Abstract
Aim
To describe patient complaints and to examine possible associations between healthcare providers’ statements and reports of satisfaction/dissatisfaction.
Design
A retrospective and descriptive design was used to examine filed complaints.
Methods
Complaints from one Patient Advisory Committee in Sweden in 2011 was examined using three different protocols/reading guides (n = 618). Associations between contents in responses from healthcare providers and reports of satisfaction/dissatisfaction from the complainants were analysed.
Results
Less than one‐third of the complainants were satisfied after handling and with healthcare providers’ statements about the complaint. The most frequent causes for dissatisfaction were that the healthcare provider ‘did not tell the truth’ or ‘gave insufficient information’. There was a statistically significant association with dissatisfaction if the statement from the healthcare provider included the category ‘disagree/defend themselves’. Four categories were associated with being satisfied and the associations were statistically significant when two or more of these were combined.
Keywords: Patient advisory committee, patient complaints, patient safety, patient satisfaction, quality of health care, Sweden
Introduction
Patient complaints are considered a valuable source for quality improvement in health care (Reader et al. 2014). Moreover, patient satisfaction is an important issue for healthcare providers to fulfil their caring duties, to ensure patient safety and also for compassionate clinical nursing (Allan et al. 2015). In Sweden, the number of healthcare complaints is growing despite an increased patient focus in health care. In 2015 a new law was enrolled in Sweden – The Patient Act (2014:821) – that aims to reinforce and clarify the patients’ position and facilitate patients’ integrity, self‐determination and participation. The legislation has long been preceded by efforts in health care to achieve a higher degree of patient‐centered care. According to the act, patients are to be informed about their condition and available treatments. The patients also have the right to participate in all decisions about care. As a consequence, many Swedish healthcare organizations are currently making changes to clinical practice. Common complaints from patients concern (perceived) disrespect, disagreements over treatment, insufficient information, lack of confidence, that physicians are unavailable and lack of communication (Wofford et al. 2004). In Sweden, 85 per cent out of the total number of complaints of health care are addressed to patient advisory committees [PACs] (Kent 2008). The PACs have two major assignments: to help and support patients on the basis of their comments and complaints and to contribute to quality improvements in patient care. PACs do not exercise authority against healthcare personnel and cannot distribute warnings or withdraw licenses. The PACs’ assignment to help and support patients is often achieved by providing community information about patient insurance and the possibility to lodge complaint also to the National Board of Health and Welfare (or since 2013 to the Health and Social Care Inspectorate). These authorities examine health care professional's right to practice and if a licensed practitioner, for example, a physician or a nurse has failed, their license can be withdrawn. In total, the PACs in Sweden receive approximately 30,000 complaints each year. In the last four years the number has increased by 17% Despite the increase, the complaints concern less than one per thousand of all patient visits (Wessel et al. 2012). Subsequently, it has been argued that complaints filed at PACs are only ‘the tip of an iceberg’ (Wessel et al. 2012).
Background
Research about patient complaints are conducted from different perspectives. From a nursing perspective, human suffering can be understood as the main motive for care (Eriksson 2002). Sometimes, however, care turns out to be a cause for human suffering (Eriksson et al. 2006). Previous studies show that patients can perceive care, caregivers or healthcare organizations as incomprehensible, strange, ambiguous and unclear leading the patients to lose trust and faith in both caregivers and organizations (Eriksson and Svedlund 2007, Nordgren et al. 2007, Soderberg et al. 2012, Wessel et al. 2013). Frequently, such experiences come from experiences of insufficient communication, of patients being disrespectfully encountered, objectified, depersonalized, ignored or from feelings of powerlessness (Arman et al. 2004, Eriksson & Svedlund 2007, Nordgren et al. 2007, Reader & Gillespie 2013, Skar & Soderberg 2012, Soderberg et al. 2012, Wessel et al. 2013). Suffering caused by care does not only involve patients but also relatives and caregivers involved in the actual situation and the healthcare organization (Eriksson & Svedlund 2007, Reader & Gillespie 2013). In addition, nurses in clinical practice need to be aware of factors that can affect the relation to the patients, including the patients’ trust in healthcare professionals and in the healthcare organization (Nilsson et al. 2015). Nurses have a key role in facilitating and mediating patient experiences and their difficult position in care situations (Jangland et al. 2011).
Another research perspective concerns how patients perceive that healthcare providers receive and react on complaints. Studies show that physicians who receive complaints about themselves may react strongly. Feelings of shock or panic, anger towards the patient, regret, depression and even suicide can follow a complaint (Jain & Ogden 1999, Cunningham 2004). This raises concerns about whether the physicians’ reactions impose a risk that the complaints lead to worse care rather than better (Cunningham 2004). It has also been described that patients can perceive healthcare organizations as closed systems that are governed by routines and that healthcare providers protect each other after complaints. Therefore, patients can fear that a complaint will make the situation even worse (Soderberg et al. 2012).
One more considerable field of research is based on the perspective of patient safety. Robinson et al. claim that patient satisfaction is an integral component for measures of healthcare quality (Robinson et al. 2014). If complaints are systematically reviewed, they provide indications of problematic trends in health care both on institutional and individual levels (Bismark et al. 2013, Reader et al. 2014). Although patient complaints are inherently personal, emotional and not intended to investigate failures systematically, they can provide unique knowledge that is hard to get in other measurements (Reader et al. 2014). In a mapping of the extent to which health care is influenced by complaints in Sweden, it was found that quality improvement measures were made in only 4·4% of cases (Hagelin 2007).
The aims of this study were to describe patient complaints to PAC and to examine possible associations between content in the statements from caregivers and reports of satisfaction/dissatisfaction from the complainants and finally to describe the complainants′ reasons for being dissatisfied after receiving a statement from the healthcare provider.
The study
Design
A retrospective and descriptive design was used to examine filed complaints.
Method
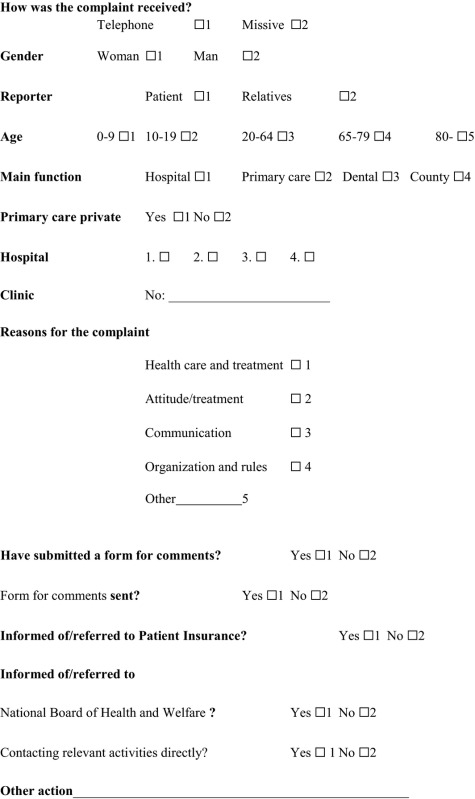
This study was based on files drawn up at a Swedish County PAC during 2011. The procedures at the PAC are that patients or relatives contact the PAC by telephone, letter or e‐mail. To communicate a written complaint the complainants are asked to fill in and return a form. If the form is returned to the PAC, it is sent to the director of the clinic with a request for a statement. Then, the statement is returned to the complainant together with a brief questionnaire (Appendix 1). There is a wide spectrum in the content of the complaints. From minor comments on medical examination/treatment, unnecessary costs and long wait, to severe remarks on discrimination, abuse or big disappointment and outrage against the caregiver in the context of death of a close relative.
Data collection
The material of the study consisted of 618 files at the PAC. The files varied in content but all contained complaints or grievances from a patient or a relative. There were both complete and incomplete files. Complete files consisted of a written complaint, a statement from the healthcare provider and a questionnaire response from a patient or a relative. In the questionnaire, the respondents were asked to answer whether they were satisfied with the healthcare providers’ statement or not. If they were dissatisfied, they were asked to state a reason. Incomplete files consisted only of notes from a phone call or a letter to the PAC and/or files where questionnaire responses were lacking. In 2011, there were 221 complete files. All these were included. In addition, 397 incomplete files (from 1 January 2011–31 August 2011) were included. The first step of the study was a pilot study of 200 cases. The first author (CS) and the third author (EMA) in cooperation read the complaints to determine variables for background factors. Next, the content of statements and questionnaire responses were analysed to establish content categories. This was made by CS and EMA through joint discussions and reflections until agreement was achieved. The material was then used to develop three reading guides/protocols: One for the details of the complaints (Appendix 2), one guide for significant/typical categories in statements from healthcare providers and one for the questionnaire responses both with 13 categories (Appendices 3 ‐ 4). In the second step of the study, data were collected according to the three reading guides/protocols. The files were read by CS and to calibrate assessments and when uncertainty aroused also by EMA and decisions about categorizations were made in cooperation.
Analysis
In the first step of the study, a qualitative approach was used to categorize content of the texts in statements and questionnaires. Quantitative methods were then used in the second step. Data were analysed with descriptive statistics and differences between groups were tested with Chi‐squared test. Bivariate odd ratios and confidence intervals were calculated. We chose a value of P < 0·05 and 95% CI as statistically significant. Statistical analyses were performed using IBM Statistical Package for the Social Sciences (SPSS) version 22.0.
Ethics
Filed cases at the PAC are covered by confidentiality. The results of the study are reported only on a group level and individuals cannot be identified. The regional ethical vetting board in Stockholm approved the study (Dnr: 2012/956‐31/5).
Results
The study included 618 complaints at different clinics from either a patient (67%) or a relative (33%). Most complained by phone (71·5%) and the remaining by letter or e‐mail. Most complaints concerned patients aged 20‐79 (80%). Patients under the age of 20 or over the age of 80 were represented in roughly equal proportions. A greater proportion of complaints concerned female patients (57%) than male patients and more women than men lodged complaints regarding themselves (60% vs. 40%). The most frequent category of relatives who lodged complaints were mothers (30%) followed by daughters and wives. The share of complaints at different clinics agrees well with the share of patient visits at each hospital clinic while primary care had a smaller proportion. In some cases, there were lodged complaints about more than one clinic, for example, both primary care and a hospital clinic.
The reasons for complaints were categorized into three groups: (1) complaints concerning healthcare/medical treatment 365 (59·1%); (2) complaints concerning organization/rules 227 (36·7%); and (3) complaints concerning attitudes/communication 214 (34·6%). More than one category may have been used. Women represented a larger proportion of those who left complaints concerning healthcare/medical treatment (60%) and attitudes/communication (58%) while the proportion of women and men were equal in the category of organization/rules. In 26% of the cases, the complainants had received information about the patient insurance and in 11·5% of the cases about the possibility to complain to National Board of Health and Welfare.
The content in the statements from the healthcare providers was categorized. One statement could relate to several categories. Associations between categories and the complainants’ satisfaction as reported in the questionnaire (being dissatisfied or being satisfied) were assessed. In all, 221 complainants responded to the questionnaire. Of those, 72% were dissatisfied and 28% were satisfied. More women (64%) than men were satisfied with the healthcare providers’ statement. More relatives (61%) than patients who had lodged complaints about themselves were satisfied.
Four of thirteen categories were associated with being dissatisfied. These were: ‘Disagree/defend themselves’, ‘Only an explanation of normal routine’, ‘Clinics refer to/blame each other’ and ‘Brief statement’. When the statement included that the healthcare provider ‘Disagreed/defended themselves’, the association with being dissatisfied was statistically significant and the odds ratios almost three times higher for being dissatisfied (OR = 2·83, P = 0·023). When the statement did not include any of these four categories a statistically significant association with being satisfied was found and the odds ratio was lower than 1, which means that this constitutes a factor against being dissatisfied (OR = 0·36, P = 0·001) (Table 1).
Table 1.
Associations between categories in statements from caregivers (more than one category may have been mentioned) and reports of dissatisfaction/satisfaction presented as percentages, OR with 95% CI and P values
| Proportion of satisfied (n = 61) | Proportion of dissatisfied (n = 160) | OR | 95% CI | P value | |
|---|---|---|---|---|---|
| Categories, most frequently reported by the dissatisfied | |||||
| Disagree/defend themselves | 10% | 24% | 2·83 | 1·13−7·09 | 0·023* |
| Only a description of adherence to standard routines | 23% | 34% | 1·70 | 0·86−3·35 | 0·14 |
| Involved clinics refer to(blame) each other | 2% | 6% | 3·97 | 0·50−31·72 | 0·30 |
| Brief statement | 7% | 10% | 1·57 | 0·50−4·91 | 0·60 |
| Combinations of above four categories | |||||
| None of the above mentioned | 64% | 39% | 0·36 | 0·20−0·67 | 0·001** |
| One of the above mentioned | 31% | 48% | 2·08 | 1·11−3·88 | 0·02* |
| Two or more of the above mentioned | 5% | 12% | 2·74 | 0·79−9·60 | 0·14 |
| Categories, most frequently reported by the satisfied | |||||
| Admit to have made mistakes but claims that this didn't affect the outcome. | 26% | 15% | 0·49 | 0·24−1·01 | 0·08 |
| Refer to internal problems (organizational) | 21% | 14% | 0·58 | 0·27−1·25 | 0·22 |
| Will review the incident and explains how for example routines will be modified | 16% | 10% | 0·56 | 0·24−1·32 | 0·24 |
| Regret | 69% | 62% | 0·72 | 0·39−1·35 | 0·35 |
| Combinations of above four categories | |||||
| None of the above mentioned | 20% | 32% | 1·90 | 0·93−3·86 | 0·10 |
| One of the above mentioned | 38% | 42% | 1·18 | 0·64−2·16 | 0·65 |
| Two or more of the above mentioned | 43% | 27% | 0·49 | 0·27−0·91 | 0·03* |
*P < 0·05; **P < 0·01.
OR, odds ratio; CI, confidence intervals.
Another four categories were associated with being satisfied: ‘Acknowledging mistakes’, ‘Refers to internal problems’, ‘Shall review the incident and/or describe how a routine will be changed’ and ‘Regrets’. When statements combined two or more of these categories, the association with being satisfied was statistically significant with an odds ratio that indicate that these combinations of two or more categories constitutes a factor against being dissatisfied (OR = 0·49, P = 0·03) (Table 1).
After receiving a statement from healthcare providers, the complainants responded to a questionnaire (Appendix 4). As previously mentioned, 72% (n = 160) reported that they were dissatisfied with the statements they had received from the healthcare providers. The two most frequent causes for reports of dissatisfaction were that the healthcare provider ‘did not tell the truth’ and ‘insufficient information’ (26% respectively). As reasons for dissatisfaction, 17% reported: ‘Not being listened to/not being taken seriously’, 16% reported ‘medical questions unanswered’ and 14% reported ‘Insufficient care’.
Discussion
The most challenging result in this study was that less than 30% of the complainants were satisfied with the healthcare providers’ statements about the complaints. On the basis of the present results, it can be assumed that Swedish PACs do not fully succeed in their two main assignments, which are to help and support patients and to contribute to quality improvement in health care.
The results show that the most common area for complaints concerned health care/treatment followed by complaints about attitude/communication and organization/rules. These results correspond with results from a recent systematic review of 59 international studies (n = 88,000 patients) (Reader et al. 2014). To identify problems concerning patient safety, the authors proposed a coding taxonomy with subcategories at three different levels. They claimed that ‘rigorous analysis of patients′ complaints’ (Reader et al. 2014, p. 678) are essential for identifying problems in patient security.
This study identified four categories of statements that were associated with dissatisfaction. These categories (‘Disagree/defend themselves’; ‘Only an explanation of normal routine’; ‘Clinics refer to/blame each other’ and ‘Brief statement’) are related to failings that mainly concern institutional and professional standards, in other words, to ‘procedure neglect’ (Reader & Gillespie 2013). However, the respondents’ perceptions for not being satisfied (‘did not tell the truth’, ‘insufficient information’; ‘not being listened to/not been taken seriously’, ‘unanswered medical questions’ and ‘insufficient care’) also reflect that procedure neglect is closely related to ‘caring neglect’. Caring neglect refers to ‘failings in care that are below the threshold of being proceduralized//yet lead patients, family and the public to believe that staff are unconcerned about the emotional and physical wellbeing of patients’ (Reader & Gillespie 2013) (p. 8 of 15). This implies that instead of providing alleviation, support, security or participation care causes confusion, frustration and abandonment (Arman et al. 2004, Nordgren et al. 2007). Suffering from care means that patient's dignity and human value is violated by activities or actions that involve neglect or exercise of power (Eriksson et al. 2006). Thus, strength of the present result is that it highlights the relation between procedure neglect and caring neglect. This underscores the importance of how healthcare providers receive and respond to complaints.
Insufficient statements from healthcare providers can have several explanations. To receive a complaint is often distressing and the criticism can fill the person, the healthcare provider, with strong emotions (Robinson et al. 2014). Previously, it has been described that a majority of physicians who receive a patient complaint react negatively, which can make it more difficult to admit mistakes (Cunningham 2004). Another reason for insufficient statements may be that Swedish healthcare providers are not fully aware of the PACs’ role for handling patient complaints. Statements are often characterized by denial or defence, which can be interpreted as the healthcare providers perceiving the PAC as an authority that can punish in the form of warnings against the clinic or against individual staff members. Moreover, health care has been described as a culture where infallibility prevails (Ödegård & Wallgren 2007), which can be a reason for strong reactions. A culture that strives for infallibility can affect the degree of honestly reported adverse events or managers’ active involvement (Ödegård & Wallgren 2007). Thus, by striving for infallibility, there is a risk that failures are denied or that patients who turn to the PAC risk being dismissed and this can be assumed to reduce patient confidence in health care (Ödegård & Wallgren 2007). Consequently, healthcare organizations need leadership that ensures both that staff receive support and that complaints are received and handled in a constructive way that lead to quality improvement (Robinson et al. 2014, Piper & Tallman 2015). It is reasonable to assume that complainants have at least two goals with their complaints: to obtain redress and to prevent that other patients experience the same flaws in health care (Jangland et al. 2009, Piper & Tallman 2015). None of these objectives are met if healthcare providers respond only in terms of disagreement, defence, explaining normal routines or referring to other clinics. It can also be assumed that a complaint will lose its meaning if it does not result in, for example, a change in routines. In turn, this means that the PACs’ assignments to help the patient and to reinforce patient safety will not be fulfilled. Finally, one reason for insufficient statements can be a lack of organizational structures for handling complaints from patients. At an organizational level, there is a need for a systematic analysis of the causes of complaints and what institutions and/or members of staff they are directed to (Bismark et al. 2013, Reader & Gillespie 2013). The aim was to find appropriate support and training. At clinic/unit level, it is necessary to ensure a leadership providing an ethical culture for receiving complaints and criticism with patients′ best in focus (Piper & Tallman 2015).
It is also important to acknowledge that patients who decide to lodge a complaint are filled by strong emotions. They may feel disappointment, grief, humiliation, anger, bitterness and sometimes even hatred (Kent 2008), which can contribute to distrustfulness. A patient who lodges a complaint can perceive that the healthcare providers protect each other instead of objectively investigating the event (Kent 2008). Thus, the complainant can perceive that he or she is at risk of being refused care by healthcare providers who suppose that the patient mistrusts the healthcare provider. Nurses have unique opportunities to listen and respond to patients’ experiences of health care and suffering. However, they need awareness about how patients conceive care. This can be organized at their work‐place in, for example, supervised reflective ethical seminars or group sessions (Berglund et al. 2012). In addition, systematic training of communication skills is valuable (Allan et al. 2015). Also, to ensure good quality of care and patient satisfaction, evaluation of nurses’ tasks regarding information, clinical pathways or guidelines and other routines can be conducted (Nilsson et al. 2015).
The present result identified four categories associated with being satisfied. When two or more of these categories were combined, or if none of the four identified categories were used, the associations were statistically significant. This may be explained in different ways. First, it can be assumed that complainants are more satisfied if they receive detailed statements. Thus, it is not receiving a statement that matters most; instead, it is a matter of what the statement contains. It has previously been described that complainants need to receive a personal explanation or apology from the involved healthcare providers (Skar & Soderberg 2012, Soderberg et al. 2012).
Second, when the statements contained information about what actions it actually led to (i.e. the category ‘Shall review the incident and/or describe how a routine will be changed’), there were associations with being satisfied. It can also be assumed that the complainant perceives that the healthcare provider has taken the complaint seriously, when expressed regret is a part of the statement although receiving solely an expression of regret not is enough. Stating that the clinic admits problems in their organizations may also be one way of showing that one is taking the complaint seriously in contrast to defending themselves. Thus, relatively simple measures can show the complainant, that the healthcare provider has considered the complainants’ physical and/or emotional wellbeing and is interested in helping the complainant (Eriksson & Svedlund 2007). In that way, complaints will result in a meaningful change for them (Robinson et al. 2014). Also from a patient safety perspective, this is an important issue. By recognizing mistakes and internal problems, the healthcare provider demonstrates that activities are critically examined and that they are prepared to change routines.
Limitations
The limitations of this study are the subjective nature of data and that the complaints filed at the PAC represent only a small share of the true number of dissatisfied patients and relatives. Furthermore, the data were collected from one single PAC, which might limit the ability to make generalizations. Another limitation is the questionnaire, since it only contained questions about whether the complainants were satisfied or not with the healthcare providers’ statements and the reasons for that. In future research, it would be interesting to ask also what has been helpful or not in the PAC's handling.
Conclusions
The results of this study provide novel insights about patients’ complaints that can contribute to a scientific knowledge base and can be applied to facilitate quality improvements in clinical practice. The present results can be used in, for example, nursing education when teaching nursing ethics or for reflection and discussion among nurses in clinical practice. Procedure neglect, untrue explanations, lack of communication, blaming other clinics etcetera indicate that healthcare providers at times neither take their caring responsibility nor their obligation to learn from mistakes/incidents. Mistakes are inevitable, but healthcare providers need to learn a lesson from them, they need to listen and they need to respond in a helpful manner. To improve patient safety and contribute to quality improvement healthcare organizations should insure a leadership providing an ethical culture for receiving complaints and strive for transparency regarding complaints.
Conflict of interest
The authors declare no conflicts of interests.
Author contributions
Charlotta Skålen (CS) and Eva‐Maria Annerbäck (EMA) conceptualized/designed the study and collected/analysed data. CS, Lena Nordgren and EMA drafted the manuscript, and revised it for important intellectual content.
All authors have agreed on the final version and meet at least one of the following criteria [recommended by the ICMJE (http://www.icmje.org/recommendations/)]:
substantial contributions to conception and design, acquisition of data or analysis and interpretation of data;
drafting the article or revising it critically for important intellectual content.
Appendix 1.
Questionnaire
TO YOU, WHO HAVE SUBMITTED COMPLAINTS TO THE PATIENT ADVISORY COMMITTEE:
In response to your communication to the patient advisory committee an investigation has been done. We have received responses from ….. … which are attached. We would be grateful if you answer the questions below and also leave comments with your answers. Please return the questionnaire in the enclosed envelope within 4 weeks, so that we can conclude your case.
| 1. Did you receive answers to your questions or comments? | |
| YES NO | |
| 2. If no, what do you miss the answer? | |
| 3. Do you feel satisfied with the answer? | |
| YES NO | |
| Write down any other comments here or use the back. | |
Appendix 2.
Reading guide for complaints Nr:
Appendix 3.
Nr: Reading guide for statements from healthcare providers
Brief statement
Regrets
Complain about treatment but receives a medical explanation
Will review the incident and describes for example how a routine will be changed
“Difficult patients”
Clinics refer to one another
Refers to internal problems (organizational)
Only an account of the normal routine and that it was followed
Encourages continued contact
Informs that the complaint constitutes a deviation
Other _______________________________________
Disagree with/defend themselves
Acknowledging mistakes but says that it has not affected the final result
Appendix 4.
Nr: Reading guide for questionnaire responses
Not satisfied
Missing someone who takes responsibility for the incident
The absence of financial compensation
Unnecessary expenditures
Medical questions unanswered
Not listened to/not taken seriously
Disagree with about the disease/diagnosis
Waiting time/not adequately treated in a timely manner
Don′t tell the truth
Administrative misses/messy organization
Freedom of choice and health care guarantee
Lack of care
Insufficient information
Other _______________________________________
References
- Allan H.T., Odelius A.C., Hunter B.J., Bryan K., Knibb W., Shawe J. & Gallagher A. (2015) Supporting staff to respond effectively to informal complaints: findings from an action research study. Journal of Clinical Nursing 24, 2106–2114. [DOI] [PubMed] [Google Scholar]
- Arman M., Rehnsfeldt A., Lindholm L., Hamrin E. & Eriksson K. (2004) Suffering related to health care: a study of breast cancer patients’ experiences. International Journal of Nursing Practice 10, 248–256. [DOI] [PubMed] [Google Scholar]
- Berglund M., Sjogren R. & Ekebergh M. (2012) Reflect and learn together ‐ when two supervisors interact in the learning support process of nurse education. Journal of Nursing Management 20, 152–158. [DOI] [PubMed] [Google Scholar]
- Bismark M.M., Spittal M.J., Gurrin L.C., Ward M. & Studdert D.M. (2013) Identification of doctors at risk of recurrent complaints: a national study of healthcare complaints in Australia. BMJ Quality and Safety 22, 532–540. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Cunningham W. (2004) The immediate and long‐term impact on New Zealand doctors who receive patient complaints. New Zealand Medical Journal 117, U972. [PubMed] [Google Scholar]
- Eriksson K. (2002) Caring science in a new key. Nursing Science Quarterly 15, 61–65. [DOI] [PubMed] [Google Scholar]
- Eriksson K., Peterson C.I., Zetterlund J.E., Olsson K.A. & Peterson C.I. (2006) The Suffering Human Being. Nordic Studies Press, Chicago, IL. [Google Scholar]
- Eriksson U. & Svedlund M. (2007) Struggling for confirmation–patients’ experiences of dissatisfaction with hospital care. Journal of Clinical Nursing 16, 438–446. [DOI] [PubMed] [Google Scholar]
- Hagelin I. (2007) Påverkas hälso‐ och sjukvården av vad patienterna för fram till patientnämnden Skåne? [Is health and healthcare affected by what patients say to the Patients’ Advisory Committee in Skåne?] Förvaltningshögskolan, Göteborg. In Swedish. [Google Scholar]
- Jain A. & Ogden J. (1999) General practitioners’ experiences of patients’ complaints: qualitative study. BMJ 318, 1596–1599. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Jangland E., Gunningberg L. & Carlsson M. (2009) Patients’ and relatives’ complaints about encounters and communication in health care: evidence for quality improvement. Patient Education and Counseling 75, 199–204. [DOI] [PubMed] [Google Scholar]
- Jangland E., Larsson J. & Gunningberg L. (2011) Surgical nurses’ different understandings of their interactions with patients: a phenomenographic study. Scandinavian Journal of Caring Sciences 25, 533–541. [DOI] [PubMed] [Google Scholar]
- Kent A. (2008) Dismissing the disgruntled: Swedish patient complaints management. International Journal of Health Care Quality Assurance 21, 487–494. [DOI] [PubMed] [Google Scholar]
- Nilsson A., Skar L. & Soderberg S. (2015) Nurses’ views of shortcomings in patent care encounters in one hospital in Sweden. Journal of Clinical Nursing 24, 2807–2814. [DOI] [PubMed] [Google Scholar]
- Nordgren L., Asp M. & Fagerberg I. (2007) An exploration of the phenomenon of formal care from the perspective of middle‐aged heart failure patients. European Journal of Cardiovascular Nursing 6, 121–129. [DOI] [PubMed] [Google Scholar]
- Ödegård S. & Wallgren G. A. 2007. I rättvisans namn: ansvar, skuld och säkerhet i vården [In the Name of Fairness: Responsibility, Guilt and Safety in Healthcare.] Liber, Stockholm. In Swedish. [Google Scholar]
- Piper L.E. & Tallman E. (2015) The ethical leadership challenge for effective resolution of patient and family complaints and grievances: proven methods and models. Health Care Manager (Frederick) 34, 62–68. [DOI] [PubMed] [Google Scholar]
- Reader T.W. & Gillespie A. (2013) Patient neglect in healthcare institutions: a systematic review and conceptual model. BMC Health Services Research 13, 156. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Reader T.W., Gillespie A. & Roberts J. (2014) Patient complaints in healthcare systems: a systematic review and coding taxonomy. BMJ Quality and Safety 23, 678–689. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Robinson L., Cotton J., Sarkar S. & Thompson P.J. (2014) A 36‐month study of patient complaints at a tertiary fertility centre. Human Fertility (Cambridge, England) 17, 45–49. [DOI] [PubMed] [Google Scholar]
- Skar L. & Soderberg S. (2012) Complaints with encounters in healthcare – men's experiences. Scandinavian Journal of Caring Sciences 26, 279–286. [DOI] [PubMed] [Google Scholar]
- Soderberg S., Olsson M. & Skar L. (2012) A hidden kind of suffering: female patient's complaints to Patient's Advisory Committee. Scandinavian Journal of Caring Sciences 26, 144–150. [DOI] [PubMed] [Google Scholar]
- The Patient Act (2014:821) Retrieved from http://www.riksdagen.se/sv/Dokument-Lagar/Lagar/Svenskforfattningssamling/sfs_sfs-2014-821/ on 18 January 2016. In Swedish.
- Wessel M., Lynoe N., Juth N. & Helgesson G. (2012) The tip of an iceberg? A cross‐sectional study of the general public's experiences of reporting healthcare complaints in Stockholm, Sweden. BMJ Open 2, e000489. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Wessel M., Helgesson G., Olsson D., Juth N., Alexanderson K. & Lynoe N. (2013) When do patients feel wronged? Empirical study of sick‐listed patients’ experiences with healthcare encounters. European Journal of Public Health 23, 230–235. [DOI] [PubMed] [Google Scholar]
- Wofford M.M., Wofford J.L., Bothra J. & Kendrick S.B. (2004) Patient complaints about physician behaviors: a qualitative study. Academic Medicine 79, 134. [DOI] [PubMed] [Google Scholar]