Abstract
Filoviruses are strongly associated with several species of bats as their natural reservoirs. In this study, we determined the replication potential of all filovirus species: Marburg marburgvirus, Taï Forest ebolavirus, Reston ebolavirus, Sudan ebolavirus, Zaire ebolavirus, and Bundibugyo ebolavirus. Filovirus replication was supported by all cell lines derived from 6 Old and New World bat species: the hammer-headed fruit bat, Buettikofer's epauletted fruit bat, the Egyptian fruit bat, the Jamaican fruit bat, the Mexican free-tailed bat and the big brown bat. In addition, we showed that Marburg virus Angola and Ebola virus Makona-WPGC07 efficiently replicated at 37°C, 37°–41°C, or 41°C, contrary to the hypothesis that temporal elevation in temperature due to flight affects filovirus replication in bats.
Keywords: filovirus, bats, replication, temperature, Ebola virus, Marburg virus
Ebola and Marburg viruses are filovirus species that cause sporadic outbreaks of disease in humans with high case fatality rates [1, 2]. There have been 35 recorded outbreaks of Ebola virus and 12 of Marburg virus [1, 3, 4]. The current ongoing outbreak of Zaire ebolavirus has been the largest documented in history, with >28 000 human cases and >11 000 deaths [5].
Filoviruses are within the order of Mononegavirales and have nonsegmented, negative-sense RNA genomes. The Filoviridae family is divided into 3 genera; Marburgvirus, Ebolavirus, and Cuevavirus. Marburgvirus is composed of 1 species, Marburg marburgvirus, which has 2 known members: Marburg virus (MARV) and Ravn virus (RAVV). Ebolavirus is composed of 5 species and their associated viruses: Taï Forest ebolavirus, Taï Forest virus (TAFV); Reston ebolavirus, Reston virus (RESTV); Sudan ebolavirus, Sudan virus (SUDV); Zaire ebolavirus, Ebola virus (EBOV); and Bundibugyo ebolavirus, Bundibugyo virus (BDBV). Cuevavirus is composed of 1 species: Lloviu virus (LLOV) [6].
Filoviruses are strongly asscociated with several species of bats as their natural reservoir. The detection and isolation of MARV from Egyptian fruit bats (Rousettus aegyptiacus) makes the host-reservoir relationship for MARV undisputed [2, 7–9]. Although Ebola virus has not been isolated from bats, the detection of antibodies and viral genomic RNA of Ebola viruses in several species of African and Asian fruit bats suggests that bats are the most likely reservoir [1, 10–12]. Atlthough LLOV has not been isolated, full genome sequences were obtained from common bent-wing bat (Miniopterus schreibersii) during an investigation of reported die-offs of this species in Spain [13].
One hypothesis to account for why bats can harbor viruses that are highly pathogenic in humans but cause no meaningful disease in bats is that elevated body temperature during flight somehow restricts viral pathogenesis in bats [14, 15]. This “flight as fever” hypothesis suggests that increased body temperature during flight mimics the fever response. The fever response during infection is poorly understood; however, elevated body tempertures are preceded by a number of physiologic events triggered by the innate immune response, including secretion of the pyrogenic cytokine interleukin 1, interferons, chemokine ligand 3 (macrophage inflammatory protein-1) and tumor necrosis factor in infected tissues, which lead to the synthesis of prostaglandins that then act on the hypothalamus to elevate body temperature [16–18]. This response may facilitate control of infectious agents by activating biomolecules and immune cells that control infectious agents.
In the current study, we aimed to evaluate the replication kinetics of MARV strain Angola, EBOV strains Kikwit 95 and Makona-WPGC07, TAFV, RESTV Reston 08-A, SUDV and BDBV in 7 bat-derived cell lines. In addition, we determined the effect of temperature on the replication kinetics of MARV Angola and EBOV Makona-WPGC07.
MATERIALS AND METHODS
Viruses and Cells
MARV Angola (MARV), Ebola virus Makona-WPGC07 and Kikwit 95 (EBOV), TAFV, RESTV Reston08-A, SUDV, and BDBV were used in the growth kinetics experiments. Ebola virus Makona-WPGC07 and MARV were used in temperature kinetics experiments. Cell lines were cultured as described elsewhere and included hammer-headed fruit bat (Hypsignathus monstrosus) kidney cells (HypNi/1.1) [19], Buettikofer's epauletted fruit bat (Epomops buettikoferi) kidney cells (EpoNi/22.1) [19], Egyptian fruit bat (Rousettus aegyptiacus) fibroblast cells (REO5 and REO6) [20], primary Jamaican fruit bat (Artibeus jamaicensis) kidney cells (AJ) [21], Mexican free-tailed bat (Tadarida brasiliensis) lung cells (Tb-lu-1), American Type Culture Collection CRL-6564 [22], and big brown bat (Eptesicus fuscus) kidney cells (EFK). The cells were cultured in Dulbecco modified Eagle medium (DMEM; Invitrogen) supplemented with 10% fetal bovine serum, 2 mmol/L glutamine, 50 U/mL penicillin, and 50 µg/mL streptomycin.
Filovirus Replication Kinetics
Multistep replication kinetics were determined by inoculating wells of cells (AJ, EFK, EpoNi/22.1, HypNi/1.1, REO5, REO6, Tb-lu-1, and Vero), in duplicate with a multiplicity of infection of 0.01. All cell lines were seeded in 6-well plates and infected for 1 hour. Cells were washed twice, and 4 mL of 2% fetal bovine serum DMEM was added to the cells. Supernatants were sampled at 0, 24, 48, 72, and 96 hours after inoculation. Filoviruses were titrated by end-point titration in quadruplicate in Vero E6 cells cultured in DMEM supplemented with 2% fetal calf serum, 1 mmol/L L-glutamine (Lonza), 50 U/mL penicillin, and 50 μg/mL streptomycin. Cells were inoculated with 10-fold serial dilutions of virus and scored for cytopathic effect 10–14 days later. The median tissue culture infective dose (TCID50) was calculated using the Spearman-Karber method [23, 24].
Cell Viability
Cell viability of the REO5 and HypNi/1.1 cell lines was measured by determining the number of viable cells during multiple passages at 3 temperature conditions: 37°C continuously, 37°C for 16 hours and 41°C for 8 hours (37°C/41°C), and 41°C continuously over a time course of 5 days. Live cell counts were measured every 24 hours and analyzed as the percentage of live cells, using a TC-20 automated cell counter (Bio-Rad).
Replication Kinetics Under Different Temperature Conditions
Multistep replication kinetics were performed on REO5 and HypNi/1.1 cell lines as described above; kinetics were determined by inoculating wells of cells in triplicate with a multiplicity of infection of 0.01. Six-well plates with cells were placed under 3 temperature conditions, as described in Cell Viability section.
RESULTS
Filovirus Replication Kinetics
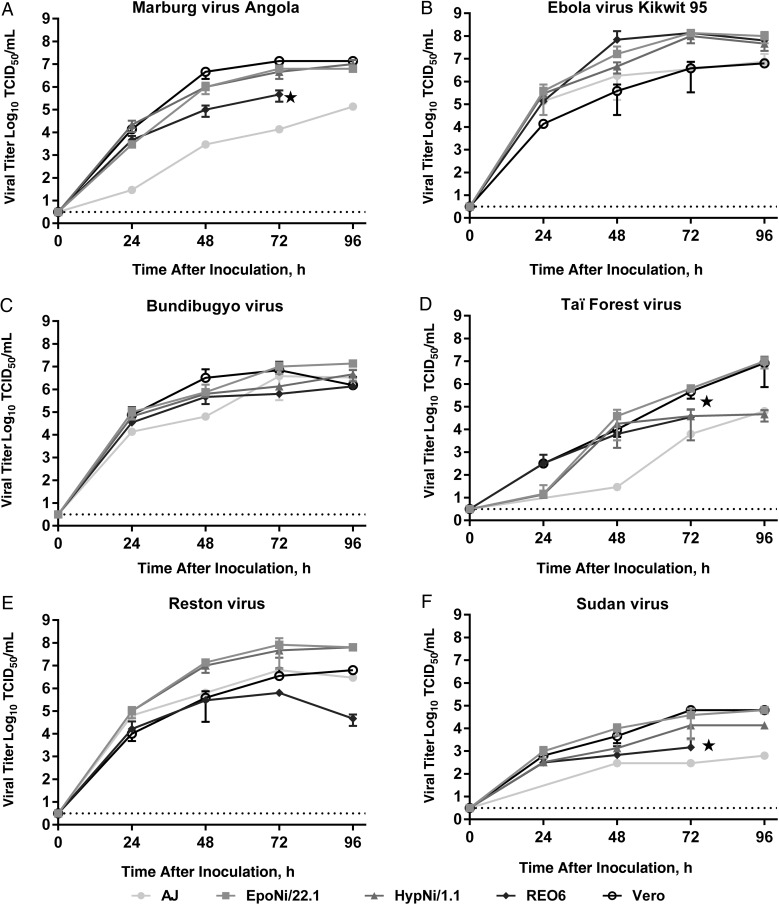
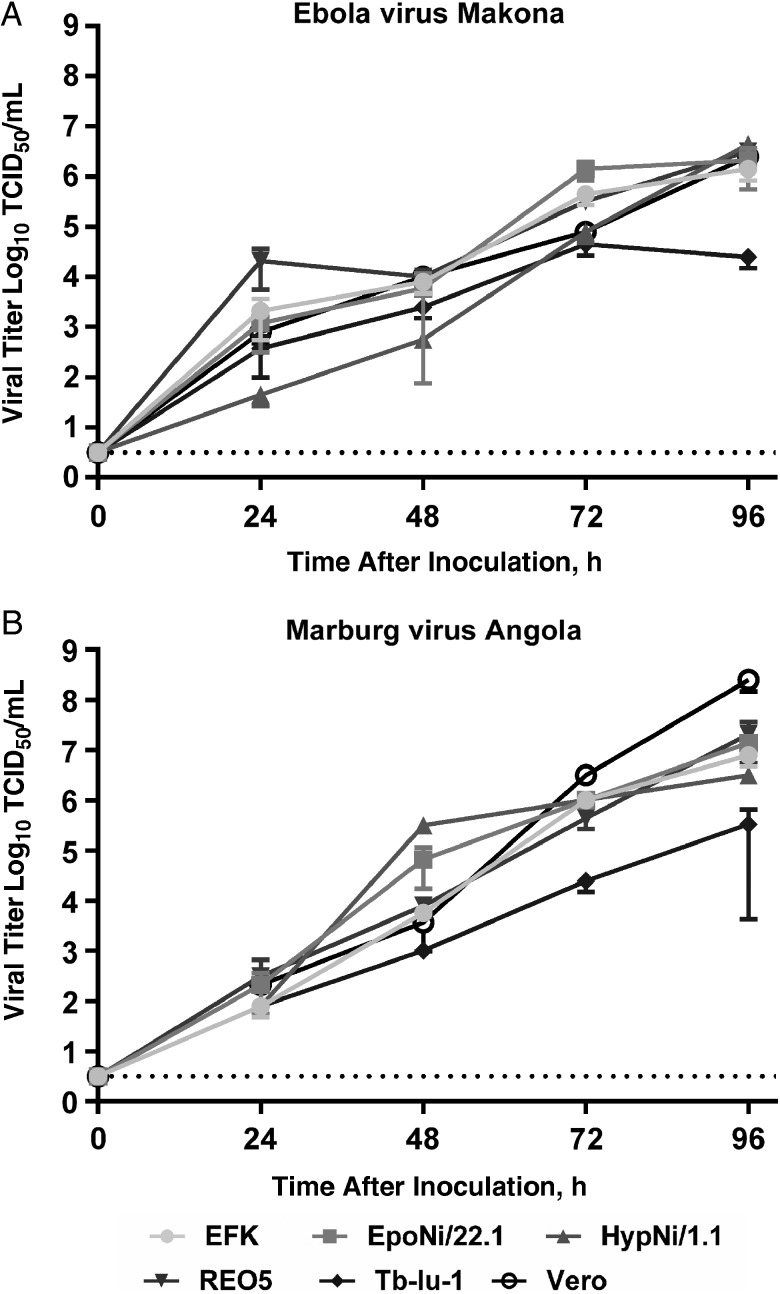
Replication kinetics of filoviruses were assessed on cells from a variety of bat species. MARV, EBOV Kikwit 95, TAFV, RESTV, SUDV, and BDBV replicated on all bat cell lines (Figure 1) End-point titers at 96 hours after inoculation varied, as follows: MARV, 9.9 × 106 TCID50/mL (HypNi/1.1) and 1.36 × 105 TCID50/mL (AJ), with Vero E6 end titers at 1.36 × 107 TCID50/mL; EBOV Kikwit 95, 9.96 × 107 TCID50/mL (EpoNi/22.1) and 7.48 × 106 TCID50/mL (AJ), with Vero end titers at 6.32 × 106 TCID50/mL; BDBV, 1.36 × 107 TCID50/mL (EpoNi/22.1) and 1.36 × 106 TCID50/mL (REO6), with Vero end titers at 1.53 × 106 TCID50/mL; TAFV, 9.97 × 106 TCID50/mL (EpoNi/22.1) and 4.63 × 104 TCID50/mL (HypNi/1.1), with Vero end titers at 8.28 × 106 TCID50/mL; RESTV, 6.32 × 107 TCID50/mL (EpoNi/22.1) and 4.63 × 104 TCID50/mL (REO6), with Vero end titers at 6.32 × 106 TCID50/mL; and SUDV, 6.32 × 104 TCID50/mL (EpoNi/22.1) and 6.31 × 102 TCID50/mL (AJ), with Vero end titers at 6.32 × 104 TCID50/mL. Ebola virus Makona-WPGC07 and MARV replication kinetics were assessed on additional bat cells lines, EFK, RE05, and Tb-lu-1 (Figure 2). Similar to what was observed in the initial replication kinetics experiments, Ebola virus Makona-WPGC07 and MARV replicated on all cell lines infected, with relatively little variation between lines (Figure 2). End-point titers varied between 4.89 × 106 log10TCID50/mL (HypNi/1.1) and 2.47 × 104 log10TCID50/mL (Tb-lu-1) with Vero end titers at 2.47 × 106 log10TCID50/mL for Ebola virus Makona-WPGC07 and 2.08 × 107 log10TCID50/mL (REO5) and 3.31 × 105 log10TCID50/mL (Tb-lu-1) with Vero end titers at 3.31 × 105 log10TCID50/mL for MARV.
Figure 1.
Replication kinetics of filoviruses in bat cells: Marburg virus Angola (A), Ebola virus Kikwit (B), Bundibugyo virus (C), Taï forest virus (D), Reston virus (E), and Sudan virus (F) on cells obtained from mammal species Artibeus jamaicensis (AJ), Epomops buettikoferi (EpoNi/22.1), Hypsignathus monstrosus (HypNi/1.1), Rousettus aegyptiacus (RE06), and Cercopithecus aethiops (Vero). Supernatants were harvested at 0, 24, 48, 72, and 96 hours after inoculation, and viral titers were determined by end-point titration in quadruplicate in Vero E6 cells. Stars indicate complete cytopathic effect and loss of cell adherence. Geometric mean titers were calculated from 3 independent experiments, and error bars indicate standard deviations. Dotted line represents assay threshold. Abbreviation: TCID50, median tissue culture infective dose.
Figure 2.
Replication kinetics of Ebola virus and Marburg virus (MARV), with Ebola virus Makona-WPGC07 (Ebola virus/H.sapiens-tc/GUI/2014/Makona-WPGC07) (A) and MARV Angola (MARV/H.sapiens-tc/ANG/2005/368) (B) on cells obtained from mammal species Eptesicus fuscus (EFK), Epomops buettikoferi (EpoNi/22.1), Hypsignathus monstrosus (HypNi/1.1), Rousettus aegyptiacus (RE06), Tadarida brasiliensis (Tb-lu-1), and Cercopithecus aethiops (Vero). Supernatants were harvested at 0, 24, 48, 72, and 96 hours after inoculation, and viral titers were determined by end-point titration in quadruplicate in Vero E6 cells. Geometric mean titers were calculated from 3 independent experiments, and error bars indicate standard deviations. Dotted line represents assay threshold. Abbreviation: TCID50, median tissue culture infective dose.
Cell Viability
To determine the effect of temperature regimes on the viability of the REO5 and HypNi/1.1 bat cell lines, we examined the cell viability over time for 3 temperature conditions: 37°C, 37°C/41°C, and 41°C. There was no significant difference in live cell count for REO5 between these conditions, with the mean percentage of live cell between 75% and 98% throughout the time course of 5 days within all 3 conditions. There was no significant difference in live cell count for HypNi/1.1 between 37°C and 37°C/41°C; however, there was a significant difference in live cell count at 41°C by 96 hours, with the mean percentage of live cells declining to below 20% by 72 hours under 41°C conditions (data not shown).
Replication Kinetics Under Different Temperature Conditions
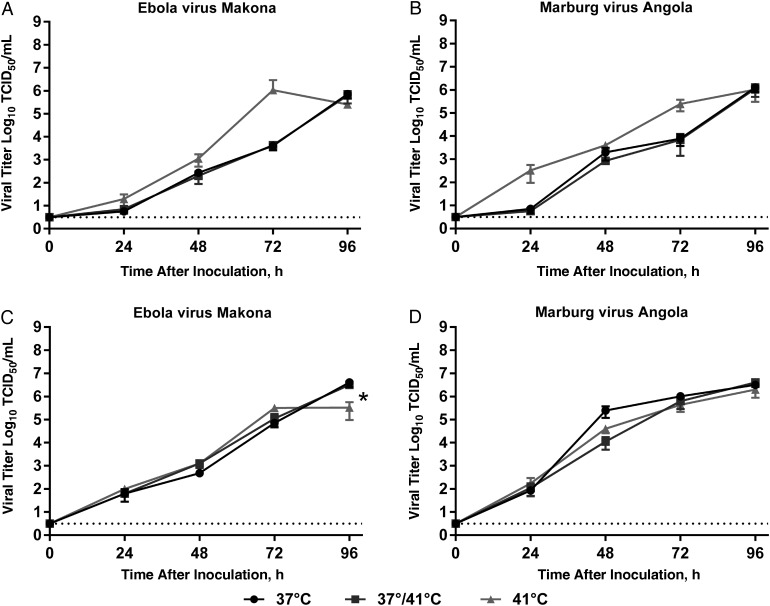
To mimic body temperature fluctuation due to flight, replication kinetics of Ebola virus Makona-WPGC07 and MARV were determined under 3 temperature conditions: 37°C, 37°C/41°C (mimicking temporary elevation of body temperature due to flight), and 41°C on 2 cell lines REO5 and HypNi/1.1 (Figure 3). Ebola virus Makona-WPGC07 reached end-point titers of 7.08 × 105 log10TCID50/mL at 37°C, 6.26 × 105 log10TCID50/mL at 37°C/41°C, and 2.54 × 105 log10TCID50/mL at 41°C on RE05 cells and 3.98 × 106, 3.16 × 106, and 3.26 × 105 log10TCID50/mL, respectively, on HypNi/1.1 cells. A statistically significant difference in end-point titer was detected between 37°C and 41°C (multiple t tests using Holm-Sidak correction; P < .01) and between 37°C/41°C and 41°C (multiple t tests using Holm-Sidak correction; P < .002) on HypNi/1.1 cells, probably due to loss of cell viability beyond 72 hours after inoculation, preventing further virus replication. MARV reached end-point titers of 1.25 × 106 log10TCID50/mL at 37°C, 1.11 × 106 log10TCID50/mL at 37°C/41°C, and 1.03 × 106 log10TCID50/mL at 41°C on RE05 and 3.16 × 106, 3.98 × 106, and 1.98 × 106 log10TCID50/mL, respectively, on HypNi/1.1 cells. No significant differences in end-point titers by temperature were observed with MARV.
Figure 3.
Replication kinetics of Ebola virus and Marburg virus (MARV) at 3 temperature conditions (37°C, 37°C/41°C, and 41°C). A, B, Ebola virus Makona-WPGC07 and MARV Angola on Rousettus aegyptiacus (RE06) cells. C, D, Ebola virus Makona-WPGC07 and MARV Angola on Hypsignathus monstrosus (HypNi/1.1) cells. Supernatants were harvested at 0, 24, 48, 72, and 96 hours after inoculation, and viral titers were determined by end-point titration in quadruplicate in Vero E6 cells. Geometric mean titers were calculated from 3 independent experiments, and error bars indicate standard deviations. *P < .01 for 37°C vs 41°C; P < .002 for 37°C/41°C vs 41°C (calculated using multiple t tests with Holm-Sidak correction). Dotted line represents virus detection threshold. Abbreviation: TCID50, median tissue culture infective dose.
DISCUSSION
Bats have been identified as reservoirs for several important emerging zoonotic viruses, including henipaviruses, coronaviruses, and filoviruses [25]. In general, assessing the growth kinetics on cell lines cannot approximate neither the potential host-range nor potential pathogenicity because of the complexity of in vivo infection and the interplay between innate and adaptive immune responses. For the filoviruses, the best examples of this are EBOV Makona-WPGC07, EBOV Kikwit 95, TAFV, RESTV, SUDV, and BDBV, which in our study replicated efficiently in cells derived from Egyptian fruit bats (R. aegyptiacus) but failed to replicate productively in Egyptian fruit bats, in contrast to MARV [12, 26, 27]. However, similar to findings in coronaviruses, whose tropism is partly determined by the presence of the appropriate entry receptor [28], by looking at bat cell lines we can partly infer species susceptibility at the receptor level. The inability of EBOV to replicate in cells originating from straw-colored fruit bats (Eidolon helvum) is due to an inability of the EBOV glycoprotein to bind to the endosomal receptor, Niemann-Pick C1 [29]. The observed broad replication potential of the filoviruses in bat cells obtained from a wide variety of bat species in our study suggest no receptor-mediated host-range restriction for the bat species from which those cells were derived. This observation, together with data showing that LLOV glycoprotein also binds to Niemann-Pick C1, could potentially suggest a wider geographic distribution for filoviruses than previously recognized.
Researchers have long speculated about the ability of bats to harbor extremely lethal viruses for humans without apparent morbidity and mortality [8, 10, 30]. One hypothesis suggests that a side effect of adaption to flight involves changes in metabolic rate, immune response, and body temperature, all of which can affect viral infection [14, 30, 31]. During flight, bat core body temperatures can range from 39°C to 41°C [14, 32]. The temporal elevation in temperature during flight potentially mimics fever, which would influence components of the innate immune response [14, 31]. Within our study, we showed that elevation of temperature has no impact on the replication of viruses in a matched pathogen-host system. MARV and EBOV were matched with cells obtained from Egyptian fruit bats (the natural host for MARV) and hammer-headed fruit bats (a putative reservoir host for EBOV) [2, 9]. Although small significant differences were observed between 41°C and 37°C and between 41°C and 37°C/41°C for EBOV, these differences are small and only observed with the 41°C condition; thus, this does do not seem biologically relevant in the context of the flight-and-fever hypothesis, because the cells were completely dead beyond 72 hours after inoculation [14]. Interestingly, MARV replicates efficiently in Egyptian fruit bats without causing any sign of disease or changes in body temperature [27]. The broad ability of filoviruses to replicate on cells from a wide variety bat species enable the use of these cells to study host-pathogen interaction in vitro. The ability of filoviruses to replicate efficiently regardless of temperature strongly suggests that that the temporal elevation in temperature due to flight does not affect filovirus replication in bats.
Notes
Acknowledgments. We thank Ingo Jordan for the REO5 and REO6 cell lines and Austin Athman for help with the figures.
Financial support. This work was supported by the Intramural Research Program of the National Institute of Allergy and Infectious Diseases (NIAID), National Institutes of Health. Megan Miller is supported by the Intramural NIAID Research Opportunities program. Bat cells (EpoNi/22.1/22.1, HypNi/1.1/1.1) were generated within the framework of EU-FP7 ANTIGONE (no. 278976) and the German Research Council (DR 772/10-1, MU 3564/1-1).
Potential conflicts of interest. All authors: No reported conflicts. All authors have submitted the ICMJE Form for Disclosure of Potential Conflicts of Interest. Conflicts that the editors consider relevant to the content of the manuscript have been disclosed.
References
- 1.Groseth A, Feldmann H, Strong JE. The ecology of Ebola virus. Trends Microbiol 2007; 15:408–16. [DOI] [PubMed] [Google Scholar]
- 2.Towner JS, Pourrut X, Albarino CG et al. Marburg virus infection detected in a common African bat. PLoS One 2007; 2:e764. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Centers for Disease Control and Prevention. Chronology of Marburg hemorrhagic fever outbreaks. http://www.cdc.gov/vhf/marburg/resources/outbreak-table.html#seven Accessed 3 March 2016.
- 4.Centers for Disease Control and Prevention. Outbreaks chronology: Ebola virus disease, 2015. http://www.cdc.gov/vhf/ebola/outbreaks/history/chronology.html. Accessed 3 March 2016.
- 5.World Health Organization. Ebola situation reports. http://apps.who.int/ebola/ebola-situation-reports Accessed 15 March 2016.
- 6.Kuhn JH, Andersen KG, Baize S et al. Nomenclature- and database-compatible names for the two Ebola virus variants that emerged in Guinea and the Democratic Republic of the Congo in 2014. Viruses 2014; 6:4760–99. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Towner JS, Amman BR, Sealy TK et al. Isolation of genetically diverse Marburg viruses from Egyptian fruit bats. PLoS Pathog 2009; 5:e1000536. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Swanepoel R, Smit SB, Rollin PE et al. Studies of reservoir hosts for Marburg virus. Emerg Infect Dis 2007; 13:1847–51. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Pourrut X, Souris M, Towner JS et al. Large serological survey showing cocirculation of Ebola and Marburg viruses in Gabonese bat populations, and a high seroprevalence of both viruses in Rousettus aegyptiacus. BMC Infect Dis 2009; 9:159. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Leroy EM, Kumulungui B, Pourrut X et al. Fruit bats as reservoirs of Ebola virus. Nature 2005; 438:575–6. [DOI] [PubMed] [Google Scholar]
- 11.Leroy EM, Epelboin A, Mondonge V et al. Human Ebola outbreak resulting from direct exposure to fruit bats in Luebo, Democratic Republic of Congo, 2007. Vector Borne Zoonotic Dis 2009; 9:723–8. [DOI] [PubMed] [Google Scholar]
- 12.Jones ME, Schuh AJ, Amman BR et al. Experimental inoculation of Egyptian rousette bats (Rousettus aegyptiacus) with viruses of the Ebolavirus and Marburgvirus genera. Viruses 2015; 7:3420–42. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Negredo A, Palacios G, Vazquez-Moron S et al. Discovery of an ebolavirus-like filovirus in Europe. PLoS Pathog 2011; 7:e1002304. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.O'Shea TJ, Cryan PM, Cunningham AA et al. Bat flight and zoonotic viruses. Emerg Infect Dis 2014; 20:741–5. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Brook CE, Dobson AP. Bats as ‘special’ reservoirs for emerging zoonotic pathogens. Trends Microbiol 2015; 23:172–80. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Hanson DF. Fever, temperature, and the immune response. Ann N Y Acad Sci 1997; 813:453–64. [DOI] [PubMed] [Google Scholar]
- 17.Ching S, Zhang H, Belevych N et al. Endothelial-specific knockdown of interleukin-1 (IL-1) type 1 receptor differentially alters CNS responses to IL-1 depending on its route of administration. J Neurosci 2007; 27:10476–86. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.Wilhelms DB, Kirilov M, Mirrasekhian E et al. Deletion of prostaglandin E2 synthesizing enzymes in brain endothelial cells attenuates inflammatory fever. J Neurosci 2014; 34:11684–90. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.Kuhl A, Hoffmann M, Muller MA et al. Comparative analysis of Ebola virus glycoprotein interactions with human and bat cells. J Infect Dis 2011; 204(suppl 3):S840–9. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20.Jordan I, Munster VJ, Sandig V. Authentication of the R06E fruit bat cell line. Viruses 2012; 4:889–900. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21.Munster VJ, Adney DR, van Doremalen N et al. Replication and shedding of MERS-CoV in Jamaican fruit bats (Artibeus jamaicensis). Sci Rep 2016; 6:21878. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22.Strong JE, Wong G, Jones SE et al. Stimulation of Ebola virus production from persistent infection through activation of the Ras/MAPK pathway. Proc Natl Acad Sci U S A 2008; 105:17982–7. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23.Fischer R, Judson S, Miazgowicz K, Bushmaker T, Prescott J, Munster VJ. Ebola virus stability on surfaces and in fluids in simulated outbreak environments. Emerg Infect Dis 2015; 21:1243–6. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24.Hierholzer J, Killington R. Virus isolation and quantitation. In: Mahy BWJ, Kangro HO, eds. Virology methods manual. San Diego, CA: Academic Press, 1996:25–46. [Google Scholar]
- 25.Calisher CH, Childs JE, Field HE, Holmes KV, Schountz T. Bats: important reservoir hosts of emerging viruses. Clin Microbiol Rev 2006; 19:531–45. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 26.Paweska JT, Storm N, Grobbelaar AA, Markotter W, Kemp A, Jansen van Vuren P. Experimental inoculation of Egyptian fruit bats (Rousettus aegyptiacus) with Ebola virus. Viruses 2016; 8:29. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 27.Amman BR, Jones ME, Sealy TK et al. Oral shedding of Marburg virus in experimentally infected Egyptian fruit bats (Rousettus aegyptiacus). J Wildl Dis 2015; 51:113–24. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 28.Graham RL, Donaldson EF, Baric RS. A decade after SARS: strategies for controlling emerging coronaviruses. Nat Rev Microbiol 2013; 11:836–48. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 29.Ng M, Ndungo E, Kaczmarek ME et al. Filovirus receptor NPC1 contributes to species-specific patterns of ebolavirus susceptibility in bats. Elife 2015; 4:e11785. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 30.Luis AD, Hayman DT, O'Shea TJ et al. A comparison of bats and rodents as reservoirs of zoonotic viruses: are bats special? Proc Biol Sci 2013; 280:20122753. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 31.Zhang G, Cowled C, Shi Z et al. Comparative analysis of bat genomes provides insight into the evolution of flight and immunity. Science 2013; 339:456–60. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 32.Voigt CC, Lewanzik D. Trapped in the darkness of the night: thermal and energetic constraints of daylight flight in bats. Proc Biol Sci 2011; 278:2311–7. [DOI] [PMC free article] [PubMed] [Google Scholar]