Abstract
Pheochromocytoma is a rare adrenal gland tumour, usually alerting the physician by causing hypertensive tachycardic attacks. Patients with pheochromocytoma can rarely present with clinical signs similar to acute coronary syndrome. QT interval prolongation and ST segment changes due to pheochromocytoma have also been reported in the literature in a few case reports. We report a patient who had been admitted to the emergency department with chest pain, ischaemic ECG changes and marked QT prolongation. Despite a normal coronary angiogram, we observed that the QT interval and ST segment morphologies had changed during the hospitalisation period. Adrenal adenoma was diagnosed incidentally on abdominal CT scan, and the final diagnosis was pheochromocytoma. The tumour was successfully excised and the patient is now symptom free. When there is lack of a typical clinical picture, the diagnosis of pheochromocytoma might be challenging. It is also very crucial, since misdiagnosis can be life-threatening.
Background
Pheochromocytoma is mostly a benign catecholamine secreting tumour originating from the adrenal gland. Sinus tachycardia, hypertensive attacks and diaphoresis are common symptoms. Atypical presentations mimicking ischaemic heart disease and repolarisation abnormalities can rarely be seen.1 Since pheochromocytoma needs a completely different treatment protocol, it is very important and challenging to make the differential diagnosis. We discussed an atypical case of pheochromocytoma presenting with clinical signs similar to acute coronary syndrome and with marked QT interval prolongation.
Case presentation
A 57-year-old woman was admitted to the emergency department with chest pain and abdominal discomfort. She had been having those symptoms intermittently since the past 2 months. A month before the admission, the patient had coronary angiography which revealed normal coronary arteries. She described her chest pain as typical angina. Abdominal discomfort and nausea were accompanying her episodes, lasting for a few days. The patient was diagnosed with hypertension 3 years ago and was under the treatment of ramipril 5 mg per day. Her blood pressure was not stable, having frequent ups and downs, especially over the past 1 month. She was prescribed 50 mg metoprolol for her palpitations at discharge, after the coronary angiography that was performed a month ago. She declared she was clinically worse and had unstable blood pressure especially after this medication.
Her ECG at admission showed precordial ST segment depression and ST segment elevation at the derivation aVR, with corrected QT interval (QTc) of 0.62 s on derivation D2, calculated by Bazzet's formula (QTc=QT/√RR, intervals in seconds) (figure 1A). Her blood pressure was 135/90 mm Hg and cardiovascular examination was normal except for the S4 sound. Serum sodium, potassium, magnesium and calcium levels were all in normal limits. There was no usage of drugs causing QT prolongation. Initial troponin I level was 0.79 ng/mL (normal <0.06 ng/mL), which peaked at 2.15 ng/mL. Echocardiographic examination revealed hypertrophic myocardium with apical akinesia with ejection fraction of 40%, calculated by the modified Simpson method. The patient was admitted to the coronary care unit and started to receive acute coronary syndrome treatment. Coronary angiography showed normal coronary arteries. Owing to the myocardial dysfunction and elevated cardiac enzymes, a presumptive diagnosis of myocarditis was made and cardiac MRI was planned for further investigation. She was followed up under ramipril 5 mg and metoprolol 25 mg per day.
Figure 1.
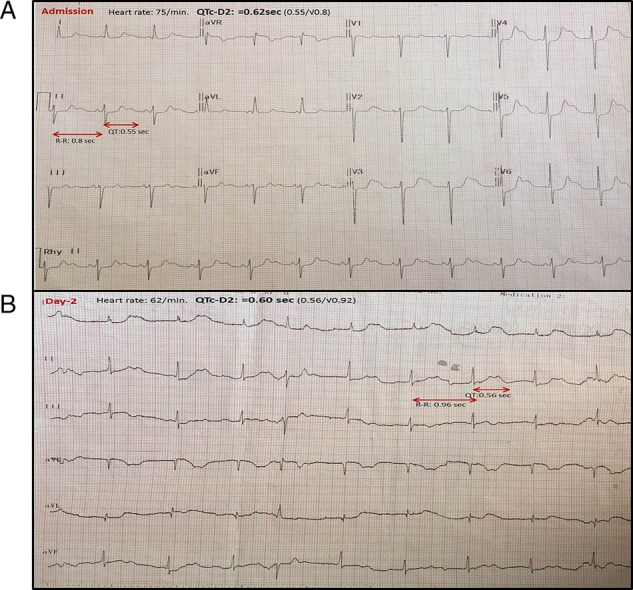
(A) ECG at admission with corrected QT interval (QTc) of 0.62 s, calculated by Bazzet's formula at derivation D2. (B) Dynamic T wave changes at day 2, with QTc of 0.60 s, calculated at derivation D2.
During the following days QTc and ST segment morphologies were noted to change and return to normal spontaneously (figures 1B and 2A, B show the ECGs on day 2, 4 and 7 of admission, respectively). Her control echocardiography at the seventh day of admission revealed normal contractility with ejection fraction of 60%, by the modified Simpson method. Her cardiac MRI that was performed at the 4th day of admission revealed no late gadolinium enhancement Therefore, myocarditis was not the diagnosis.
Figure 2.
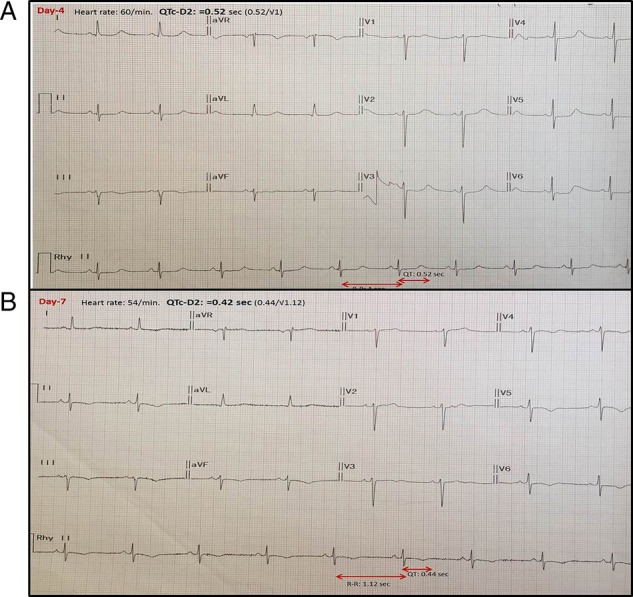
(A) At day 4, corrected QT interval (QTc) of 0.52 s at derivation D2. (B) At the end of the first week of admission, QTc was of 0.42 s (in normal limits) at derivation D2.
Investigations
During the follow-up, the patient had an abdominal CT scan for further investigation of her intermittent abdominal pain. As a result, a 25×35 mm left adrenal mass was detected (figure 3). Endocrinological assays for the adrenal gland were carried out for differential diagnosis. Plasma renin, aldosterone, morning adrenocorticotropic hormone (ACTH) and cortisol levels were all in normal limits, but normetanephrine and vanillylmandelic acid levels in 24-hour urine were detected as eight times and five times higher than the upper normal limit, respectively. The patient's diagnosis was of pheochromocytoma.
Figure 3.
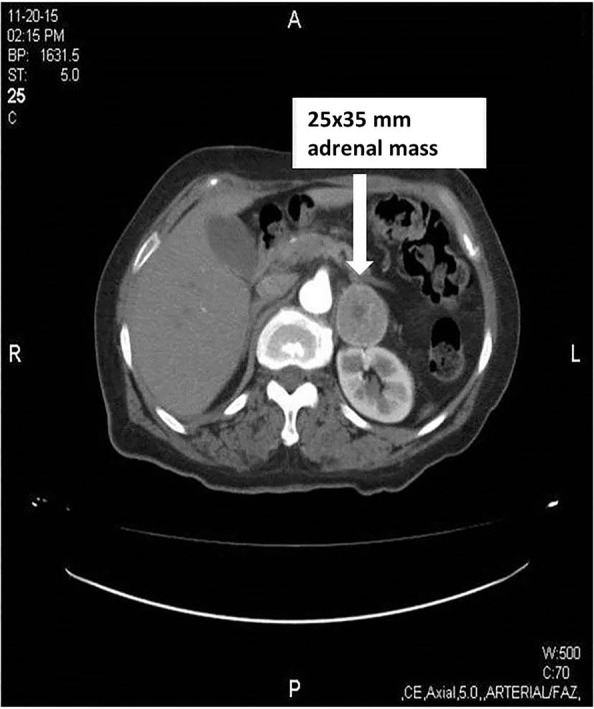
Abdominal CT scan revealing left adrenal solid mass of 25×35 mm.
Treatment
The β-blocker treatment that she had been taking for the past 6 weeks, was terminated and doxazosin treatment was initiated and titrated. The tumour was excised by left adrenalectomy and the pathology confirmed a non-malignant adrenal pheochromocytoma.
Outcome and follow-up
Her postoperative ECG was completely normal with QTc of 0.40 s. The patient has had an uneventful follow-up since the past 8 months, free of chest or abdominal pain and she has had no ECG changes.
Discussion
Cardiac presentation with typical chest pain and ischaemic ECG changes can be the initial presenting sign in patients with pheochromocytoma, as it was in our case report. Also, abdominal discomfort was accompanying the chest pain and these symptoms were experienced as attacks by our patient. We were able to make the diagnosis of pheochromocytoma only during the further investigation period of the abdominal symptoms. She had no hypertensive attacks or tachycardia during her hospitalisation. But, her history of intermittent symptoms of chest pain and abdominal discomfort with a normal coronary angiography, left ventricular hypertrophy in echocardiography and hypertensive attacks especially after the β-blocker treatment, should have alerted us about the possible diagnosis.
The ECG abnormalities in patients with pheochromocytoma occur mostly due to excessively high circulating catecholamine levels stimulating the myocardium.2 Different ratios of norepinephrine and epinephrine levels affect the diversity of the clinical manifestations.3 QT prolongation has been described in 16–35% of patients at various degrees, but QTc is rarely more than 0.60 s as described in the literature.1 4 In our case, QTc at admission was 0.62 s at derivation D2, calculated by Bazzet's formula. Catecholaminergic discharge during the pheochromocytoma attack leads to abnormalities of repolarisation, presenting mainly with prolonged QT interval and ST segment changes as in our case, and sometimes with deep symmetrical inverted T waves.1 These repolarisation abnormalities seldom give rise to dangerous ventricular arrhythmias.5 6
In our case, we demonstrated the dynamic QTc interval and ST segment changes that occurred daily after the pheochromocytoma attack. At day 7, it was almost normalised, as well as the wall motions at the echocardiography. All these dynamic changes were attributed to the dynamic changes of catecholamine levels after the initial attack.
Stress cardiomyopathy, also called as apical ballooning syndrome, occurs after an intense physical or emotional stress. It can lead to QT interval prolongation and predisposition to ventricular arrhythmias.7 It is also induced by triggered high levels of catecholamines, toxic to the myocardium. Our patient had no history of recent intense stress or surgical intervention, but she had apical akinesia without ballooning, which as well as the ECG changes were reversible. This reversible and similar type of cardiac dysfunction at pheochromocytoma and stress cardiomyopathy illustrates the similar toxic effects of the adrenergic system on the myocardium.
We believe our case demonstrates the importance of keeping the catecholaminergic states in mind for differential diagnosis, especially when ST segment and QT interval changes are accompanied with normal coronary arteries. Pheochromocytoma is well-known for its presentation with tachycardia, headache and diaphoresis triad. In our case, typical chest pain with ECG changes and abdominal discomfort were the presenting symptoms, without the typical signs of the classical triad.
Learning points.
When it lacks a typical clinical picture, the diagnosis of pheochromocytoma is challenging.
Intermittency of the cardiac symptoms accompanied by QT interval prolongation, ischaemic ST segment changes and transient ventricular dysfunction should alert us about the possible diagnosis of pheochromocytoma, of course after ruling out the acute coronary syndrome.
Variant angina should also be kept in mind when cardiac symptoms are intermittent. However, typical clinical presentation in variant angina is with prominent ST segment elevation accompanying chest pain and immediately resolving when the pain subsides.
In pheochromocytoma, suspicion may be the key clue to the diagnosis. Misdiagnosis can lead to β-blocker usage, which can be life-threatening.
Patient's perspective.
I had been having intermittent chest and abdominal pain for the last 2 months; I had two coronary angiograms in that period, both revealing normal coronary arteries. The prescribed drug after the first coronary angiography, made my health worse. Now, by the diagnosis of my disease ‘pheochromocytoma’ I had an operation and my adrenal gland with tumour was removed. I am living a healthy life now, no chest or abdominal discomfort and the doctors tell my heart is functioning normally.
Footnotes
Contributors: NO contributed in the conception and design of the case report, interpretation of data, patient follow-up, and in writing and revising of the manuscript. SA contributed in the study design, data collection, patient follow-up, literature search and in writing of the manuscript. TSTK contributed in data collection and processing, writing of the manuscript, and in critical revision of the final draft. CE contributed in supervision of the study, interpretation of data and in critical revision of the manuscript. All authors state that they agree for final revision of the article and ensure that all questions regarding the accuracy or integrity of the article are investigated and resolved.
Competing interests: None declared.
Patient consent: Obtained.
Provenance and peer review: Not commissioned; externally peer reviewed.
References
- 1.Liao WB, Liu CF, Chiang CW et al. . Cardiovascular manifestations of pheochromocytoma. Am J Emerg Med 2000;18:622–5. 10.1053/ajem.2000.7341 [DOI] [PubMed] [Google Scholar]
- 2.Agarwal V, Kant G, Hans N et al. . Takotsubo-like cardiomyopathy in pheochromocytoma. Int J Cardiol 2011;153:241–8. 10.1016/j.ijcard.2011.03.027 [DOI] [PubMed] [Google Scholar]
- 3.Paulin FL, Klein GJ, Gula LJ et al. . QT prolongation and monomorphic VT caused by pheochromocytoma. J Cardiovasc Electrophysiol 2009;20:931–4. 10.1111/j.1540-8167.2008.01405.x [DOI] [PubMed] [Google Scholar]
- 4.Stenström G, Swedberg K. QRS amplitudes, QTc intervals and ECG abnormalities in pheochromocytoma patients before, during and after treatment. Acta Med Scand 1988;224:231–5. 10.1111/j.0954-6820.1988.tb19366.x [DOI] [PubMed] [Google Scholar]
- 5.Leite LR, Macedo PG, Santos SN et al. . Life-threatening cardiac manifestations of pheochromocytoma. Case Rep Med 2010;2010:976120 10.1155/2010/976120 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Choi SY, Cho KI, Han YJ et al. . Impact of pheochromocytoma on left ventricular hypertrophy and QTc prolongation: comparison with takotsubo cardiomyopathy. Korean Circ J 2014;44:89–96. 10.4070/kcj.2014.44.2.89 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Madias C, Fitzgibbons TP, Alsheikh-Ali AA et al. . Acquired long QT syndrome from stress cardiomyopathy is associated with ventricular arrhythmias and torsades de pointes. Heart Rhythm 2011;8:555–61. 10.1016/j.hrthm.2010.12.012 [DOI] [PubMed] [Google Scholar]


