Abstract
Introduction:
Human immunodeficiency virus (HIV) infection gradually destroys the body's immune system, which makes it harder for the body to fight infections. HIV infection causes a quantitative and qualitative depletion of CD4 lymphocyte count, which increases the risk of opportunistic infections. Thus, CD4 count is one of the key factors in determining both the urgency of highly active antiretroviral therapy (HAART) initiation and the need of prophylaxis for opportunistic infections.
Aim:
This study aims to evaluate the prevalence and variations in the oral manifestations of HIV/acquired immune deficiency syndrome patients on HAART therapy in urban population and their association with CD4 count.
Materials and Methods:
A study was conducted by screening eighty patients who were HIV positive in an urban location. Both adult and pediatric patients were screened for oral manifestations and simultaneously CD4 count was also evaluated. Patients with HIV infection for variable time period who are under HAART were considered.
Statistical Analysis:
Measures of central tendency were used to analyse the data.
Results:
HIV infection destroys the immune system of an individual, making the patient susceptible to various infections and malignancies. With the advent of antiretroviral therapy, the scenario has changed drastically. We have observed that patients with CD4 counts between 164 and 1286 show relatively few oral manifestations. Long-term HAART therapy causes pigmentation, xerostomia and angular cheilitis but is taken up quite well by the patients.
Conclusion:
In this study, eighty patients with HAART from urban population showed very minimal oral findings because of good accessibility for treatment and awareness about HIV infections. The patients who were on long-standing HAART treatment also showed minimal oral manifestation such as pigmentation and xerostomia. Hence, we conclude that recognition, significance and treatment of these lesions in patients with HIV infection do not require elaborate setup and can be treated with basic primary health care.
Keywords: Antiretroviral therapy, CD4 lymphocytes, human immunodeficiency virus, oral manifestations of AIDS, pigmentation, xerostomia
INTRODUCTION
Acquired immune deficiency syndrome (AIDS) is caused by the human immunodeficiency virus (HIV) and is highly lethal.[1] India is the third largest country in the number of HIV-infected patients and according to the WHO, in 2012, an estimated 2.3 million individuals worldwide were newly infected with HIV.[2] It is a critical disorder of the immune system which severely damages the body's normal defense to infections, thereby making the host vulnerable to various infections and conditions including malignancies, which then become life-threatening.[1] With the advent of highly active antiretroviral therapy (HAART), people are living longer and are suffering fewer opportunistic infections. The primarily targeted cells in HIV are CD4 helper T lymphocytes.[1,2,3]
In people with HIV infection, antibodies are developed but are not protective. The virus may remain silent and causes CD4 cell death. This results in a subsequent decrease in T-helper cell number, with a resultant loss in immune function which hampers the body's ability to fight infections.[3]
The most common signs and symptoms seen with HIV/AIDS patients are generalized lymphadenopathy, sore throat, fever, dysphagia, night sweat, maculopapular rash, headache, myalgia, diarrhea and peripheral neuropathies. Oral changes include mucosal erythema, focal ulcerations,[4] candidiasis and hairy leukoplakia.
The most frequently associated oral lesions in HIV-infected children are candidiasis, herpes simplex infection, linear gingival erythema, parotid enlargement and recurrent aphthous stomatitis. Other viral and bacterial infections, including periodontal infections are less commonly associated, while hairy leukoplakia and Kaposi's sarcoma are rarely seen in HIV-infected children.[4,5,6]
HIV infection causes a quantitative and qualitative depletion of CD4 lymphocyte count, which increases the risk of opportunistic infections. It is one of the key factors in determining both the urgency of HAART initiation and the need for prophylaxis for opportunistic infections.[1,3]
Dental expertise is necessary for the proper management of oral complications in HIV infection or AIDS, but many patients do not receive adequate dental care.[7]
Medical clinicians should be able to recognize HIV-associated oral disease and provide appropriate care and referral. Factors that predispose to HIV-related oral conditions include CD4+ cell count of <200/μL.[1,7]
For individuals with unknown HIV status, oral manifestations may suggest possible HIV infection, although they are not diagnostic of infection. For persons living with HIV disease who are not yet on therapy, the presence of certain oral manifestations may signal progression of HIV disease.[1,2,7]
HIV-related oral abnormalities are present in 30%–80% of HIV-infected individuals and these abnormalities are often inaccurately described in medical literature. Treatment for oral conditions are also very low. Factors predictive of receiving oral care include education beyond a high school level, participation in clinical trials and utilization of support services such as medical social workers. The overall prevalence of oral manifestations of HIV disease has changed since the advent of potent antiretroviral therapy (ART).[5,6,7,8]
One study by Patton et al. noted a reduction of oral lesions from 47.6% prepotent ART to 37.5% during the potent ART era.[5] Overall, there appears to be a reduced incidence of candidiasis, Kaposi's sarcoma, oral hairy leukoplakia and necrotizing ulcerative periodontitis; an increased incidence of salivary gland disease, oral warts and dental caries in the form of “brittle teeth syndrome” and a relatively unchanged incidence of oral ulcers.[5,7,9]
MATERIALS AND METHODS
Source of data
In this study, a total of eighty patients belonging to an urban population suffering from HIV infection and on therapy for the same were considered. In a total of eighty patients, 67 were adults and 13 were pediatric. The patients were attached to the foundation of the hospital for their primary health care and regular checkup.
Ethical clearance
The study protocol was approved by the research committee at hospital and by institutional ethical committee. All information about the patients and their identity was anonymous. Subjects were given both verbal and written information about the nature of the study and written consent was obtained.
Method of collection of data
A cross-sectional study was conducted on eighty randomly chosen patients who were diagnosed as HIV positive and were on HAART therapy independent of age and sex. The patients who were in the window period and not on HAART therapy were excluded from the study. All the patients were examined for their oral manifestations, current CD4 counts and duration of the HAART therapy.
Statistical analysis
All the findings were tabulated and the results were analyzed using measures of central tendency. The subjects were grouped according to the status of CD4 count and duration of HAART received as follows:
The CD4 counts which were recorded were divided into under three ranges:
CD4 count <400
CD4 count between 400 and 800
CD4 count >800.
The duration of the HAART therapy was also divided into three ranges:
HAART therapy >4 years
HAART therapy between 4 and 8 years
HAART therapy <8 years.
All the ranges were expressed in percentages.
RESULTS
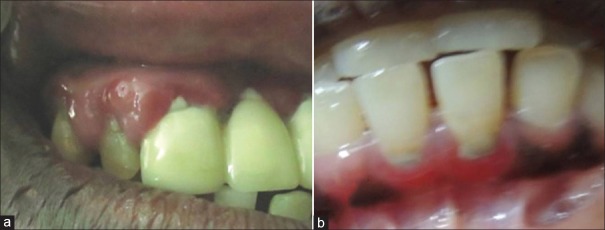
In this study, out of eighty patients, 67 were adult patients and 13 were pediatric patients. The clinical parameters such as age, sex, CD4 counts, duration of HAART therapy and oral manifestations of adult and pediatric patients were noted. Out of 67 adult patients, 21 (31.3%) were males and 46 (68.6%) were females; the mean age of adult patients was 37.25 years. The most common manifestations observed in adults were melanin pigmentation (32.8%) [Figure 1], gingivitis (7.4%) [Figure 2], xerostomia (4.4%), candidiasis (2.9%) and combinations of the same [Table 1]. The most common manifestations seen in pediatric patients were melanin pigmentation (30.7%) [Figure 3], angular cheilitis (23.0%) [Figure 4], gingivitis (7.6%), oral ulcerations (7.6%) and combinations of the same [Table 2].
Figure 1.
Clinical photograph revealing oral melanin pigmentation in adults patients. (a) Buccal mucosa. (b) Tongue
Figure 2.
Clinical photograph revealing gingivitis in adult patients. (a) Upper free and attached gingiva. (b) Lower free gingiva
Table 1.
Percentage distribution of oral manifestations in adult patients

Figure 3.
Clinical photograph revealing oral melanin pigmentation in pediatric patients. (a) Attached gingiva. (b) Buccal mucosa and tongue
Figure 4.

Clinical photograph revealing angular cheilitis at the right corner of the mouth
Table 2.
Percentage distribution of oral manifestations in pediatric patients

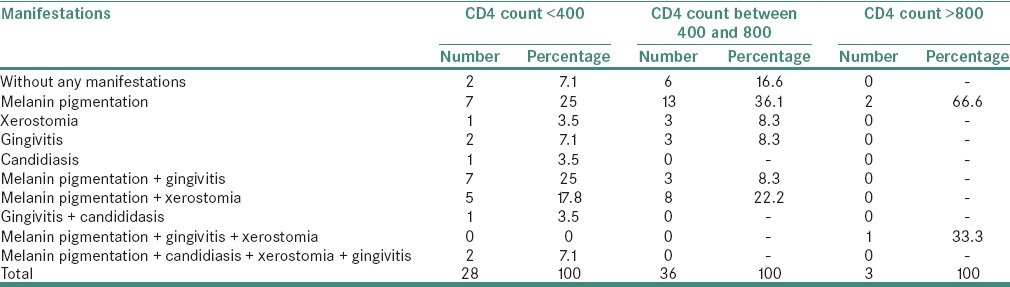
Correlation between different range of CD4 count and the variation of the oral manifestations in adult patients (n = 67) are tabulated in Table 3. In the patients with CD4 count <400, most common manifestation seen was melanin pigmentation (25%), least common was xerostomia and candidiasis (3.5%) and 7.1% of patients were without any manifestations. In the patients with the CD4 count ranging between 400 and 800, most common manifestation was again melanin pigmentation (36.1%), least common was xerostomia and candidiasis (8.3%) and 16.6% of patients were without any manifestations. In the patients with the CD4 count >800, most common manifestation was again the melanin pigmentation (66.6%) and other manifestations were hardly seen
Table 3.
Percentage distribution of oral manifestation in adult patients with different CD4 counts (n=67)
Correlation between the CD4 count and the variation of the oral manifestations in pediatric patients (n = 13) are presented in Table 4. In the patients with CD4 count <400, most common manifestation seen was melanin pigmentation (50%) and least common was gingivitis (25%). In the patients with the CD4 count ranging between 400 and 800, most common manifestation was angular cheilitis (50%) next was melanin pigmentation (33.3%) and 16.6% of patients were without any manifestation. In the patients with the CD4 count >800, most common manifestation was again the melanin pigmentation (66.6%) and the least was oral ulcerations (33.3%).
Table 4.
Percentage distribution of oral manifestation in pediatric patients with different CD4 count (n=13)
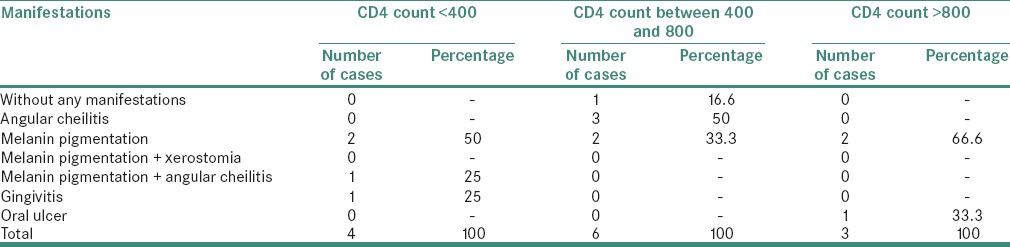
With the above compilation, we can infer that as the CD4 counts were increasing, the percentage of oral manifestations were reducing in both adult and pediatric patients and vice versa.
With this, we can assume that as the CD4 counts were increasing the pathological manifestations were decreasing, and the physiological manifestations were increasing, which is a positive sign for the patients. These CD4 counts were raised with the advent of HAART therapy. The adverse effect with the therapy was an increase in melanin pigmentation which is a physiological manifestation, but the opportunistic infections were reduced.[9,10]
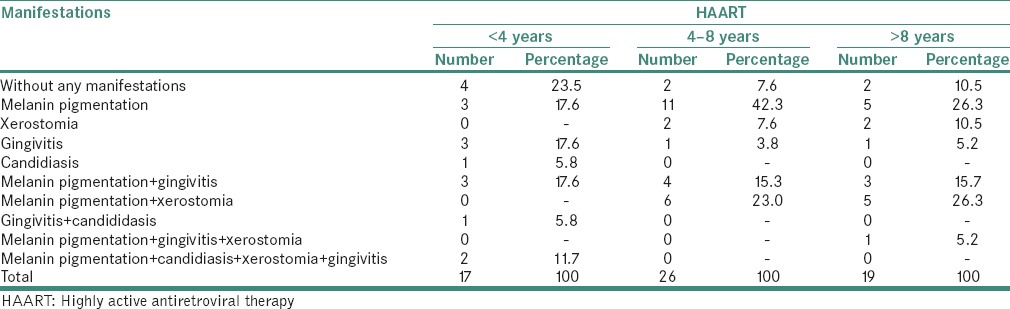
Correlation between the duration of HAART therapy and the oral manifestations in adult patients are tabulated in Table 5. In the patients with HAART <4 years duration, most common manifestation seen was melanin pigmentation and gingivitis (17.6%), least common was candidiasis (5.8%) and the patients who were without any manifestation were 23.5%. In the patients with HAART between 4 and 8 years duration, most common manifestation seen was melanin pigmentation (42.3%), least common was gingivitis (3.8%) and the patients who were without any manifestation were 7.6%. In the patients with HAART >8 years duration, most common manifestation seen was melanin pigmentation (26.3%) and melanin pigmentation along with xerostomia (26.3%), least common was gingivitis (5.2%) and the patients who were without any manifestation were 10.5%.
Table 5.
Percentage distribution of oral manifestations in adult patients with different duration of highly active antiretroviral therapy (n=67)
Correlation between the duration of HAART therapy and the oral manifestations in pediatric patients are presented in Table 6. In the patients with HAART <4 years duration, most common manifestation seen was angular cheilitis (50%), least common was gingivitis (25%) and the patients who were without any manifestation (25%). In the patients with HAART between 4 and 8 years duration, most common manifestation seen was melanin pigmentation (33.3%), least common was angular cheilitis (16.6%) and the patients who were without any manifestation were 16.6%. In the patients with HAART >8 years duration, the only manifestation which was seen was melanin pigmentation (100%).
Table 6.
Percentage distribution of oral manifestations in pediatric patients with different duration of highly active antiretroviral therapy (n=13)
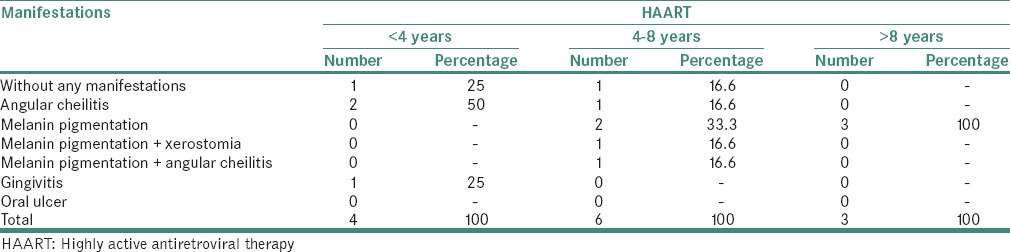
The comparison of the above tables also gives the similar results as that of the CD4 count results. As the duration of the HAART therapy was increasing, the pathological manifestations were decreasing and vice versa. This gives us a clear clue that the HAART therapy is effective against opportunistic infections.
DISCUSSION
AIDS is caused by a HIV, a retrovirus. AIDS is a critical disorder of the immune system which severely damages the body's normal defense system as it has specific affinity for CD4 cells on entry into the host's body. The HIV attacks and disturbs the delicate balance of host's immune response, thereby rendering the host susceptible to a lot of life-threatening opportunistic infections, neurological disorders, unusual malignancies and oral lesions.[1,2] HIV infection is an extremely complex disease which affects numerous systems such as central nervous system, cardiovascular system and hematolymphoid organs.[11]
Oral manifestations are among the earliest and most important indicators of HIV infection.[12,13] Oral manifestations are seen in 50% of HIV-infected patients and up to 80% of them will be due to acquired immunodeficiency.[14]
At present, three groups of oral manifestations are defined by Coogan et al., based on their intensity and features [Table 7].[14]
Table 7.
Represents three groups of oral manifestations as defined by Greenspan et al.

HIV has become one of the World's most serious health and developmental challenges. The first cases were reported in 1981 and today there are approximately 36.9 million people currently living with HIV, and tens of millions of people have died of AIDS-related causes since the beginning of the epidemic. The introduction of highly active antiretroviral therapy in HIV patients has brought a dramatic reduction in morbidity and mortality rates, and patients are living longer with a better quality of life.[12,15] Along with increasing life expectancy, the incidence of comorbidities are also increasing, this might be because of the use of antiretrovirals or due to the advanced age.[16]
The patients who are on HAART will also show some common secondary manifestation like oral melanotic pigmentation, which is one of the physiologic manifestations.[2,10]
Out of different manifestation seen in HIV patients on HAART, oral candidiasis stands first and oral melanotic pigmentation is the second most common manifestation according to studies by several authors.[17] But according to a study by Patil et al. oral melanotic pigmentation is the first most common manifestation.[2] Even in this study, oral melanotic pigmentation was the most common manifestation seen. Ranganathan et al. had found it to be the third most common lesion in their study[10] whereas Hamza et al. found this to be the second most common manifestation.[17] The possible reason for the occurrence of this pigmentation may be the increased release of α melanocyte stimulating hormone due to deregulated release of cytokines in HIV and use of melanocyte stimulating drugs like certain antiviral or antifungal agents and Addison's disease.[1,10]
The next finding seen was xerostomia. This was proved by a study conducted by Lin et al. to assess the effects of HAART therapy on salivary gland flow rates and composition among 39 HIV-negative and 147 HIV-positive patients. They found that there was a significant decrease in the salivary flow rates of the HIV-positive group as compared to the control group.[18] A study done by Navazesh et al. in 2009 found that protein inhibitors-based HAART therapy is a significant risk factor for developing reduced salivary flow rates and also have a role to play in salivary gland enlargement in HIV-positive patients.[18] Sandra Lopez-Verdin et al. studied 293 patients with and without HAART. The therapy group showed a significantly lower average salivary flow than did the group without therapy and they observed that the decreased flow rate after 1 year of therapy. The results were not conclusive, despite significant differences in xerostomia and flavor alteration between the groups was evident. They concluded that the ART could cause cumulative damage that affects the amount of salivary flow.[19] Xerostomia may be a side effect of drugs or may be due to the proliferation of CD8+ cells in salivary glands. This may be a factor responsible for dental decay in HIV patients on longstanding HAART.[20] Our study also showed that patients developed xerostomia with longer duration of HAART therapy that is patients who were on HAART therapy for more than 8 years showed xerostomia to be a common manifestation.
Gingivitis is seen due to reduced CD4 counts leading to susceptibility to opportunistic infections.[1,2,3] Our study showed a decrease in the incidence of gingivitis as the CD4 counts were increasing.
Angular cheilitis which is more commonly seen in pediatric patients is mainly because of certain drugs used for both therapeutic and recreational purposes in HAART. The most common side effect occurring in almost all patients on isotretinoin use is acne conglobata, which often are the earliest presenting signs of toxicity and measures of patient compliance.[21] Supporting this a study by Bodhade et al. in a total of 399 patients on HAART, angular cheilitis was found in 17 patients which is 4.3% of the study population. Even in our study, four patients out of eighty showed angular cheilitis which is 3% which is close to results obtained by Bodhade.[1] Angular cheilitis was seen mainly in children with <4 years of HAART.
Other manifestations seen in our study was marginal gingivitis which was 18% and was close to a study done by Pedreira et al. where it was 28%.[22]
Oral manifestations are common in HIV-positive patients and can be used to diagnose the immune status of patients. Long-term use of HAART reduced the opportunistic infections and increased certain physiologic manifestations like melanin pigmentation. A dramatic decrease in the prevalence of HIV-related oral opportunistic lesions was seen in our study which are similar to the other studies done by Hamza et al.[17] and Umadevi et al.[23]
As the oral lesions can be readily detected by a trained clinician in a standardized, objective fashion without any complicated or expensive diagnostic technique, the utility of oral manifestations has increased.[1,2] Patients with HIV may not have a regular dental checkup, so physicians must regularly examine patients of suspected HIV for oral manifestations and make a strong working relationship with dentists to provide diagnostic insight and valuable treatment.[20]
CONCLUSION
Our study of eighty patients from urban population showed very minimal oral findings. There was a decrease in oral manifestations with the increase in the CD4 count levels and the duration of HAART, but certain physiological manifestations like melanin pigmentation were increasing due to HAART. The urban population showed minimal oral findings because of awareness of HIV and good accessibility for treatment. Thus, we want to conclude that recognition, significance and treatment of these lesions in urban population does not require an elaborate setup, it can be treated with basic primary health care.
Financial support and sponsorship
Nil.
Conflicts of interest
There are no conflicts of interest.
REFERENCES
- 1.Bodhade AS, Ganvir SM, Hazarey VK. Oral manifestations of HIV infection and their correlation with CD4 count. J Oral Sci. 2011;53:203–11. doi: 10.2334/josnusd.53.203. [DOI] [PubMed] [Google Scholar]
- 2.Patil N, Chaurasia VR, Babaji P, Ramesh D, Jhamb K, Sharma AM. The effect of highly active antiretroviral therapy on the prevalence of oral manifestation in human immunodeficiency virus-infected patients in Karnataka, India. Eur J Dent. 2015;9:47–52. doi: 10.4103/1305-7456.149640. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Okoye AA, Picker LJ. CD4(+) T-cell depletion in HIV infection: Mechanisms of immunological failure. Immunol Rev. 2013;254:54–64. doi: 10.1111/imr.12066. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Aggarwal M, Rein J. Acute human immunodeficiency virus syndrome in an adolescent. Pediatrics. 2003;112:e323. doi: 10.1542/peds.112.4.e323. [DOI] [PubMed] [Google Scholar]
- 5.Patton LL, McKaig R, Strauss R, Rogers D, Eron JJ., Jr Changing prevalence of oral manifestations of human immuno-deficiency virus in the era of protease inhibitor therapy. Oral Surg Oral Med Oral Pathol Oral Radiol Endod. 2000;89:299–304. doi: 10.1016/s1079-2104(00)70092-8. [DOI] [PubMed] [Google Scholar]
- 6.Ceballos-Salobreña A, Gaitán-Cepeda LA, Ceballos-Garcia L, Lezama-Del Valle D. Oral lesions in HIV/AIDS patients undergoing highly active antiretroviral treatment including protease inhibitors: A new face of oral AIDS? AIDS Patient Care STDS. 2000;14:627–35. doi: 10.1089/10872910050206540. [DOI] [PubMed] [Google Scholar]
- 7.Reznik DA. Oral manifestations of HIV disease. Top HIV Med 2005. 2006;13:143–8. [PubMed] [Google Scholar]
- 8.Schmidt-Westhausen AM, Priepke F, Bergmann FJ, Reichart PA. Decline in the rate of oral opportunistic infections following introduction of highly active antiretroviral therapy. J Oral Pathol Med. 2000;29:336–41. doi: 10.1034/j.1600-0714.2000.290708.x. [DOI] [PubMed] [Google Scholar]
- 9.Arirachakaran P. Highly active antiretroviral therapy and its oral manifestations in HIV patients. Chulalongkorn Univ Dent J. 2013;32:69–88. [Google Scholar]
- 10.Ranganathan K, Reddy BV, Kumarasamy N, Solomon S, Viswanathan R, Johnson NW. Oral lesions and conditions associated with human immunodeficiency virus infection in 300 South Indian patients. Oral Dis. 2000;6:152–7. doi: 10.1111/j.1601-0825.2000.tb00326.x. [DOI] [PubMed] [Google Scholar]
- 11.Imtiaz SS, Kenchannavar PS. HIV and anaesthesia. Int J Biomed Res. 2014;1:1–4. [Google Scholar]
- 12.Ponnam SR, Srivastava G, Theruru K. Oral manifestations of human immunodeficiency virus in children: An institutional study at highly active antiretroviral therapy centre in India. J Oral Maxillofac Pathol. 2012;16:195–202. doi: 10.4103/0973-029X.98499. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Bajpai S, Pazare AR. Oral manifestations of HIV. Contemp Clin Dent. 2010;1:1–5. doi: 10.4103/0976-237X.62510. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Coogan MM, Greenspan J, Challacombe SJ. Oral lesions in infection with human immunodeficiency virus. Bull World Health Organ. 2005;83:700–6. [PMC free article] [PubMed] [Google Scholar]
- 15.Brady MT, Oleske JM, Williams PL, Elgie C, Mofenson LM, Dankner WM, et al. Declines in mortality rates and changes in causes of death in HIV-1-infected children during the HAART era. J Acquir Immune Defic Syndr. 2010;53:86–94. doi: 10.1097/QAI.0b013e3181b9869f. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Konopnicki D, Mocroft A, de Wit S, Antunes F, Ledergerber B, Katlama C, et al. Hepatitis B and HIV: Prevalence, AIDS progression, response to highly active antiretroviral therapy and increased mortality in the EuroSIDA cohort. AIDS. 2005;19:593–601. doi: 10.1097/01.aids.0000163936.99401.fe. [DOI] [PubMed] [Google Scholar]
- 17.Hamza OJ, Matee MI, Simon EN, Kikwilu E, Moshi MJ, Mugusi F, et al. Oral manifestations of HIV infection in children and adults receiving highly active anti-retroviral therapy [HAART] in Dar es Salaam, Tanzania. BMC Oral Health. 2006;6:12. doi: 10.1186/1472-6831-6-12. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.Navazesh M, Mulligan R, Karim R, Mack WJ, Ram S, Seirawan H, et al. Effect of HAART on salivary gland function in the Women's Interagency HIV Study (WIHS) Oral Dis. 2009;15:52–60. doi: 10.1111/j.1601-0825.2008.01456.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.López-Verdín S, Andrade-Villanueva J, Zamora-Perez AL, Bologna-Molina R, Cervantes-Cabrera JJ, Molina-Frechero N. Differences in salivary flow level, xerostomia, and flavor alteration in Mexican HIV Patients who did or did not receive antiretroviral therapy. AIDS Res Treat 2013. 2013:613278. doi: 10.1155/2013/613278. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20.Shrimali L. A study of oral manifestation of HIV/AIDS. Int J Oral Maxillofac Pathol. 2010;1:8–12. [Google Scholar]
- 21.Park KK, Brodell RT, Helms SE. Angular cheilitis, part 2: Nutritional, systemic, and drug-related causes and treatment. Cutis. 2011;88:27–32. [PubMed] [Google Scholar]
- 22.Pedreira EN, Cardoso CL, Barroso Edo C, Santos JA, Fonseca FP, Taveira LA. Epidemiological and oral manifestations of HIV-positive patients in a specialized service in Brazil. J Appl Oral Sci. 2008;16:369–75. doi: 10.1590/S1678-77572008000600003. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23.Umadevi KM, Ranganathan K, Pavithra S, Hemalatha R, Saraswathi TR, Kumarasamy N, et al. Oral lesions among persons with HIV disease with and without highly active antiretroviral therapy in Southern India. J Oral Pathol Med. 2007;36:136–41. doi: 10.1111/j.1600-0714.2006.00505.x. [DOI] [PubMed] [Google Scholar]