Abstract
Enhanced virulence and/or transmission of West African Ebola virus (EBOV) variants, which are divergent from their Central African counterparts, are suspected to have contributed to the sizable toll of the recent Ebola virus disease (EVD) outbreak. This study evaluated the pathogenicity and shedding in rhesus macaques infected with 1 of 2 West African isolates (EBOV-C05 or EBOV-C07) or a Central African isolate (EBOV-K). All animals infected with EBOV-C05 or EBOV-C07 died of EVD, whereas 2 of 3 EBOV-K–infected animals died. The viremia level was elevated 10-fold in EBOV-C05–infected animals, compared with EBOV-C07– or EBOV-K–infected animals. More-severe lung pathology was observed in 2 of 6 EBOV-C05/C07–infected macaques. This is the first detailed analysis of the recently circulating EBOV-C05/C07 in direct comparison to EBOV-K with 6 animals per group, and it showed that EBOV-C05 but not EBOV-C07 can replicate at higher levels and cause more tissue damage in some animals. Increased virus shedding from individuals who are especially susceptible to EBOV replication is possibly one of the many challenges facing the community of healthcare and policy-making responders since the beginning of the outbreak.
Keywords: Ebola virus, nonhuman primates, pathogenicity, Kikwit, Makona
The first documented outbreak of Ebola virus (EBOV) infection occurred in Yambuku, Zaire (the present-day Democratic Republic of the Congo [DRC]), during 1976, killing 288 of 380 infected individuals [1]. Since then, EBOV has sporadically reemerged in Central Africa in the DRC, the Republic of the Congo, and Gabon. Outbreaks lasted several months on average, were limited geographically, and numbered no more than several hundred cases. In addition to Yambuku, the only EBOV outbreaks to exceed 200 total cases occurred in 1995, in Kikwit, Zaire (254 deaths and 315 cases), and in 2007, in Kasai-Occidental Province, DRC (187 deaths and 264 cases) [1]. Owing to its limited impact on public health in comparison with other infectious diseases alone, Ebola virus disease (EVD) was regarded before 2014 as a neglected tropical disease caused by a high-consequence pathogen of rare occurrence and limited reach [2].
This changed when EBOV unexpectedly emerged in West Africa after the suspected index case, a 2-year-old child from Meliandou, Guinea, died in December 2013 [3]. EBOV transmission was widespread and intense throughout Guinea, Liberia, and Sierra Leone, with >11 000 deaths and 28 000 infections, but the implementation of effective measures has led to substantial improvements, and all 3 countries have now been declared free of EBOV as of 9 June 2016 [4]. This outbreak was unprecedented in that limited infection and/or transmission was observed from imported/repatriated cases in Nigeria, Mali, Senegal, Spain, the United States, and the United Kingdom; and that a significant number of health workers, including prominent local and international physicians, have contracted and died of EBOV infection [5]. There are also concerns that suboptimal immunization rates against vaccine-preventable diseases, directly resulting from the inability of overburdened health systems to provide adequate preventive care, will lead to secondary and tertiary outbreaks of infections involving other pathogens [6]. As a result, the World Health Organization described the EBOV outbreak in 2014–2016 as the “most severe acute health emergency of modern times” [7].
A number of reasons have been suggested to explain why the outbreak of EBOV infection devastating western Africa is so different from past outbreaks in Central Africa. According to the World Health Organization [8], these include (1) damaged public health infrastructures, (2) high population mobility across porous borders, (3) severe shortage of health workers, (4) cultural beliefs and behavioral practices, (5) reliance on traditional healers, (6) community resistance and strikes by health workers, (7) public health messages that fuelled hopelessness and despair, (8) spread by international air travel, (9) background noise from endemic infectious diseases, and (10) a virus with different clinical and epidemiological features. However, with the exception of the last 2 reasons, the other factors had also existed on a smaller scale in past outbreaks. A recent study has shown that the EBOV isolated from patients in West Africa is divergent from the EBOV isolated from past outbreaks in the DRC and Gabon, with 97% homology [3]. The possibility that the virulence of West African EBOV variants may differ from that of their Central African counterparts is therefore a plausible premise for further investigation.
A preliminary study evaluated the replication and clinical evolution of a West African EBOV isolate (EBOV-C07) in parallel to the Mayinga isolate of EBOV (EBOV-May), which originated from the Yambuku outbreak in the DRC during 1976. Infection of cynomolgus macaques (3 per group) suggested that EBOV-C07 was less virulent than EBOV-May, mainly based on a longer time to reach criteria for euthanasia and comparable viremia levels [9]. In contrast, other studies showed higher viremia levels (approximately >108 plaque-forming units) in some but not all control macaques infected with EBOV-C07, when compared to historical data derived from infection with EBOV-K [10–12], which was isolated from an individual during the 1995 outbreak in the DRC [13] and was widely used in previous nonhuman primate (NHP) studies. The current study evaluated the pathogenicity of 2 different isolates of the EBOV Makona strain alongside the reference Kikwit strain in rhesus macaques, using larger groups for the West African EBOV isolates to obtain greater statistical power.
MATERIALS AND METHODS
Viruses
The challenge viruses used in these studies were passage 1 of EBOV H.sapiens-tc/GIN/2014/Makona-Gueckedou-C05 (EBOV-C05; order Mononegavirales, family Filoviridae, and species Zaire ebolavirus; GenBank accession no. KJ660348.2) [3], passage 1 of EBOV H.sapiens-tc/GIN/2014/Gueckedou-C07 (EBOV-C07; order Mononegavirales, family Filoviridae, and species Zaire ebolavirus; GenBank accession no. KJ660347.2) [3], and passage 3 of EBOV H.sapiens-tc/COD/1995/Kikwit-9510621 (EBOV-K and HIST-K; order Mononegavirales, family Filoviridae, and species Zaire ebolavirus; GenBank accession no. AY354458) [14].
NHP Studies
Animal experiments were performed at the National Microbiology Laboratory and approved by the Animal Care Committee located at the Canadian Science Center for Human and Animal Health, in accordance with the guidelines provided by the Canadian Council on Animal Care. Fifteen rhesus macaques (Macaca mulatta) were separated into 3 groups (n = 6 for the EBOV-C05 and EBOV-C07 groups, and n = 3 for the EBOV-K group); housed in stainless steel cages with a built-in perch; fed standard monkey chow, fruits, vegetables, and treats ad libitum; and given plastic balls/rubber chew toys as enrichment devices. Data from 4 rhesus macaques challenged with EBOV-K from past experiments (HIST-K) are also provided, for statistical and comparison purposes to the EBOV-K group. Clinical tests for complete blood counts, serum biochemistry analyses of and measurement of the viremia level in blood specimens, as well as tests for detection of EBOV in oral/rectal/nasal swabs were performed on the NHPs between 0 and 5 days before challenge, to establish a baseline. NHPs were challenged intramuscularly with a back-titered dose of 680 times the 50% tissue culture infective dose (TCID50) of EBOV-C05, EBOV-C07, or EBOV-K or with 1000 times the TCID50 of EBOV-K, for the HIST-K group. The animals were then scored daily for observable signs of disease, in addition to changes in food and water consumption. Animals were euthanized with an intracardiac injection of pentobarbital sodium if the clinical score reached ≥20, to ameliorate suffering. Animals were sampled at the indicated days after infection, as well as on dates of mandatory euthanasia. On these dates, a blood specimen was collected for serum biochemistry analysis, cell count determination, and quantification of viremia. Oral, nasal, and rectal swab specimens were collected to quantify levels of virus shedding. Organs were harvested after death for histopathology and immunohistochemistry studies. Lung scores were obtained by observing photos of the dorsal surfaces of the lungs. Each of 4 lobes (left cranial, left caudal, right cranial, and right caudal) was given a score from 1 to 4, based on the percentage of lung surface affected (<25%, 1; 25%–50%, 2; 51%–75%, 3; and >75%, 4). The scores from each lobe were totaled to obtain a score out of a total of 16. The experiment was not blinded, and all animals were included in the analysis.
Processing of Blood, Sera, and Swab Samples
Complete blood counts and blood biochemistry analyses were performed on whole-blood and sera specimens, respectively, using the VetScan HM5 or the VetScan VS2 (Abaxis Veterinary Diagnostics) according to the manufacturer's instructions. EBOV viremia and shedding in NHPs were determined by real-time quantitative reverse transcription–polymerase chain reaction (qRT-PCR) or live EBOV titration. Briefly, total RNA was extracted from whole-blood samples with the QIAamp viral RNA mini kit (Qiagen). EBOV genomic material was detected using the LightCycler 480 RNA Master Hydrolysis Probes (Roche) kit, targeting the RNA polymerase gene (nucleotides 16472–16538; AF086833). PCR conditions were as follows: 63°C for 3 minutes, 95°C for 30 seconds, and cycling of 95°C for 15 seconds and 60°C for 30 seconds for 45 cycles on the ABI StepOnePlus Thermocycler. The lower detection limit for this assay is 86 genome equivalents (GEQ)/mL. The sequences of primers used were as follows: EBOVLF2 (CAGCCAGCAATTTCTTCCAT), EBOVLR2 (TTTCGGTTGCTGTTTCTGTG), and EBOVLP2FAM (FAM-ATCATTGGCGTACTGGAGGAGCAG-BHQ1). Live EBOV titers were determined by adding whole blood (serially diluted 10-fold in Dulbecco's modified Eagle's medium supplemented with 2% fetal bovine serum and 1% penicillin/streptomycin) to Vero E6 cells, with 3 replicates per dilution. The cells were scored for the presence of cytopathic effect 14 days after infection, and titers were calculated with the Reed and Muench method [15].
Statistics
Survival was compared using the Mantel-Cox log-rank test in GraphPad PRISM 5, and results were considered significant if the P value was < .05. Differences between average values were compared using the unpaired, 2-tailed t test with the Welch correction, which assumes unequal variances. Results were considered significant if the P value was < .05.
Histopathology and Immunohistochemistry
For histopathology, lung tissue samples were collected and fixed in 10% neutral buffered formalin, embedded in paraffin, sectioned, and stained with hematoxylin and eosin. For immunohistochemistry, paraffin-embedded tissue sections were quenched for 10 minutes in aqueous 3% H2O2 and then pretreated with proteinase K for 10 minutes. The primary antibody was a rabbit polyclonal anti-EBOV VP40 antibody that was used at a 1:2000 dilution for 1 hour. The tissue sections were then visualized using a horseradish peroxidase–labeled polymer Envision + system (anti-rabbit; Dako) and reacted with the chromogen diaminobenzidine. The sections were then counterstained with Gill hematoxylin.
RESULTS
Rhesus Macaques Infected With EBOV-C05/C07 Sustained More-Severe Organ Damage
Rhesus macaques were used as a surrogate for EBOV infection in humans, and the animals (6 per group) were given, via intramuscular injection, 680 times the TCID50 of a West African EBOV strain (EBOV-C05 or EBOV-C07). EBOV-C05 and EBOV-C07 were isolated from a surviving patient and a nonsurviving patient, respectively, in Guinea [3]. For purposes of comparison, a group of 3 animals was given the same dose by intramuscular injection of EBOV-K. The moderate challenge dose of <700 times the TCID50 was selected to amplify any possible differences between these related EBOV variants, and only 3 animals were used for EBOV-K challenge, owing to the large amount of historical data already available. Clinical information and virus shedding for a group of 4 rhesus macaques infected with a slightly higher dose of EBOV-K (HIST-K, administered at a dose of 1000 times the TCID50) were compiled from control animals over past experiments, to address any potential concerns over using only 3 animals for EBOV-K infection.
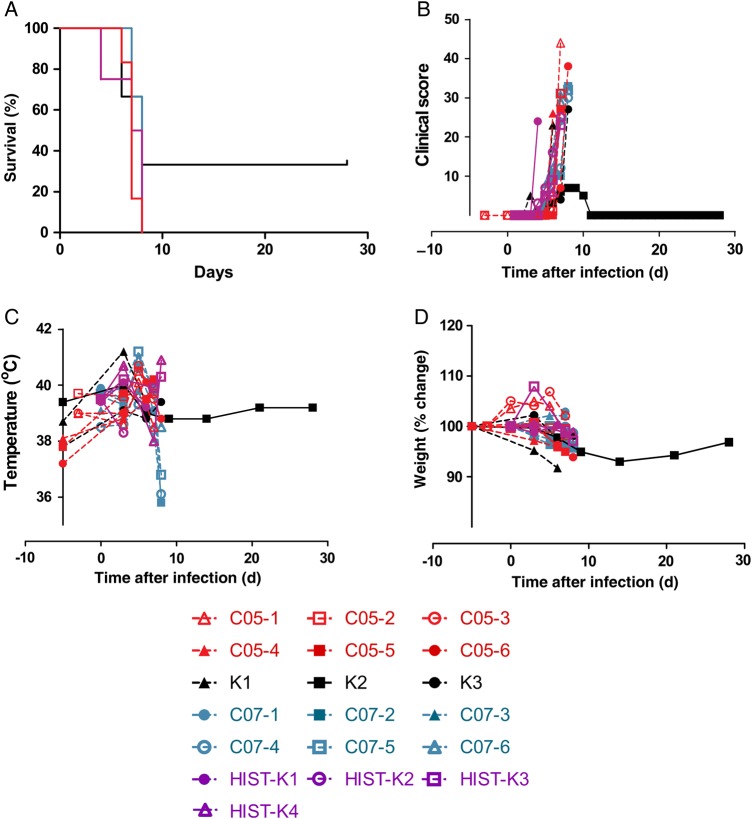
All 6 animals infected with EBOV-C05 (C05-1 to C05-6) or EBOV-C07 (C07-1 to C07-6) died of disease 6–7 days after infection (mean [±SD], 7.0 ± 0.6 days and 7.6 ± 0.5 days after infection, respectively). Two of 3 animals challenged with EBOV-K (K1-K3) died 6–8 days after infection (mean [±SD], 7.0 ± 1.4 days after infection), and animal K2, the lone survivor, and all 4 historical animals infected with EBOV-K (HIST-K1 to HIST-K4) died 4–8 days after infection (mean [±SD], 6.8 ± 1.9 days after infection; Figure 1A). Observed symptoms were typical with that of EVD (Table 1), and clinical scores increased during disease progression for all groups (Figure 1B). K2 also exhibited signs of disease, as evidenced by the rise in clinical scores, as well as leukocytopenia and thrombocytopenia 6 and 9 days after infection, but eventually recovered from the disease (Table 1). Fever was detected in all animals except C05-2, K2, C07-1 to C07-4, HIST-K2, and HIST-K3 (Figure 1C), whereas weight loss was observed in all animals, including K2 (Figure 1D). Moderate-to-severe rash was observed in 5 of 6 animals in the EBOV-C05 group, all 6 in the EBOV-C07 group, and 1 of 3 in the EBOV-K group at the time of euthanasia (Table 1); unfortunately, this information was not available for HIST-K animals. Analysis of blood counts and serum biochemistry findings after challenge revealed abnormal white blood cell and lymphocyte counts, lymphocyte percentage, platelet and neutrophil counts, and neutrophil percentage (Table 1 and Supplementary Figure 1A–1F). The trends were similar, and values did not considerably differ between all groups. Alkaline phosphatase levels were elevated in 2 of 6 in the EBOV-C05 group, all in the EBOV-C07 group, and 3 of 4 in the HIST-K group (Supplementary Figure 1G), and alanine aminotransferase levels were on average higher in EBOV-C05/C07–infected NHPs as compared to EBOV-K–infected NHPs, with levels in 3 of 6 in the EBOV-C05 group and 5 of 6 in the EBOV-C07 group >200 U/L, compared with 1 of 4 in the HIST-K group (Supplementary Figure 1H). Total bilirubin levels were elevated for all EBOV-C05/C07–infected NHPs, 1 of 3 EBOV-K–infected NHPs, and 2 of 4 HIST-K–infected NHPs (Supplementary Figure 1I). Blood urea nitrogen levels were higher in the EBOV-C05/C07 group, with levels in 3 of 6 EBOV-C05–infected NHPs, all 6 EBOV-C07–infected NHPs, and 2 of 4 HIST-K–infected NHPs >40 mg/dL (Supplementary Figure 1J). Creatinine tests showed that animals from both the EBOV-C05 group and the EBPV-C07 group exhibited higher levels than animals in the EBOV-K group and that only 1 of 4 HIST-K–infected NHPs showed elevated creatinine levels (Supplementary Figure 1K). Overall, the serum biochemistry profile showed that, compared with EBOV-K–infected NHPs and HIST-K–infected NHPs, animals in the EBOV-C05 and EBOV-C07 groups sustained more-severe organ damage (Table 1). HIST-K–infected NHPs on average showed more abnormalities in blood counts and serum biochemistry findings, compared with EBOV-K–infected animals (Table 1), which may be due to a slightly higher challenge dose.
Figure 1.
Survival (A), clinical scores (B), rectal temperature (C), and weight change (D) among animals challenged with Ebola virus isolate C05 (EBOV-C05; red), EBOV-C07 (blue), EBOV-K (black), or HIST-K (purple) .
Table 1.
Clinical Findings of Rhesus Macaques Inoculated With the Makona (C05 or C07) or the Kikwit Ebola Virus (EBOV) Variants, as Well as Historical Animals Challenged With Kikwit EBOV
| Animal ID | Age and Weight at Time of Challenge | Challenge Groupa | Clinical Finding (Days After Infection) |
Outcome (Days After Infection) | ||||
|---|---|---|---|---|---|---|---|---|
| Feverb | Rash Severityc | WBC Countd | Platelet Countd | Biochemistry Parameter Level | ||||
| C05-1 | 3 y, 4.80 kg | Makona C05 | Yes (5) | Severe (7 ) | Leukocytosis (3, 5 ) | Thrombocytopenia (7 ) | ALT↑↑↑, BUN↑ (7 ) | Died (7) |
| C05-2 | 4 y, 6.00 kg | Makona C05 | … | Severe (7 ) | Leukocytopenia (7 ) | Thrombocytopenia (7 ) | ALT↑↑↑, TBIL↑, BUN↑, CRE↑ (7 ) | Died (7) |
| C05-3 | 3 y, 4.70 kg | Makona C05 | Yes (5 ) | Moderate (7 ) | Leukocytopenia (3, 7 ) | Thrombocytosis (3, 5 ) | ALT↑↑↑, TBIL↑, BUN↑, CRE↑ (7 ) | Died (7) |
| C05-4 | 2 y, 2.94 kg | Makona C05 | Yes (6 ) | Severe (6 ) | … | Thrombocytopenia (6 ) | … | Died (6) |
| C05-5 | 3 y, 2.78 kg | Makona C05 | Yes (3, 6, 7 ) | Moderate (7 ) | Leukocytopenia (7 ) | Thrombocytopenia (6, 7 ) | ALP↑, ALT↑↑↑ (6, 7 ) | Died (7) |
| C05-6 | 2 y, 2.86 kg | Makona C05 | Yes (3, 6, 8 ) | … | Leukocytopenia (8 ) | Thrombocytopenia (3, 6, 8 ) | CRE↑ (6 ), ALP↑, ALT↑, CRE↑ (8 ) | Died (8) |
| K1 | 3 y, 3.32 kg | Kikwit | Yes (3 ) | Moderate (6 ) | Leukocytopenia (6 ) | Thrombocytopenia (6 ) | ALT↑ (6 ), TBIL↑ (6 ) | Died (6) |
| K2 | 2 y, 2.44 kg | Kikwit | … | … | Leukocytopenia (6, 9 ) | Thrombocytopenia (6, 9, 14 ) | ALT↑ (9 ) | Survived |
| K3 | 2 y, 2.76 kg | Kikwit | Yes (3, 6, 8 ) | … | Leukocytopenia (8 ) | Thrombocytopenia (8 ) | ALT↑ (8 ) | Died (8) |
| C07-1 | 8 y, 6.20 kg | Makona C07 | … | Severe (7 ) | Leukocytopenia (3, 5, 7 ) | Thrombocytopenia (5, 7 ) | ALP↑↑↑, ALT↑↑↑, TBIL↑↑↑, BUN↑↑↑, CRE↑↑ (7 ) | Died (7) |
| C07-2 | 8 y, 7.20 kg | Makona C07 | … | Mild (7 ), severe (8 ) | Leukocytopenia (5, 7, 8 ) | Thrombocytopenia (7, 8 ) | ALP↑, ALT↑↑↑, BUN↑, CRE↑ (7 ), ALP↑↑↑, ALT↑↑↑, TBIL↑, BUN↑↑↑, CRE↑↑↑ (8 ) | Died (8) |
| C07-3 | 9 y, 5.40 kg | Makona C07 | … | Mild (5 ), Severe (7 ) | Leukocytopenia (5 ) | Thrombocytopenia (5, 7 ) | ALP↑, ALT↑, TBIL↑↑, BUN↑ (7 ) | Died (7) |
| C07-4 | 8 y, 7.90 kg | Makona C07 | … | Moderate (7 ), severe (8 ) | Leukocytopenia (3, 5, 7, 8 ) | Thrombocytopenia (5, 7, 8 ) | ALP↑, ALT↑↑↑, TBIL↑, BUN↑, CRE↑↑↑ (8 ) | Died (8) |
| C07-5 | 10 y, 8.70 kg | Makona C07 | Yes (5 ) | Severe (7, 8 ) | Leukocytopenia (5, 7, 8 ) | Thrombocytopenia (7, 8 ) | ALP↑↑, ALT↑↑↑, TBIL↑, CRE↑ (7 ), ALP↑↑↑, ALT↑↑↑, TBIL↑↑↑, BUN↑↑, CRE↑↑↑ (8 ) | Died (8) |
| C07-6 | 8 y, 6.40 kg | Makona C07 | Yes (5 ) | Severe (7, 8 ) | Leukocytopenia (3, 5, 7, 8 ) | Thrombocytopenia (7, 8 ) | ALP↑, ALT↑, TBIL↑, BUN↑, CRE↑ (7 ), ALP↑, ALT↑, TBIL↑↑↑, BUN↑↑↑, CRE↑ (8 ) | Died (8) |
| HIST-K1 | 3 y, 5.42 kg | Kikwit; dose, 1000 × TCID50 | Yes (3 ) | NA | Leukocytopenia (7 ) | Thrombocytopenia (6, 7 ) | ALT↑↑↑, TBIL↑, BUN↑, CRE↑ (6 ), ALP↑, ALT↑↑↑, TBIL↑, BUN↑↑, CRE↑↑↑ (7 ) | Died (7) |
| HIST-K2 | 2 y, 2.80 kg | Kikwit; dose, 1000 × TCID50 | … | NA | Leukocytopenia (3 ) | Thrombocytopenia (3 ) | ALT↑ (3 ) | Died (4) |
| HIST-K3 | 2 y, 2.41 kg | Kikwit; dose, 1000 × TCID50 | … | NA | Leukocytopenia (7, 8 ) | Thrombocytopenia (8 ) | ALP↑, ALT↑↑ (7 ), ALT↑↑↑ (8 ) | Died (8) |
| HIST-K4 | 2 y, 2.46 kg | Kikwit; dose, 1000 × TCID50 | Yes (4, 8 ) | NA | Leukocytopenia (7, 8 ) | Thrombocytopenia (7, 8 ) | ALP↑ (7 ), ALT↑, TBIL↑ (8 ) | Died (8) |
Abbreviations: ALP, alkaline phosphatase; ALT, alanine aminotransferase; AMY, amylase; BUN, blood urea nitrogen; CRE, creatinine; GLOB, globulin; GLU, glucose; NA, not available; PHOS, phosphate; TBIL, total bilirubin; TCID50; 50% tissue culture infective dose; WBC, white blood cell; ↑, 2–3-fold increase; ↑↑, 4–5-fold increase; ↑↑↑, >5-fold increase.
a Challenge doses were 680 times the TCID50, unless specified otherwise, and were administered intramuscularly.
b Fever was defined as a rectal temperature ≥1.0°C higher than the baseline value.
c Mild rash was defined as focal areas of petechiae covering <10% of the skin, moderate rash as areas of petechiae covering 10%–40% of the skin, and severe rash as areas of petechiae and/or ecchymosis covering >40% of the skin.
d Leukocytopenia and thrombocytopenia were defined as a >30% decrease the WBC and platelet counts, respectively. Leukocytosis and thrombocytosis were defined as a ≥2-fold increase in WBC and platelet counts over baseline counts, when the WBC count was >11 × 103.
Viremia Level Was Significantly Elevated in Rhesus Macaques Infected With EBOV-C05
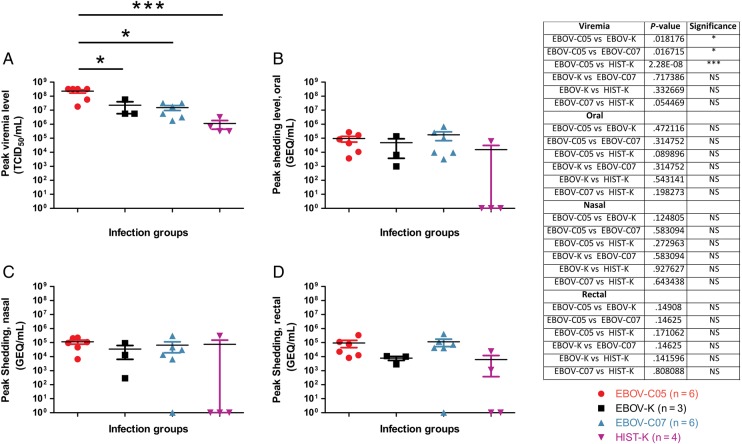
Peak viremia level in each group was detected 6–8 days after infection, with the exception for HIST-K2, which died of EVD 4 days after infection. For EBOV-C05–infected animals, peak viremia level ranged from 1.78 × 107 to 3.16 × 108 TCID50/mL. The average peak viremia level in EBOV-C05–infected animals was 2.23 × 108 TCID50/mL, with 4 of 6 animals with a viremia level of >108 TCID50/mL (Figure 2). For EBOV-C07–infected animals, peak viremia level ranged from 3.16 × 106 to 3.16 × 107 TCID50/mL. The average peak viremia level in EBOV-C07–infected animals was 1.53 × 107 TCID50/mL, and none had a viremia level >108 TCID50/mL (Figure 2). In contrast, peak viremia level for EBOV-K–infected animals ranged from 5.62 × 106 to 5.62 × 107 TCID50/mL. The average peak viremia level for this challenge group was 2.25 × 107 TCID50/mL (Figure 2A), which was approximately 10-fold lower than that observed for EBOV-C05–infected animals but consistent with previously reported findings [16]. Peak viremia level for HIST-K–infected animals ranged from 6.81 × 105 to 3.16 × 106 TCID50/mL. The average peak viremia level for this challenge group was 2.54 × 106 TCID50/mL (Figure 2A). Statistical analysis showed that the difference in average peak viremia level was significant between the EBOV-C05 and EBOV-K/HIST-K groups (P = .0182/2.28 × 10−8, respectively), as well as the EBOV-C05 and EBOV-C07 groups (P = .0167). The difference between the EBOV-K and HIST-K groups was not significant (P = .3327). These findings were also supported by findings from qRT-PCR, in which average peak viremia level in the EBOV-C05, EBOV-C07, and EBOV-K groups was 1.14 × 107, 1.24 × 106, and 1.39 × 106 GEQ/mL, respectively (Supplementary Figure 2). Unfortunately, viremia data determined by qRT-PCR was not available for HIST-K–infected animals.
Figure 2.
Peak levels of viremia and virus shedding among infected rhesus macaques. A, Peak viremia level of each animal. Blood from each animal was sampled from Ebola virus isolate C05 (EBOV-C05), EBOV-K, EBOV-C07, or HIST-K groups. Values are expressed on a logarithmic scale. B–D, Peak EBOV shedding levels from the oral (B), nasal (C), and rectal (D) routes of challenged animals. The EBOV-C05, EBOV-K, EBOV-C07, and HIST-K challenge groups are in red, black, blue, and purple, respectively. Values are expressed on a logarithmic scale. The P values between different groups are presented in the adjacent table and, if statistically significant, are denoted on the graphs. *P<.05 and ***P<.001. GEQ, genome equivalent; NS, not significant; TCID50; 50% tissue culture infective dose.
Virus Shedding Level was Elevated in Rhesus Macaques Infected With EBOV-C05/C07
Virus shedding from the oral, nasal, and rectal passages were also quantified and compared. The average level of peak virus shedding from the oral, nasal, and rectal cavities of EBOV-C05–infected animals was 9.46 × 104, 1.12 × 105, and 9.38 × 104 GEQ/mL, respectively (Figure 2B–2D). The average level of peak virus shedding from the oral, nasal, and rectal cavities of EBOV-C07–infected animals was 1.73 × 105, 7.85 × 104, and 1.27 × 105 GEQ/mL, respectively (Figure 2B–2D). Alternatively, the average level of peak virus shedding from the oral, nasal, and rectal cavities of EBOV-K animals was 4.78 × 104, 3.42 × 104 and 7.76 × 103 GEQ/mL, respectively (Figure 2B–2D), which is similar to results in a past report [17]. The average level of peak virus shedding from the oral, nasal, and rectal cavities of HIST-K animals was 1.51 × 104, 7.38 × 104 and 6.13 × 103 GEQ/mL, respectively (Figure 2B–2D). On average, EBOV-C05–infected animals shed 2-, 3-, and 12-fold higher amounts of virus than their EBOV-K–infected counterparts through the oral, nasal, and rectal cavities, respectively (Figure 2B–2D), but the differences were not statistically significant (P = .472, .124, and .149, respectively). EBOV-C07–infected animals had approximately 3-, 2-, and 16-fold higher shedding in the oral, nasal, and rectal cavities, respectively, compared with animals infected with EBOV-K (Figure 2B–2D), but the differences were also not statistically significant (P = .315, .500, and .140, respectively). HIST-K–infected animals had approximately 2-fold higher shedding from the nasal mucosa and a similar level of virus shedding from the rectal cavity, compared with EBOV-K–infected animals, but 3-fold less shedding from the oral cavity. HIST-K–infected animals also shed less virus than animals in the EBOV-C05/C07 groups, despite being challenged with a slightly higher dose of virus (Figure 2B–2D).
Enhanced Lung Pathology Was Observed in Some Rhesus Macaques Infected With EBOV-C05/C07
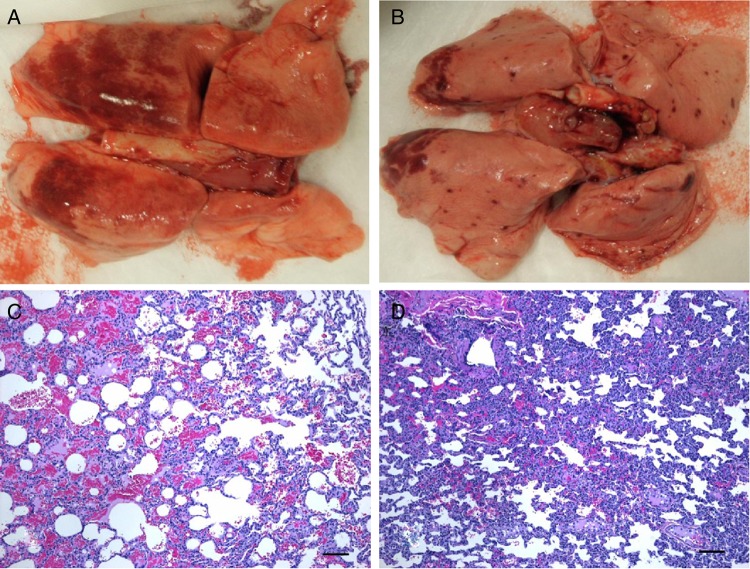
Differences were noted in the lungs between EBOV-C05/C07–infected and EBOV-K–infected animals at necropsy following euthanasia (lungs were not available from HIST-K–infected animals). Large diffuse lesions could be observed all over the lungs from 2 of 6 EBOV-C05–infected animals (Figure 3A), as well as from 2 of 6 EBOV-C07–infected animals, indicating considerable lung damage. In the rest of the animals (including those in the EBOV-K group), there were only focal-to-multifocal hemorrhages (Figure 3B). Blind scoring of the gross pathology of all harvested lungs revealed that animals in both the EBOV-C05 and EBOV-C07 groups had higher scores on average than those in the EBOV-K group (Supplementary Figure 3), but the difference just failed to reach statistical significance for EBOV-C05–infected animals (EBOV-C05 vs EBOV-K, P = .0519; and EBOV-C07 vs EBOV-K, P = .3467), likely due in part to the limited number of EBOV-K–infected lungs available for analysis. Further investigation into the pathology shows that the observed lung lesions were consistent with systemic viral infection as characterized by the thrombosis of vessels and a mild increase in inflammatory cells within alveolar walls (neutrophils and macrophages). Although focal-to-multifocal hemorrhages were observed in all NHPs, widespread hemorrhage was only observed in C05-3 and C05-4 (Figure 3C and 3D) and in 2 of 6 EBOV-C07–infected animals. In most animals, viral antigen was detected in cells morphologically consistent with macrophages scattered throughout alveolar septae (Figure 4A) and within bronchiolar-associated lymphoid tissues (Figure 4B). In C05-2 and C05-3, there were 1–2 small focal areas of intense immunoreactivity (Figure 4C) that corresponded to perivascular cuffing with inflammatory cells (Figure 4D).
Figure 3.
Gross pathology and initial histopathology findings in the lungs of Ebola virus (EBOV)–infected rhesus macaques. A and B, Representative picture of lungs from nonsurviving animals infected with (A) EBOV isolate C05 (EBOV-C05; A) and EBOV-K (B). An image from the EBOV-C07 group was not included since findings were similar to those for the EBOV-C05 group, and lungs from HIST-K–infected animals were not available. C and D, Histopathology findings of widespread hemorrhage in the lung of an EBOV-C05–infected nonhuman primate (C) focal or multifocal hemorrhage in the lung of an EBOV-K–infected animal (D). Bars denote 20 μm for panels A–C and 200 μm for panel D.
Figure 4.
Histopathology and immunohistochemistry findings of interest in the lungs of Ebola virus (EBOV)–infected rhesus macaques. A and B, Cells morphologically consistent with macrophages are scattered throughout the alveolar septae (A) and the bronchiolar-associated lymphoid tissues (B) for animals infected with EBOV isolate C05 (EBOV-C05)/EBOV-C07 and EBOV-K. C and D, Areas of intense immunoreactivity (C) in an EBOV-C05–infected animal, corresponding to perivascular cuffing with inflammatory cells (D). Bars denote 20 μm.
DISCUSSION
The findings from this study suggest that EBOV-C05 replicates at higher levels than EBOV-C07 and EBOV-K on average in rhesus macaques and that some animals infected with EBOV-C05/C07 can occasionally shed more viruses from the oral, nasal, and rectal routes, compared with EBOV-K–infected animals, although this difference was not statistically significant. Therefore, the concept of super spreader could be associated with any and all of these viruses. Future studies focusing on viremia in relation to shedding and transmission will be useful to learn more about molecular determinants of virus propagation and spread in animals and humans. Our results show that the Makona EBOV isolates tested in the current conditions are of at least similar if not higher virulence than the reference EBOV-K variant. An interesting observation is that the lungs of animals infected with EBOV-C05/C07 appear to have enhanced pathology on average as compared to their EBOV-K–infected counterparts. Respiratory distress was noted to be associated with a higher risk of death in patients during the EBOV outbreak in West Africa [18, 19], but it is not known whether the frequency of respiratory disease observed among patients in West Africa was higher than that of previous outbreaks. More parameters of EBOV disease, including coagulation abnormalities and cytokine/chemokine responses, will be important to fully characterize and compare the severity of clinical disease caused by EBOV infection with the different isolates.
The results of this study are different from the results of a previous study [9], in which groups of 3 NHPs were challenged with either 1000 times the TCID50 of EBOV-C07 or EBOV-May, and it was concluded that EBOV-C07 is less virulent than EBOV-May, based primarily on delayed disease progression, resulting in a longer time to death. Unfortunately, because of the different NHP species and Central African EBOV variant used between the study by Marzi et al [9] and the current study, it is difficult to interpret and compare the results, and a study directly contrasting the pathogenic potential of EBOV-C05, EBOV-C07, EBOV-May, and EBOV-K will be needed.
It is also important to note that the EBOV-C05/C07 isolates used in these studies were collected early in the outbreak. The outbreak virus has since undergone extensive cycles of replication and passage in humans over a wide geographical area, and it cannot be ruled out that past or currently circulating isolates are of different virulence in vivo, similar or dissimilar to our observations with EBOV-C05 and EBOV-C07. The EBOV mutation rate in the beginning stages of the outbreak was initially thought to be twice the rate observed between outbreaks [20], but later studies, including a reanalysis of the data collected in the study by Gire et al [20], demonstrated that the overall mutation rate of EBOV had not increased [21, 22] despite the appearance of multiple novel lineages [21]. Statistically powered studies comparing representative EBOV sequences isolated from the 3 countries in relation to induced pathology in vivo, at different time points of the outbreak, will be necessary to answer many remaining questions.
Interestingly, in 28% of EBOV cases from Kailahun, Sierra Leone, sampled during June 2014, the viral loads were higher than those measured later at the same location and during a simultaneous outbreak in the DRC [23, 24]. In the current study, a subset of EBOV-C05–infected NHPs also amplified the virus to levels not previously described in macaques with any strains predating the Makona EBOV isolates. Increased viremia level in control NHPs infected with EBOV-C07 was observed in some but not all previous studies of vaccination against and treatment for infection with Makona EBOV [10–12]. This apparent discrepancy may be attributed to the group size selected for each study. While groups of 6 animals were studied here for the 2 less well-characterized Makona isolates, other studies used groups of 3 animals, making phenomena that occur in only a subset of individuals more difficult to detect. The number of times the virus was passaged in cell culture can introduce mutations into the viral genome [25], which may also result in different in vivo phenotypes. The current study used a virus stock produced by a single amplification of the clinical sample on cultured cells for the Makona EBOV isolates, as opposed to at least 2 amplification rounds on cultured cells for the other studies [9–12]. A past study showed that multiple rounds of EBOV amplification on cultured cells was associated with decreased virus potency in a lethal cynomolgus macaque model of infection [26].
An interesting concept emerging from these observations is that a subgroup of individuals with higher virus loads may have been playing a role in driving the 2014–2016 EBOV outbreak through potentially increased virus shedding. Indeed, bodily fluids containing virus loads higher than the ones from other individuals, even from a minority of cases, would represent a more dangerous and potent source of infection. In addition, similar to minority clusters transmitting strain of higher virulence, increased viral loads in a minority subset of infected individuals would not necessarily result in an observable change in overall case-fatality rates. The concept of disease super spreaders had been hypothesized during past outbreaks with EBOV and with other pathogens [27–30] and is consistent with observations during the current outbreak, in which a traditional healer was shown to have directly infected 13 others after dying of EVD [20] and was eventually linked to >300 EBOV cases [31]. A recent study also reported several chains of EBOV transmissions in Guinea, showing how a small number of infected individuals can transmit the virus to a larger number of people and drive the overall spread of EBOV in the community, as opposed to the majority of patients, who infect few others [32]. The combination of societal, organizational, and viral factors is likely to have contributed to the prolonged presence of EBOV in West Africa. The current findings contribute to a better understanding of the differences between this novel, divergent EBOV and its phylogenetic cousins and may be considered in the effective management and termination of this outbreak.
Supplementary Data
Supplementary materials are available at http://jid.oxfordjournals.org. Consisting of data provided by the author to benefit the reader, the posted materials are not copyedited and are the sole responsibility of the author, so questions or comments should be addressed to the author.
Notes
Financial support. This work was supported by the Public Health Agency of Canada (Canadian Safety and Security Program grant to G. P. K. and X. Q.), the Canadian Institutes of Health Research (Banting Postdoctoral Fellowship to G. W.), and the Chinese Academy of Sciences President's International Fellowship Initiative (fellowship to G. W.).
Potential conflicts of interest. All authors: No reported conflicts. All authors have submitted the ICMJE Form for Disclosure of Potential Conflicts of Interest. Conflicts that the editors consider relevant to the content of the manuscript have been disclosed.
References
- 1.Centers for Disease Control and Prevention. Outbreaks chronology: Ebola virus disease. http://www.cdc.gov/vhf/ebola/outbreaks/history/chronology.html Accessed 15 February 2015.
- 2.Leroy EM, Gonzalez JP, Baize S. Ebola and Marburg haemorrhagic fever viruses: major scientific advances, but a relatively minor public health threat for Africa. Clin Microbiol Infect 2011; 17:964–76. [DOI] [PubMed] [Google Scholar]
- 3.Baize S, Pannetier D, Oestereich L et al. Emergence of Zaire Ebola virus disease in Guinea. N Engl J Med 2014; 371:1418–25. [DOI] [PubMed] [Google Scholar]
- 4.World Health Organization. Ebola virus disease situation report—10 June 2016. apps.who.int/iris/bitstream/10665/208883/1/ebolasitrep_10Jun2016_eng.pdf?ua=1. Accessed 22 June 2016.
- 5.World Health Organization. Unprecedented number of medical staff infected with Ebola. www.who.int/entity/mediacentre/news/ebola/25-august-2014/en/index.html. Accessed 22 June 2016.
- 6.Takahashi S, Metcalf CJ, Ferrari MJ et al. Reduced vaccination and the risk of measles and other childhood infections post-Ebola. Science 2015; 347:1240–2. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.WHO Director-General's speech to the Regional Committee for the Western Pacific, 2014. http://who.int/dg/speeches/2014/regional-committee-western-pacific/en/ Accessed 22 June 2016.
- 8.World Health Organization. One year into the Ebola epidemic: a deadly, tenacious and unforgiving virus. http://www.who.int/csr/disease/ebola/one-year-report/ebola-report-1-year.pdf Accessed 27 March 2015.
- 9.Marzi A, Feldmann F, Hanley PW, Scott DP, Gunther S, Feldmann H. Delayed disease progression in cynomolgus macaques infected with Ebola virus Makona strain. Emerg Infect Dis 2015; 21:1777–83. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Marzi A, Robertson SJ, Haddock E et al. EBOLA VACCINE. VSV-EBOV rapidly protects macaques against infection with the 2014/15 Ebola virus outbreak strain. Science 2015; 349:739–42. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Mire CE, Matassov D, Geisbert JB et al. Single-dose attenuated Vesiculovax vaccines protect primates against Ebola Makona virus. Nature 2015; 520:688–91. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Thi EP, Mire CE, Lee AC et al. Lipid nanoparticle siRNA treatment of Ebola-virus-Makona-infected nonhuman primates. Nature 2015; 521:362–5. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Maruyama T, Rodriguez LL, Jahrling PB et al. Ebola virus can be effectively neutralized by antibody produced in natural human infection. J Virol 1999; 73:6024–30. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Jahrling PB, Geisbert TW, Geisbert JB et al. Evaluation of immune globulin and recombinant interferon-alpha2b for treatment of experimental Ebola virus infections. J Infect Dis 1999; 179(suppl 1):S224–34. [DOI] [PubMed] [Google Scholar]
- 15.Reed LJ, Muench H. A simple method of estimating fifty per cent endpoints. Am J Hyg 1938; 27:493–7. [Google Scholar]
- 16.Geisbert TW, Hensley LE, Larsen T et al. Pathogenesis of Ebola hemorrhagic fever in cynomolgus macaques: evidence that dendritic cells are early and sustained targets of infection. Am J Pathol 2003; 163:2347–70. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.Qiu X, Wong G, Audet J et al. Reversion of advanced Ebola virus disease in nonhuman primates with ZMapp. Nature 2014; 514:47–53. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.West TE, von Saint Andre-von Arnim A. Clinical presentation and management of severe Ebola virus disease. Ann Am Thorac Soc 2014; 11:1341–50. [DOI] [PubMed] [Google Scholar]
- 19.Petrosillo N, Nicastri E, Lanini S et al. Ebola virus disease complicated with viral interstitial pneumonia: a case report. BMC Infect Dis 2015; 15:432. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20.Gire SK, Goba A, Andersen KG et al. Genomic surveillance elucidates Ebola virus origin and transmission during the 2014 outbreak. Science 2014; 345:1369–72. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21.Tong YG, Shi WF, Liu D et al. Genetic diversity and evolutionary dynamics of Ebola virus in Sierra Leone. Nature 2015; 524:93–6. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22.Hoenen T, Safronetz D, Groseth A et al. Virology. Mutation rate and genotype variation of Ebola virus from Mali case sequences. Science 2015; 348:117–9. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23.Osterholm MT, Moore KA, Kelley NS et al. Transmission of Ebola viruses: what we know and what we do not know. MBio 2015; 6:e00137. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24.de La Vega MA, Caleo G, Audet J et al. Ebola viral load at diagnosis associates with patient outcome and outbreak evolution. J Clin Invest 2015; 125:4421–8. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25.Kugelman JR, Lee MS, Rossi CA et al. Ebola virus genome plasticity as a marker of its passaging history: a comparison of in vitro passaging to non-human primate infection. PLoS One 2012; 7:e50316. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 26.Alfson KJ, Avena LE, Beadles MW et al. Particle-to-PFU ratio of Ebola virus influences disease course and survival in cynomolgus macaques. J Virol 2015; 89:6773–81. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 27.Fleck F. How SARS changed the world in less than six months. Bull World Health Organ 2003; 81:625–6. [PMC free article] [PubMed] [Google Scholar]
- 28.Wang Sh X, Li YM, Sun BC et al. The SARS outbreak in a general hospital in Tianjin, China -- the case of super-spreader. Epidemiol Infect 2006; 134:786–91. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 29.Lo Iacono G, Cunningham AA, Fichet-Calvet E et al. Using modelling to disentangle the relative contributions of zoonotic and anthroponotic transmission: the case of Lassa fever. PLoS Negl Trop Dis 2015; 9:e3398. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 30.Wong G, Liu W, Liu Y, Zhou B, Bi Y, Gao GF. MERS, SARS, and Ebola: The Role of Super-Spreaders in Infectious Disease. Cell Host Microbe 2015; 18:398–401. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 31.World Health Organization. Sierra Leone: a traditional healer and a funeral. http://www.who.int/csr/disease/ebola/ebola-6-months/sierra-leone/en/ Accessed 25 May 2015.
- 32.Faye O, Boelle PY, Heleze E et al. Chains of transmission and control of Ebola virus disease in Conakry, Guinea, in 2014: an observational study. Lancet Infect Dis 2015; 15:320–6. [DOI] [PMC free article] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.