Abstract
A molecular diagnostic method for robust detection of Ebola virus (EBOV) at the point of care (POC) directly from blood samples is described. This assay is based on reverse transcriptase loop-mediated isothermal amplification (RT-LAMP) of the glycoprotein gene of EBOV. Complete reaction formulations were lyophilized in 0.2-mL polymerase chain reaction tubes. RT-LAMP reactions were performed on a battery-operated isothermal instrument. Limit of detection of this RT-LAMP assay was 2.8 × 102 plaque-forming units (PFU)/test and 1 × 103 PFU/test within 40 minutes for EBOV-Kikwit and EBOV-Makona, respectively. This assay was found to be specific for the detection of EBOV, as no nonspecific amplification was detected in blood samples spiked with closely related viruses and other pathogens. These results showed that this diagnostic test can be used at the point of care for rapid and specific detection of EBOV directly from blood with high sensitivity within 40 minutes.
Keywords: Ebola virus, isothermal amplification, point of care, diagnostic test, RT-LAMP
Outbreaks of infectious diseases can turn into epidemics and/or pandemics causing massive loss of life and huge economic disruptions [1]. This threat was indeed highlighted during the recent outbreak of Ebola virus disease (EVD) in West Africa in December of 2013, which quickly became the deadliest occurrence of the disease since it was discovered in 1976. As of 10 February 2016, the Centers for Disease Control and Prevention reported 15 251 confirmed cases out of 28 639 suspected cases and a morbidity count of 11 316 [2]. However, the World Health Organization (WHO) believes these numbers are underestimates, owing to the inherent difficulty of collecting data in low resource and often geographically isolated environments. Although there has been a steady decline in the number of new cases in all 3 affected countries, a low level of EVD transmission might still be happening, as demonstrated by a new case in Sierra Leone [3].
The incubation period, or the time from infection to onset of symptoms, ranges from 2 to 21 days for EVD. Humans are not infectious until symptoms appear; however, once the disease presents, it still may take up to 3 days before the viral load reaches a level detectable by current methods [2]. Additionally, many of the symptoms of EVD resemble those of other, more common infectious diseases, such as malaria, typhoid fever, measles, West Nile virus infection, and other viral hemorrhagic fevers, such as those due to Crimean-Congo hemorrhagic fever virus, dengue virus, Lassa virus, and Marburg virus [4]. Timely diagnosis of infection and isolation of infected individuals is important for prevention and control [5] of these outbreaks.
Without any approved therapeutics or vaccines to treat patients with Ebola virus (EBOV) infection [6], the role of diagnostics is even more important to ensure implementation of control measures and optimization of healthcare resources [7]. To date, many diagnostic tests such as GeneXpert [8], Idylla [9], real-time reverse transcription–polymerase chain reaction (RT-PCR) assays [10], and immunoassays [11], have been developed for the detection of EBOV, but most of these assays are meant to be used by trained laboratory personnel and require additional infrastructure, such as cold storage of regents, laboratory equipment, and lengthy sample-preparation steps [12]. While these diagnostic tests are easy to run in countries that have a good healthcare system, they are problematic in many parts of the world, because of limited laboratory capacity and logistical infrastructure [13]. Also, transportation of samples to specialized laboratories from remote areas forces patients and their families to wait several days for test results, postponing treatment and increasing the chances for further transmission. This crucial delay in treatment also leads to longer hospitalization times, which increases the burden on the healthcare system and increases the likelihood of nosocomial transmission [12, 14]. Long delays in transportation of samples from the point of collection in remote areas to the central testing facilities also affect the integrity of the sample, thus compromising the test results [15]. Concerned over the lack of rapid diagnostic tests for EVD, the WHO issued a call for developing rapid and simple EVD diagnostic tests that can be used in low resource settings [13, 16].
Isothermal amplification methods such as helicase-dependent amplification [17] and loop-mediated isothermal amplification (LAMP) [18] are suitable for diagnostic assays that can be used at the point of care (POC). These methods offer advantages over other nucleic acid testing methods, such as PCR, in terms of faster time to results, capacity to use crude sample, simple instrumentation, and ease of use. These advantages allow the diagnostic assays to be performed outside of centralized laboratories, in POC environments like remote clinics, hospital emergency rooms, and particularly in remote areas of need.
Here we report on the development of an RT-LAMP method for rapid detection of EBOV directly from whole blood. This assay is based on the amplification of glycoprotein (GP) gene of EBOV and performed on a small, portable, battery-operated device, AmpliFire (Douglas Scientific, Minnesota), with a total assay time of 40 minutes. Furthermore, assay reagents were dried in reaction tubes, and a simple, rapid sample-preparation method was also developed to aid in quick reaction set up.
MATERIALS AND METHODS
Viral RNA Extracts
Viral RNA extracts of 2 strains of EBOV, H. sapiens wt/GIN/2014/Makona- Gueckedou-C05 (EBOV-Makona; KJ660348.2) and Zaire ebolavirus strain Kikwit 1995 (EBOV-Kikwit; JQ352763), were obtained from the University of Texas Medical Branch (UTMB; Galveston, Texas). RNA extraction was performed using Trizol LS (Invitrogen, California) at a ratio of 1 mL of virus supernatant to 5 mL of Trizol LS, which has been shown to inactivate filoviruses [19]. Briefly, in the biosafety level 4 (BSL-4) facility, 1 mL of virus supernatant was added to 5 mL of Trizol LS for each virus examined, and the mixture was vortexed and allowed to sit for 10 minutes at room temperature. This preparation was then placed in a new tube and disinfected and passed through the disinfectant dunk tank for RNA extraction at a BSL-2 facility. RNA was then extracted with a Direct-zol RNA mini-prep kit (Zymo Research, California) per the manufacturer's instructions.
LAMP Primer Design
Conserved regions of the EBOV GP were identified by aligning the nucleotide sequences of various EBOV isolates (JQ352763, KM233114, KM233110, KT725293, KR006941, KP096420, KP342330, AF086833.2, KR006950, KP260802, KR817090, KR817211, KJ660348, and KR534529) from GenBank (available at: http://www.ncbi.nlm.nih.gov) using ClustalW (available at: http://www.megasoftware.net). LAMP primers targeting conserved 200–400 bp regions were designed using the online primer design software Primer Explorer (available at: https://primerexplorer.jp/e/). Primers were designed to provide 100% specificity, based on BLAST analysis (available at: http://www.ncbi.nlm.nih.gov; Table 1).
Table 1.
List of Loop-Mediated Isothermal Amplification Primers Used in the Present Study
| Target, Primer Name | Sequence (5′ to 3′) | Genome Position | Reference |
|---|---|---|---|
| Ebola virus | |||
| F3 | GACGGGAGTGAGTGTCTACC | 6388-6406 | This study |
| B3 | AGCTTGGGGCAGTATCAGAA | 6605-6586 | |
| FL | GCACATACCGGCACC | 6453-6440 | |
| BL | CTTCCTGTATGATCGACTTGCTTC | 6516-6538 | |
| FIP (F1c + F2) | GGCACATGGTCCCGTTCCTGATTTTTTAGCGCCAGACGGGATTCG | 6482-6462; 6411-6427 | |
| BIP (B1c + B2) | TGCCTTCCACAAAGAGGGTGCTTTTTGCGAAAGTCGTTCCTCGGT | 6492-6511; 6568-6551 | |
| MS2 phage | |||
| F3 | TGTCATGGGATCCGGATGTT | 2050-2069 | [20] |
| B3 | CAATAGAGCCGCTCTCAGAG | 2252-2233 | |
| FL | CCAGAGAGGAGGTTGCCAA | 2113-2095 | |
| BL | TGCAGGATGCAGCGCCTTA | 2176-2194 | |
| FIP (F1c + F2) | GCCCAAACAACGACGATCGGTAAAACCAGCATCCGTAGCCT | 2136-2115; 2074-2092 | |
| BIP (B1c + B2) | GCACGTTCTCCAACGGTGCTGGTTGCTTGTTCAGCGAACT | 2140-2158; 2218-2200 |
Cloning of EBOV LAMP Target Sequence
For use in a BSL-2 facility, a recombinant EBOV (rEBOV) was generated by amplifying a short region of the GP gene (370 bp) containing the EBOV target region corresponding to the amplicon generated by LAMP primers and cloning it into a plasmid. For this, extracted EBOV-Makona RNA was reverse transcribed into complementary DNA (cDNA), using the OmniScript RT Kit (Qiagen, Valencia, California) and the primers EBM13 For (5′- GATTGAATTCAAGATGGGGCTTCAGGTC-3′; 6284-6301) and EBM13 Rev (5′- GATTAAGCTTACATGGGTAATCCTCATGTTTGTGGTAGAATAATAGCCACTCGAC-3′; 6654-6629), according to the manufacturer's instructions. The cDNA was purified and cloned into the HindIII-EcoRI sites of a kanamycin-resistant derivative of pT3T7. The plasmid was transformed into the bacterial strain E. cloni 10G (Lucigen, Wisconsin).
Instrumentation and Threshold Cutoff
Initial optimization experiments were performed on a real-time thermocycler instrument (iQ5, Bio-Rad, California). Amplification was monitored by detection of FionaGreen fluorescence and quantified by the instrument software at 30-second intervals. The time to result was set as the time at which the fluorescence crossed a threshold of 10% of maximum fluorescence. Samples were considered negative if they failed to cross the threshold. Later experiments were performed on the AmpliFire instrument (Douglas Scientific, Minnesota). This device is optimized for isothermal chemistry and allows real time monitoring of amplification. To calculate the time to result, threshold was set as half of the maximum fluorescence.
Optimization of EBOV RT-LAMP Assay
An RT-LAMP assay for detection of EBOV was developed using OmniAmp 2X Isothermal Master Mix (Lucigen, Wisconsin). This master mix is formulated for LAMP and contains optimal concentrations of betaine, salts, dNTPs, and OmniAmp polymerase [20]. The final concentrations of the reaction mixes were 1X OmniAmp Master Mix, 2 mM FionaGreen dye (Marker Gene, OR), 1X LAMP primer mix (IDT, IA; stock solution, 20X), and 5 μL of RNA, brought to volume (25 μL) with DNase-RNase–free water and incubated in a real-time thermocycler (iQ5, Bio-Rad, California) at an optimum temperature for 40 minutes. The optimum reaction temperature was determined using a gradient of 68°C–74°C. To further verify the results, reaction products were visualized by electrophoresis on ethidium bromide–stained 2% agarose gels.
EBOV RT-LAMP With Lyophilized Reagents
To allow ambient storage, 50-µL aliquots of the complete 1X RT-LAMP formulation, including OmniAmp polymerase, primers, and Fiona Green dye, were dispensed into 0.2-mL PCR tubes (USA Scientific, Florida) and lyophilized in-house, using a VirTis AdVantage 2.0 bench-top lyophilizer (SP Scientific, New York). To overcome the inhibitory effect of the sample input matrix (whole blood), the optimal lyophilized formulation contained higher concentrations of magnesium sulfate, dye, and primers relative to the wet formulation. Additionally, 10% Trehalose (Sigma, St. Louis, Missouri; stock solution, 40%) was used as an excipient to aid in the lyophilization process. After lyophilization, tubes were capped and packed in foil bags (Sorbent Systems, California) with a desiccant pouch and stored at room temperature until used.
Development of a Rapid Sample-Preparation Method
For use in low-resource settings, we developed a rapid sample-preparation method based on dilution of the sample into a lysis buffer, followed by filtration and addition to the lyophilized reagents. Field samples were simulated by using human whole blood (BioreclamationIVT, New York) spiked with E. cloni cells containing a plasmid carrying the LAMP target sequence. Samples were added to the lysis buffer (Lucigen, Wisconsin) at 5% dilution followed by filtration using an SQ Easy filter (pore size, 10 μm; Porex, Georgia) into a clean 1.5-mL microcentrifuge tube. As a positive control for the sample-preparation step, MS2 phage (Zeptomatrix, New York) was included in the lysis buffer at a final concentration of 107 PFU/mL and detected with MS2-specific LAMP primers (Table 1). The resulting filtrate was used directly as a template in the LAMP reaction.
Sensitivity and Specificity of EBOV RT-LAMP Assay
For sensitivity testing, 10-fold serial dilutions of EBOV RNA (ZEBOV-Kikwit and EBOV-Makona) were made in 25 mM Tris buffer (pH 8.0), and 5 µL of each dilution was used as the template in a 25-µL reaction mixture. Reaction tubes were incubated at 72°C in a real-time thermocycler (iQ5, Bio-Rad, California) for 40 minutes.
To determine the sensitivity of the rapid sample-preparation method, 10-fold serial dilutions of target viruses, ZEBOV-Kikwit (stock concentration, 1.12 × 107 PFU/mL) and EBOV-Makona (4 × 107 PFU/mL) were made in human whole blood (BioreclamationIVT, New York). Blood with viral dilutions of 10−1 to 10−4 was added to the lysis buffer (containing 107 PFU/mL MS2 phage) at 5% vol/vol, followed by filtration into 1.5-mL microcentrifuge tubes. One tube with no template added was used as a negative control. Fifty microliters of each filtrate was added to the lyophilized reagents and incubated in the AmpliFire instrument at 72°C for 40 minutes.
Specificity of this RT-LAMP assay was evaluated using various bacterial and viral pathogens (Table 2). For specificity testing, a 1:10 dilution of each pathogen was made in human whole blood (BioreclamationIVT, New York) and analyzed as described above. Final reaction products were visualized by electrophoresis on 2% agarose gels stained with ethidium bromide.
Table 2.
List of the Pathogens Used for the Evaluation of the Specificity of Ebola Virus (EBOV) Reverse Transcription–Loop-Mediated Isothermal Amplification (RT-LAMP)
| Sample | Isolate | Source | Part Number | Stock Titer | Titer/Test (50 µL) |
|---|---|---|---|---|---|
| 1a | Marburg virus–Angola | UTMB | Not available | 8 × 107 PFU/mL | 2 × 104 PFU/mL |
| 2a | Marburg virus–Musoke | UTMB | Not available | 4.4 × 106 PFU/mL | 1.1 × 103 PFU/mL |
| 3a | Lassa virus | UTMB | Not available | 1.75 × 106 PFU/mL | 4.25 × 102 PFU/mL |
| 4a | Crimean-Congo hemorrhagic fever virus | UTMB | Not available | 1 × 107 PFU/mL | 2.5 × 103 PFU/mL |
| 5 | Respiratory syncytial virus A (2006 isolate) | Zeptometrix | 0810040ACF | 1.95 × 107 U/mL TCID50 | 5.36 × 103 units |
| 6 | Respiratory syncytial virus B (CH93(18)-18) | Zeptometrix | 0810040CF | 1.51 × 106 U/mL TCID50 | 4.16 × 102 units |
| 7 | Influenza A virus (Wisconsin/67/05) | Zeptometrix | 0810252CF | 1.41 × 105 U/mL TCID50 | 3.88 × 101 units |
| 8 | Influenza B virus (Massachusetts/2/12) | Zeptometrix | 0810239CF | 1.41 × 105 U/mL TCID50 | 3.88 × 101 units |
| 9 | Salmonella enterica subspecies arizonae | ATCCd | ATCC 13314 | 1.30 × 108 CFU/vial (1 mL) | 3.58 × 104 CFU |
| 10 | Salmonella enterica serotype Typhi | Zeptometrix | 0801933 | 1.89 × 109 CFU/mL | 5.20 × 105 CFU |
| 11 | Pseudomonas aeruginosa | ATCC | ATCC 10145 | 9.15 × 107 CFU/mL | 2.52 × 104 CFU |
| 12 | Salmonella sonnei | ATCC | ATCC 29930 | >104 CFU/mL | 2.75 × 101 CFU |
| 13 | Plasmodium vivax | ATCC | ATCC 30152 | 4.90 × 106 U/mL TCID50 | 1.35 × 103 units |
| 14 | Plasmodium falciparum | ATCC | ATCC 30932 | 2.84% parasitemia/vial (0.7 mL) | 0.02% parasitemia |
| 15 | Dengue virus serotype 1 (Hawaii) | Zeptometrix | 0810088CF | 2.45 × 105 U/mL TCID50 | 6.74 × 101 units |
| 16 | Dengue virus serotype 2 (New Guinea) | Zeptometrix | 0810089CF | 3.16 × 105 U/mL TCID50 | 8.69 × 101 units |
| 17 | Dengue virus serotype 3 (strain H87) | Zeptometrix | 0810090CF | 1.15 × 107 U/mL TCID50 | 3.16 × 103 units |
| 18 | Dengue virus serotype 4 (H241) | Zeptometrix | 0810091CF | 3.39 × 107 U/mL TCID50 | 9.32 × 103 units |
| 19 | Vibrio cholerae (Z133) | Zeptometrix | 0801902 | 1.90 × 1010 CFU/mL | 5.23 × 106 CFU |
Abbreviations: ATTC, American Type Culture Collection; CFU, colony-forming units; PFU, plaque-forming units; TCID50, 50% tissue culture infective dose; UTMB, University of Texas Medical Branch, Galveston.
a Specificity experiments using these pathogens were done at the UTMB in a biosafety level 4 facility.
Real-time RT-PCR
Primers/probe targeting the VP30 gene of EBOV were used for quantitative real-time PCR [21] with the probe 6-carboxyfluorescein (6FAM)-5′-CCG TCA ATC AAG GAG CGC CTC -3′-6 carboxytetramethylrhodamine (Life Technologies, California). EBOV RNA was detected using the CFX96 detection system (BioRad Laboratories, California) in One-step probe qRT-PCR kits (Qiagen, California) with the following cycle conditions: 50°C for 10 minutes, 95°C for 10 seconds, and 40 cycles of 95°C for 10 seconds and 59°C for 30 seconds. Cycle thresholds representing EBOV genomes were analyzed with CFX Manager Software, and data are shown as genome equivalents (GEq). To create the GEq standard, RNA from EBOV stocks was extracted, and the number of EBOV genomes was calculated using Avogadro's number and the molecular weight of the EBOV genome.
Biosafety Testing of Sample-Preparation Buffer
A virus seed stock for ZEBOV-Makona (NCBI accession KJ660347) was used to spike 100 μL into 100 μL of blood or cell culture medium. A total of 25 μL of this mixture was added to 475 μL of sample-preparation buffer (Lucigen, Wisconsin) or cell culture medium alone as a positive control. Virus and inactivation buffer mixtures were allowed to incubate for 10 minutes at room temperature or at 80°C. Tubes were allowed to cool (if necessary) for 5 minutes and then the mixtures were transferred to a new tube and allowed to incubate for another 10 minutes to mimic the time it would take to retrieve the sample after disinfection procedures for removal.
Inactivation was assessed by placing dialyzed sample onto Vero E6 cells and observing cells for cytopathic effect (CPE) or by plaque-forming unit (PFU) analysis. Prior to the addition of the ZEBOV/inactivation buffer mixture to the cell culture, the mixture was subjected to dialysis, using a single-use Rapid Equilibrium Dialysis device to remove cell-toxic salts. The inactivation efficiency of the buffer was determined by adding the dialysate to Vero E6 cells (ATCC, CRL-1586) and monitoring the CPE over 12 days of incubation. If any virus CPE was observed at day 8 after infection, the PFU assay was used to verify and quantify any remaining live virus in the medium.
PFU were assessed by 10-fold dilutions of cell culture supernatant from inactivation tests, placing 100 μL of supernatant into 900 μL of diluent. Duplicate wells using 200 μL from the dilutions were used to inoculate Vero E6 monolayers.
Statistical Analysis
The Tukey-Kramer honest significant difference test was used to compare the mean values of the time to result (minutes), with a P value of <.05 considered to be significant. The analysis was performed using JMP statistical software (JMP, SAS Institute, 2003).
RESULTS
Optimization of Reaction Temperature
For determination of optimum temperature, reactions were performed using viral RNA extracts of EBOV-Makona as a template at temperatures of 68°, 70°, 72°, and 74°C for 40 minute. Optimum time to result (minutes), sensitivity, and lack of nonspecific amplification were obtained when the reaction was performed at 72°C. All subsequent reactions were performed at 72°C.
Sensitivity and Specificity of the RT-LAMP Assay
The sensitivity of EBOV detection by this new RT-LAMP method was compared to that of real-time RT-PCR, using 10-fold serial dilutions of viral RNA of 2 strains of EBOV, Makona and Kikwit. The limit of detection (LOD) was about 10 RNA copies/µL for both the strains. These results were comparable or superior to those of real-time PCR (Table 3).
Table 3.
Comparative Sensitivity of Reverse Transcription–Loop-Mediated Isothermal Amplification (RT-LAMP) With Real-time Polymerase Chain Reaction (PCR) Analysis
| RNA Level, Copies/µL | EBOV-Kikwit |
EBOV-Makona |
||
|---|---|---|---|---|
| LAMP, Time to Result, min | Real-time PCR, GEq | LAMP, Time to Result, min | Real-time PCR, GEq | |
| 1 × 108 | 11.3 | 19.7 | 8.0 | 18.8 |
| 1 × 107 | 12.3 | 24.3 | 9.2 | 22.5 |
| 1 × 106 | 15.5 | 28.6 | 10.5 | 26.1 |
| 1 × 105 | 19.0 | 31.0 | 12.9 | 29.7 |
| 1 × 104 | 26.5 | 34.1 | 16.4 | 33.2 |
| 1 × 103 | 31.2 | 38.3 | 20.4 | 36.9 |
| 1 × 102 | 28.2 | ND | 25.3 | 39.9 |
| 1 × 101 | 26.3 | ND | 27.2 | ND |
For RT-LAMP, 5 µL of template (genomic RNA) was used in a 25-µL reaction. For qRT-PCR, Ct values representing EBOV genomes were analyzed with CFX Manager Software, and data are shown as genome equivalents, based on an EBOV RNA genomic standard.
Abbreviations: EBOV, Ebola virus; GEq, genome equivalent; ND, not detected.
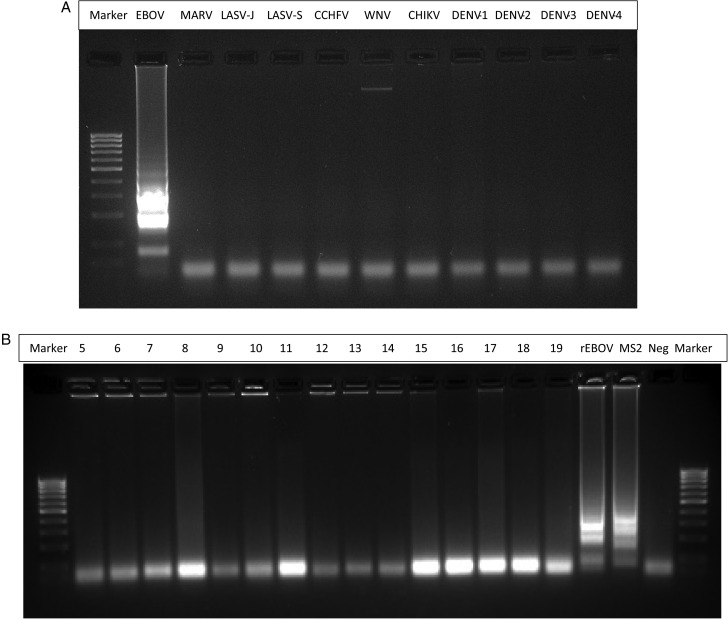
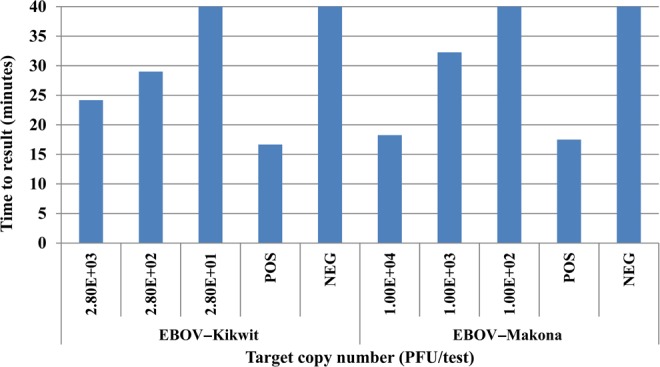
Sensitivity and Specificity of the Rapid Sample Preparation Method
To evaluate the sensitivity of the rapid sample-preparation method, 10-fold serial dilutions of the target (EBOV-Kikwit and EBOV-Makona) were made in human whole blood, and dilutions of 10−1–10−4 were tested using lyophilized RT-LAMP reagents. The assay gave a positive result down to 2.8 × 102 PFU/test for EBOV-Kikwit and 1 × 103 PFU/test for EBOV-Makona within 40 minutes (Figure 1). No amplification was observed with non-EBOV targets when tested in the presence of blood. To further confirm the result, postamplification reaction products were analyzed by gel electrophoresis. The MS2-positive control and EBOV samples showed a ladder-like pattern of multiple amplification bands, as is typical for LAMP products; none of the other pathogens showed any amplification (Figure 2), suggesting that this RT-LAMP method is specific for EBOV.
Figure 1.
Sensitivity of the Ebola virus (EBOV) reverse transcription–loop-mediated isothermal amplification method. Sensitivity was determined against 2 strains of EBOV, EBOV-Kikwit (stock concentration, 1.12 × 107 plaque-forming units [PFU]/mL) and EBOV-Makona (4 × 107 PFU/mL). Ten-fold serial dilutions of each virus were made in human whole blood. Each dilution was added to the lysis buffer at 5%, and 50 µL of this suspension was used to reconstitute lyophilized reagents. Abbreviations: NEG, negative control; POS, positive control (MS2 phage).
Figure 2.
Specificity of the Ebola virus (EBOV) reverse transcription–loop-mediated isothermal amplification (RT-LAMP) method. After completion of the reaction (40 minutes) LAMP reaction products were separated on 2% agarose gel. A, Specificity of EBOV RT-LAMP, using RNA extracts. A total of 5 µL of RNA was used as template in a 25-µL reaction mix. The reaction was performed at 72°C for 40 minutes. CCHFV, Crimean-Congo hemorrhagic fever virus; CHIKV: Chikungunya virus; DENV-1, dengue virus serotype 1; DENV-2, dengue virus serotype 2; DENV-3, dengue virus serotype 3; DENV-4, dengue virus serotype 4; EBOV, Ebola virus-Makona; LASV-J, Lassa virus–Josiah; LASV-S, Lassa virus–Sauer; MARV, Marburg virus–Musoke; WNV: West Nile virus. B, Specificity of EBOV RT-LAMP, using different pathogens. Each pathogen was diluted 1:10 in human whole blood. Each dilution was added to the lysis buffer at 5%, and 50 µL of this suspension was used to reconstitute lyophilized reagents. The reaction was performed at 72°C for 40 minutes. Abbreviations: MS2, MS2 phage (positive control); Neg, negative control (no target); rEBOV, recombinant EBOV-Makona complementary DNA plasmid. A list of other pathogens is provided in Table 2.
Biosafety Testing of Sample Preparation Buffer
Results of biosafety testing of sample-preparation buffer are presented in Table 4. Results indicate that no detectable ZEBOV could be detected 8 days after infection in the presence of the sample-preparation buffer after 10-minute incubation at 80°C. No loss in virus titer was observed in positive controls, with or without incubation at 80°C.
Table 4.
Biosafety Testing of Sample Preparation Buffer
| Treatment | Virus Titer 8 d After Infection |
|
|---|---|---|
| Room Temperature (22°C) | 80°C | |
| Positive control | ||
| Virus + CCMa | >1 × 107 | >1 × 107 |
| Virus + blood | >1 × 106 | >1 × 107 |
| Negative control | ||
| Bufferb + CCM | Not tested | <25 |
| Test | ||
| Virus + CCM + buffer | >1 × 107 | <25 |
| Virus + blood + buffer | >1 × 107 | <25 |
Zaire ebolavirus strain Makona (National Center for Biotechnology Information accession no. KJ660347) was mixed with whole blood and added to cell culture medium or sample-preparation buffer. After incubation for 10 minutes at room temperature (22°C) and 80°C, samples were added to monolayers of Vero E6 cells.
a Minimum essential medium for cell culture (Gibco, New York).
b Sample preparation buffer (Lucigen, Wisconsin).
Guard Banding
To ensure robustness of the RT-LAMP diagnostic test, we tested a range of blood input volumes (from 3.5% to 6%). We also tested different volumes of filtrate, ranging from 40 µL to 60 µL, used to reconstitute the lyophilized reagents. This test showed a broad working range at the LOD, tolerating blood inputs of 4%–5.5% without any significant differences in the time to result (Figure 3A and 3B). Similarly, the test was able to tolerate variations of ±10% in volume of filtrate without any significant change in the time to result when tested at LOD.
Figure 3.
Performance of the Ebola virus (EBOV) reverse transcription–loop-mediated isothermal amplification method using different levels of sample input. A, Human whole blood was spiked with target (E. colni cells and recombinant EBOV) and added to the lysis buffer at various levels (3.5%–6%). A total of 50 µL of this suspension was used to reconstitute lyophilized reagents, followed by incubation at 72°C for 40 minutes. Means with the same letter are not significantly different from each other (P > .05, by the Tukey-Kramer test,). B, Human whole blood was spiked with target (recombinant EBOV) and added to the lysis buffer at 5%. Various volumes (40–60 µL) of this suspension were used to reconstitute lyophilized reagents, followed by incubation at 72°C for 40 minutes. Means with the same letter are not significantly different from each other (P > .05, by the Tukey-Kramer test).
DISCUSSION
The recent outbreak of EVD in West Africa demonstrated that national and world health organizations are ill prepared for countering such infectious disease crises. One factor that contributed to the severity of the outbreak was the lack of diagnostic tests that could be used at the POC for patient screening. Although the WHO and other international organizations deployed mobile laboratories for sample testing [13], their effectiveness was hampered by numerous challenges, such as testing cost, time to result, maintenance of cold storage for reagents, and a high level of biosafety [12]. But, most importantly, the majority of these testing laboratories were based in urban centers, thus requiring blood samples to be transported from remote rural areas for testing. This centralized testing of samples delayed the reporting of results from a few days to up to a week [22]. As a result, the WHO issued a call for developing “rapid, sensitive, safe and simple Ebola diagnostic tests” and issued guidelines for an ideal rapid diagnostic test [13, pp 4–5].
Toward this goal, we have developed a diagnostic test for rapid detection of EBOV at the POC. This assay is based on RT-LAMP amplification of the GP gene of EBOV and uses a thermotolerant enzyme, OmniAmp polymerase, which allows the reaction to be performed at an elevated temperature, which was 72°C in the present study [19]. Most diagnostic assays for EBOV detection target either the polymerase, nucleoprotein, or GP genes [8, 10, 23] For this RT-LAMP assay, we chose the GP gene because it is an important virulence factor of EBOV [21]. The GP gene is the target for other assays, such as Xpert [8], Idylla [9], and another RT-LAMP [7].
RT-LAMP methods for EBOV detection have been previously reported [7, 24–26], but all these methods require extraction of RNA from blood samples. Because the reaction developed in the present study is performed at high temperature, lysis and amplification occur concurrently. Because of this modification, reaction set up is easy, requires little time or expertise for sample preparation, and requires only simple equipment. Also, to reduce dependence on a cold chain for storage of reagents during shipping as well as in the laboratory, we lyophilized a complete formulation sufficient for 50-µL volumes in 0.2-mL PCR tubes without any loss in amplification efficiency for up to 60 days when stored at 22°C or 15 days at 42°C (data not shown).
To aid in interpretation, this assay is performed on a simple and easy to use isothermal amplification and detection platform, the AmpliFire instrument (Douglas Scientific, Minnesota). AmpliFire is a small bench-top instrument that is lightweight and battery operated, allowing it to be used at the POC. In this RT-LAMP, we used a fluorescent DNA-binding dye, FionaGreen, in the reaction mixture. Double-stranded DNA generated as a result of amplification binds to dye, allowing the reaction to be monitored in real time. On-board software determines whether a sample has positive, negative, or invalid results, thus minimizing user interpretation. In the RT-LAMP method described by Xu et al [7], lateral flow devices were used to visualize the amplification reaction. This method requires an additional step after amplification because reaction tubes need to be transferred into the lateral flow cassette, which increases the chance of sample mix-up. The cost of the assay is also higher because of the addition of lateral flow cassettes. Kurosaki et al [26] developed an RT-LAMP method performed on the Genie II instrument (Optigene, United Kingdom), in which the readout is based on detection of turbidity. This method is suitable for use with only extracted RNA and cannot be used to detect EBOV directly from blood samples, as the color of blood will make it difficult to detect the turbidity, making it unstable for POC situations. Use of dye in the RT-LAMP method described in this study enables the amplification signal to be detected even in presence of blood.
The sensitivity of our RT-LAMP method was found to be 10 RNA copies/µL, which is similar to that reported by others [7, 24], and the specificity was high. This RT-LAMP method showed sensitivity similar to that of the real-time RT-PCR method for both strains of EBOV (Makona and Kikwit), indicating that this method can detect the low copy numbers of target RNA. Although the real-time RT-PCR used in this study targets different region of EBOV genome, this method [21] is highly sensitive for the detection of EBOV.
The total assay time for RT-LAMP was 40 minutes, which is similar to that reported by Xu et al [7] but faster than what was reported by Kurosaki et al [26]. Furthermore, the LOD of this assay for direct detection of EBOV particles spiked into blood samples was 2.8 × 102 PFU/test for ZEBOV-Kikwit and 1 × 103 PFU/test for EBOV-Makona. Also, the assay was shown to have a wide working range (4%–5.5% blood input) without any loss in sensitivity.
Preliminary data indicate that 10-minute incubation at 80°C in the presence of the sample-preparation buffer inactivates EBOV. However, further studies are needed to verify this. Given the highly infectious nature of EBOV, this assay should be performed using full personal protective equipment, and any waste generated (before and after amplification) should be considered infectious and disposed of by following established guidelines for biohazardous waste.
In conclusion, the RT-LAMP assay described in this article can detect EBOV directly from blood within 40 minutes by using a portable instrument. This test meets the criteria for use at the POC as set by the WHO for a rapid diagnostic test. Advantages of this test are (1) the use of lyophilized reagents; (2) direct detection of EBOV from blood, with no sample-preparation step required; (3) easy work flow, as the reaction can be set up in 4 easy steps with no measuring required (Figure 4); and (4) the need for only a simple, easy-to-use instrument, with results displayed on screen at the end of a run and no need for interpretation by the user. This test can be used as an aid to gold-standard testing methods, as samples can be quickly screened at the POC and only presumptive positive samples tested further for confirmation by a secondary method such as real-time PCR. Use of this test enables healthcare workers to be better prepared to respond to EBOV outbreaks or any other disease outbreaks that can happen in the future.
Figure 4.
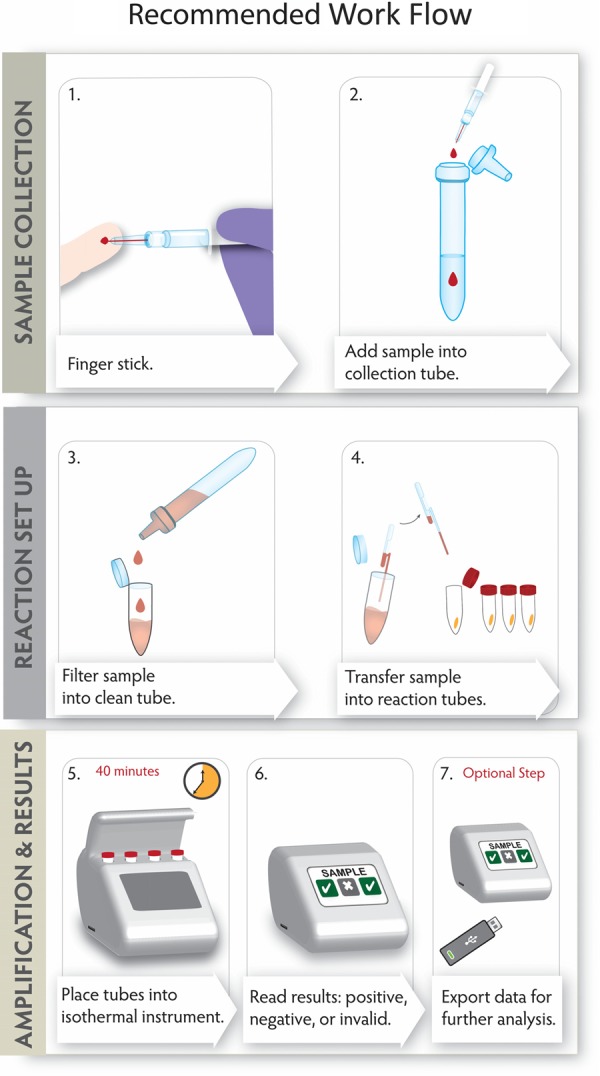
Recommended workflow for using the Ebola virus (EBOV) reverse transcription–loop-mediated isothermal amplification diagnostic test at the point of care. In step 1, a sample is collected using a 50-µL Minivette POCT (Sarstedt, Germany). In step 2, the sample is added to the lysis buffer predispensed (950 µL) in a sample collection module (SCM; Lucigen, Wisconsin). The nozzle of the SCM is fitted with a 10-μm filter. In step 3, sample is filtered into a clean 1.5-mL tube by squeezing the SCM. In step 4, using a 50-µL fixed-volume pipette, filtered sample is dispensed into reaction tubes. Step 5: Reaction tubes are incubated on AmpliFire (Douglas Scientific, Minnesota). In step 6, after 40 minutes, results are displayed on screen. In step 7, amplification data can be exported onto a USB for further analysis, if needed.
Notes
Acknowledgments. We thank Dr Tom Ksiazek, for providing the original EBOV-Kikwit, Marburg virus, Lassa virus, and Crimean-Congo hemorrhagic fever virus stocks used for this work.
Disclaimer. The content is solely the responsibility of the authors and does not necessarily represent the official views of the National Institutes of Health or the University of Texas Medical Branch at Galveston.
Financial support. This work was supported by the National Institute of Allergy And Infectious Diseases of the National Institutes of Health (awards R33AI100182 and UC7AI094660 for BSL-4 operations support of the Galveston National Laboratory).
Potential conflicts of interest. J. W. B., K. B., R. G., B. C., K. G., D. A. M., and Y. C. are employees of Lucigen, which intends to commercialize this diagnostic test after securing necessary approval from regulatory agencies. All other authors report no potential conflicts. All authors have submitted the ICMJE Form for Disclosure of Potential Conflicts of Interest. Conflicts that the editors consider relevant to the content of the manuscript have been disclosed.
References
- 1.Sands P, Mundaca-Shah C, Dzau VJ. The neglected dimension of global security – a framework for countering infectious disease crises. N Engl J Med 2016; 374:1281–7. [DOI] [PubMed] [Google Scholar]
- 2.Centers for Disease Control and Prevention. 2014 Ebola outbreak in West Africa. http://wwwcdcgov/vhf/ebola/outbreaks/2014-west-africa/indexhtml Accessed 10 February 2016.
- 3.World Health Organization. New Ebola case in Sierra Leone. WHO continues to stress risk of more flare-ups. http://apps.who.int/mediacentre/news/statements/2016/newebola-case/en/index.html Accessed 10 February 2016.
- 4.Racsa LD, Kraft CS, Olinger G, Hensley L. Viral hemorrhagic fever diagnostics. Clin Infect Dis 2016; 62:214–9. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Grolla A, Lucht A, Dick D, Strong JE, Feldmann H. Laboratory diagnosis of Ebola and Marburg hemorrhagic fever. Bull Soc Pathol Exot 2005; 98:205–9. [PubMed] [Google Scholar]
- 6.Cooper CL, Bavari S. A race for an Ebola vaccine: promises and obstacles. Trends Microbiol 2015; 23:65–6. [DOI] [PubMed] [Google Scholar]
- 7.Xu C, Wang H, Jin H et al. . Visual detection of Ebola virus using reverse transcription loop-mediated isothermal amplification combined with nucleic acid strip detection. Arch Virol 2016; 161:1125–33. [DOI] [PubMed] [Google Scholar]
- 8.Pinsky BA, Sahoo MK, Kleman M et al. . Analytical Performance Characteristics of the Cepheid GeneXpert Ebola Assay for the Detection of EbolaVirus. PLoS One 2015; 10:e0142216. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Cnops L, Eede PV, Pettitt J et al. . Development, evaluation, and integration of a quantitative reverse-transcription polymerase chain reaction diagnostic test for Ebola virus on a molecular diagnostics platform. J Infect Dis 2016; 214(suppl 3):S192–202. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Cherpillod P, Schibler M, Vieille P et al. . Ebola virus disease diagnosis by real-time RT-PCR: A comparative study of 11 different procedures. J Clin Virol 2016; 77:9–14. [DOI] [PubMed] [Google Scholar]
- 11.Broadhurst MJ, Kelly JD, Miller A et al. . ReEBOV Antigen Rapid Test kit for point-of-care and laboratory-based testing for Ebola virus disease: a field validation study. Lanccet 2015; 386:867–74. [DOI] [PubMed] [Google Scholar]
- 12.Nouvellet P, Garske T, Mills HL et al. . The role of rapid diagnostics in managing Ebola epidemics. Nature 2015; 528:S109–16. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Chua AC, Cunningham J, Moussy F, Perkins MD, Formenty P. The case for improved diagnostic tools to control Ebola virus disease in West Africa and how to get there. PLoS Negl Trop Dis 2015; 9:e0003734. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Zachariah R, Harries AD. The WHO clinical case definition for suspected cases of Ebola virus disease arriving at Ebola holding units: reason to worry? Lancet Infect Dis 2015; 15:989–90. [DOI] [PubMed] [Google Scholar]
- 15.Strecker T, Palyi B, Ellerbrok H et al. . Field evaluation of capillary blood samples as a collection specimen for the rapid diagnosis of Ebola virus infection during an outbreak emergency. Clinical Infect Dis 2015; 61:669–75. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.World Health Organization. Urgently needed: rapid, sensitive, safe and simple Ebola diagnostic tests. http://www.who.int/mediacentre/news/ebola/18-november-2014-diagnostics/en/ Accessed 1 March 2106.
- 17.Vincent M, Xu Y, Kong H. Helicase-dependent isothermal DNA amplification. EMBO Rep 2004; 5:795–800. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.Notomi T, Okayama H, Masubuchi H et al. . Loop-mediated isothermal amplification of DNA. Nucleic Acids Res 2000; 28:E63. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.Towner JS, Sealy TK, Ksiazek TG, Nichol ST. High-throughput molecular detection of hemorrhagic fever virus threats with applications for outbreak settings. J Infect Dis 2007; 196(suppl 2):S205–12. [DOI] [PubMed] [Google Scholar]
- 20.Chander Y, Koelbl J, Puckett J et al. . A novel thermostable polymerase for RNA and DNA loop-mediated isothermal amplification (LAMP). Front Microbiol 2014; 5:395. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21.Thi EP, Mire CE, Lee AC et al. . Lipid nanoparticle siRNA treatment of Ebola-virus-Makona-infected nonhuman primates. Nature 2015; 521:362–5. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22.Pathmanathan I, O'Connor K, Adams M et al. . Rapid assessment of Ebola infection prevention and control needs - six districts, Sierra Leone, October 2014. Morb Mortal Wkly Rep 2014; 63:1172–4. [PMC free article] [PubMed] [Google Scholar]
- 23.Gibb TR, Norwood DA, Woollen N, Henchal EA. Development and evaluation of a fluorogenic 5′ nuclease assay to detect and differentiate between Ebola virus subtypes Zarie and Sudan. J Clin Microbiol 2001; 39:4125–30. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24.Li H, Wang X, Liu W et al. . Survey and visual detection of Zaire ebolavirus in clinical samples targeting the nucleoprotein gene in Sierra Leone. Front Microbiol 2015; 6:1332. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25.Kurosaki Y, Takada A, Ebihara H et al. . Rapid and simple detection of Ebola virus by reverse transcription loop-mediated isothermal amplification. J Virol Methods 2007; 141:78–83. [DOI] [PubMed] [Google Scholar]
- 26.Kurosaki Y, Magassouba N, Oloniniyi OK et al. . Development and evaluation of reverse transcription-loop-mediated isothermal amplification (RT-LAMP) assay coupled with a portable device for rapid diagnosis of Ebola virus disease in Guinea. PLoS Negl Trop Dis 2016; 10:e0004472. [DOI] [PMC free article] [PubMed] [Google Scholar]