Abstract
Uterine fibroids are the most common uterine neoplasm of uterus and the female pelvis and the most common indication for hysterectomy worldwide. When the fibroid is large and fills the whole pelvis or is pedunculated, it becomes difficult to differentiate from ovarian mass clinically. Cervical fibroids pose enormous surgical difficulty by virtue of their relative inaccessibility and proximity to the anterior bladder, posterior rectum, and distorting the normal anatomical relationship of pelvic structures. A cervical fibroid especially with degenerative changes mimics an ovarian tumor and poses a clinical dilemma. This case is also exemplified for its rarity and diagnostic difficulty.
Keywords: Cervical fibroid, degenerating fibroid, gynecologic surgery
INTRODUCTION
Uterine fibroids are the most common uterine neoplasm of uterus and the female pelvis and the most common indication for hysterectomy as well.[1] When the tumor fills the whole pelvis or is pedunculated, there is always an uncertainty regarding the uterine or ovarian origin of the tumor. A cervical fibroid especially with degenerative changes mimics an ovarian tumor and causes a clinical dilemma.[2] This case is also exemplified for its rarity and diagnostic difficulty.
CASE REPORT
A 40-year-old woman, P 2 living 2, presented in the Department of Gynaecology with the complaint of progressively increasing distension in abdomen for last 1 year. It was associated with pain lower abdomen for last 6 months. Surprisingly, there were no complaints regarding change of menstrual pattern, urinary or bowel habits, anorexia or fever.
On examination, a huge abdominal mass occupying whole of the hypogastrium, both iliac fossa, umbilicus, and left hypochondrium, was noted. The mass was 10 × 8 inches in size, smooth surfaced with regular margin, soft to firm in consistency, nontender, side to side mobile, lower limit not reachable, and engaged in the pelvis more toward the left side. There were no ascites clinically. On per vaginal examination, the same mass was felt obliterating all the fornices; uterus was easily palpable of normal size but dextro deviated.
Ultrasonography revealed a huge complex mass arising from the pelvis and extending into the abdomen occupying almost whole of the abdomen with well-defined margins; complex internal echotexture, predominantly echogenic with multiple poorly hypoechoic areas along with two cystic areas, each measuring around 4 cm × 5 cm in size. Doppler sonography showed minimal blood flow to the tumor. Both the ovaries could not be visualized. A normal size uterus was seen pushed to the right side with normal central endometrium. Free intraperitoneal fluid or lymphadenopathy was absent. CA 125 was 5.2 IU. Computed tomography scan was not done due to financial reasons.
Clinically provisional diagnosis of the benign ovarian tumor was made based on Doppler and biomarker CA 125 levels. After preanesthetic work up, the patient was taken up for laparotomy. Per operatively soft mass of size 12 × 10 inches with intact external capsule was seen, growing into the leaves of left broad ligament and extending above the umbilicus. Both ovaries, right tube and uterus was normal but left fallopian tube was stretched over the mass. On opening the broad ligament leaf, it was found to be arising from posterior surface of upper part of cervix. Left ureter was catheterized to avoid injury. Mass was shelled out followed by total hysterectomy with left-sided salpingo-oophorectomy [Figure 1]. There were no pressure changes in ureter or bowel. Omentum and rest of the abdominal organs were normal. Cut section showed few solid areas along with multiple cystic areas, one containing black tarry material suggestive of red degeneration. Postoperative period was uneventful.
Figure 1.
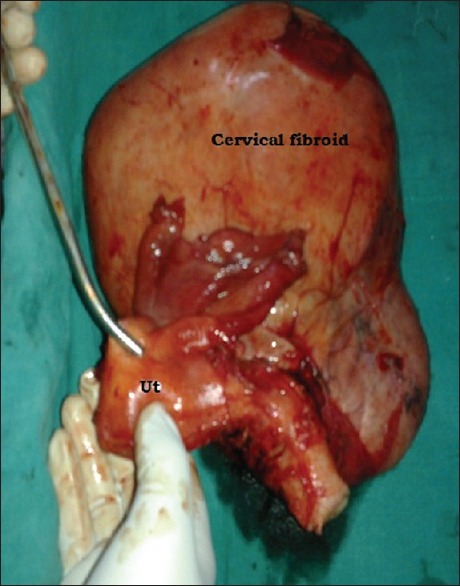
Surgical specimen showing normal uterus with huge cervical fibroid
Histopathology of the mass revealed benign spindle cell tumor (leiomyoma uteri) with red, cystic, myxoid and hyaline degenerations and dystrophic calcification [Figure 2]. The definitive diagnosis came out to be cervical fibroid with marked degenerative changes.
Figure 2.
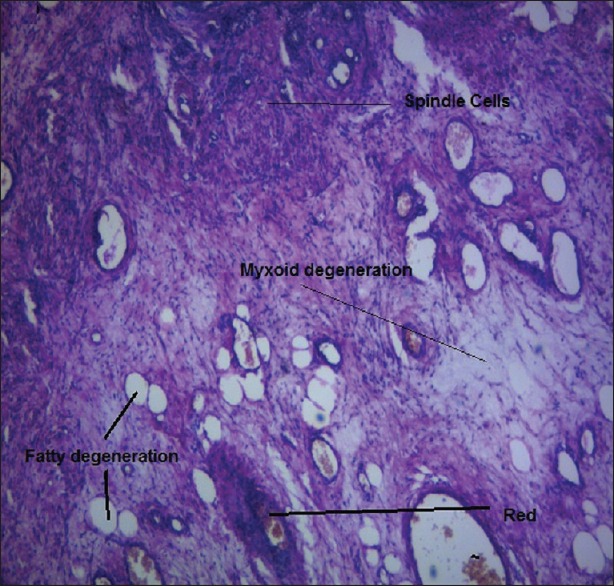
Histology: Spindle cells tumor (leiomyoma) with cystic, fatty, myxoid, and red degenerations
DISCUSSION
Fibroids extending into broad ligament are rare and may mimic an ovarian tumor.[3] It is known that degenerative changes result in unusual appearance that adds to diagnostic confusion.[4] Pedunculated uterine, cervical, and true broad ligament fibroid, especially with degeneration, may be mistaken for lesion of ovarian origin and therefore must be kept in the differential diagnosis.[5] Cervical fibroids pose enormous surgical difficulty by virtue of their relative inaccessibility and proximity to bladder and uterus[6] and distorting the normal anatomical relationships. As in this case cervical fibroid presented as huge abdominal mass pushing the uterus upward and sideways. It bulges outward between the layers of broad ligament, displacing uterine artery outward and upward and ureter outward toward the pelvic side wall.[7]
Financial support and sponsorship
Nil.
Conflicts of interest
There are no conflicts of interest.
REFERENCES
- 1.Jones HW, Rock JA. Leiomyomata uteri and myomectomy. Te Linde's Operative Gynaecology. 10th ed. Philadelphia PA, USA: Lippincott Williams and Wilkins; 2008. pp. 687–96. [Google Scholar]
- 2.Basnet N, Banerjee B, Badani U, Tiwari A, Raina A, Pokharel H, et al. An unusual presentation of huge cervical fibroid. Kathmandu Univ Med J (KUMJ) 2005;3:173–4. [PubMed] [Google Scholar]
- 3.Yuel VI, Kaur V. Broad ligament fibroid – An unusual presentation. JK Sci. 2006;8:217–8. [Google Scholar]
- 4.Baltarowich OH, Kurtz AB, Pennell RG, Needleman L, Vilaro MM, Goldberg BB. Pitfalls in the sonographic diagnosis of uterine fibroids. AJR Am J Roentgenol. 1988;151:725–8. doi: 10.2214/ajr.151.4.725. [DOI] [PubMed] [Google Scholar]
- 5.Low SC, Chong CL. A case of cystic leiomyoma mimicking an ovarian malignancy. Ann Acad Med Singapore. 2004;33:371–4. [PubMed] [Google Scholar]
- 6.Kaur AP, Saini AS, Kaur D, Madhulika, Dhillon SP. Huge cervical fibroid:Anunusual presentation. J Obstets Gynaecol India. 2002;52:164–5. [Google Scholar]
- 7.Monaghan JM. Bonney's Gynecological Surgery. 10th ed. Hong Kong: Blackwell Science; 2004. Total hysterectomy for cervical and broad ligament fibroids; pp. 74–85. [Google Scholar]


