Abstract
Background. The 2013–2016 Ebola epidemic in West Africa resulted in accelerated development of rapid diagnostic tests for emergency outbreak preparedness. We describe the development and evaluation of the Idylla™ prototype Ebola virus test, a fully automated sample-to-result molecular diagnostic test for rapid detection of Zaire ebolavirus (EBOV) and Sudan ebolavirus (SUDV).
Methods. The Idylla™ prototype Ebola virus test can simultaneously detect EBOV and SUDV in 200 µL of whole blood. The sample is directly added to a disposable cartridge containing all reagents for sample preparation, RNA extraction, and amplification by reverse-transcription polymerase chain reaction analysis. The performance was evaluated with a variety of sample types, including synthetic constructs and whole blood samples from healthy volunteers spiked with viral RNA, inactivated virus, and infectious virus.
Results. The 95% limits of detection for EBOV and SUDV were 465 plaque-forming units (PFU)/mL (1010 copies/mL) and 324 PFU/mL (8204 copies/mL), respectively. In silico and in vitro analyses demonstrated 100% correct reactivity for EBOV and SUDV and no cross-reactivity with relevant pathogens. The diagnostic sensitivity was 97.4% (for EBOV) and 91.7% (for SUDV), the specificity was 100%, and the diagnostic accuracy was 95.9%.
Conclusions. The Idylla™ prototype Ebola virus test is a fast, safe, easy-to-use, and near-patient test that meets the performance criteria to detect EBOV in patients with suspected Ebola.
Keywords: Ebolavirus, diagnosis, EBOV, SUDV, RT-PCR, outbreak
The 2013–2016 outbreak of Ebola virus (EBOV) infection in West Africa is the largest and most geographically widespread Ebola virus disease (EVD) epidemic since discovery of the virus, in 1976. The end of the 2-year epidemic was declared on 14 January 2016, after >28 637 cases and 11 315 deaths [1]. However, since then a few new EVD cases have been reported in West Africa [1], and there is a potential ongoing risk for flare ups of EBOV infection or outbreaks involving other filoviruses.
The magnitude and duration of this outbreak clearly demonstrate the weaknesses in the local healthcare systems and the current lack of tools to manage patients effectively. Affordable high-quality diagnostic tests that are easily deployable under field conditions and rapidly yield results are an important component in controlling an outbreak and should be incorporated within a sustainable healthcare system. Unfortunately, shortcomings in the diagnostic capacity infrastructure in West Africa were apparent from the start of the outbreak, with only a few fully functional laboratories installed during the initial phase of the outbreak. In August 2014, at the height of the epidemic, the Food and Drug Administration justified the authorization of emergency use of in vitro diagnostics for the detection of EBOV (available at: https://www.federalregister.gov/articles/2014/08/12/2014-19026/declaration-regarding-emergency-use-of-in-vitro-diagnostics-for-detection-of-ebola-virus). Additional field laboratories were installed, each using their own specific RNA extraction methods and polymerase chain reaction (PCR) assays [2]. Besides the lack of standardization between these tests and corresponding difficulties in comparative analysis of results [3], the time from blood draw to a result typically took several hours and often longer than a day, as evidenced during the West African outbreak.
Since its first use in the field during the 2000 Ebola outbreak in Gabon [4], reverse-transcription (RT-PCR) has become the standard test in EVD diagnosis. According to the World Health Organization (WHO), RT-PCR is the method of choice because rapid antigen tests, despite their reasonable sensitivity for patients with high-level viremia, might have high false-positive rates in the context of low disease prevalence [5]. When the incidence and prevalence of EVD decreases in the postepidemic era, assays with high sensitivity and specificity will be especially necessary. RT-PCR tests combine these characteristics but remain labor intensive and require multiple steps, skilled laboratory personnel, substantial training, and technical laboratory infrastructure. In an epidemic context, access to accurate, rapid, highly sensitive, and easy-to-use assays with minimal manipulation of potentially highly infectious samples would therefore be a great asset [6, 7]. The outbreak in West Africa spurred the development and clinical evaluation of several RT-PCR assays implemented on automated molecular detection platforms, such as the GeneXpert Ebola assay (Cepheid) [8] and the FilmArray Ebola test (BioFire) [9].
Biocartis, a molecular diagnostics company based in Mechelen, Belgium, has developed a rapid sample-to-result molecular test for EVD diagnosis, in collaboration with the Institute of Tropical Medicine (ITM; Antwerp, Belgium) and Janssen Diagnostics (Beerse, Belgium). The Idylla™ prototype Ebola virus test integrates sample preparation with qualitative detection of EBOV and Sudan virus (SUDV). All reagents required to perform the test, including controls, are contained within the cartridge. The test is developed to be used on the Idylla™ system, a Conformité Européenne–marked, commercial molecular diagnostics platform. Here, we report on the development and subsequent laboratory evaluation of the Idylla™ prototype Ebola virus test.
METHODS
Idylla™ System
The Idylla™ system is a miniaturized laboratory that integrates all sample-processing and RT-PCR analytical procedures and is composed of 3 physical components: a console, an instrument, and a disposable test-specific cartridge (Figure 1). The Idylla™ system provides a sample in–result out workflow that operates in fully automated and controlled fashion. The sample is loaded into the cartridge without requiring any sample-pretreatment steps. One sample loaded into the cartridge can be tested per instrument module. Up to 8 separately and independently operating stackable modules can be used per console.
Figure 1.
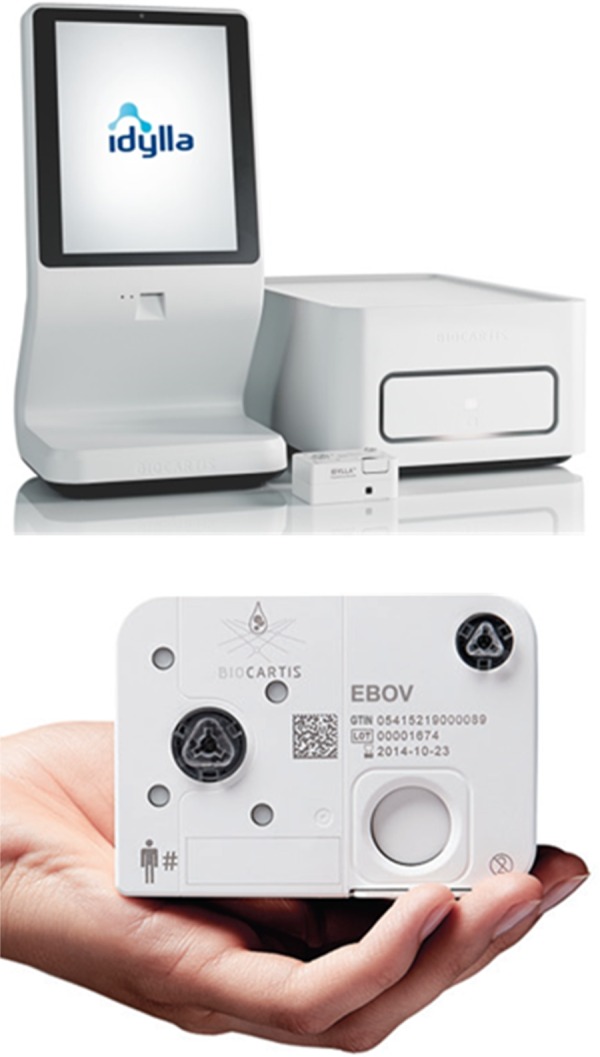
The Idylla™ molecular diagnostic platform. The console is a touch-screen-operated computer supplemented with barcode scanning and communication capabilities and works as a local command center where sample information is entered, tests are initiated, and test results are displayed. The instrument executes a test-specific protocol within the cartridge through multipurpose instrument-cartridge interfaces. Each instrument has a computer, memory and a variety of sensors on board. A single instrument measures 30.5 × 50.6 × 19 cm and weighs 20 kg. Up to 8 instruments can be connected to a single console to accommodate higher-throughput needs. The total power consumption of an installation consisting of a console and an instrument is as low as 200 W. The cartridge is a single-use, disposable plastic consumable with all necessary reagents and controls onboard in lyophilized or liquid form. After the clinical sample is loaded into the cartridge, the latter is closed with an airtight seal and placed in the instrument, which then automatically executes a predefined assay protocol, including the complete measurement and analysis of the data. The cartridge contains an extraction component and a polymerase chain reaction (PCR) disk with 5 individual chambers in which the reverse-transcription PCR takes place. In each chamber, up to 6 differently fluorescent–labeled reporter dyes can be detected. Cartridges do not require cold chain transport and are stored at ambient conditions. This figure is available in black and white in print and in color online.
Idylla™ Prototype Ebola Virus Test
A 200-µL whole-blood sample is directly dispensed into the sample-processing chamber of the cartridge. After sample lysis, the viral RNA is extracted on board, using an extraction method adapted from Boom et al [10]. Following extraction and purification, the eluate is then pumped toward the PCR amplification and detection module within the cartridge, which contains prespotted RT-PCR reagents in 5 reaction chambers.
The Idylla™ prototype Ebola virus test detects EBOV and SUDV, as well as a sample-processing control. The sample-processing control is an armored RNA with a sequence encoding part of the nucleocapsid protein of the negative-stranded RNA virus Phocine Distemper Virus (Asuragen, Austin, Texas) and is spotted in the sample-processing chamber of the cartridge. Besides the triplex PCR, the assay also contains an endogenous control, targeting a locus in the RPP30 gene of the human genome. For EBOV and SUDV, forward and reverse degenerated primers were used as described before [11] to target a conserved region of 112 base pairs in the glycoprotein (GP) coding region of the EBOV genome together with one EBOV-specific and one SUDV-specific probe that differ from each other by seven nucleotides. The fluorescently labeled detection probes were adapted (reverse complement) from the previous design [11]. All primer and probe sequences used are presented in Table 1.
Table 1.
Primers and Probes Used in the Idylla™ Prototype Ebola Virus Test
| Primer Name | Position in Reference Sequence | NCBI/GenBank Accession Number | Oligonucleotide Sequence (5′–3′) |
|---|---|---|---|
| 5EBO-GP_1D (sense) | 6348–6369 | NC_002549 | TGGGCTGAAAAYTGCTACAATC |
| 3EBO-GP_1D (antisense) | 6440–6459 | NC_002549 | CTTTGTGMACATASCGGCAC |
| EBO-GP_1DZ-FIBFQ (antisense) | 6421–6402 | NC_002549 | CCGTCTGGCGCTGCTGGTAG (56-FAM/3IAbkFQ) |
| EBO-GP_1DS-TRIBRQ (antisense) | 6402–6420 | NC_006432 | CATCCGGCGGTGGGGGTAA (5TexRd-XN/3IAbRQSP) |
| PDV FW20 (sense) | 20430–20452 | NC_028249 | GCTGTCTGGGTATACTTCTGATG |
| PDV_Rev20 (antisense) | 20 578–20 599 | NC_028249 | CCTCCCCATTTGTATCTGACTG |
| PDV_Prb20 (antisense) | 20 496–20 519 | NC_028249 | TTGTCATGGTCCCCTTCCTGTGTC (5ATTO647/3IABRQS) |
| RNaseP63fw (sense) | 41–58 | U77665 | CAGATTTGGACCTGCGAG |
| RNaseP63rev (antisense) | 87–103 | U77665 | CGGCTGTCTCCACAAGT |
| RNaseP63Pr (antisense) | 65–83 | U77665 | CTGACCTGAAGGCTCTGCG (5TexRd-XN/3IAbRQSP) |
Abbreviation: NCBI, National Center for Biotechnology Information.
PCR curve interpretation and classification occurs automatically via a built-in decision algorithm. The test result is qualitative and has 3 possible outcomes: EBOV detected, EBOV not detected, or invalid. The EBOV-detected result is reported if the sample is positive for EBOV or SUDV, even when the sample-processing control is not positive (which may exceptionally happen in case of a high viral load, owing to competitive inhibition). An invalid result is reported if the system is unable to detect the sample-processing control in the absence of EBOV and/or if no endogenous control is detected.
Sample Types
Synthetic Constructs
RNA transcripts and double-stranded DNA (gBlock, Integrated DNA technologies, Leuven, Belgium) containing the EBOV and SUDV GP target gene sequence were synthesized.
External Control
To monitor the interrun reproducibility of the Idylla™ prototype Ebola virus test, a positive external control (human gDNA spiked with Armored RNA EBOV and SUDV [Asuragen]) and a negative external control (human gDNA) were tested on each test day.
Viral RNA
RNA of SUDV (Boniface strain), Bundibugyo, Tai Forest, and Reston virus were obtained from BEI Resources (Manassas, VA; available at: https://www.beiresources.org/). In addition, RNA extracted from 3 EBOV strains (76, 95, and C07) and from 2 SUDV strains (Boniface and Gulu) were kindly provided by Dr Heinz Feldmann (National Institute of Allergy and Infectious Diseases [NIAID], National Institutes of Health [NIH]). To prevent degradation of viral RNA upon spiking in whole-blood samples, the RNA was first incubated at room temperature for 5 minutes in a 1:1 volume ratio with Lipofectamine 2000 Reagent (Invitrogen, Life Technologies, Carlsbad, California) to obtain encapsulated viral RNA.
Inactivated Virus
Trizol-inactivated virus stocks were obtained from the European Virus Archive (available at: http://www.european-virus-archive.com/rubrique1.html). In total, 5 inactivated virus strains of EBOV (Mayinga, Gabon 2003, Gueckedou-C05, Gueckedou-C07, and Kissidougou-C15) and 1 of SUDV (Gulu) were purchased.
Infectious Virus
Infectious virus stock of EBOV strain Makona (IRF-0138) and of SUDV strain Gulu (IRF-0154) were used during performance testing in the biosafety level 4 (BSL4) facility of the NIAID Integrated Research Facility, Fort Detrick, Maryland. The concentration of the virus stocks has been defined using the Avicel plaque assay as described by Smither et al [12].
Mock Clinical Samples
Whole-blood samples collected in tubes containing ethylenediaminetetraacetic acid (EDTA; hereafter “EDTA whole-blood samples) and spiked with infectious EBOV (n = 76) and SUDV (n = 109) were used as positive contrived clinical samples.
Blood Samples From Healthy Subjects
A total of 155 deidentified EDTA whole-blood samples (n = 74 for blank testing and n = 81 for diagnostic specificity testing) were collected from healthy subjects after they provided written informed consent and in accordance with a dedicated sampling protocol subjected to ethical review (ethical approval was obtained from the institutional review board of the Jan Palfijn Hospital, Merksem, Belgium, and the NIH Integrated Research Facility, National Cancer Institute, Fort Detrick, Frederick, Maryland).
Clinical Samples From Patients With Suspected EVD
Five clinical samples from 4 travelers returning from West Africa and hospitalized in Belgium with suspected EVD, but confirmed to be EVD negative by reference RT-PCR testing were evaluated (the ITM Institutional Review Board approved the institutional presumed consent policy of using leftover samples from patients for research unless the patient explicitly states otherwise, provided that patients' identities are not disclosed to third parties). Additionally, clinical samples from 2 individuals with suspected EVD (1 with EVD and 1 without EVD) were tested in Sierra Leone. In the research study, 2 samples containing leftover plasma after performance of the standard RT-PCR test were analyzed under the informed consent of the Emergency Ebola Hospital.
Reference Methods
All samples were extracted using the QIAamp viral RNA mini kit (Qiagen, Germany), according to the procedure outlined in the Emergency Use Authorization (EUA) instruction booklet [13, 14]. Extractions were performed in the BSL4 facility of the NIAID Integrated Research Facility at Fort Detrick, for the infectious and Trizol-inactivated samples, and in the BSL3 facility of the Antwerp Institute of Tropical Medicine, for clinical and plasma samples.
Because analyses of samples were performed at different collaborating centers, different RT-PCR methods were consequently used as reference methods. The reference RT-PCRs used were the EZ1 RT-PCR, targeting the GP gene of EBOV [13]; the Trombley RT-PCR [15], targeting the GP gene of SUDV; and the in-house real-time RT-PCR (ITM GP RT-PCR), targeting the GP gene of EBOV and SUDV [11].
The EZ1 RT-PCR and Trombley RT-PCR were evaluated on an ABI 7500 Fast Dx Real-Time PCR System (Life Technologies) with the EUA Critical Reagent Program in the BSL4 facility of the NIAID Integrated Research Facility. EZ1 RT-PCR reagents and assay parameters were used as described elsewhere [13, 14], and data were plotted and analyzed using GraphPad Prism. For the Trombley RT-PCR, parameters were identical to the method described by Trombley et al [15]. The ITM GP RT-PCR was performed on a SmartCycler II (Cepheid Benelux, Bouwel, Belgium) in a 1-step reaction with a RT step of 10 minutes at 50°C and a denaturation step of 5 minutes at 95°C, followed by 50 cycles of 10 seconds at 95°C and 30 seconds at 60°C in a 25-µL reaction volume, using 5 µL of RNA and 1-step iScript RT-PCR Master Mix (Bio-Rad Laboratories, Belgium).
Limit of Detection/Analytical Sensitivity
The limit of detection (LoD) of the Idylla™ prototype Ebola virus test was determined by diluting infectious virus stock of EBOV (Makona strain) and SUDV (Gulu strain) spiked in whole-blood samples from healthy individuals. Experiments were done in triplicate. The LoD testing was conducted in 3 phases. The initial and refined LoD was defined as the lowest dilution at which all samples tested were positive in all 4 PCR chambers. First, the initial LoD was determined using a 10-fold dilution series (1-log difference) in 3 replicates and for which the initial LoD was defined as the lowest concentration at which all 3 replicates obtained a positive result. The expected concentration in each diluted sample was calculated on the basis of the virus stock concentration. In addition, the actual virus concentration in the sample was also determined by the reference RT-PCR. Second, the LoD was refined using a 2.15-fold dilution series around the initial LoD (±0.3-log difference) that was tested in triplicate. Finally, the 95% LoD was calculated by repetitive testing (24 replicates) of the spiked whole-blood sample at concentrations equivalent to and 1.5 times the concentration of the refined LoD. The 95% LoD was defined as the lowest dilution at which at least 95% of the samples tested positive in all 4 chambers.
Analytical Reactivity
Reactivity was tested both in vitro and in silico. The in vitro tests were done on synthetic constructs of EBOV and SUDV GP, on whole-blood samples spiked with RNA extracts of EBOV and SUDV reference strains, and on inactivated EBOV and SUDV strains spiked in whole-blood samples. In silico comparison of the primers and probes was performed with sequences of 10 different EBOV and SUDV strains, available in GenBank. Multiple sequence alignment was done with exonerate (available at http://www.ebi.ac.uk/about/vertebrate-genomics/software/exonerate) [16].
Analytical Specificity
Cross-reactivity was evaluated by testing a number of clinically relevant pathogens, including non-EBOV and non-SUDV members of the genus Ebolavirus, filoviruses, and other viruses causing (hemorrhagic) fever, as well as common blood pathogens, such as bacteria, yeast, and parasites. Pathogen culture stocks were used when available. In the absence of culture-derived material, genomic DNA/RNA was used at the highest possible concentration or clinically relevant concentrations, depending on material availability. Samples were obtained from BEI Resources, BCCM, and ATCC-LGC or were kindly provided by Janssen Pharmaceuticals and the Antwerp Institute of Tropical Medicine. All samples were tested in triplicate.
Blank Testing
To assess the ability of the Idylla™ prototype Ebola virus test to correctly score negative samples, human whole-blood samples and negative controls (catalog no. G3041; Promega, the Netherlands) were analyzed. In addition, the test was run without adding a sample (no-template controls).
Diagnostic Accuracy
The diagnostic accuracy is the combined analysis of the diagnostic sensitivity in clinical samples from patients with EVD and the diagnostic specificity in clinical samples from patients without EVD. The diagnostic accuracy is defined by the proportion of correctly identified subjects (ie, those with true-positive results plus those with true-negative results) among all subjects tested. Sensitivity and specificity were calculated with 95% confidence intervals (CIs).
Diagnostic Sensitivity
Owing to the very limited access to whole-blood samples from subjects with confirmed EBOV infection, mock clinical samples were evaluated at the NIAID. A total of 76 EBOV-positive and 109 SUDV-positive contrived clinical samples were tested, as well as 1 plasma sample from a subject with confirmed EVD.
Diagnostic Specificity
A total of 81 whole-blood samples from healthy individuals and 6 whole-blood samples from individuals with suspected EVD were tested to determine the diagnostic specificity.
Stability Testing
Stability testing was performed in 2 phases. In a first phase, cartridges were stressed by mimicking shipment conditions followed by a second phase of prolonged storage at 30°C. To mimic shipment conditions, test cartridges were stressed using the following mean thermal conditions (±standard deviation [SD]): 2 days at −20°C ± 5°C, followed by 6 days at 5°C ± 3°C and subsequently 2 days at 40°C ± 2°C. After this transport simulation, cartridges (n = 56) were stored at 30°C ± 2°C for 4 months. Testing of the positive control sample and a no-template control were used for transport-simulation testing.
To test in-use stability (ambient conditions: a mean temperature [±SD] of 30°C ± 2°C and 70% humidity), after storage at 30°C, 15 cartridges were removed from their pouch, and 200 µL of EDTA whole blood was loaded into all. Five cartridges were tested immediately after loading, and 10 were stored at 30°C with 70% humidity. After 1 hour, 5 more cartridges were tested, and after 2 hours, the last 5 were tested.
RESULTS
LoD Testing
The initial LoD testing for the Idylla™ prototype Ebola virus test resulted in a LoD of 1000 PFU/mL (equivalent to 3837 genomic copies/mL) for EBOV and of 1000 PFU/mL (equivalent to 26 902 genomic copies/mL) for SUDV. The measured virus concentration was comparable to the expected values of the dilutions, in copies per milliliter, calculated from the virus stock concentration (Table 2). After further refinement, the LoD was estimated at 465 PFU/mL for EBOV and at 216 PFU/mL for SUDV. The refined LoD corresponds to 1010 genomic copies/mL for EBOV and 5469 copies/mL for SUDV. Moreover, the refined LoD test results demonstrated that the Idylla™ prototype Ebola virus test has an analytical sensitivity for EBOV and SUDV that is comparable to that of the reference RT-PCR (Table 3). To determine the 95% LoD, 24 samples were tested at 2 concentrations, first at the refined LoD (n = 24) and then at 1.5 times the refined LoD (n = 24). The 95% LoD was confirmed in 24 of 24 EBOV-positive samples at both the refined and 1.5 times the refined LoD. For SUDV, the 95% LoD was confirmed in 24 of 24 samples at the refined LoD and in 22 of 23 samples (1 sample resulted in an aborted run and was not retested) tested at 1.5 times the refined LoD. Based on these results, the 95% LoD of the Idylla™ prototype Ebola virus test was 465 PFU/mL and 1010 genomic copies/mL for EBOV and 324 PFU/mL and 8204 genomic copies/mL for SUDV.
Table 2.
Initial LoD Testing on Ebola Virus (EBOV) Strain Makona and Sudan Virus (SUDV) Strain Gulu Spiked in EDTA Whole Blood Samples, Using Reference RT-PCR Assays
| Strain, Dilution in PFU/mL | Theoretical Genomic Concentration, Copies/mL | Experimental Genomic Concentration, Copies/mL |
Detection Rate, Proportion of Samples |
Detection Rate, Idylla™ Prototype Ebola Virus Test, Proportion of Samples |
|---|---|---|---|---|
| EZ1 RT-PCR | ||||
| EBOV strain Makona | ||||
| Undiluted stock | 81 500 000 | 81 500 000 | 3/3 | 3/3 |
| 10 000 | 27 167 | 69 547 | 3/3 | 3/3 |
| 1000 | 2717 | 3837 | 3/3 | 3/3 |
| 100 | 272 | 135 | 3/3 | 3/3a |
| 10 | 27 | ND | 0/3 | 1/3a |
| 1 | 3 | ND | 0/3 | 0/3 |
| Trombley RT-PCR | ||||
| SUDV strain Gulu | ||||
| Undiluted stock | 182 000 000 | 182 000 000 | 3/3 | 3/3 |
| 10 000 | 206 116 | 134 818 | 3/3 | 3/3 |
| 1000 | 20 612 | 26 902 | 3/3 | 3/3 |
| 100 | 2061 | 2838 | 3/3 | 3/3a |
| 10 | 206 | 812 | 2/3 | 1/3 |
| 1 | 20 | 122 | 1/3 | 0/3 |
Abbreviations: EBOV, Ebola virus; GP, glycoprotein; ITM, Institute of Tropical Medicine; LoD, limit of detection; ND, not detected; PFU, plaque-forming units; RT-PCR, reverse-transcription polymerase chain reaction; SUDV, Sudan virus.
a Results were not positive in all 4 PCR chambers.
Table 3.
Refined LoD Testing and 95% LoD Testing on Ebola Virus (EBOV) Strain Makona and Sudan Virus (SUDV) Strain Gulu Spiked in EDTA Whole Blood Samples
| Strain, Dilution in PFU/mL | Theoretical Genomic Concentration, Copies/mL | Experimental Genomic Concentration, Assay, Copies/mL |
Detection Rate, Proportion of Samples |
Detection Rate, Idylla™ Prototype Ebola Virus Test, Proportion of Samples |
|---|---|---|---|---|
| EZ1 RT-PCR | ||||
| EBOV strain Makona | ||||
| 2150 | 5841 | 4521 | 3/3 | 3/3 |
| 1000 | 2717 | 1799 | 3/3 | 3/3 |
| 698 | 1896 | 1515 | ND | 24/24a |
| 465 | 1263 | 1010 | 3/3 | 3/3; 24/24a |
| 216 | 587 | 178 | 3/3 | 3/3b |
| 100 | 272 | 80 | 2/3 | 2/3 |
| Trombley RT-PCR | ||||
| SUDV strain Gulu | ||||
| 2150 | 44 315 | 30 713 | 3/3 | 3/3 |
| 1000 | 20 612 | 19 093 | 3/3 | 3/3 |
| 465 | 9585 | 11 494 | 3/3 | 3/3 |
| 324 | 6678 | 8204 | ND | 22/23a |
| 216 | 4452 | 5469 | 3/3 | 3/3; 24/24a |
| 100 | 2061 | 3068 | 3/3 | 3/3b |
Abbreviations: LoD, limit of detection; ND, not done; RT-PCR, reverse-transcription polymerase chain reaction.
a 95% LoD testing.
b Results were not positive in all 4 PCR chambers.
Analytical Reactivity
The analytical reactivity of the Idylla™ prototype Ebola virus test was assessed in vitro on a panel of samples representing different EBOV and SUDV strains isolated during previous EVD outbreaks (between 1979 and 2014; Table 4). The Idylla™ prototype Ebola virus test successfully amplified the GP target sequence of EBOV and SUDV in synthetic constructs and detected different EBOV and SUDV strains from which inactivated virus or RNA was spiked in EDTA whole blood. All replicates reproduced the same positive result, except for 1 of the 7 replicates of the SUDV Boniface strain that was tested at a dilution with a low viral copy number (195 copies/mL).
Table 4.
In Vitro Reactivity Testing With the Idylla™ Prototype Ebola Virus Test at Approximately 2× the Limit of Detection (LoD) Concentration and Threshold Cycle (Ct) Values Detected Using the ITM GP Reverse-Transcription Polymerase Chain Reaction as a Reference Test
| Virus/strain | Specimen Type | Concentration | Ct Value, ITM GP RT-PCR | Detection Rate, Idylla™ Prototype Ebola Virus Test Proportion of Samples |
|---|---|---|---|---|
| EBOV | GP RNA transcript | 10−6 | 19.70 | 1/1 |
| EBOV | GP dsDNA (gBlock), spiked in whole blood | 10−4 | 30.80 | 1/1 |
| EBOV/Guinea C07 | Encapsulated RNA, spiked in whole blood | NA | 19.12 | 2/2 |
| EBOV/Zaire 76 | Encapsulated RNA, spiked in whole blood | NA | 20.24 | 2/2 |
| EBOV/Zaire 95 | Encapsulated RNA, spiked in whole blood | NA | 19.95 | 2/2 |
| EBOV/Gabon 2003 | Inactivated virus, spiked in whole blood | 2× the LoD | 20.27 | 6/6 |
| EBOV/Gueckedou-C05 | Inactivated virus, spiked in whole blood | 2× the LoD | 16.75 | 6/6 |
| EBOV/Gueckedou-C07 | Inactivated virus, spiked in whole blood | 2× the LoD | 16.40 | 6/6 |
| EBOV/Kissidougou-C15 | Inactivated virus, spiked in whole blood | 2× the LoD | 17.70 | 6/6 |
| EBOV/Mayinga | Inactivated virus, spiked in whole blood | 2× the LoD | 18.66 | 6/6 |
| SUDV | GP RNA transcript | 10−6 | 20.00 | 1/1 |
| SUDV | GP dsDNA (gBlock), spiked in whole blood | 10−4 | 31.90 | 1/1 |
| SUDV/Boniface | Encapsulated RNA, spiked in whole blood | NA | 19.45 | 2/2 |
| SUDV/Boniface | RNA, spiked in whole blood | 0.25 <LoD | ND | 6/7 |
| SUDV/Gulu | Encapsulated RNA, spiked in whole blood | NA | 22.09 | 2/2 |
| SUDV/Gulu | Inactivated virus, spiked in whole blood | 2× the LoD | 19.96 | 6/6 |
Abbreviations: dsDNA, double-stranded DNA; NA, not applicable; ND, not detected.
In silico analysis was performed to predict the reactivity of the Idylla™ prototype Ebola virus test for various EBOV and SUDV strains (Supplementary Table 1). The analysis showed 100% in silico reactivity based on the best match obtained from the primers and probes with the 10 EBOV sequences, including strains that were not available for in vitro testing. The SUDV-specific probe showed 100% sequence identity with 3 of 10 analyzed SUDV genomes, while 1 mismatch in the SUDV probe sequence was noticed with 7 of 10 SUDV strains. The SUDV-specific probe matched perfect with the Boniface strain but had 1 mismatch with the Gulu strain. This mismatch was located 5 nucleotides away from the 5′ end of the probe and had no significant influence, as demonstrated by in vitro reactivity testing (Table 4). Therefore, the Gulu strain was selected for defining the final LoD and diagnostic sensitivity for SUDV.
Analytical Specificity
In vitro cross-reaction with other pathogens was evaluated by testing several other Ebolavirus species, other (hemorrhagic fever) viruses, and common blood pathogens such as bacteria, yeast, and parasites. The species and concentrations used in the sample are shown in Table 5. The Idylla™ prototype Ebola virus test did not cross-react with any of the pathogens tested (n = 37).
Table 5.
In Vitro Cross-reactivity Testing
| Pathogen | Concentration | Specimen Type | Test Result |
|---|---|---|---|
| Viruses | |||
| Bundibugyo virus | 90 copies | Nucleic acid | Not detected |
| Reston virus | 1.84E+04 copies | Nucleic acid | Not detected |
| Tai Forest virus | 2.60E+04 copies | Nucleic acid | Not detected |
| Rift Valley Fever virus | 9.00E+05 copies | Nucleic acid | Not detected |
| Marburg virus (strain Ravn) | 4.60E+07 copies | Nucleic acid | Not detected |
| Marburg virus (strain Voege) | 1.46E+09 copies | Nucleic acid | Not detected |
| Marburg virus (strain Musoke [GP]) | 6 ng | Plasmid DNA | Not detected |
| Lassa virus | 2.20E+04 copies | Nucleic acid | Not detected |
| Crimean Congo hemorrhagic fever virus | 5.00E+04 copies | Nucleic acid | Not detected |
| Dengue virus serotype 1 | 1.86E+05 CCID50 | Nucleic acid | Not detected |
| Dengue virus serotype 2 | 1.72E+06 CCID50 | Nucleic acid | Not detected |
| Dengue virus serotype 3 | 1.86E+05 CCID50 | Nucleic acid | Not detected |
| Dengue virus serotype 4 | 1.00E+06 CCID50 | Nucleic acid | Not detected |
| Hepatitis B virus | 4.20E+06 copies | Nucleic acid | Not detected |
| Hepatitis C virus | 2.80E+03 cells | Replicon | Not detected |
| Human immunodeficiency virus | 3.05E+05 CCID50 | Infectious culture | Not detected |
| Influenza A virus | 6.34E+05 copies | Infectious culture | Not detected |
| Influenza B virus | 1.26E+07 copies | Infectious culture | Not detected |
| Bacteria | |||
| Acinetobacter baumannii | 4.76E+09 CFU | Nucleic acid | Not detected |
| Enterococcus faecalis | 3.22E+09 CFU | Nucleic acid | Not detected |
| Enterococcus faecium | 1.10E+09 CFU | Nucleic acid | Not detected |
| Escherichia coli | 2.00E+05 copies | Nucleic acid | Not detected |
| Klebsiella oxytoca | 2.00E+05 copies | Nucleic acid | Not detected |
| Klebsiella pneumonia | 2.00E+05 copies | Nucleic acid | Not detected |
| Pseudomonas aeruginosa | 2.00E+05 copies | Nucleic acid | Not detected |
| Salmonella Typhimurium | 16.4 µg | Nucleic acid | Not detected |
| Staphylococcus aureus | 2.00E+05 copies | Nucleic acid | Not detected |
| Staphylococcus epidermidis | 2.00E+05 copies | Nucleic acid | Not detected |
| Streptococcus pneumoniae | 2.00E+05 copies | Nucleic acid | Not detected |
| Fungi | |||
| Aspergillus fumigatus | 2.00E+05 copies | Nucleic acid | Not detected |
| Candida albicans | 3.63–4.27 µg | Nucleic acid | Not detected |
| Candida glabrata | 2.59E+08 CFU | Nucleic acid | Not detected |
| Candida krusei | 2.00E+05 copies | Nucleic acid | Not detected |
| Parasites | |||
| Plasmodium falciparum | 3.14E+06 copies | Nucleic acid | Not detected |
| Plasmodium vivax | 1581 ng | Nucleic acid | Not detected |
| Schistosoma mansoni | 0.1 µg | Nucleic acid | Not detected |
| Trypanosoma brucei gambiense | 603 ng | Nucleic acid | Not detected |
Abbreviations: CCID50, 50% cell-culture infectious dose; CFU, colony-forming units; GP, glycoprotein.
Blank Testing
To evaluate the ability of the test to correctly differentiate a negative sample from no sample, we tested 74 human blood samples, 20 negative control samples (containing human gDNA), and 20 no-template control samples. All samples were reported correctly. The endogenous control correctly detected the presence of the human blood samples and negative control samples. The endogenous control was negative and the sample-processing control positive in all 20 no-template control samples, and results were reported invalid, as expected.
Diagnostic Accuracy
The diagnostic sensitivity was tested on 77 EBOV-positive and 109 SUDV-positive samples. Two EBOV-positive and 9 SUDV-positive samples tested negative by the Idylla™ prototype Ebola virus test. All other 175 samples that tested positive with the reference method also tested positive with the Idylla™ prototype Ebola virus test, resulting in an overall diagnostic sensitivity of 94.1% (175 of 186; 95% CI, 90.7%–97.5%) and diagnostic sensitivities of 97.4% (95% CI, 93.9%–100%) for EBOV and 91.7% (95% CI, 86.6%–96.9%) SUDV.
The diagnostic specificity was evaluated using 87 clinical samples from 81 healthy individuals and 6 individuals with suspected EBOV infection. Analyses of all samples that were identified as negative on the basis of the clinical status of the individuals from whom they were collected subsequently correctly yielded EBOV-not-detected results by the Idylla™ prototype Ebola virus test, except for 3 samples from healthy subjects that were reported as invalid and excluded from further analysis. Overall, 84 of 84 samples were correctly identified as truly negative, resulting in a diagnostic specificity of 100%. The overall diagnostic accuracy was 95.9% (175 + 84 of 270; Table 6).
Table 6.
Diagnostic Sensitivity, Specificity and Accuracy. Evaluation of (Mock) Positive and Negative Clinical Samples With the Idylla™ Prototype Ebola Virus Test in Comparison to the Ebola Status of Those Samples
| EBOV Positive | SUDV Positive | Negative | Total | |
|---|---|---|---|---|
| Ebola detected | 75 | 100 | 0 | 175 |
| Ebola not detected | 2 | 9 | 84 | 95 |
| Total | 77 | 109 | 84 | 270 |
| Sensitivity EBOV | 75/77 (97.4%) | … | … | … |
| Sensitivity SUDV | 100/109 (91.7%) | … | … | |
| Overall sensitivity | 175/186 (94.1%) | … | … | |
| Specificity | … | … | 84/84 (100%) | … |
| Accuracy | … | … | … | 259/270 (95.9%) |
Abbreviations: EBOV, Ebola virus; SUDV, Sudan virus.
Of note, one sample, obtained from a patient who was vaccinated with rVSV ZEBOV-GP as postexposure prophylaxis [17], that was weakly positive by the ITM GP RT-PCR kit but negative by the Altona RT-PCR kit was negative by the Idylla™ prototype Ebola virus test.
Reproducibility
The positive control and the negative control that were evaluated daily before and after the test runs were always correctly reported as EBOV-detected and EBOV-not-detected results, respectively. Over 39 test days, the positive and negative control gave a 100% reproducible result.
Turnaround
The average turnaround of the Idylla™ prototype Ebola virus test was calculated as the average time needed to complete the test (without manual steps), based on 251 test runs. The runs included analysis of different sample types, such as pure nucleic acids, whole-blood samples spiked with reference strains, or nucleic acids and whole-blood samples. The average turnaround time of all experiments executed was 97 minutes.
Stability Testing
After simulation of transport conditions by storage of the cartridges at different temperatures (−20°C, 4°C, and 30°C) and further storage for 4 months at 30°C, all 56 cartridges passed the testing of the positive control and the no-template control. The in-use stability testing of 15 cartridges stored first for 9 days at 30°C were loaded with EDTA whole blood at ambient conditions of 30°C ± 2°C at 70% humidity, showed correct detection of the controls immediately after loading (n = 5), after 1 hour (n = 5), and after 2 hours (n = 5).
DISCUSSION
Handling highly pathogenic viruses is complex and not without risk. BSL4 laboratories are required to manipulate these pathogens with the highest biosecurity measures, but because use of BSL4 containment facilities for diagnostic purposes, especially in the field, is usually not feasible, diagnostic assays are commonly performed in mobile or local laboratories with deployable biosafety cabinets. The urgent need for improved (ie, safer, more rapid, and accurate) diagnostic assays for EVD has been evidenced explicitly during the recent 2013–2016 Ebola outbreak.
The Idylla™ prototype Ebola virus test was developed to specifically address these needs. The Idylla™ platform, a miniaturized laboratory that integrates all of the sample-processing and analytical steps required to provide high-quality molecular diagnostic results at the point of care, has several features facilitating near-patient testing. It has a small footprint, does not require calibration or regular maintenance, and has a low level of electricity consumption, allowing it to be temporarily powered by batteries in case of a power outage. The performance life of the battery packs, which are not built-in, is restricted from a few hours to 1 day, depending on the number of instrument modules that need to be powered. The system can be easily connected to uninterruptible power supplies to guarantee successful termination of a test run in case of a power outage. Further, test cartridges contain all reagents for sample processing and amplification on board, do not require cold chain storage (they are stable up to 30°C and even after exposure to 40°C), and are sealed in a liquid-impenetrable enclosure, allowing surface decontamination and reducing the risk of exposure to EBOV when manipulating clinical samples for diagnosis. As a result, the test can be performed by healthcare professionals with minimal training and without expertise in real-time PCR data interpretation. Because of this simplicity, manipulator errors are highly unlikely to occur, and it is easier to perform the quality control and logistics management activities associated with operating remote laboratories. Although Idylla™ is not a batch-based system that requires simultaneous testing of a large number of samples, 1–8 samples can be processed immediately and simultaneously upon arrival, thereby avoiding the need to batch samples that postpone the analysis.
A key advantage over classical EBOV PCR assays [18] is that whole-blood samples can be entered directly into the cartridge without prior inactivation or pretreatment steps. The GeneXpert Ebola assay (Cepheid) and FilmArray Ebola test (BioFire) are 2 other platforms providing a fully integrated and automated PCR workflow for EVD testing, but they still require preloading manipulation steps [8, 9, 19, 20]. In addition, we demonstrated that the Idylla™ prototype Ebola virus test can withstand a short exposure up to 40°C (2 days) and humidity of 70% at 30°C and that the cartridge reagents are stable for 4 months at 30 °C, while most other PCR tests require a cold chain [18].
The time to EVD diagnosis is of vital importance. Fast and accurate diagnosis is essential for proper case management and rapid patient isolation. We demonstrated that, with the Idylla™ prototype Ebola virus test, it is feasible to load a sample and receive results in <100 minutes, which is a significant improvement over the standard manual extraction and PCR workflows, with a mean processing time of 300 minutes [21]. This turnaround is fast for a molecular test and acceptable for a rapid test to be used in the control of an Ebola outbreak [21]. Of note, rapid diagnostic tests based on antigen detection are much faster, with time to results between 5–15 minutes [22, 23], but are less sensitive and as such still require confirmation testing using RT-PCR. Although rapid diagnostic tests are conceptually very relevant, concerns with biosafety remain, and interpretation of test results is much less unambiguous than for RT-PCR.
During the 2013–2016 epidemic, the WHO highlighted the need for diagnostic facilities in the outbreak region and recommended that every country needs to have access to diagnostic laboratories capable of diagnosing EVD [2]. Access to easy and fast EBOV diagnostic tests is of primary benefit to the patient, their close contacts, and healthcare workers and will improve patient care and management. Although no licensed treatment for EBOV is yet available, early administration of supportive care with rehydration and symptomatic treatment does affect survival [24]. The acute symptoms of EVD at onset are similar to those of many other infectious diseases caused by tropical pathogens. Early diagnosis of EVD thus also facilitates the formulation of a differential diagnosis to exclude other diseases with similar symptoms that require different treatment like antibiotics or antimalarials. Given the multiplexing capacity of the Idylla™ platform, a future, syndrome-based diagnostic approach is possible by extending the panel to include infectious pathogens with a similar clinical presentation. Early diagnosis of EVD is also crucial to stop transmission, to initiate early contact tracing, and for accurate epidemiological surveillance. The Idylla™ system has the capability to allow remote retrieval of data, which may help epidemiological monitoring of an outbreak.
Many in-house RT-PCR assays and most commercial kits on the market target only EBOV, the causative agent of the 2013–2016 outbreak in West Africa and several previous outbreaks in Central Africa. However, SUDV, another member of the Ebolavirus genus, caused outbreaks in Sudan during 1976, 1979, and 2004 and outbreaks in Uganda during 2000, 2004, 2011, and 2012 [25]. The test evaluated here is designed to detect both EBOV and SUDV, and it thus targets the 2 most important Ebolavirus members that have caused EVD outbreaks in the past.
False-positive and false-negative test results have a significant influence on the individual involved and on public health systems, thus warranting highly sensitive and specific diagnostic tests. The evaluation of the analytical sensitivity of the Idylla™ prototype Ebola virus test resulted in a 95% LoD of 465 PFU/mL (1010 copies/mL) for EBOV and 324 PFU/mL (8204 copies/mL) for SUDV. The lower sensitivity for SUDV can probably be explained by the one mismatch of the probe for some of the SUDV strains, as seen during in silico analysis. We believe that this will not significantly affect the sensitivity for detection in clinical samples obtained from patients with EVD during the acute phase of infection, when the viral load is high. Patients with EVD have viral loads, peaking above 105 copies/mL at the time of presentation [26]. Three studies in Sierra Leone reported a mean EBOV load at admission of 106 copies/mL (for 606 patients), 4.89 log copies/mL (for 632 patients), and 6.68 log copies/mL (for 288 patients) [27, 28, 29]. During the SUDV outbreak in Uganda during 2001, the average peak viremia level in cases with a fatal outcome was 3.4 × 109 RNA copies/mL, while in nonfatal cases it was 4.3 × 107 RNA copies/mL [26]. Our experiments show that the LoD of the Idylla™ prototype Ebola virus test to detect both EBOV and SUDV is more than sufficient to support clinical diagnostic use. However, it is evident that the primer/probe design of diagnostic assays for rapidly evolving viruses will need continuous validation to monitor their effectiveness [18] when mutations occur, as demonstrated during the recent and previous EVD outbreaks [30, 31]. The analytical sensitivity for EBOV, as stated by the assay manufacturers, is 1000–5000 PFU/mL for the EZ1 RT-PCR assay, 1116–6750 copies/mL for the RealStar Filovirus Screen RT-PCR kit (Altona Diagnostics), 1 × 103 copies/mL for the Liferiver EBOV Real-time RT-PCR kit (Shanghai ZJ BioTech), 10 000 PFU/mL for the FilmArray NGDS BT-E assay (Biofire Defense), 4781 PFU/mL for the LightMix Ebola Zaire rRT-PCR test (Roche Molecular Systems), and 0.13–1 PFU/mL (232 copies/mL) for the GeneXpert Ebola Assay (Cepheid). Obviously, direct comparison of LoD data between different PCR tests is difficult because no standardized reference method or standard reagents are available for EVD viral load quantification [3]. Of note, LoD estimations were found to be 1–2 logs higher for inactivated samples, compared with samples spiked with live virus in the CDC RT-PCR assay [18].
We demonstrated that the Idylla™prototype Ebola virus testcan be used for rapid EVD diagnosis with an analytical and diagnostic specificity of 100% and a diagnostic sensitivity for EBOV infection of 97.4%. The WHO target product profile for Ebola diagnostic tests targets a clinical sensitivity of ≥95% [2]. Another target product profile, put forward by Chua et al [21], for rapid and simple EBOV tests set the acceptable analytical specificity at >99% and the clinical sensitivity at >95%.
Our study also has a number of shortcomings. Owing to the difficulty in obtaining clinical specimens positive for EBOV, the Idylla™ prototype Ebola virus test was evaluated with contrived specimens spiked with infectious or inactivated virus and with extracted viral RNA or RNA transcripts of different EBOV and SUDV strains. So far, only a single blood sample from an individual with confirmed EVD has been tested.
The diagnostic sensitivity for SUDV detection using the Idylla™ prototype Ebola virus test was 91.7% and, thus, below the preset WHO criteria. This could have resulted from the mismatch in the probe. The diagnostic sensitivity reported by the manufacturers of the 9 Food and Drug Administration–approved EUA EBOV molecular tests varies between 87% and 100%, illustrating that the performance of the available diagnostic methods differs significantly. When evaluation was performed under field conditions in the context of the West African outbreak, the diagnostic sensitivity (84%) and specificity (87%) of the Biofire assay were shown to be lower than stated by the manufacturer [9]. Therefore, a future field evaluation of our test is required.
In conclusion, we present the development and subsequent evaluation of a new rapid molecular diagnostic test for EBOV and SUDV. The IIdylla™ prototype Ebola virus test has a high diagnostic sensitivity and specificity, and its implementation on a fully automated sample-to-result platform makes it extremely useful for rapid diagnosis, contact tracing, and surveillance with mobile Idylla™ units. Further evaluation studies in West and Central Africa are ongoing to ensure that this platform and the test will be ready for deployment as a powerful alternative diagnostic tool during a new EVD outbreak.
Supplementary Data
Supplementary materials are available at http://jid.oxfordjournals.org. Consisting of data provided by the author to benefit the reader, the posted materials are not copyedited and are the sole responsibility of the author, so questions or comments should be addressed to the author.
Notes
Acknowledgments. We thank Dr Guido van der Groen, codiscoverer of EBOV in 1976, for valuable discussions; Dr Heinz Feldmann (National Institute of Allergy and Infectious Diseases [NIAID], National Institutes of Health), for providing EBOV RNA; and Dr Erwin Sablon and Dr Geert Maertens, for critically reading the manuscript.
Disclaimer. The content of this publication does not necessarily reflect the views or policies of the NIAID.
Financial support. This work was supported in part by the Agency for Innovation by Science and Technology, Flemish Government (to L. C. and K. K. A.); Janssen Diagnostics, Janssen Pharmaceutica; and Biocartis.
Potential conflicts of interest. P. V. d. E., I. A., and T. P. are employees of Janssen Diagnostics, Janssen Pharmaceutica; L. V. H., G. M., S. V. D. H., D. N., R. T., and N. V. are employees of Biocartis. All other authors report no potential conflicts. All authors have submitted the ICMJE Form for Disclosure of Potential Conflicts of Interest. Conflicts that the editors consider relevant to the content of the manuscript have been disclosed.
References
- 1.WHO. Situation report, Ebola response roadmap. Geneva, Switzerland: World Health Organisation, 2016. http://www.who.int/csr/disease/ebola/situation-reports/en/ Accessed 26 February 2016. [Google Scholar]
- 2.WHO. Target Product Profile for Zaïre ebolavirus rapid, simple test to be used in the control of the Ebola outbreak in West Africa. Geneva, Switzerland: World Health Organisation, 2014. http://www.finddiagnostics.org/export/sites/default/programs/ebola/docs/target-product-profile.pdf Accessed 20 January 2015. [Google Scholar]
- 3.Cnops L, van Griensven J, Honko AN et al. Essentials of filoviral load quantification. Lancet Infect Dis 2016. In press. [DOI] [PubMed] [Google Scholar]
- 4.Leroy EM, Baize S, Lu CY et al. Diagnosis of Ebola haemorrhagic fever by RT-PCR in an epidemic setting. J Med Virol 2000; 60:463–7. [PubMed] [Google Scholar]
- 5.WHO. Emergency guidance, Selection and use of Ebola in vitro diagnostic assays. Geneva, Switzerland: World Health Organisation, 2015. http://apps.who.int/iris/bitstream/10665/175554/1/WHO_EVD_HIS_EMP_15.2_eng.pdf?ua=1&ua=1 Accessed 15 January 2015. [Google Scholar]
- 6.Nouvellet P, Garske T, Mills HL et al. The role of rapid diagnostics in managing Ebola epidemics. Nature 2015; 528:S109–16. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Woolhouse ME, Rambaut A, Kellam P. Lessons from Ebola: Improving infectious disease surveillance to inform outbreak management. Sci Transl Med 2015; 7:307rv5. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Pinsky BA, Sahoo MK, Sandlund J et al. Analytical performance characteristics of the cepheid GeneXpert Ebola assay for the detection of Ebola virus. PLoS One 2015; 10:e0142216. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Weller SA, Bailey D, Matthews S et al. Evaluation of the Biofire FilmArray BioThreat-E Test (v2.5) for Rapid Identification of Ebola Virus Disease in Heat-Treated Blood Samples Obtained in Sierra Leone and the United Kingdom. J Clin Microbiol 2016; 54:114–9. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Boom R, Sol CJ, Salimans MM, Jansen CL, Wertheim-van Dillen PM, van der Noordaa J. Rapid and simple method for purification of nucleic acids. J Clin Microbiol 1990; 28:495–503. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Gibb TR, Norwood DA Jr, Woollen N, Henchal EA. Development and evaluation of a fluorogenic 5′ nuclease assay to detect and differentiate between Ebola virus subtypes Zaire and Sudan. J Clin Microbiol 2001; 39:4125–30. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Smither SJ, Lear-Rooney C, Biggins J, Pettitt J, Lever MS, Olinger GG Jr. Comparison of the plaque assay and 50% tissue culture infectious dose assay as methods for measuring filovirus infectivity. J Virol Methods 2013; 193:565–71. [DOI] [PubMed] [Google Scholar]
- 13.Naval Medical Research Center for the U.S. Department of Defense. Ebola Zaire (EZ1) rRT-PCR (TaqMan) assay on ABI 7500 Fast Dx, Lightcycler, and JBAIDS: instruction booklet. Version 2.0 2014. http://www.fda.gov/downloads/MedicalDevices/Safety/EmergencySituations/UCM408334.pdf Accessed 20 January 2016.
- 14.Pettitt J, Higgs ES, Adams RD, Jahrling PB, Hensley LE. Use of existing diagnostic reverse-transcription polymerase chain reaction assays for detection of Ebola virus RNA in semen. J Infect Dis 2016; 213:1237–9. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Trombley AR, Wachter L, Garrison J et al. Comprehensive panel of real-time TaqMan polymerase chain reaction assays for detection and absolute quantification of filoviruses, arenaviruses, and New World hantaviruses. Am J Trop Med Hyg 2010; 82:954–60. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Slater GS, Birney E. Automated generation of heuristics for biological sequence comparison. BMC Bioinformatics 2005; 6:31. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.Cnops L, Gerard M, Vandenberg O et al. Risk of Misinterpretation of Ebola Virus PCR Results After rVSV ZEBOV-GP Vaccination. Clin Infect Dis 2015; 60:1725–6. [DOI] [PubMed] [Google Scholar]
- 18.Whitehouse CA, Bavari S, Perkins MD. United States FDA's emergency use authorization of Ebola virus diagnostics: current impact and lessons for the future. Expert Rev Mol Diagn 2015; 15:1231–5. [DOI] [PubMed] [Google Scholar]
- 19.Southern TR, Racsa LD, Albariño CG et al. Comparison of FilmArray and Quantitative Real-Time Reverse Transcriptase PCR for Detection of Zaire Ebolavirus from Contrived and Clinical Specimens. J Clin Microbiol 2015; 53:2956–60. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20.Perkins MD, Kessel M. What Ebola tells us about outbreak diagnostic readiness. Nat Biotechnol 2015; 33:464–9. [DOI] [PubMed] [Google Scholar]
- 21.Chua AC, Cunningham J, Moussy F, Perkins MD, Formenty P. The case for improved diagnostic tools to control Ebola virus disease in West Africa and how to get there. PLoS Negl Trop Dis 2015; 9:e0003734. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22.Broadhurst MJ, Kelly JD, Miller A et al. ReEBOV Antigen Rapid Test kit for point-of-care and laboratory-based testing for Ebola virus disease: a field validation study. Lancet 2015; 386:867–74. [DOI] [PubMed] [Google Scholar]
- 23.Walker NF, Brown CS, Youkee D et al. Evaluation of a point-of-care blood test for identification of Ebola virus disease at Ebola holding units, Western Area, Sierra Leone, January to February 2015. Euro Surveill 2015; 20:pii:21073. [DOI] [PubMed] [Google Scholar]
- 24.Uyeki TM, Mehta AK, Davey RT Jr et al. Clinical management of Ebola virus disease in the United States and Europe. N Engl J Med 2016; 374:636–46. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25.de La Vega MA, Stein D, Kobinger GP. Ebolavirus evolution: Past and present. PLoS Pathog 2015; 11:e1005221. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 26.Towner JS, Rollin PE, Bausch DG et al. Rapid diagnosis of Ebola hemorrhagic fever by reverse transcription-PCR in an outbreak setting and assessment of patient viral load as a predictor of outcome. J Virol 2004; 78:4330–41. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 27.Li J, Duan HJ, Chen HY et al. Age and Ebola viral load correlate with mortality and survival time in 288 Ebola virus disease patients. Int J Infect Dis 2016; 42:34–9. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 28.Lu HJ, Qian J, Kargbo D et al. Ebola virus outbreak investigation, Sierra Leone, September 28-November 11, 2014. Emerg Infect Dis 2015; 11:1921–7. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 29.de La Vega MA, Caleo G, Audet J et al. Ebola viral load at diagnosis associates with patient outcome and outbreak evolution. J Clin Invest 2015b; 125:4421–8. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 30.Carroll MW, Matthews DA, Hiscox JA et al. Temporal and spatial analysis of the 2014–2015 Ebola virus outbreak in West Africa. Nature 2015; 524:97–101. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 31.Hoenen T, Safronetz D, Groseth A et al. Virology. Mutation rate and genotype variation of Ebola virus from Mali case sequences. Science 2015; 348:117–9. [DOI] [PMC free article] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.


