Abstract
There is an increase in population of elderly above the age of 65. As age advances, more diseases develop resulting in use of more medications. Physiological changes, alterations in homeostatic regulation and diseases modify pharmacokinetics and drug response in older patients. The risk for drug interactions and drug-related problems increases along with multiple medications. Periodic evaluation of the patients’ drug regimen is essential to minimize polytherapy. Clinicians must be alert to the use of herbal and dietary supplements as they are prone to drug-drug interactions. This article focuses on the possible pharmacokinetic, pharmacodynamic, and herbal drug interactions occurring in the elderly.
Keywords: Drug interactions, pharmacodynamics, pharmacokinetics, polytherapy
INTRODUCTION
There is an increase in the total population worldwide, and a sizable number of this population is of elderly above the age of 65. India with people aged 60 years and above is going to be the highest in Asia. The population study has shown that population of this + 65 aged people in Sweden was 17.4%, Australia was 12.1%, China was 6.8%, and India was 7% in the year 2000, and the predictive value for 2030 will be 25%, 20%, 15.7%, and 9.6%, respectively.[1] As people age, they develop multiple symptoms and illnesses. In addition to chronic diseases of adulthood, they have an increased incidence of many conditions including Alzheimer's disease, Parkinson's disease, vascular dementia, stroke, arthritis, osteoporosis, and fractures. Hence, polytherapy is often mandatory in the management of the common ailments. The term polytherapy refers to the use of multiple medications, ranging from 5 to 10.[2] Nowadays, it has been used to describe the use of inappropriate medications/more medications than clinically indicated, and the prevalence of inappropriate medication use in the elderly ranges from 11.5% to 62.5%.[3] Consequences of polypharmacy include adverse drug reactions and interactions, nonadherence, increased risk of cognitive impairment, impaired balance and falls, increased risk of morbidity, hospitalization, and mortality.[4,5,6]
POLYTHERAPY AND DRUG INTERACTIONS
Specific combination of various drugs in a given patient has the potential to result in an interaction.[7] As number of medications increase, the potential for drug interactions increases. The risk of an adverse drug event has been estimated at 13% for two drugs, 58% for five drugs, and 82% for seven or more drugs.[8] The overall incidence of drug reactions in geriatric patients is estimated to be at least twice that in the younger population because of errors both in prescription pattern of practitioners and drug usage by the patients.[9] Practitioner errors occur because of lack of knowledge of geriatric clinical pharmacology and not conducting medication review with the patient. Patient errors may result from noncompliance and use of multiple pharmacies. Poor compliance in geriatric patients is due to poor communication with health professionals and decline in cognitive abilities. Other predictors for drug interactions include severity of the diseases being treated, age of the patient, and renal and hepatic dysfunction. The increase in the drug counters with fixed dose combinations, self-medication, etc., further contributes to the increased incidence of drug interactions.
MECHANISM OF DRUG INTERACTIONS
The action and interaction of drugs are dependent on their “pharmacokinetics” (PK) and “pharmacodynamics.”[10] Physiological changes, alterations in homeostatic regulation, and diseases modify PK and drug response in older patients. Hence, many medications need to be used with special caution. Most drug interactions are pharmacokinetic and can be classified as alterations in absorption, distribution, and protein-binding effects, changes in drug metabolism, or alterations in elimination.
Absorption
It is delayed due to reduced blood flow to gut, alteration in gastric pH, reduced motility, and formation of complexes.
Gastric pH
An alteration in gastric pH due to antacids, H2 antagonists, and proton pump inhibitors affects the absorption of other drugs. Drugs such as ketoconazole, itraconazole, and salicylates require gastric acidity for their optimum absorption. If both these are given concurrently, the bioavailability of the latter is reduced. This potential interaction can be reduced by giving a gap of 2–3 h between antacid and potentially interacting drug.
Gastric motility
Prolonged gastric emptying may delay absorption of some drugs in elderly. Anticholinergic drugs used in the control of movement disorders delay gastric emptying. They reduce bioavailability of levodopa by 50%.[11]
Complex formation
Drugs interfering with metals such as Al, Mg, Ca, and Fe form complexes resulting in the reduced absorption. Bisphosphonates are often co-prescribed with calcium supplements in the treatment of osteoporosis. Calcium binds to the bisphophonates and reduces its absorption with a possibility of therapeutic failure.[12] This may be avoided by allowing sufficiently long dosage interval; possible approach is to give bisphophonates for 2 weeks and calcium supplements for 10 weeks.[11]
Distribution
The distribution of drugs in elderly is altered due to reduction in lean body mass, total body water content, increase in the percentage of body fat, and decrease in serum albumin.
Body composition
as age increases, muscle mass and body water may decrease with an increase in body fat. Hence, the volume of distribution (Vd) of fat-soluble drugs (e.g., diazepam) may be increased thereby delaying maximal effects or leading to accumulation with continued use. Conversely, Vd of water-soluble drugs (e.g., lithium and digoxin) decreases. Hence, the loading doses must be decreased.
Protein binding
Plasma albumin may be reduced with age resulting in increase in the free form of acidic drugs and consequent risk. Drugs competing for binding sites on albumin such as warfarin, phenytoin, and tolbutamide may exaggerate the displacement of one drug by another, with potential toxic effects of the unbound form of the displaced drug, for example, warfarin causes bleeding and glipizide causes hypoglycemia. In contrast, the concentration of α1 acid glycoprotein may be increased resulting in decrease in the free form of basic drugs such as antidepressants, antipsychotics, and β blockers.
Metabolism
Hepatic parenchymal mass and blood flow decrease by about 30% in old age,[11] together with changes in enzyme activity. Changes in drug metabolism represent the largest number and best-known types of drug interactions.[13] The most frequent change involves the microsomal mixed function in oxidative system but little or no change occurs in the conjugative processes. Cytochrome p450 isoenzymes are important for oxidative metabolism in liver; those most commonly involved in drug metabolism are 3A4, 2D6, and 1A2. A good understanding of substrates, inhibitors, and inducers can help predict the risk for drug interaction in certain drug combinations.
Enzyme induction
Induction of the enzymes results in reduced plasma concentration of the substrate agent due to its increased metabolism. Phenytoin, an enzyme inducer, when combined with simvastatin causes a reduced response. Increase in cholesterol level from 9.4 mmol/L to 15.9 mmol/L can be observed.[11] Similarly, when omeprazole is combined with warfarin/imipramine, their metabolism is enhanced resulting in a reduced response.
Enzyme inhibition
It is usually caused by competitive binding at an enzyme's binding site. Cisapride is a prokinetic drug given to treat gastroparesis, ileus, and gastroesophageal reflux disease. When it is combined with erythromycin, it blocks the metabolism of cisapride, increasing its plasma concentration. This results in prolongation of QT intervals[14] leading to torsade de pointes.
Excretion
Renal blood flow, glomerular filtration rate, and tubular secretion start decrease after 55 years. As renal function declines, the clearance of many drugs is reduced in elderly.[15] Toxicity may result with drugs which are mainly eliminated through kidneys and have narrow therapeutic index such as lithium, digoxin, and aminophylline.
Pharmacodynamic interactions
Physiologic changes and loss of homeostatic resilience change the pharmacodynamics of drugs in elderly. Many serious interactions occur as a result of decreased drug activity with diminished efficacy or increased drug activity with exaggerated or unusual effects. These include hemorrhage from anticoagulants even if dosage is appropriately adjusted, increased central nervous system depression at any given plasma concentration, and hypotension from psychotropic medications.[16] For example, aspirin when combined with warfarin increases the risk of bleeding and angiotensin-converting enzyme inhibitors combined with potassium-sparing diuretics increase the risk of hyperkalemia. The most important adverse interactions between drugs occur with drugs that have serious toxicity and a low therapeutic index.
DRUG–HERB INTERACTIONS
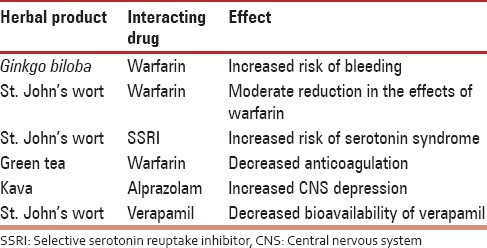
The elderly frequently use medicinal herbs and other dietary supplements and ignore to tell their health-care providers. Medicinal herbs can interact with drugs and lead to adverse effects. Table 1 outlines few examples of potential drug interactions with herbal products.
Table 1.
Drug interactions with herbal products
CONCLUSION
Polytherapy is often mandatory in the management of most of the common ailments affecting geriatric patients. Drug prescription in elderly is a serious challenge as there is an increased possibility of drug interaction resulting in toxicity, treatment failure, or loss of drug effect. Duplicative prescribing within the same drug class often occurs, and unrecognized drug side effects are treated with more drugs. To minimize polytherapy, periodic evaluation of patient's drug regimen is necessary. Prescribers need to know what other prescriptions patient is taking including herbs and teas. Drugs such as digoxin and theophylline with a narrow therapeutic index should be carefully evaluated for potential interactions. Small number of drugs in low doses with simple regimen is good for drug therapy in elderly.
Financial support and sponsorship
Nil.
Conflicts of interest
There are no conflicts of interest.
REFERENCES
- 1.New Delhi: Registrar General, India; 1996. Population Projections for India and States – 1996-2016. Census of India 1991 (Report) [Google Scholar]
- 2.Ferner RE, Aronson JK. Communicating information about drug safety. BMJ. 2006;333:143–5. doi: 10.1136/bmj.333.7559.143. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Guaraldo L, Cano FG, Damasceno GS, Rozenfeld S. Inappropriate medication use among the elderly: A systematic review of administrative databases. BMC Geriatr. 2011;11:79. doi: 10.1186/1471-2318-11-79. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Salazar JA, Poon I, Nair M. Clinical consequences of polypharmacy in elderly: Expect the unexpected, think the unthinkable. Expert Opin Drug Saf. 2007;6:695–704. doi: 10.1517/14740338.6.6.695. [DOI] [PubMed] [Google Scholar]
- 5.Shah BM, Hajjar ER. Polypharmacy, adverse drug reactions, and geriatric syndromes. Clin Geriatr Med. 2012;28:173–86. doi: 10.1016/j.cger.2012.01.002. [DOI] [PubMed] [Google Scholar]
- 6.Huang AR, Mallet L, Rochefort CM, Eguale T, Buckeridge DL, Tamblyn R. Medication-related falls in the elderly: Causative factors and preventive strategies. Drugs Aging. 2012;29:359–76. doi: 10.2165/11599460-000000000-00000. [DOI] [PubMed] [Google Scholar]
- 7.Montamat SC, Cusack BJ, Vestal RE. Management of drug therapy in the elderly. N Engl J Med. 1989;321:303–9. doi: 10.1056/NEJM198908033210507. [DOI] [PubMed] [Google Scholar]
- 8.Fulton MM, Allen ER. Polypharmacy in the elderly: A literature review. J Am Acad Nurse Pract. 2005;17:123–32. doi: 10.1111/j.1041-2972.2005.0020.x. [DOI] [PubMed] [Google Scholar]
- 9.Katzung BG. Basic and Clinical Pharmacology. 11th ed. New Delhi: McGraw-Hill Medical; 2009. [Google Scholar]
- 10.Robyn AS. Durg interaction. In: Charles FC, Keith FW, Hans Lee, editors. The Washington Manual of Medical Therapeutics. 29th ed. Philadelphia, New York: Lippincott, Raven; 1998. [Google Scholar]
- 11.Van Boxtel CJ, Santoso B, Ralph Edwards I. Revised 2nd Edition. The Netherlands: IOS Press; 2008. Drug Benefits and Risks. International Text Book of Clinical Pharmacology. [Google Scholar]
- 12.Solomon CG. Bisphosphonates and osteoporosis. N Engl J Med. 2002;346:642. doi: 10.1056/NEJM200202283460902. [DOI] [PubMed] [Google Scholar]
- 13.Michalets EL. Update: Clinically significant cytochrome P-450 drug interactions. Pharmacotherapy. 1998;18:84–112. [PubMed] [Google Scholar]
- 14.Wysowski DK, Bacsanyi J. Cisapride and fatal arrhythmia. N Engl J Med. 1996;335:290–1. doi: 10.1056/NEJM199607253350416. [DOI] [PubMed] [Google Scholar]
- 15.Salzman C. Clinical Geriatric Psychopharmacology. 2nd ed. Baltimore: Williams and Wilkins; 1992. [Google Scholar]
- 16.Meyer UA. Drugs in special patient groups. In: Melmon KL, Morrelli H, Hoffman BB, editors. Clinical Pharmacology, Basic Principles in Therapeutics. 3rd ed. New York: McGraw Hill; 1992. [Google Scholar]


