Abstract
Nonhuman primate (NHP) models of Ebola virus (EBOV) infection primarily use parenteral or aerosol routes of exposure. Uniform lethality can be achieved in these models at low doses of EBOV (≤100 plaque-forming units [PFU]). Here, we exposed NHPs to low doses of EBOV (Makona strain) by the oral or conjunctival routes. Surprisingly, animals exposed to 10 PFU by either route showed no signs of disease. Exposure to 100 PFU resulted in illness and/or lethal infection. These results suggest that these more natural routes require higher doses of EBOV to produce disease or that there may be differences between Makona and historical strains.
Keywords: Ebola virus, pathogenesis, nonhuman primate
The filoviruses, Ebola virus and Marburg virus, are among the most lethal human pathogens, with case-fatality rates of up to 90% [1]. The recent outbreak of Zaire ebolavirus (ZEBOV) infection in West Africa, with 28 638 cases and 11 316 fatalities, is the largest ever recorded [2]. This outbreak differs substantially from previous outbreaks not only in the number of people affected but also in the duration and geographic range. Natural questions arise as to why this outbreak is so different from past episodes. Poor public health infrastructure of the affected countries has been attributed as one factor. It is also possible that factors related to differences in virulence or transmissibility of the Makona strain of ZEBOV that caused the outbreak could have also played a role [3]. Filoviruses are transmitted by close contact with infected patients or contact with infectious body fluids. In natural settings, it is presumed that filoviruses gain entry to the host either through small abrasions in the skin or by contact with mucous membranes.
Previous studies in nonhuman primates (NHPs) with filoviruses have shown that very low doses of virus can be lethal. Specifically, for the Angola strain of Marburg virus, intramuscular injection of either 1 plaque-forming unit (PFU) or 10 PFU is uniformly lethal in cynomolgus monkeys [4], whereas small-particle aerosol delivery of doses ranging from 2 PFU to 59 PFU is also uniformly lethal [5]. For Sudan ebolavirus, aerosol exposure of cynomolgus monkeys to 50 PFU is uniformly lethal [6]. In regard to ZEBOV, intraperitoneal exposure of cynomolgus monkeys to 6 PFU of the Mayinga strain [7] or intramuscular exposure to 18 PFU of the Kikwit strain [8] caused uniform lethality. Additionally, Reed et al concluded that the median lethal dose of the Kikwit strain for small-particle aerosol exposure in cynomolgus monkeys is <10 PFU [9]. While numerous studies have used parenteral or aerosol routes of exposure in macaques, only 1 study has assessed transmission of a filovirus by oral or conjunctival exposure. Specifically, Jaax et al showed that oral or conjunctival exposure of rhesus monkeys to high doses (158 000 PFU) of the Mayinga strain of ZEBOV caused a lethal infection [10]. However, no study has assessed low-dose exposure of any filovirus by the oral or conjunctival routes. Here, we performed a narrowly focused study to examine whether mucosal exposure of cynomolgus monkeys to low doses of the Makona strain of ZEBOV can produce a lethal infection.
MATERIALS AND METHODS
Challenge Virus
The ZEBOV Makona strain seed stock originated from serum from a fatal case during the 2014 outbreak in Guékédou, Guinea (ZEBOV isolate Homo sapiens-wt/GIN/2014/
Makona-Gueckedou-C07, accession number KJ660347.2) and was passaged twice in authenticated Vero E6 cells obtained from ATCC (ATCC, CRL-1586) [11, 12].
Animal Challenge
Six healthy adult cynomolgus macaques (Macaca fascicularis) of Chinese origin (weight range, 4.3–7.0 kg; age range, 4–8 years) were used for these studies. In an initial study, 2 animals were exposed to a target dose of 10 PFU of ZEBOV Makona by droplet administration into the medial canthus of each eye, whereas 2 animals were exposed to a target dose of 10 PFU of ZEBOV Makona by droplet administration to the oropharynx. In a second study, 1 animal was exposed to a target dose of 100 PFU of ZEBOV Makona by droplet administration into the medial canthus of each eye, while 1 animal was exposed to a target dose of 100 PFU of ZEBOV Makona by droplet administration to the oropharynx. All 6 animals underwent physical examinations, had swab specimens collected from mucosal surfaces, and had blood specimens collected at the time of challenge and on days 2, 3, 4, 5, 6, 7, 8, 10, 15, 21, and 28 (for the 10 PFU study) or 3, 5, 7, 9, 14, 21, and 28 (for the 100 PFU study) after virus challenge. Any surviving animals were euthanized on day 28.
Animal studies were completed under biosafety level 4 biocontainment at the Galveston National Laboratory (GNL) and were approved by the University of Texas Medical Branch (UTMB) Institutional Laboratory Animal Care and Use Committee, in accordance with state and federal statutes and regulations relating to experiments involving animals, and the UTMB Institutional Biosafety Committee.
Detection of Viremia and Viral RNA
RNA was isolated from samples using the Viral RNAMini Kit or RNeasy Kit (Qiagen), using 100 µL of blood/swab in 600 µL of buffer AVL or 100 mg of tissue, respectively, per the manufacturer's instructions. Primers/probe targeting the VP30 gene of all known ZEBOV strain sequences were used for quantitative reverse transcription polymerase chain reaction (qRT–PCR), with the probe used here being 6-carboxyfluorescein (6FAM)-59-CCGT CAATCAAGGAGCGCCTC39-6 carboxytetramethylrhodamine (TAMRA) (Life Technologies). ZEBOV RNA was detected using the CFX96 detection system (BioRad) in One-step probe qRT–PCR kits (Qiagen), with cycle conditions and genomic RNA standard determination as previously described [11, 12]. Virus titration was performed by a plaque assay with Vero E6 cells obtained from plasma samples as previously described [11, 12]. In brief, increasing 10-fold dilutions of the samples were adsorbed to Vero E6 monolayers in duplicate wells (200 µL); the limit of detection was 5 PFU/mL.
Hematologic and Serum Biochemical Analysis
Total white blood cell counts, white blood cell differentials, red blood cell counts, platelet counts, hematocrit values, total hemoglobin concentrations, mean cell volumes, mean corpuscular volumes, and mean corpuscular hemoglobin concentrations were analyzed in blood specimens collected in tubes containing ethylenediaminetetraacetic acid, using a laser based hematologic analyzer (Beckman Coulter). Serum samples were tested for concentrations of albumin, amylase, alanine aminotransferase, aspartate aminotransferase, alkaline phosphatase, γ glutamyl transferase, glucose, cholesterol, total protein, total bilirubin, blood urea nitrogen, creatinine, and C-reactive protein by using a Piccolo point-of-care analyzer and Biochemistry Panel Plus analyzer discs (Abaxis).
Histopathologic and Immunohistochemical (IHC) Analyses
Necropsy was performed on all subjects. Tissue samples from major organs were collected for histopathological and IHC examination, immersion fixed in 10% neutral buffered formalin, and processed for histopathologic analysis as previously described [11, 12]. For IHC analysis, specific anti-ZEBOV immunoreactivity was detected using an anti-ZEBOV VP40 protein rabbit primary antibody (Integrated BioTherapeutics) at a 1:4000 dilution. Tissue sections were processed for IHC analysis, using the Dako Autostainer (Dako). Secondary antibody used was biotinylated goat anti-rabbit immunoglobulin G (IgG; Vector Laboratories) at 1:200 followed by Dako LSAB2 streptavidin–horseradish peroxidase (Dako). Slides were developed with Dako DAB chromagen (Dako) and counterstained with hematoxylin. Nonimmune rabbit IgG was used as a negative control.
RESULTS AND DISCUSSION
No study has examined the pathogenicity of the Makona strain of ZEBOV in NHPs when given at low doses and using routes of exposure more likely to be associated with a natural outbreak. In an initial study, we exposed 4 cynomolgus macaques to a target dose of 10 PFU by either the oral route (2 animals) or the conjunctival route (2 animals; the actual dose of 10 PFU received was determined by back titration of each inoculum). Surprisingly, none of the 4 animals showed any evidence of clinical illness, and there were no changes in any hematologic or serum biochemical parameters during the course of the study (Table 1). No infectious virus was detected by plaque assay in plasma from any of the 4 animals, and viral RNA was below the limit of detection as assessed by qRT-PCR in whole-blood specimens from these animals. With the exception of the nasal swab obtained on day 10 from subject O-2 (1.62 × 105 genome copies/mL), all swab samples were negative for all 4 animals at all time points. We were unable to isolate infectious virus from the day 10 nasal swab samples from this animal. Analysis of sera from all 4 animals at days 21 and 28 after exposure showed only low anti-ZEBOV GP ELISA IgG titers in subject O-1 (1:100 at day 21 and 1:50 at day 28). Histopathologic and IHC staining for ZEBOV antigen revealed no significant lesions and no viral antigen present in tissues of any of the animals.
Table 1.
Clinical Description and Outcome of Zaire ebolavirus (ZEBOV)–Challenged Nonhuman Primates
| Subject No. | Sex | Route | Dose, PFU | Clinical Illness | Clinical Pathology | Viremia Level, Log10 PFU/mL | Anti-ZEBOV IgG Titer |
|---|---|---|---|---|---|---|---|
| O-1 | M | Oral | 10 | None, survived | None | 1:100 (21); 1:50 (28) | |
| O-2 | F | Oral | 10 | None, survived | None | 0 (21, 28) | |
| C-1 | M | Conjunctival | 10 | None, survived | None | 0 (21, 28) | |
| C-2 | F | Conjunctival | 10 | None, survived | None | 0 (21, 28) | |
| O-3 | M | Oral | 100 | Fever (d 7), loss of appetite (d 7–9), depression (d 7, 8), mild rash (d 7, 8), emesis (d 7), hematemesis (d 8), animal euthanized in the morning of d 8 | Leukocytosis (d 7, 8), thrombocytopenia (d 7, 8), hypoalbuminemia (d 8), >2-fold increase in ALT level (d 7), >7-fold increase in ALT level (d 8), >8-fold increase in AST level (d 7), >10-fold increase in AST level (d 8), >4-fold increase in ALP level (d 7), >7-fold increase in ALP level (d 8), >8-fold increase in BUN level (d 8), >5-fold increase in CRE level (d 8), >3-fold increase in GGT level (d 7), >6-fold increase in GGT level (d 8), >4-fold increase in CRP level (d 5), >10-fold increase in CRP level (d 7, 8) | 6.60 (d5); 8.75 (d7); 8.79 (d8) | NT |
| C-3 | M | Conjunctival | 100 | Loss of appetite (d 10), survived | Lymphopenia (d 7) | 1.70 (d14) | 1:50 (21) |
Days after ZEBOV challenge are in parentheses. Fever is defined as a temperature >1.4°C higher than the baseline level or either ≥0.7°C higher than baseline and ≥39.7°C or 0.6°C higher than baseline and ≥40°C. Mild rash is characterized by focal areas of petechiae covering <10% of the skin. Lymphopenia and thrombocytopenia are defined as a ≥35% drop in numbers of lymphocytes and platelets, respectively. Leukocytosis is defined by a ≥2-fold increase in the white blood cell count, compared with baseline. Hypoalbuminemia is defined by a ≥35% decrease in levels of albumin.
Abbreviations: ALP, alkaline phosphatase; ALT, alanine aminotransferase; AST, aspartate aminotransferase; BUN, blood urea nitrogen; CRE, creatinine; CRP, C-reactive protein; GGT, γ glutamyl transferase; IgG, immunoglobulin G; NT, not tested; PFU, plaque-forming units.
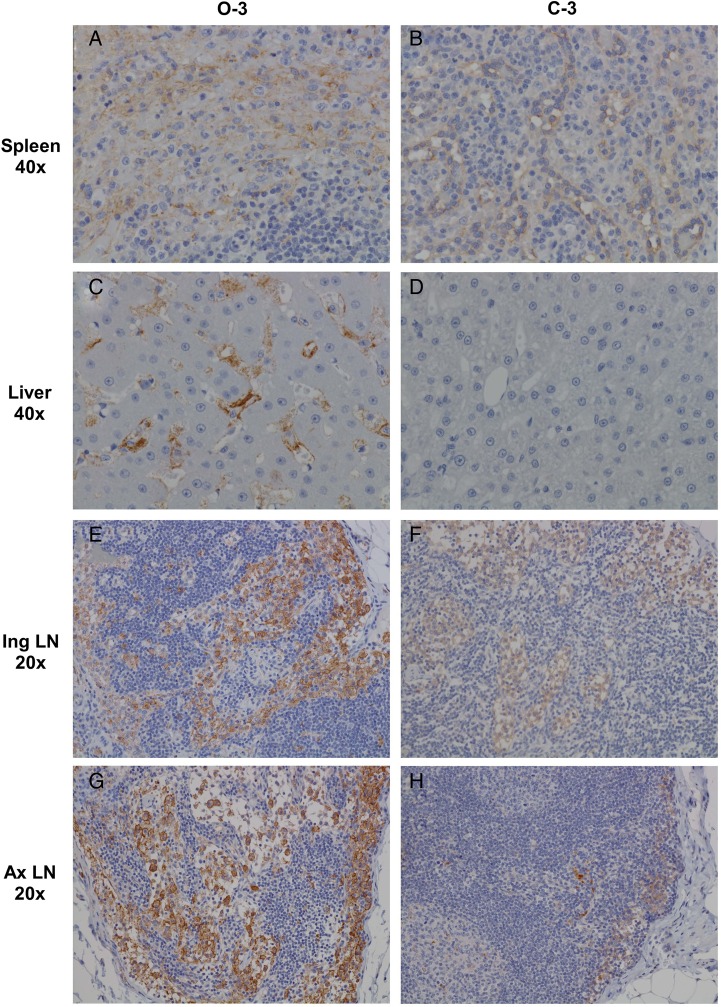
As it appeared that exposure of cynomolgus macaques to a very low dose of ZEBOV Makona by either the oral or conjunctival route did not result in a productive infection causing clinical disease, we performed a second study to determine whether exposure to a slightly higher dose would cause disease in macaques. Two animals were exposed to a target dose of 100 PFU by either the oral route (1 animal) or the conjunctival route (1 animal; actual doses of 120 PFU and 150 PFU were determined by back titration of the oral and conjunctival inocula, respectively). The animal exposed by the oral route (subject O-3) initially showed signs of clinical illness on day 7, which was characterized by fever, anorexia, and the presence of a macular rash (Table 1). This animal rapidly deteriorated and was euthanized on day 8 after infection. A high circulating viremia level was noted in subject O-3 beginning at day 5 and increasing at day 8. Lesions observed by histopathologic staining were consistent with ZEBOV infection and included histiocytosis of axillary and inguinal lymph nodes, lymphocytolysis of white pulp and deposition of fibrin in red pulp of spleen, sinusoidal leukocytosis, rare multifocal necrotizing hepatitis, and numerous pleomorphic intracellular eosinophilic viral inclusion bodies in hepatocytes. These lesions had correlative strong positive IHC staining for anti-ZEBOV VP40 antigen of mononuclear cells (macrophages, monocytes, and dendritic) in red and white pulp of the spleen, sinusoidal spaces of the liver and rare hepatocytes, and mononuclear cells within sinuses of the inguinal and axillary lymph nodes (Figure 1A, 1C, 1E, and 1G). Conversely, the animal exposed by the conjunctival route (subject C-3) did not show any evidence of clinical illness, with the exception of lymphopenia on day 7 and anorexia on day 10; this animal survived to the study end point (Table 1). Low-level viremia was detected by plaque assay at day 14 in plasma from subject C-3 (Table 1), while viral RNA genomes were detected by qRT-PCR in nasal swabs obtained on days 7 and 9 and the oral swab sample obtained on day 9. A low anti-ZEBOV GP enzyme-linked immunosorbent assay IgG titer (1:50) was noted in subject C-3 at day 21. Histopathologic examination of tissues from this animal failed to show lesions that were consistent with ZEBOV infection. However, weak positive IHC staining for anti-ZEBOV VP40 antigen of mononuclear cells in red pulp of the spleen and in subcapsular and medullary sinuses of the inguinal and axillary lymph nodes (Figure 1B, 1F, and 1H) was noted at the study end point, although the liver was free of any antigen-positive cells (Figure 1D).
Figure 1.
Comparison of Zaire ebolavirus (ZEBOV) antigen in representative tissues of cynomolgus monkeys infected via the oral or conjunctival routes. A, Stained spleen tissue section showing strong, diffuse cytoplasmic immunolabeling (brown) of dendriform mononuclear cells in the red and white pulp of a ZEBOV-orally infected animals. B, Stained spleen tissue section showing weak, diffuse cytoplasmic immunolabeling of the endothelium and rare dendriform mononuclear cells in the red pulp of a ZEBOV-conjunctivally infected animal. C, Stained liver tissue section showing strong, diffuse cytoplasmic immunolabeling of Kupffer cells and rare sinusoidal-lining cells and hepatocytes in a ZEBOV-orally infected animal. D, Stained liver tissue section showing no immunolabeling of ZEBOV-conjunctivally infected animal. E, Stained inguinal lymph node (Ing LN) section showing strong, diffuse cytoplasmic immunolabeling of dendriform mononuclear cells within the subcapsular and medullary sinuses in a ZEBOV-orally infected animal. F, Stained Ing LN section showing very weak, diffuse cytoplasmic immunolabeling of dendriform mononuclear cells within the subcapsular and medullary sinuses in a ZEBOV-conjunctivally infected animal. G, Stained axillary lymph node (Ax LN) showing strong, diffuse cytoplasmic immunolabeling of dendriform mononuclear cells within the subcapsular and medullary sinuses in a ZEBOV-orally infected animal. H, Stained Ax LN showing moderate, diffuse cytoplasmic immunolabeling of dendriform mononuclear cells within the subcapsular and medullary sinuses in a ZEBOV-conjunctivally infected animal. Spleen and liver representative images were taken at 40x original magnification and inguinal and axillary lymph node images at 20x original magnification from orally infected animal O-3 (A, C, E, and G) or conjunctivally infected animal C-3 (B, D, F, and H).
Previous studies have clearly demonstrated that low doses of the Kikwit or Mayinga strains of ZEBOV administered to macaques by parenteral injection or small-particle aerosol result in uniformly lethal disease [7–9]. Additionally, oral or conjunctival exposure of macaques to a high dose of ZEBOV Mayinga resulted in severe disease and near uniform lethality [10]. Our results show that low doses (10 PFU) of ZEBOV Makona administered by the oral or conjunctival routes resulted in minimal replication of virus and failed to cause a lethal infection. There are a number of possible explanations for this result. For example, the dose required to produce a lethal infection may be higher for exposure of conjunctival or pharyngeal mucosal membranes than for parenterally injected virus or small-particle aerosols delivered deep into the lungs. Each route represents different risks. Parenteral exposure simulates an accidental needle stick; aerosol exposure mimics deliberate release; and mucosal surface exposure simulates the most likely mode of contact during a natural outbreak. Current knowledge suggests that low-dose exposure from a laboratory accident or intentional release represents a significant risk of lethal ZEBOV infection to any exposed individual, whereas it appears that the threshold of the lethal dose for oral or conjunctival exposure may be at least ≥10-fold higher than parenteral or aerosol exposure. While this was a narrowly focused study, our findings are a first step to understanding how much infectious virus is needed for transmission to occur in a natural outbreak. Alternatively, as has been suggested in other studies, there may be phenotypic differences between the Makona strain and the historical Mayinga and Kikwit strains [3]. As in our current study, the numbers are still too low with the Makona strain to have a completely sound comparison with the Mayinga and Kikwit strains, but initial steps must be taken to further our understanding. Future studies should focus on determining whether low doses of ZEBOV Makona are lethal by the more conventional intramuscular route and by the small-particle aerosol route and to determine whether low doses of other ZEBOV strains are lethal if administered by the oral or conjunctival routes.
Notes
Acknowledgments. We thank the Animal Resource Center staff and the UTMB Research Histopathology Core at the UTMB and GNL for assistance.
Disclaimer. The opinions, interpretations, conclusions, and recommendations contained herein are those of the authors and are not necessarily endorsed by the UTMB at Galveston.
Financial support. This work was supported by the Department of Microbiology and Immunology, University of Texas Medical Branch at Galveston (to T. W. G.); and the National Institute of Allergy and Infectious Diseases (grant UC7AI094660).
Potential conflicts of interest. All authors: No reported conflicts. All authors have submitted the ICMJE Form for Disclosure of Potential Conflicts of Interest. Conflicts that the editors consider relevant to the content of the manuscript have been disclosed.
References
- 1.Feldmann H, Sanchez A, Geisbert TW. Filoviridae. In: Knipe DM, Howley PM, eds. Field's virology. Philadelphia, PA: Lippincott Williams & Wilkins, 2013:923–56. [Google Scholar]
- 2.World Health Organization. Ebola situation report, 2016. http://apps.who.int/iris/bitstream/10665/204172/1/ebolasitrep_20Jan2016_eng.pdf?ua=1. Accessed 4 April 2016.
- 3.Marzi A, Feldmann F, Hanley PW, Scott DP, Günther S, Feldmann H. Delayed disease progression in cynomolgus macaques infected with Ebola virus Makona strain. Emerg Infect Dis 2015; 21:1777–83. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Johnston SC, Lin KL, Twenhafel NA et al. . Dose response of MARV/Angola infection in cynomolgus macaques following IM or aerosol exposure. PLoS One 2015; 10:e0138843. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Alves DA, Glynn AR, Steele KE et al. . Aerosol exposure to the Angola strain of Marburg virus causes lethal viral hemorrhagic Fever in cynomolgus macaques. Vet Pathol 2010; 47:831–51. [DOI] [PubMed] [Google Scholar]
- 6.Zumbrun EE, Bloomfield HA, Dye JM et al. . A characterization of aerosolized Sudan virus infection in African green monkeys, cynomolgus macaques, and rhesus macaques. Viruses 2012; 4:2115–36. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Sullivan NJ, Sanchez A, Rollin PE, Yang ZY, Nabel GJ. Development of a preventive vaccine for Ebola virus infection in primates. Nature 2000; 408:605–9. [DOI] [PubMed] [Google Scholar]
- 8.Sullivan NJ, Geisbert TW, Geisbert JB et al. . Accelerated vaccination for Ebola virus haemorrhagic fever in non-human primates. Nature 2003; 424:681–4. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Reed DS, Lackemeyer MG, Garza NL, Sullivan LJ, Nichols DK. Aerosol exposure to Zaire ebolavirus in three nonhuman primate species: differences in disease course and clinical pathology. Microbes Infect 2011; 13:930–6. [DOI] [PubMed] [Google Scholar]
- 10.Jaax NK, Davis KJ, Geisbert TW et al. . Lethal experimental infection of rhesus monkeys with Ebola-Zaire (Mayinga) virus by the oral and conjunctival route of exposure. Arch Pathol Lab Med 1996; 120:140–55. [PubMed] [Google Scholar]
- 11.Mire CE, Matassov D, Geisbert JB et al. . Single-dose attenuated Vesiculovax vaccines protect primates against Ebola Makona virus. Nature 2015; 520:688–91. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Thi EP, Mire CE, Lee AC et al. . Lipid nanoparticle siRNA treatment of Ebola-virus-Makona-infected nonhuman primates. Nature 2015; 521:362–5. [DOI] [PMC free article] [PubMed] [Google Scholar]