Abstract
Selective autophagy of the endoplasmic reticulum (termed ER-phagy) is controlled by members of the FAM134 reticulon protein family. Here we used mouse embryonic fibroblasts from mice deficient in FAM134B to examine the role of the ER in replication of historic (Mayinga) or contemporary (Makona GCO7) strains of Ebola virus (EBOV). Loss of FAM134B resulted in 1–2 log10 higher production of infectious EBOV, which was associated with increased production of viral proteins GP and VP40 and greater accumulation of nucleocaspid lattices. In addition, only 10% of wild-type cells contained detectable nucleoprotein, whereas knockout of FAM134B resulted in 80% of cells positive for nucleoprotein. Together, these data suggest that FAM134B-dependent ER-phagy is an important limiting event in EBOV replication in mouse cells and may have implications for further development of antiviral therapeutics and murine models of infection.
Keywords: Ebolavirus, selective autophagy, ER-phagy, reticulon, FAM134B, mouse models, virus replication
The Makona strain of Ebola virus (EBOV-Makona) responsible for the 2013–2016 outbreak in West Africa belongs to the Zaire lineage of EBOV. Although it is difficult to directly compare virulence and case-fatality rates between outbreaks, EBOV-Makona may be less virulent than historical Zaire EBOV strains such as the 1976 Mayinga strain, owing to case-fatality rates of 40% and 90%, respectively [1–3]. Whether this apparent difference is supported by assessment of clinical disease caused following experimental infection of cynomolgus macaques [4] is debated. Sequence differences associated with emergence of EBOV-Makona include changes throughout the genome, with multiple nonsynonymous mutations clustered in the glycoprotein (GP) present on the surface of the virion [2]. This is not unexpected, because the GP is a major target of the host immune response and must interact with host-cell receptors for viral entry. Thus, GP is likely undergoing positive selection in association with these events [2]. However, it is of interest that GP expression is linked to endothelial cell toxicity and virus virulence [5, 6], suggesting that GP interactions with the host cell other than entry receptors may be important in viral pathogenesis.
EBOV RNA replication occurs in cytosolic inclusion bodies that contain nucleoprotein (NP), VP35, VP30, and L (viral polymerase) and contain nucleocapsids or nucleocapsid-like structures [7–10]. Although full-length EBOV GP accumulates in the endoplasmic reticulum (ER) [11] and filovirus inclusion bodies are tightly juxtaposed with rough ER [12], the ER itself is not a site of viral replication. However, the ER is important for processing GP from its immature form to a fully glycosylated form prior to its transit to the Golgi apparatus and eventual cleavage to the mature GP form, GP1,2 [13]. More generally, the ER is important for functions that impinge on virus replication, including protein quality control, lipid synthesis, calcium homeostasis and organelle communication [14]. ER turnover occurs through selective autophagy (termed ER-phagy) and is controlled by the FAM134 reticulon protein family. Specifically, downregulation of the ER-resident protein FAM134B prevents autophagic clearance of the ER and results in ER expansion [15, 16]. The genetic ablation of FAM134B in mice [15] allows unprecedented manipulation of the ER for examining its role in various processes, including virus replication. Although adaptation of EBOV is required to induce disease in mice [17], virus replication occurs in mouse embryonic fibroblasts (MEFs), and this cell type has been used to examine various virus-host interactions [18, 19]. Furthermore, the mechanisms underlying restriction of EBOV replication in rodents are not well understood and are of interest in development of better small-animal models of disease [20]. Therefore, to begin to examine the role of the ER in EBOV replication and how this may differ between viral strains, we compared the replication of EBOV–Makona GCO7 or EBOV-Mayinga in MEFs from wild-type or FAM134B−/− mice. This revealed a remarkable antiviral role of ER-phagy in limiting EBOV replication.
METHODS
Biosafety Statement
All infections with EBOV-Mayinga (1976) and EBOV-Makona (GCO7 2014) were performed under biosafety level 4 (BSL-4) conditions at the Rocky Mountain Laboratories Integrated Research Facility (Hamilton, Montana). Standard operating protocols for working with EBOV and removing samples from BSL-4 conditions were approved by the institutional biosafety committee.
Cell Culture
MEFs from wild-type (FAM134B+/+) and FAM134B−/− mice have been previously described [15]. Cells were cultured in Dulbecco's minimal essential medium (DMEM; Sigma-Aldrich) supplemented with 10% (v/v) fetal bovine serum (inactivated by heat [56°C] for 30 minutes; Life technologies), 1% L-glutamine (2 mM; Life technologies), and 1% penicillin/streptomycin (100 U/mL; Life technologies) in 5% CO2 in a humidified incubator at 37°C. Cells were starved for 6 hours under Earl's balanced salt solution (Sigma-Aldrich) or Hank's buffered saline solution (Sigma-Aldrich). Lysosomal degradation was inhibited using bafilomycin A1 (BAFA1) at 100 nM for 6 hours. Cell-culture-grade BAFA1 and dimethyl sulfoxide (DMSO) were obtained from Sigma-Aldrich.
Viruses
The EBOVs used in the study were propagated on Vero E6 cells as previously described [4, 21], and titration was performed using serial 10-fold dilutions in triplicate across Vero cell monolayers in 96-well tissue culture plates (Corning). Following infection for 1 hour at 37°C, cells were overlayed with 1.2% carboxymethyl cellulose (Sigma) in modified Eagle's medium (Gibco) containing 3% heat-inactivated fetal bovine serum (Gibco), 1% L-glutamine, and 1% penicillin/streptomycin. At 4 days after infection, cells were washed with phosphate-buffered saline (PBS) and fixed with 10% formalin for 48 hours. Viral infectivity titers were determined using an indirect immunofluorescence assay and expressed as focus-forming units (FFU). Formalin-fixed cells were permeabilized with 0.1% Triton X-100 (Sigma) and blocked with 1% bovine serum antigen (Sigma), followed by incubation with primary antibody (poly-clonal rabbit anti-VP40 [1:500]) and then secondary antibody (goat anti-rabbit immunoglobulin G conjugated to fluorescein isothiocyanate [1:200]; Sigma). For each dilution, immunofluorescent foci were counted and averaged before calculating the number of FFU per milliliter.
Western Blot Analysis
Cells were washed in PBS and harvested with a cell scraper, collected by centrifugation, and lysed in RIPA buffer (50 mM Tris-HCl, 150 mM NaCl, 0.1% sodium dodecyl sulfate, 1% NP-40, 0.5% Na-deoxycholate, and DNase I) with complete protease and phosphatase inhibitors (Roche). Cellular membranes were pelleted by centrifugation, and the supernatant was reserved. An equal amount of protein was resolved by electrophoresis in the presence of sodium dodecyl sulfate on 10% polyacrylamide gels (Invitrogen). Proteins were transferred to a nitrocellulose membrane, using the iBlot Dry Blotting System (Invitrogen), and were probed with primary and secondary antibodies. Immunoreactive proteins were detected by the ECL Plus chemiluminescent system (GE Healthcare).
Antibodies
Primary and secondary antibodies were used at indicated dilutions. Anti-FAM134B (1:1000) was kindly provided by Dr Ingo Kurth (Jena University Hospital) [15]; anti-VP40 (1:2000) [22], anti-GP (1:10 000), and anti-NP (1: 500) were kindly provided by Dr Ayato Takada (Hokkaido University); and anti-actin (1:10 000), anti-vinculin (1:1000), and secondary anti–horseradish peroxidase (1:1000) were purchased from Sigma.
Immunofluorescence Microscopy
Cells were grown on cover slips and infected with EBOV–Makona GCO7 at a multiplicity of infection (MOI) of 0.1. At 6 days after infection, cells were fixed with 10% formalin for 48 hours. Cells were permeabilized with Triton-X 100 (0.1%) and sodium citrate (0.1%) for 10 minutes and then blocked with 3% goat serum in PBS (1×) for 30 minutes. Subsequently, the cover slips were incubated with primary antibody for 1 hour, washed in PBS (1×), and incubated with secondary antibody solution for 1 hour. Cover slips were then washed 3 times in PBS (1×) and then once in double-distilled water and mounted on microscopy slides, using mounting medium containing DAPI (Molecular Probes, Thermo Fisher). Images were captured using a LSM 710 (Zeiss) laser-scanning confocal microscope with a 40× objective. Four fields (approximately 500–600 cells/field) in both wild-type and FAM134B−/− MEFs were imaged. Image analysis of percentage-infected cells was determined using ImageJ software. The total number of cells and the number of infected cells were determined by staining nuclei with DAPI and anti-NP, respectively. Cells were set to threshold and subjected to background subtraction and image segmentation. The percentage of infected cells was calculated by dividing the number of cells positive for NP by the total number of cells.
Transmission Electron Microscopy
Cells grown on Thermanox cover slips were fixed with 2.5% glutaraldehyde in 0.1 M sodium cacodylate buffer and processed in a PELCO BioWave Pro laboratory microwave (Ted Pella, Redding, California). The cover slips were postfixed with 1% osmium tetroxide reduced with 0.8% potassium ferrocyanide, followed by treatment with 1% tannic acid and en bloc staining with uranyl acid replacement (UAR) stain. The cells were dehydrated using a gradient of ethanol series and infiltrated with Embed 812 resin. The resin blocks were polymerized overnight in an oven at 65°C. Thin sections were cut using a Leica UC6 ultramicrotome (Leica Microsystems, Vienna, Austria), stained with uranyl acid replacement and Reynolds’ lead citrate, and imaged on 120 kV Tecnai Bio Twin Spirit (FEI, Hillsboro, Oregon), using a Hammamatsu XR-100 digital camera system (AMT, Danvers, Massachusetts).
Statistical Analysis
Differences in viral titer between wild-type and FAM134B−/− MEFs were analyzed by 2-way ANOVA with the Sidak multiple comparisons post hoc test. Differences in percentage infection detected by immunofluorescence assay were determined by a Student t test, using Prism 6.0.
RESULTS
FAM134B Negatively Regulates EBOV Replication
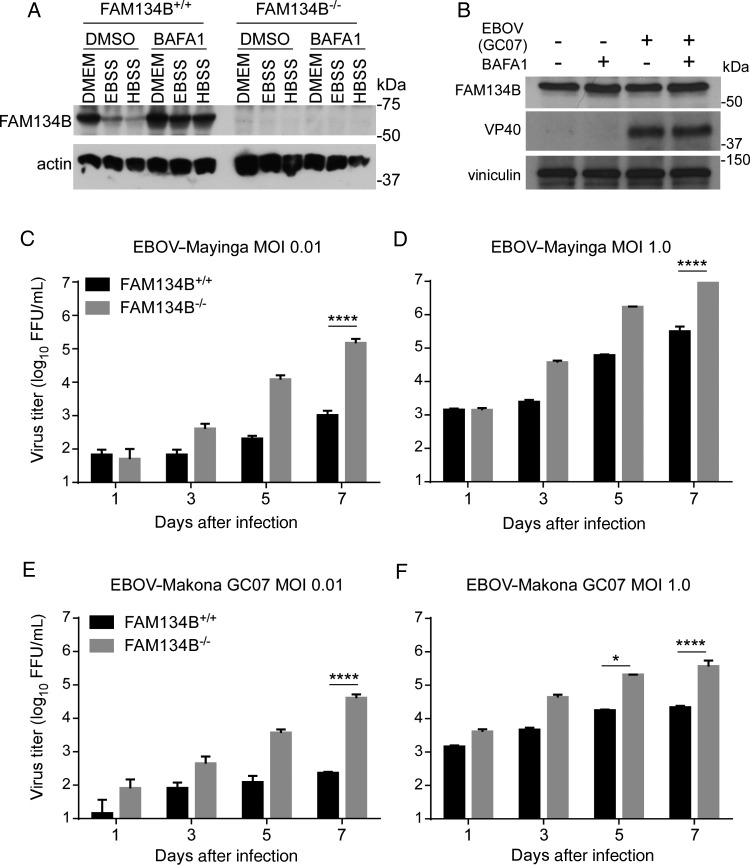
Expression of FAM134B was first confirmed in MEFs cultured with Earl's balanced salt solution or Hank's buffered saline solution, to induce starvation, in the presence or absence of BAFA1, to block lysosomal degradation (Figure 1A). FAM134B expression was as expected [15], with expression reduced under starvation conditions and rescued following lysosomal inhibition. FAM134B was not expressed in MEFs derived from FAM134B−/− mice. ER turnover by FAM134B-dependent selective autophagy is an ongoing event involved in normal ER homeostasis. One indicator that this process is active is an increase in FAM134B following lysosomal inhibition that prevents FAM134B degradation (Figure 1A) [15]. EBOV-Makona infection did not change FAM134B expression levels in untreated cells or alter the modest accumulation of FAM134B in the presence of BAFA1, suggesting that ER-phagy is ongoing in EBOV-infected cells and is not accelerated by infection (Figure 1B). To determine whether FAM134B expressed at physiological levels influenced EBOV replication, we evaluated virus replication in MEFs from FAM134B knockout mice. FAM134B+/+ (wild-type) and FAM134B−/− MEFs were infected with EBOV-Mayinga or EBOV-Makona GCO7 at 2 different MOIs, 0.01 or 1, and samples were harvested 1, 3, 5, and 7 days after infection. Compared with wild-type MEFs, FAM134B−/− cells produced approximately 1–2 log10 more (P < .0001) infectious EBOV 3, 5, and 7 days after infection (Figure 1C–F). The effect of FAM134B was observed at both MOIs, although larger differences in virus titers were observed at the lower MOI (0.01). The replication of both EBOV-Mayinga and EBOV–Makona GCO7 was increased in the absence of FAM134B, although EBOV-Mayinga replicated to overall higher levels in MEFs.
Figure 1.
FAM134B restricts replication of Ebola virus (EBOV) in mouse embryonic fibroblasts (MEFs). A, Endogenous expression of FAM134B in MEFs. FAM134B+/+ (wild-type) or FAM134B−/− cells were cultured under complete medium (Dulbecco's modified Eagle's medium [DMEM]) or subjected to nutrient deprivation with Earl's balanced salt solution (EBSS) or Hank's buffered saline solution (HBSS) for 6 hours in the presence of dimethyl sulfoxide (DMSO) or bafilomycin A1 (BAFA1). FAM134B levels were analyzed by Western blots. B, FAM134B expression upon EBOV strain Makona GCO7 (EBOV–Makona GCO7) infection. FAM134B+/+ cells were infected with EBOV–Makona GCO7 at a multiplicity of infection (MOI) of 10 for 3 days. Cells were treated with vehicle or BAFA1 (100 nM) for 6 hours before samples were harvested. FAM134B expression was analyzed by Western blots. C–F, FAM134B+/+ or FAM134B−/− MEFs were infected with EBOV-Mayinga or EBOV–Makona GCO7 at MOIs of 0.01 or 1, and supernatants were harvested 1, 3, 5, and 7 days after infection for titration. Error bars represent mean ± SD of experimental triplicates. Data are representative of 1 of 2 experiments. *P < .05 and ****P < .0001, by 2-way analysis of variance with the Sidak multiple comparison test. Abbreviation: FFU, focus-forming units.
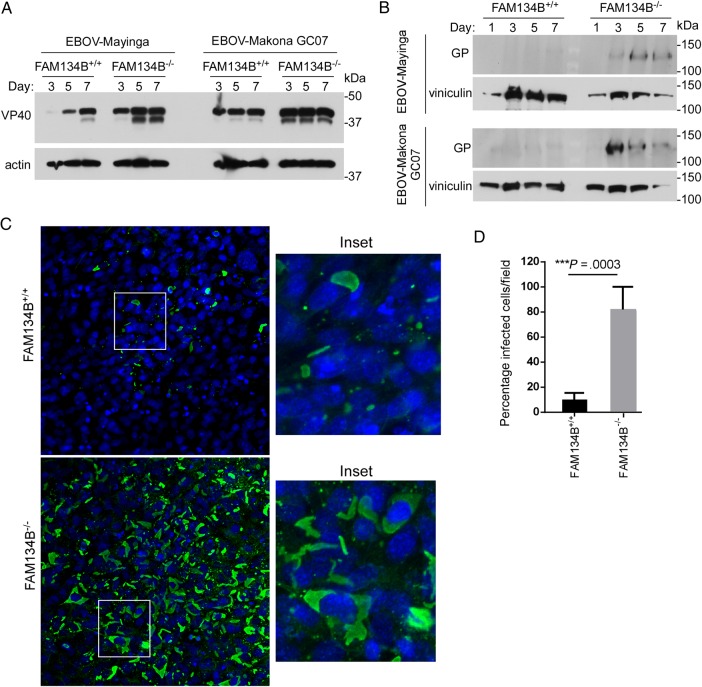
The observation of increased virus replication in the absence of FAM134B was supported by Western blot analysis demonstrating higher expression levels of 2 EBOV proteins, the major matrix protein VP40 (Figure 2A) and GP (Figure 2B). However, in contrast to the higher levels of infectious EBOV-Mayinga, the intracellular expression of EBOV–Makona GCO7 VP40 appeared to be greater than EBOV-Mayinga. Expression of GP was also apparent earlier in cells infected with EBOV–Makona GCO7. To determine whether the effects of FAM134B were mediated on a per cell basis or were the result of increased infection throughout the culture, the expression of NP was examined by immunofluorescence in cells infected with EBOV–Makona GCO7 (Figure 2C and 2D). Approximately 10% of wild-type MEFs were positive for NP, whereas 80% of FAM134B−/− cells were positive for this viral antigen (Figure 2D). In addition, NP-positive inclusions tended to be larger in the absence of FAM134B−/− (Figure 2C). This latter observation was supported by examining the ultrastructural phenotype of FAM134B−/− cells infected with either EBOV-Mayinga or EBOV-Makona (Figure 3). As expected, uninfected FAM134B−/− cells contained expanded ER (white arrow) with no obvious changes in other subcellular compartments as compared to wild-type MEFs. FAM134B−/− cells infected with either EBOV-Mayinga or EBOV–Makona GCO7 contained accumulations of nucleocapsid assemblies that often occupied the entire cytosol of infected FAM134B−/− cells as compared to more-limited accumulations of NP in wild-type controls (Figure 3). Taken together, these data demonstrate that endogenous FAM134B represents a substantial barrier to EBOV replication in MEFs.
Figure 2.
Expression of VP40 (A) and glycoprotein (GP; B) in FAM134B+/+ or FAM134B−/− cells. MEFs were infected with Ebola virus strain Mayinga (EBOV-Mayinga) or EBOV–Makona GCO7 at a multiplicity of infection (MOI) of 1. Visualization of actin or vinculin (for high-molecular-weight proteins) were used as loading controls. C, Nucleoprotein (NP) staining in EBOV-Makona–infected FAM134B+/+ or FAM134B−/− MEFs. Cells were infected with EBOV-Makona at a MOI of 1 for 6 days. Samples were stained for NP (green) and nuclei (DAPI; blue), and images were obtained by confocal microscopy. D, Quantification of infected NP-positive cells.
Figure 3.
Ultrastructural analysis of FAM134B+/+ or FAM134B−/− cells uninfected or infected with Ebola virus strain Mayinga (EBOV-Mayinga) or EBOV–Makona GCO7 at a multiplicity of infection of 1. Cells were fixed with 2.5% glutaraldehyde 3 days after infection and processed for transmission electron microscopy. Subcellular localization of endoplasmic reticulum (ER) (white arrows) and cytoplasmic nucleocapsid accumulation (white arrowheads) is indicated. Scale bar, 2 µm.
DISCUSSION
Processes of autophagy can be proviral or antiviral, depending on the virus and the cellular context [23]. Here we show that ER-phagy imposes a significant impediment to EBOV replication in MEFs. The absence of FAM134B rendered a relatively nonpermissive cell type permissive to EBOV replication. Both EBOV-Mayinga and EBOV–Makona GCO7 were equally sensitive to FAM134B-dependent restriction and replicated to a level of approximately 2 log10 higher in the absence of this selective receptor for ER-phagy when an MOI of 0.01 was used. This was associated with greater expression of viral proteins, including GP, VP40, and NP, and increased accumulation of nucleocapsids in cytosolic inclusion bodies. The increased levels of virus replication in FAM134B−/− cells enabled observation of some differences between virus strains. EBOV–Makona GCO7 did not replicate as efficiently as EBOV-Mayinga in MEFs despite the expression of higher levels of GP 3 days after infection in FAM134B−/− cells and higher levels of VP40 in both FAM134B+/+ and FAM134B−/− 3 days after infection. This may indicate that blocks in virus assembly or release may impede production of infectious virions by EBOV–Makona GCO7, at least in mouse cells. However, these results may be complicated by differences in virus stocks, such as the relative contribution of defective interfering particles. Further studies using reverse genetics and minigenomes derived from strains Makona or Mayinga in FAM134B knockout cells will help to clarify these observations.
Specifically, in regard to the role of FAM134B, it is conceivable that increased capacity of the ER leads to increased translation and processing of GP and may influence related events such as ER stress responses. However, the absence of FAM134B resulted in increased expression of multiple viral proteins, increased inclusion body formation, and greater production of infectious virus. Therefore, although GP has been shown to interact with the ER, this data shows that the ER, and, specifically, turnover of the ER by autophagy, is an important limiting factor to multiple facets of EBOV replication. This may be related to additional observations, including that intracellular trafficking of VP40 is associated with COPII vesicles, essential for transport from the ER to the Golgi apparatus [24, 25]. Alternatively, the loss of FAM134B may simply provide more ER and rough ER for general viral protein translation. However, the ER controls many aspects of cell biology [14], and therefore a number of questions remain, including the precise steps in virus infection and replication that are limited by FAM134B and whether this is associated with specific sequence differences between virus strains. Linking the role of the ER to particular events in virus replication will yield considerable insight into cellular mechanisms that restrict EBOV replication.
The observation that FAM134B is a limiting factor in EBOV replication raises two important possibilities. The first is that inducing ER-phagy may be a therapeutic target to limit EBOV replication. FAM134B is specific to ER-phagy and is not involved in either bulk autophagy or other types of selective autophagy [15, 16]. The precise pathways that control FAM134B-dependent ER-phagy are not yet clearly elucidated, but it might be expected that points of control mediated through enzymatic activity could be feasible targets for therapeutic manipulation. Antivirals based on targeting the host rather than the virus are thought to impart a high barrier to the evolution of viral resistance and therefore have desirable qualities as therapeutics [26]. Thus, further understanding ER-phagy and its role in human infection may identify drug targets to induce this pathway and limit EBOV replication. Second, the striking increases in production of infectious virus in the absence of FAM134B suggests that FAM134B−/− mice should be tested to determine whether their susceptibility to EBOV infection and their usefulness as a small-animal model of disease. FAM134B−/− mice are viable but experience neurodegeneration that is restricted to peripheral sensory nerves [15]. Despite this, a model using FAM134B−/− mice may have advantages over current rodent models if they do not require infection with host-adapted viruses to observe disease. Such a model could then be used for preclinical testing of therapeutics or vaccine efficacy against distinct viruses as they emerge, without the need for immunocompromised mice (such as those with knockout of the type I interferon receptor) or virus adaptation.
Notes
Acknowledgments. We thank Drs Ivan Dikic (Goethe University School of Medicine) and Christian Hübner (Jena University Hospital), for FAM134B−/− mouse embryonic fibroblasts; Dr Ingo Kurth (Jena University Hospital), for anti-FAM134B antibody; and Dr Ayato Takada (Hokkaido University), for the anti-glycoprotein and anti-nucleoprotein antibodies.
Financial support. This work was supported by the Division of Intramural Research, National Institute of Allergy and Infectious Diseases, National Institutes of Health.
Potential conflicts of interest. All authors: No reported conflicts. All authors have submitted the ICMJE Form for Disclosure of Potential Conflicts of Interest. Conflicts that the editors consider relevant to the content of the manuscript have been disclosed.
References
- 1.Bah EI, Lamah MC, Fletcher T et al. Clinical presentation of patients with Ebola virus disease in Conakry, Guinea. N Engl J Med 2015; 372:40–7. [DOI] [PubMed] [Google Scholar]
- 2.de La Vega MA, Stein D, Kobinger GP. Ebolavirus evolution: past and present. PLoS Pathog 2015; 11:e1005221. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Schieffelin JS, Shaffer JG, Goba A et al. Clinical illness and outcomes in patients with Ebola in Sierra Leone. N Engl J Med 2014; 371:2092–100. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Marzi A, Feldmann F, Hanley PW, Scott DP, Gunther S, Feldmann H. Delayed disease progression in cynomolgus macaques infected with Ebola virus makona strain. Emerg Infect Dis 2015; 21:1777–83. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Chan SY, Ma MC, Goldsmith MA. Differential induction of cellular detachment by envelope glycoproteins of Marburg and Ebola (Zaire) viruses. J Gen Virol 2000; 81:2155–9. [DOI] [PubMed] [Google Scholar]
- 6.Yang ZY, Duckers HJ, Sullivan NJ, Sanchez A, Nabel EG, Nabel GJ. Identification of the Ebola virus glycoprotein as the main viral determinant of vascular cell cytotoxicity and injury. Nat Med 2000; 6:886–9. [DOI] [PubMed] [Google Scholar]
- 7.Boehmann Y, Enterlein S, Randolf A, Muhlberger E. A reconstituted replication and transcription system for Ebola virus Reston and comparison with Ebola virus Zaire. Virology 2005; 332:406–17. [DOI] [PubMed] [Google Scholar]
- 8.Hoenen T, Shabman RS, Groseth A et al. Inclusion bodies are a site of ebolavirus replication. J Virol 2012; 86:11779–88. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Nanbo A, Watanabe S, Halfmann P, Kawaoka Y. The spatio-temporal distribution dynamics of Ebola virus proteins and RNA in infected cells. Sci Rep 2013; 3:1206. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Noda T, Ebihara H, Muramoto Y et al. Assembly and budding of Ebolavirus. PLoS Pathog 2006; 2:e99. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Bhattacharyya S, Hope TJ. Full-length Ebola glycoprotein accumulates in the endoplasmic reticulum. Virol J 2011; 8:11. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Dolnik O, Stevermann L, Kolesnikova L, Becker S. Marburg virus inclusions: a virus-induced microcompartment and interface to multivesicular bodies and the late endosomal compartment. Eur J Cell Biol 2015; 94:323–31. [DOI] [PubMed] [Google Scholar]
- 13.Volchkov VE, Feldmann H, Volchkova VA, Klenk HD. Processing of the Ebola virus glycoprotein by the proprotein convertase furin. Proc Natl Acad Sci U S A 1998; 95:5762–7. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Phillips MJ, Voeltz GK. Structure and function of ER membrane contact sites with other organelles. Nat Rev Mol Cell Biol 2016; 17:69–82. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Khaminets A, Heinrich T, Mari M et al. Regulation of endoplasmic reticulum turnover by selective autophagy. Nature 2015; 522:354–8. [DOI] [PubMed] [Google Scholar]
- 16.Mochida K, Oikawa Y, Kimura Y et al. Receptor-mediated selective autophagy degrades the endoplasmic reticulum and the nucleus. Nature 2015; 522:359–62. [DOI] [PubMed] [Google Scholar]
- 17.Bray M, Davis K, Geisbert T, Schmaljohn C, Huggins J. A mouse model for evaluation of prophylaxis and therapy of Ebola hemorrhagic fever. J Infect Dis 1998; 178:651–61. [DOI] [PubMed] [Google Scholar]
- 18.Okumura A, Rasmussen AL, Halfmann P et al. Suppressor of cytokine signaling 3 is an inducible host factor that regulates virus egress during Ebola virus infection. J Virol 2015; 89:10399–406. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.Saeed MF, Kolokoltsov AA, Freiberg AN, Holbrook MR, Davey RA. Phosphoinositide-3 kinase-Akt pathway controls cellular entry of Ebola virus. PLoS Pathog 2008; 4:e1000141. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20.Rasmussen AL, Okumura A, Ferris MT et al. Host genetic diversity enables Ebola hemorrhagic fever pathogenesis and resistance. Science 2014; 346:987–91. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21.Marzi A, Robertson SJ, Haddock E et al. EBOLA VACCINE. VSV-EBOV rapidly protects macaques against infection with the 2014/15 Ebola virus outbreak strain. Science 2015; 349:739–42. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22.Tsuda Y, Hoenen T, Banadyga L et al. An improved reverse genetics system to overcome cell-type-dependent Ebola virus genome plasticity. J Infect Dis 2015; 212(suppl 2):S129–37. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23.Dong X, Levine B. Autophagy and viruses: adversaries or allies? J Innate Immun 2013; 5:480–93. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24.Reynard O, Reid SP, Page A et al. Unconventional secretion of Ebola virus matrix protein VP40. J Infect Dis 2011; 204(suppl 3):S833–9. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25.Yamayoshi S, Noda T, Ebihara H et al. Ebola virus matrix protein VP40 uses the COPII transport system for its intracellular transport. Cell Host Microbe 2008; 3:168–77. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 26.Baumert TF, Verrier ER, Nassal M, Chung RT, Zeisel MB. Host-targeting agents for treatment of hepatitis B virus infection. Curr Opin Virol 2015; 14:41–6. [DOI] [PubMed] [Google Scholar]