Abstract
Background
Resilience strategies are what we use to avoid and recover from error. In this study, we used the grounded theory approach to evaluate the resilience of Japanese patients with Type 1 diabetes.
Methods
Semi-structured interviews were conducted with 15 adults with Type 1 diabetes. Then, using grounded theory, we created a new model of resilience in this population.
Results
The results suggested a core category, “to make progress along the resilience path,” comprising seven concepts classified into three stages. These seven concepts were as follows: “suffering from treatment,” “damaged trust as a person,” “persistence of afflictions,” “awareness of supporters,” “joy to be kept alive by insulin,” “actively seeking a future,” “being able to manage by oneself.” Individuals with Type 1 diabetes used difficult experiences to motivate their resilience and to improve their situation. Additionally, resilience was an important contributor to these individuals’ beliefs in their ability to face difficulties, to accept their illness and insulin therapy, and to control their illness. Resilience was also important to these individuals’ faith in the future and in medical care. Our results are applicable to clinical care and research, such as the development of preventive interventions aimed at building or strengthening protective skills related to diabetes and its management.
Conclusion
Ultimately, our goal is to equip adults with Type 1 diabetes with the tools to obtain sufficient behavioral and health-related resilience. Furthermore, these results highlight that maintaining resilience-related coping skills is important for adults and indicate that different psychological processes underlie resilience across the lifespan.
Keywords: adult, comparative analysis, grounded theory, resilience, type 1 diabetes
Type 1 diabetes (T1D) is a disease characterized by deficient insulin production and it requires daily insulin administration.1 Patients with T1D require lifelong self-care, including daily management of their blood glucose levels to maintain their health and prevent future complications. Patients with T1D must suitably modify their behavior after diagnosis, and it is important that they learn to self-manage their condition.
Good self-managers have been defined as individuals who have learned the skills to cope with their illness, know how to continue with their daily activities, and can regulate their ever-changing emotions related to their chronic illness.2 For patients with T1D, self-management can be difficult because they experience physical, emotional, and social distress, and often need to communicate this to co-workers and supporters. Notably, however, while some T1D patients who face such distress struggle to manage it, others excel in doing so. This phenomenon is evident across the academic, social, and developmental domains. Those who excel in dealing with distress related to their disease are considered “resilient,” and these individuals are the focus of the present study. Resilience has been studied both domestically and internationally, and many studies of it have been considered to support “positive health” approaches. Thus, it is important to promote knowledge of resilience among both the research and lay populations.
Previous studies of patients with T1D have focused on the negative psychological aspects of their disease, such as anxiety, depressive symptoms, or feelings of struggle.3–6 Therefore, we focused on a positive aspect—namely, their resilience. Resilience has been defined as the capacity to deal with, overcome, learn from, or be transformed by life’s inevitable adversities.7–10 Resilient youths overcome challenges expected to derail them from their expected progress and demonstrate competence at or above common levels of functioning.11–13 People with chronic diseases often talk about how their diagnosis helped them to recognize their own resilience; that is, they felt able to tap into sources of strength and to be resourceful in ways that they had never thought possible. At the same time, one of life’s “curveballs,” or a series of curveballs, can leave anyone feeling depleted.
Hilliard and Harris (2012)11 performed a study of resilience theory regarding T1D management and control, wherein they constructed a theoretical model of pediatric (i.e., adolescent) T1D resilience. However, very little qualitative research is available of the resilience of people diagnosed with T1D, and none of it was conducted in Japan.
The aim was to clarify the process of resilience in adult Japanese patients with T1D and to devise a model of resilience in this population.
MATERIALS AND METHODS
Design
To ascertain a model of the resilience process in adults with T1D, we used the grounded theory method.14, 15 This method was used because it focuses on exploring processes and generating new understanding of these processes from available data.14, 15 It was suitable because it allowed us to use the participants’ own words to understand the effects of a T1D diagnosis on the meaning of resilience.
Participants
Inclusion criteria were being a Japanese speaker with T1D and being aged 20 years or over. All participants resided in Tottori Prefecture, Japan and were recruited from two diabetes outpatient clinics that specifically served adults with T1D. All patients were recruited from the short-term wards (i.e., wards for short-term care) in these clinics. Approximately 5% of patients who visit these wards have a diagnosis of T1D with hypoglycemia or hyperglycemia symptoms, and nurses in these wards provide self-care management and group therapy with the goal of discharge. We recruited 15 individuals with T1D who were recommended by health professionals, and whose reactions, behaviors, and facial expressions we had observed before conducting the study. Sampling was then used to continue recruitment until data saturation occurred. Sampling involved having participants recommend other participants to join the study because it was difficult to identify appropriate and willing participants. Details of the study were explained to all clinic patients, after which they were invited to participate; interested patients who agreed to participate contacted the researchers for further information.
Ethical considerations
This study was approved by the ethics committee of Tottori University (Record Number 2307, January 2013). Informed consent was obtained from all patients using the procedure approved by the ethics committee, and the confidentiality of the participants’ information was protected. Furthermore, they were told that they could stop the interview at any time they wished and could refuse to answer any unwanted questions. Pseudonyms were allocated to all the patients to ensure confidentiality and all data were stored securely during the research process.
Data collection
Data were collected from 15 patients with T1D between July 2013 and March 2014 via in-depth semi-structured interviews that took place in the clinic waiting rooms. The author conducted all interviews using a standardized interview schedule.
Participants were asked to share their experiences, since being diagnosed, of coping with self-management and diabetes control issues, the meaning of living with diabetes, and their support from family and friends. The participants were initially informed of the topics and then were asked to freely reflect on and discuss their experiences of living with T1D. Follow-up questions were posed to obtain more detailed descriptions or explanations. The interviews (which each lasted for 60–75 minutes) were audio-recorded, transcribed verbatim, and stored for analysis. Data collection was stopped when we reached saturation—namely, when no new findings or themes were extracted from newly collected data.
Data analysis
In grounded theory, data analysis follows a constant comparative method of simultaneous interviewing, transcribing, and analysis until data saturation occurs.14-15 Constant comparison methods involve concurrently asking questions, creating memos and diagrammatic records, and reading literature from data collection commencement until achievement of theoretical saturation.14–15 Before coding each interview, the first author listened to the interview tape several times and read the typed transcripts through completely. This ensured a full understanding of the raw data. The verbatim translations were then coded and analyzed in the same way as the interview transcripts. All transcripts were translated into English and subjected to the same coding and analysis process as the Japanese interview transcripts were. The results did not differ from the Japanese language analysis. The next step was line-by-line in vivo coding. The codes were then compared according to their differences and similarities and sorted into categories and subcategories. Subsequently, we identified the linkages among these categories and subcategories.
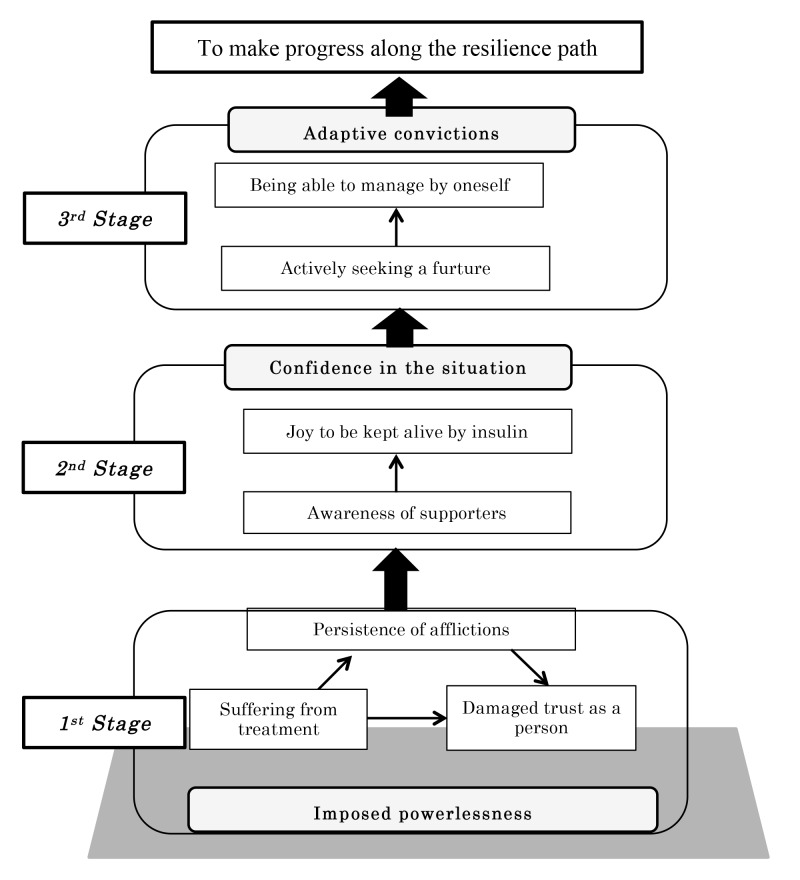
Finally, the core category was identified, which allowed us to build a new resilience model for T1D (Fig. 1). In other words, the core category—namely, the category to which all other subcategories are related—was named and used to build a conceptual framework of resilience in adult T1D patients. The core category was established upon completion of the 15th interview; this was confirmed in later interviews with participants who were interested in discussing the research, during which we explained the categories and subcategories to them. Data analysis was undertaken using the QSR NVivo 10 software (QSR International, Melbourne, Australia).
Fig. 1.
A model of resilience among adult Japanese patients with type 1 diabetes.
RESULTS
Table 1 shows the study participants’ basic attributes. Table 2 shows an outline of the concepts, subcategories, categories, and core category. The core category identified was “to make progress along the resilience path,” which comprised three categories: “imposed powerlessness,” “confidence in the situation,” and “adaptive convictions.” These categories, in turn, comprised seven concepts in three stages related to participants’ attempts to reduce stress and develop resilience in the face of adverse experiences from T1D. The concepts were as follows: “suffering from treatment,” “damaged trust as a person,” “persistence of afflictions,” “awareness of supporters,” “joy to be kept alive by insulin,” “actively seeking a future,” and “being able to manage by oneself.” Figure 1 shows the model of T1D resilience comprising “to make progress along the resilience path” and concepts related to it. The aforementioned processes formed three stages of coping with T1D.
Table 1.
Demographic characteristic of the 15 study participants with type 1 diabetes
| Participant characteristics | n | |
| Gender | ||
| Female | 13 | |
| Male | 2 | |
| Employment status | ||
| Full time | 7 | |
| Part time | 3 | |
| Unemployed | 5 | |
| Age groups (years old) | ||
| 20–30 | 1 | |
| 31–40 | 7 | |
| 41–50 | 3 | |
| 51–60 | 2 | |
| > 60 | 2 | |
| Time living with Type 1 diabetes (years) | ||
| < 5 | 8 | |
| 6–10 | 6 | |
| 11–20 | 0 | |
| > 21 | 1 | |
| Living | ||
| Alone | 6 | |
| Cohabiting | 9 | |
| †HbA1c (NGSP) (%) | 5.3–9.0 (7.1 ± 1.1) | |
| Insulin therapy | ||
| MDI | 12 | |
| CSII | 3 | |
†glycated hemoglobin.
CSII, continuous subcutaneous insulin infusion; MDI, multiple daily injection; NGSP, National Glycohemoglobin Standardization Program.
Table 2.
Outline of the concepts, subcategories, categories and core category
| Core Category | Category | Concept | Codes |
| To make progress along the resilience path | Imposed powerlessness | Suffering from treatment | Resistance to injections |
| Troubles related to injections | |||
| Presence of visible injection sites | |||
| Not correctly adjusting the insulin dose | |||
| Being unable to explain one’s suffering from hypoglycemia | |||
| Damaged trust as a person | Distorted view of character building | ||
| Not working because of sickness | |||
| Caregiver worry too much | |||
| Others have biased attitudes | |||
| Persistence of afflictions | Unable to avoid giving injections | ||
| Not talking about sickness | |||
| Resignation to absence of cure | |||
| Marginal physical ability | |||
| Confidence in the situation | Awareness of supporters | Presence of famous people | |
| Encouragement from other diabetics | |||
| Care from family | |||
| Cooperation with co-workers | |||
| Joy to be kept alive by insulin | Escaped death thanks to insulin | ||
| Adaptive convictions | Actively seeking a future | Advantage of experience | |
| Control of their situation | |||
| Realizing that this situation isn’t uncommon | |||
| Being able to manage by oneself | Living a normal life | ||
| Attitude of self-reliance | |||
| Creation of new lifestyle | |||
| Realization of gain from disease | |||
| Hope for a fresh start |
First stage: imposed powerlessness (suffering from treatment, damaged trust as a person, persistence of afflictions)
This first stage comprised three concepts describing how patients with T1D had strong negative feelings about their disease because of their numerous exhausting experiences related to it. However, they had no other choice but to endure these negative feelings, which gave them additional inner strength and led to the “resilience path.”
Suffering from treatment
This concept reflected participants’ experiences such as “troubles related to injections,” “not correctly adjusting the insulin dose,” and “being unable to explain one’s suffering from hypoglycemia.” Participants were highly aware of the “presence of visible injection sites,” which for them reinforced the notion that there is no cure for their lifelong disease. Furthermore, although patients with T1D understood that they had to continue with insulin therapy for the rest of their lives, they experienced a “resistance to injections”:
“I just hated injections. I didn’t like that I had to take a break from work to inject in the restroom.” (Participant B)
“Adjusting my insulin dose according to the volume I eat is a little stressful. The pain of injecting [insulin] hasn’t been a problem. I worry [instead] about the numbers [blood sugar levels] and about messing up the dose because I don’t quite know how to adjust it.” (Participant K)
“My job kept me so busy that I had no time for it [the insulin injection]. I didn’t even have time to eat. Therefore, results were always bad on my regular [clinic] visits. I couldn’t do anything about it. It became a kind of dilemma for many years. I was sometimes reluctant to go to the clinic knowing that I would be told something bad [by the doctor] or get scolded again.” (Participant J)
Damaged trust as a person
Some participants had negative experiences when disclosing their feelings to others because others reacted poorly to the participant’s disclosures. This led to participants’ trust being unconsciously damaged around others and shutting them out. Often, participants reported feeling emotionally unstable for a number of reasons: “caregivers worry too much” and “others have biased attitudes.” Participants had to cope with “not working because of sickness,” which caused them to feel socially isolated from others. Notably, some disclosed their private experiences about coping with T1D to members of patient-support programs and received considerable sympathy by having done so.
Participants were highly aware of their worsening relationships with others because of others’ insensitive words and behaviors. Furthermore, they experienced a “distorted view of character building” when others suddenly softened their attitudes toward them:
“People built a wall around me. They treated me like a sick person. They felt they should not invite me out. They asked me if I could eat this and that and I would say, “Yes, of course!” (Participant D)
“When I first developed symptoms of T1D, I told people [around me] about it. But, I gradually shut down because people said things that hurt my feelings when I mentioned the disease. I have learned to hide my condition ever since.” (Participant O)
“I didn’t like it when people treated me like an invalid just because I had this condition. They said things like “Don’t you have to get an [insulin] injection?” or “Are you okay?” over and over again.” (Participant E)
“I was told by my boss that I could not be a caregiver because my body required care. I basically got fired.” (Participant B)
Persistence of afflictions
The concept of “persistence of afflictions” refers to the phenomenon in which patients endured increased suffering because of “resignation to the absence of a cure” and having to live with the disease. Patients with T1D felt that others did not understand the disease and that they had a prejudiced view of those with chronic illnesses. This led to embarrassment and feelings of despair due to “not talking about their sickness.” Furthermore, participants had to cope with absence due to sickness and not working, which caused them to feel socially isolated from others. They reported being deeply hurt by others’ careless behaviors and shut them out.
Patients with T1D experienced a range of daily life restrictions, such as “marginal physical ability”; they did not feel free. Participants were also “unable to avoid giving injections,” which reinforced the notion that there is no cure for their lifelong disease:
“Well, I felt comfortable [talking about the disease] with some people at work. One day, I casually mentioned my condition. This person I talked to advised me to tell our boss. I was told that he should know so that he could prepare for when something happens. I simply couldn’t tell our boss.” (Participant B)
“The things I used to do without any problems are now difficult because of hypoglycemic reactions. For example, [it used to be that] when I cleaned, I was able to do it all day long without feeling tired but now I can’t. I have to take that [my condition] into account [when doing anything].” (Participant A)
“The fact that I had to give myself an insulin injection made me realize that I had a disease. I used to feel that way every time I injected insulin back then.”
Second stage: confidence in the situation (awareness of supporters, joy to be kept alive by insulin)
This stage comprised two concepts that outlined how patients with T1D gradually bridge a gap from their pain.
Awareness of supporters
This stage described how participants became aware of the support that they received from others to overcome their difficulties. Participants were able to talk freely about their physical, emotional, and social distress with other patients with T1D (“encouragement from other diabetics”), which helped them to become more resilient. Furthermore, the knowledge that famous people also suffered from T1D made participants feel more positive about their future expectations (“presence of famous people”). “Care from family” and “cooperation with co-workers” represented how patients with T1D became conscious of avoiding hypoglycemia and were often given a room wherein they could perform insulin injections privately:
“When I got the disease, the doctor and nurses told me about people with diabetes who are famous in society; for example, professional athletes. That kind of information made me realize that I didn’t need to change and it was okay to stay the way I was.” (Participant G)
“When I was hospitalized, my doctor introduced me to another patient from the same generation. We became good friends and this friendship really saved me.” (Participant A)
“I went [back] to work after I got out of the hospital. People [at work] were worried about hypoglycemia and always gave me sweets. It was a nice environment.” (Participant I)
Joy to be kept alive by insulin
This concept involved participants’ experiences of having “escaped death thanks to insulin”:
“When I was diagnosed with T1D, I was very happy because I knew I could get treatment. If an insulin injection enables me to work, that’s a good thing.” (Participant J)
Third stage: adaptive convictions (actively seeking a future and being able to manage by oneself)
This stage comprised two concepts that outlined how patients with T1D gradually overcame their difficulties. It reflected how participants learned strategies to overcome their difficulties from experience and thereby acquire a state of “making progress along the resilience path.”
Actively seeking a future
Participants completely changed their lifestyles as a result of their T1D diagnosis. Although the diagnosis caused them to experience a loss of pleasure and enjoyment, they eventually became aware that their situation could only improve if they changed their negative mindset. Participants often could only take a step forward due to the “advantage of experience.” Indeed, as time passed, they experienced “realizing that this situation is not uncommon” and “receiving good treatment,” and were able to find sources of pleasure. By being confronted with an uncertain future, they were forced to perform careful assessments of their present status and capacity in order to “control their situation”:
“I was very happy [with this treatment]. I would give it an A++! I’ve been living with it [T1D] for years. I got it [an insulin injection] when I didn’t get to eat and other times I could not get it [an insulin injection] when I was able to eat. It was like that for many years. Now that I have the insulin pump, my condition has been stable.” (Participant J)
“I wasn’t working particularly hard. It wasn’t because I was sick. I did what I could. I asked for help with what I couldn’t do. I couldn’t work too much on what I wanted to do.” (Participant N)
“I decided not to let the disease affect the way I lived. Injecting [insulin] was what differentiated me from others but we lived in the same way after all. I just had to be careful of more things [than they did]. I tried not to think about it too much; I thought that this way of thinking was my strength.” (Participant M)
Being able to manage by oneself
Participants overcame their weaknesses by drawing on their experiences. For instance, they devised coping methods, such as “living a normal life” and “adopting an attitude of self-reliance,” which they used in the “creation of a new lifestyle.” Additionally, by drawing on their past experiences, they could obtain a clearer perspective of their future prospects. Ultimately, participants felt ready to “hope for a fresh start.” Furthermore, participants felt more positive and began to “expect medical advances”:
“Being aware of my disease, I set short-term goals, such as that I should try hard for three months or maintain a 5% (HbA1c) level for that three-month period. I split up the future into short periods and tried to feel happy about short-term goals.” (Participant I)
“I might not be able to get the kind of job I wish to, but I will and want to work someday. I [also] want to gradually start seeing the friends I stopped seeing again.” (Participant E)
“You know iPS [induced pluripotent stem] cells? I have read news articles that said they might cure the disease. I have really begun to hope that I could be free from having to inject insulin sometime soon.” (Participant H)
DISCUSSION
The results of this study indicated that patients with T1D experience three stages when developing resilience to face adversity. These three stages and related concepts formed a model of resilience for adults with T1D, centered on the core concept of “to make progress along the resilience path.” In this study, the characteristic of the process of acquiring resilience in our country produced a feeling of powerlessness related to the disease; however, T1D patients accepted the disease, and they could gradually manage their disease to acquire resilience. The resilience of T1D patients was important for reducing distress with T1D and to strengthen the management skills and processes related to diabetes. 11, 12, 24 The results of this study are the same as that of studies overseas.
The concepts inherent to each stage focused on individuals’ development of inner strength via external support and active personal effort. This is reminiscent of the definition of resilience used by Werner (1993),8 Rutter (1985),9 and Grotberg (2003)10: namely, being able to cope with and overcome difficulties and, in the process, becoming strengthened or transformed by these difficulties. These authors proposed that resilience in coping with diseases (including diabetes) could be organized into the factors of external support, inner strength, and interpersonal and problem-solving skills.
Regarding the structure of “to make progress along the resilience path,” previous qualitative research has shown that resilience is not a stable characteristic; rather, it is a constantly changing and developing construct,16, 17 as reflected in the 10 concepts extracted in the present study, which describe how adverse experiences stimulate and forge resilience.
The first stage involved their coping with various burdens, such as “suffering from treatment,” “damaged trust as a person,” and “persistence of afflictions.” At this stage, patients with T1D expressed negative feelings about their experiences. Nevertheless, insulin benefited their lives, so they endured the treatment. This endurance provided additional inner strength and led to functional resilience. This, in turn, resulted in greater emotional stability because of the balance of negative and positive experiences.
In the second stage (“awareness of supporters”), patients with T1D sought the support of others to help them overcome their difficult situation. During this stage, participants became dedicated to working through their crisis. They consulted with trusted others about their thoughts, which helped them to feel recognized and supported. Previous research has shown that sympathetic supporters are strong sources of encouragement for coping with difficult feelings.18–20 Furthermore, “joy to be kept alive by insulin” was considered the first stage because it reflected how patients with T1D began to appreciate that insulin was beneficial for their lives, which in turn helped to build their resilience.
In the third stage, which comprised the concepts of “actively seeking a future” and “being able to manage by oneself,” patients with T1D felt weak and struggled with the various restrictions of their disease; for instance, they felt “wounded” and experienced despair. Consequently, however, they experienced a state of emotional and mental maturation; by enduring difficulty, they realized the meaning of truly being alive. This process of growth suggested that they had adopted a new mental state in which they could accept their own feelings. Furthermore, they were not confused by others’ opinions. Relatedly, Travelbee (1971)21 reported that acceptance does not differ from optimism; in other words, people who accept their difficulties can overcome them. This was very similar to the process of resilience described herein, where patients with T1D learned to accept their difficulties. Affleck and Tennen (1996)22 similarly reported the benefits of perceived positive changes in personality, such as the development of greater patience, tolerance, empathy, and courage. Other common benefits are positive changes in values, life priorities, and personal goals.
In this study, a key aspect of the participants’ realization of functional perpetual resilience was talking with supporters about their experiences. This is notable because nurses, being closely acquainted with patients, can be directly involved in eliciting patients’ resilience.23, 24 To do so, however, nurses must first understand the totality of patients’ accumulated experiences of their disease. This qualitative study highlights the process of resilience that patients with T1D experience in managing their diabetes and responding to new social circumstances. By studying resilience and exploring the possibilities presented by resilience-based interventions, practitioners from many fields could capitalize on a number of unique opportunities for promoting positive adaptation.16 Functional perpetual resilience underpins other resilience strategies used by patients with T1D to stay well, minimize psychological maladjustment, and improve mental health. Many patients experience T1D as a catastrophic life event, after which they must confront related challenges. Thus, resilience can be considered both a positive and negative consequence of T1D.
Our results indicate that nurses must understand patients’ experience of T1D in terms of both the social and psychological perspectives. Furthermore, the findings suggest that providers might consider asking patients with T1D how they manage the disease and accept their disease through insulin therapy, as well as their expectations for medical care and hopes for the future.
In summary, resilient adults with T1D can offer researchers practical, clinically relevant lessons and strategies to support those who struggle with the same condition. Through a synergistic emphasis on both alleviation of symptoms and promotion of positive processes in clinical care and research, we can prepare adults with T1D to respond well to disease-related challenges and, ultimately, set the stage for resilient behavioral and health outcomes.
Limitations
The main limitation of this study was that participants were recruited from only two clinics in one prefecture of Japan; thus, the results cannot be generalized to the whole country. We recruited 15 individuals with T1D, who were recommended by health professionals, for this study; however, this may have introduced bias into the participant selection because they had an experience of resilience. In addition, this study did not include participants who had difficulty in the acquisition of resilience.
Furthermore, this study was cross-sectional. Therefore, the impact of the resilience development process of diabetes must be explored in larger longitudinal studies.
Acknowledgments
Ackonwlegments: We thank all patients with type 1 diabetes who participated in this study.
The authors declare no conflict of interest.
REFERENCES
- 1. American Diabetes Association. Standard of medical care in diabetes 2015. Diabetes Care. 2015;38:S5-S76. 25537709 [Google Scholar]
- 2. Lorig K, Holman H, Sobel D, Laurent D, Gonzalez V, Minor M. Living a Healthy Life with Chronic Conditions. 3rd ed Boulder: Bull Publishing Company; 2006. p.317-41. [Google Scholar]
- 3. Patel N, Eborall H, Khunti K, Davies M J, Stone M A. Disclosure of Type 1 Diabetes Status: A Qualitative Study in a Mixed South Asian Population in Central England. Diversity Health Care. 2011;8:217-23. [Google Scholar]
- 4. Polonsky W H, Fisher L, Earles J, Dudl R J, Lees J, Mullan J, Jackson R A, et al. Assessing Psychosocial Distress in Diabetes Development of the Diabetes Distress Scale. Diabetes Care. 2005;28:626-31. [DOI] [PubMed] [Google Scholar]
- 5. Rasmussen B, Ward G, Jenkins A, King S J, Dunning T. Young Adults’ Management of Type 1 Diabetes During Life Transitions. J Clin Nurs. 2011;20:1981-92. [DOI] [PubMed] [Google Scholar]
- 6. Zoffmann V, Kirkevold M. Relationships and Their Potential for Change Developed in Difficult Type 1 Diabetes. Qual Health Res. 2007;17:625-38. [DOI] [PubMed] [Google Scholar]
- 7. [The Road to Resilience: What is Resilience?] [Internet]. Washington, DC: American Psychological Association; [cited 2016 April 26]. Available from: http://www.apa.org/helpcenter/road-resilience.aspx. [Google Scholar]
- 8. Grotberg EH, Resilience for Today: Gaining Strength from Adversity. Greenwood: Praeger Publishers; 2003. p.1-3. [Google Scholar]
- 9. Rutter M. Resilience in the Face of Adversity. Protective Factors and Resistance to Psychiatric Disorder. Br J Psychiatry. 1985;147:598-611. [DOI] [PubMed] [Google Scholar]
- 10. Werner E E. Risk Resilience and Recovery: Perspectives from the Kauai Longitudinal Study. Development and Psychopathology. 1993;5:505-13. [Google Scholar]
- 11. Hilliard M E, Harris M A, Weissberg-Benchell J. Diabetes Resilience: A Model of Risk and Protection in Type 1 Diabetes. Curr Diab Rep. 2012;12:739-48. [DOI] [PubMed] [Google Scholar]
- 12. Jaser S S, White L E. Coping and Resilience in Adolescents with Type 1 Diabetes. Child Care Health Dev. 2011;37:335-42. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13. Livingstone W, Mortel TF, Taylor B. A Path of Perpetual Resilience: Exploring the Experience of a Diabetes-related Amputation through Grounded Theory. Contemp Nurse. 2011;39:20-30. [DOI] [PubMed] [Google Scholar]
- 14. Glaser BG, Strauss A, The Discovery of Grounded Theory: Strategies for Qualitative Research. Hawthorne NY: Aldine de Gruyter; 1967. p.37-46. [Google Scholar]
- 15. Glaser BG, Basics of Grounded Theory Analysis. Mill Valley, CA: Sociology Press; 1992. p.101-16. [Google Scholar]
- 16. Earvolino-Ramirez M. Resilience: A Concept Analysis. Nursing Forum. 2007;42:73-82. [DOI] [PubMed] [Google Scholar]
- 17. Gooding P A, Hurst A, Johnson J, Tarrier N. Psychological Resilience in Young and Older Adults. Int J Geriatr Psychiatry. 2012;27:262-70. [DOI] [PubMed] [Google Scholar]
- 18. Sjölander C, Berterö C. The Significance of Social Support and Social Networks Among Newly Diagnosed Lung Cancer Patients in Sweden. Nurs Health Sci. 2008;10:182-7. [DOI] [PubMed] [Google Scholar]
- 19. West C, Stewart L, Foster K, Usher K. The Meaning of Resilience to Persons Living with Chronic Pain: An Interpretive Qualitative Inquiry. J Clin Nurs. 2012;21:1284-92. [DOI] [PubMed] [Google Scholar]
- 20. Williams S, Murray C. The Lived Experience of Older Adults’ Occupational Adaptation Following a Stroke. Aust Occup Ther J. 2013;60:39-47. [DOI] [PubMed] [Google Scholar]
- 21. Travelbee J, Interpersonal Aspects of Nursing. (2nd ed) Philadelphia: FA Davis Company; 1971. p.217-8. [Google Scholar]
- 22. Affleck G, Tennen H. Constructing Benefits from Adversity: Adaptation Significance and Dispostional Underpinnings. J Pers. 1996;64:899-922. [DOI] [PubMed] [Google Scholar]
- 23. Steinhard M A, Mamerow M M, Brown S A, Jolly C A. A Resilience Intervention in African American Adults with Type 2 Diabetes: A Pilot Study of Efficacy. Diabetes Educ. 2009;35:274-84. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24. Yi-Frazier J P, Smith R E, Vitaliano P P, Yi J C, Mai S, Hillman M, Weinger K. A Person-Focused Analysis of Resilience Resource and Coping in Patients with Diabetes. Stress Health. 2009;26:51-60. [DOI] [PMC free article] [PubMed] [Google Scholar]