliefs about birth control: Barriers to pregnancy prevention among African Americans of reproductive age. Health Education & Behavior. 2005;32:474–487. doi: 10.1177/1090198105276220. [DOI] [PubMed] [Google Scholar]
- Thornton A, Camburn D. The influence of the family on premarital sexual attitudes and behavior. Demography. 1987;24:323. [PubMed] [Google Scholar]
- Trussell J, Vaughan B. Contraceptive failure, method-related discontinuation and resumption of use: Results from the 1995 National Survey of Family Growth. Family Planning Perspectives. 1999;31:64–72. 93. [PubMed] [Google Scholar]
- Vaughan B, Trussell J, Kost K, Singh S, Jones R. Discontinuation and resumption of contraceptive use: Results from the 2002 National Survey of Family Growth. Contraception. 2008;78:271–283. doi: 10.1016/j.contraception.2008.05.007. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Welti K, Wildsmith E, Manlove J. Trends and recent estimates: Contraceptive use among U.S. teens and young adults. Child Trends; Washington, DC: 2011. (Child Trends Research Brief, No. 2011-23) [Google Scholar]
- Western B, Bloome D, Sosnaud B, Tach L. Economic insecurity and social stratification. Annual Review of Sociology. 2012;38:341–359. [Google Scholar]
- Whitehead TL. Urban low-income African American men, HIV/AIDS, and gender identity. Medical Anthropology Quarterly. 1997;11:411–447. doi: 10.1525/maq.1997.11.4.411. [DOI] [PubMed] [Google Scholar]
- Williams DR, Collins C. US socioeconomic and racial differences in health: Patterns and explanations. Annual Review of Sociology. 1995;21:349–386. [Google Scholar]
- Wilson WJ. The truly disadvantaged: The inner-city, the underclass and public policy. University of Chicago Press; Chicago, IL: 1987. [Google Scholar]
- Wilson WJ. When work disappears: The world of the new urban poor. Knopf; New York, NY: 1996. [Google Scholar]
- Wilson WJ, Neckerman KM. Poverty and family structure: The widening gap between evidence and public policy issues. In: Danziger S, Weinberg DH, editors. Fighting poverty: What works and what doesn’t. Harvard University Press; Cambridge, MA: 1986. pp. 232–259. [Google Scholar]