The temporal inverted internal limiting membrane flap technique, which is a simple surgical strategy to treat macular holes, provides scaffolding for retinal gliosis and may facilitate bridge formation between the walls of the macular hole beneath the flap. The procedure may be a good option to achieve macular hole closure without postoperative prone positioning.
Key words: macular hole, temporal inverted internal limiting membrane flap technique, prone positioning
Purpose:
To report the surgical technique and efficacy of the temporal inverted internal limiting membrane (ILM) flap technique for a patient with an idiopathic macular hole (MH) who is unable to maintain postoperative prone positioning.
Methods:
Case report.
Results:
A 73-year-old man with a Stage III MH in his left eye was scheduled to undergo surgery. Owing to his inability to maintain postoperative prone positioning for continuous placement of a transdermal bladder catheter after radical cystoprostatectomy to treat urinary bladder cancer, he underwent pars plana vitrectomy combined with the temporal inverted ILM flap technique and intraocular sulfur hexafluoride gas tamponade. The technique included ILM peeling at a temporal area of the macula to create one 2-disk-diameter semicircular ILM flap and inversion of the ILM flap nasally to cover the MH. Optical coherence tomography showed that MH closure started from the top of the MH just beneath the covered ILM flap; the closure process gradually extended toward the bottom of the MH. The well-aligned fovea recovered in 5 weeks postoperatively. The visual acuity was 20/200 preoperatively and improved to 20/50 postoperatively.
Conclusion:
The temporal inverted ILM flap technique, a simple surgery to treat MHs, provides scaffolding for retinal gliosis and may facilitate bridge formation between the walls of the MH beneath the flap. The procedure may be a good option to achieve MH closure without postoperative prone positioning.
Macular hole (MH) surgery combined with pars plana vitrectomy, internal limiting membrane (ILM) peeling, and intraocular gas tamponade has been a standard technique for the surgical repair of idiopathic MHs in recent years. Although some investigators have reported satisfactory results with single-procedure MH closure rates of 60% to 100% without postoperative face-down positioning,1,2 most surgeons instruct patients to remain face-down postoperatively to facilitate optimal surgical results. Thus, patients incapable of maintaining that position due to older age or other physical and psychological reasons may achieve a poor MH closure rate and remain challenging. Michalewska et al first reported the inverted ILM flap technique as a new surgical strategy that was successfully used for large MHs and MHs in highly myopic eyes for which a poor single-procedure MH closure rate was expected.3,4 The modified original inverted ILM flap technique for large MHs—in the temporal inverted ILM flap technique, a 2-disk-diameter ILM is removed from the temporal side of the fovea and inverted to cover the macular hole while leaving the nasal ILM in place—was newly reported to decrease the risk of surgical trauma and dissociated optic nerve fiber layer appearance with the same anatomical and functional results compared with the original inverted ILM flap technique.5 Michalewska and Nawrocki6 performed the original inverted ILM flap technique combined with intraocular silicone oil tamponade to treat a patient with a MH who could not remain face-down because of thyroid excision.6 We report one case of a successful temporal inverted ILM flap technique performed in combination with intraocular sulfur hexafluoride (SF6) gas tamponade to treat a patient with a MH who could not maintain postoperative prone positioning.
Case Report
A 73-year-old man was referred to Shimane University Hospital for metamorphopsia and decreased vision in his left eye for 2 months. His best-corrected visual acuity was 20/200 left eye. Optical coherence tomography showed a full-thickness Stage III MH (maximal diameter, 351 μm) (Figure 1, A and B). Because of continuous placement of a transdermal bladder catheter after radical cystoprostatectomy to treat urinary bladder cancer, the patient could not maintain the postoperative face-down or prone position; thus, a poor single-procedure MH closure rate was expected. After providing written informed consent, he underwent 25-gauge pars plana vitrectomy combined with the temporal inverted ILM flap technique. The technique included ILM staining with 0.125% solution of indocyanine green for better ILM visualization, making a semicircular ILM notch at 2-disk-diameter distance from MH in a temporal area by a 25-gauge MVR knife (MANI, Utsunomiya, Japan), ILM peeling at a temporal area of the macula to create a semicircular ILM flap using the 25-gauge end-grasping forceps (Alcon, Fort Worth, TX), inversion of the ILM flap in the nasal direction to fully cover the MH (Figure 2, A and B), and then placement of a low-molecular-weight viscoelastic material (VISCOAT; Alcon) on the inverted flap to stabilize it (Figure 2C). After fluid–air exchange, SF6 gas was injected into the vitreous cavity. The patient was advised to lie on his right side postoperatively. Optical coherence tomography showed that the ILM flap covered the MH at postsurgical Week 1 (Figure 3A), movement of both edges of the MH toward the center with formation of a thick wall beneath the ILM flap at postoperative Week 3 (Figure 3B), and MH closure leaving a partial defect in the inner segment/outer segment line at postoperative Week 4 (Figure 3C). At postoperative Week 5, the defect in the inner segment/outer segment line resolved and the best-corrected visual acuity improved to 20/50 left eye (Figure 3D).
Fig. 1.
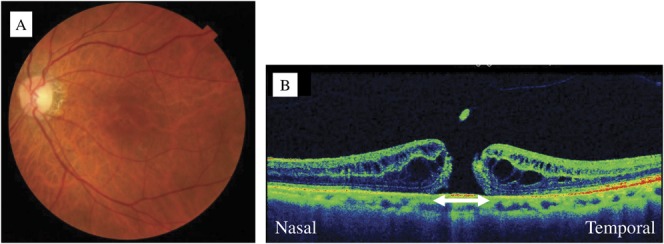
A. A preoperative fundus photograph of the left eye. B. An optical coherence tomography image shows a stage III MH. The maximal diameter of the MH is 351 μm (arrow).
Fig. 2.
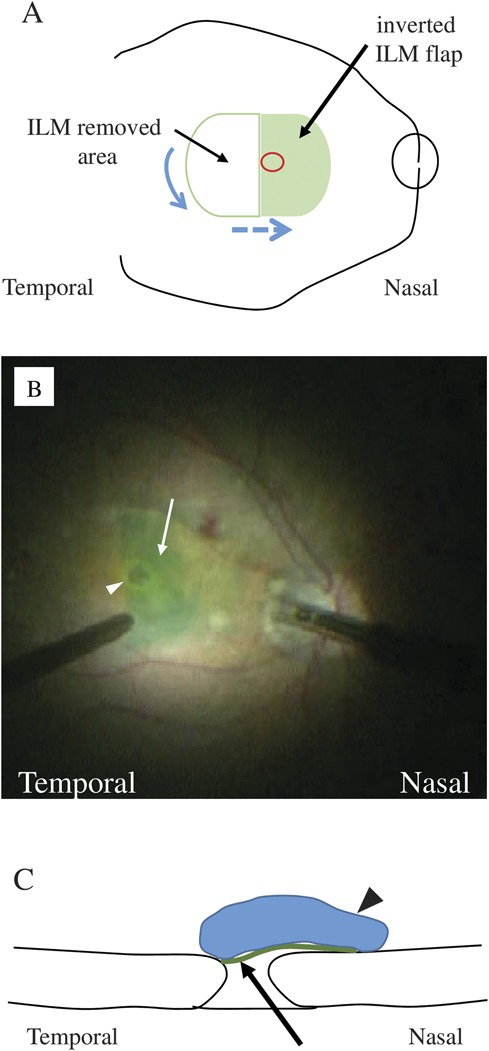
A. Schematic drawing of the temporal ILM flap technique. After a semicircular ILM notch (blue arrow) is created at 2-disk-diameter distance from temporal edge of MH (red circle), ILM is peeled and inverted in the nasal direction to fully cover the MH (blue dotted arrow). B. Capture of surgical video. An indocyanine green-stained temporal internal limiting membrane flap created at the temporal macular is inverted in the nasal direction (arrow) to cover the macular hole (arrowhead). C. Crosssectional drawing of the temporal ILM flap technique. The temporal ILM flap (arrow) is inverted to the direction of nasal retina to cover the MH and is stabilized with a low-molecular-weight viscoelastic material (arrow head).
Fig. 3.
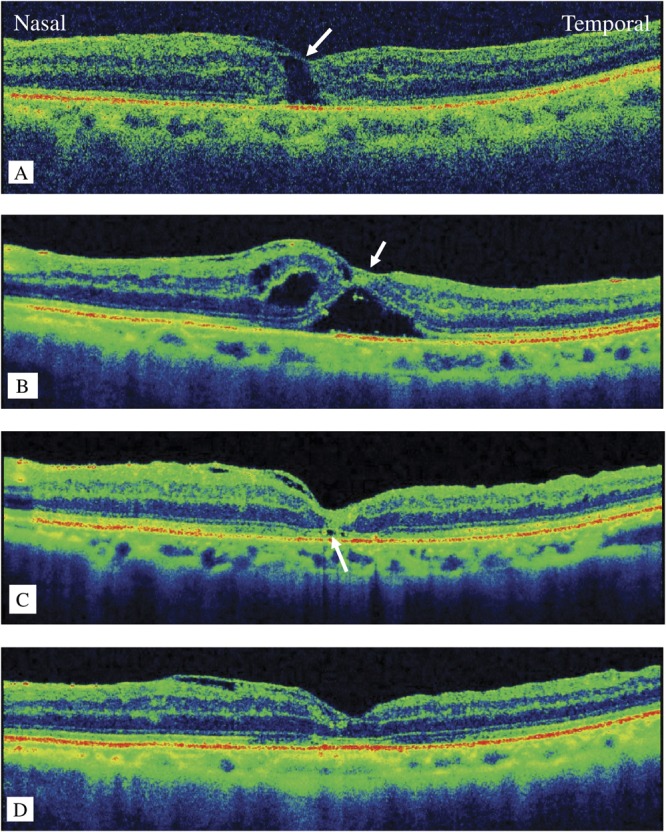
Postoperative optical coherence tomography images. A. at postoperative Week 1, the macular hole (MH) remains open under the covered internal limiting membrane (ILM) flap (arrow). B. at postoperative Week 3, the MH edges form a bridge beneath the ILM flap. C. at postoperative Week 4, the MH has closed leaving a partial defect in the inner segment/outer segment line (arrow). D. at postoperative Week 5, the full thickness of the fovea has recovered.
In the original inverted ILM flap technique, to create several small ILM flaps, the ILM is peeled circumferentially around the MH leaving the ILM unpeeled at the MH edge. The trimmed flaps then were inverted and placed over the surface of MH from all sides. In the original technique, the inverted ILM flap was detached spontaneously in 14% of cases during fluid–air exchange.3 Shin et al7 used perfluoro-n-octane to keep the single-layered ILM flap of 1-disk-diameter size inverted until the completion of fluid-air exchange. Conversely, in the temporal inverted ILM flap technique one ILM flap of about 2-disk diameters, which was created on the temporal side of the MH, was inverted to the nasal side to cover the MH. One large flap with a wider connection to the retina does not detach spontaneously and does not easily flip back owing to the use of viscoelasitic material during fluid-air exchange. Thus, this technique is much simpler and easier to achieve the procedure certainly than the original technique. The rationale for the original method of MH closure is explained by filling the MH space with residual proliferating glial cells from both the surface of the peeled ILM and inside the retina around the MH. Other investigators suggested that the small trimmed ILM flaps, which settle at the bottom of the MH, become an obstacle to natural MH closure and/or functional recovery of the outer retina.8 However, in the temporal inverted ILM flap technique, one large ILM flap can hardly move to the bottom of the MH and become an obstacle to natural MH closure.
Serial optical coherence tomography observations of this patient provided the manner of early structural recovery of macula after the MH surgery with the temporal inverted ILM flap technique. The exact mechanism of MH closure using the original or temporal inverted ILM flap technique is not precisely understood. In this case, MH closure started from the top of the MH space just beneath the covered ILM flap (Figure 3B). With the current technique, glial cells, if present and adhering to the ILM flap, should be on the surface side of the retina and therefore could not migrate to the MH space; thus, glial cells inside the MH wall were speculated to play an important role. Adherent cells hardly proliferate and migrate without a basement membrane; for example, lens epithelial cells cannot migrate into an open area after posterior capsulotomy. Thus, providing a scaffold for MH wall gliosis at the top of the MH space without providing a possible obstacle to the bottom of the MH may be the mechanism of the temporal inverted ILM flap technique. From a more detailed observation of the optical coherence tomography images, we realized that the initial bridging just beneath the covered ILM flap seemed to start around the outer nuclear layer edges. This manner of initial gliosis and later alignment of the inner segment/outer segment line observed in this case resembles observations reported in spontaneous MH closure9 and MH closure after vitrectomy combined with ILM peeling.10 Thus, the temporal inverted ILM flap technique likely enhances the “natural” course of MH closure.
In conclusion, the temporal inverted ILM flap technique is a simple surgical strategy, which provides a scaffold for retinal gliosis and possibly facilitates bridge formation between the walls of the MH just beneath the ILM flap especially in a patient with an idiopathic MH who is unable to maintain postoperative prone positioning. Regarding the MH closure rate and functional recovery, a further study should be able to confirm the advantages of this technique over other techniques.
Footnotes
None of the authors have any financial/conflicting interests to disclose.
References
- 1.Lange CA, Membrey L, Ahmad N, et al. Pilot randomised controlled trial of face-down positioning following macular hole surgery. Eye (Lond) 2012;26:272–277. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Iezzi R, Kapoor KG. No face-down positioning and broad internal limiting membrane peeling in the surgical repair of idiopathic macular holes. Ophthalmology 2013;120:1998–2003. [DOI] [PubMed] [Google Scholar]
- 3.Michalewska Z, Michalewski J, Nawrocki J, et al. Inverted internal limiting membrane flap technique for large macular holes. Ophthalmology 2010;117:2018–2025. [DOI] [PubMed] [Google Scholar]
- 4.Kuriyama S, Hayashi H, Jingami Y, et al. Efficacy of inverted internal limiting membrane flap technique for the treatment of macular hole in high myopia. Am J Ophthalmol 2013;156:125–131.e121. [DOI] [PubMed] [Google Scholar]
- 5.Michalewska Z, Michalewski J, Nawrocki J, et al. Temporal inverted internal limiting membrane flap technique versus classic inverted internal limiting membrane flap technique: a comparative study. Retina 2015;35:1844–1850. [DOI] [PubMed] [Google Scholar]
- 6.Michalewska Z, Nawrocki J. Macular hole surgery in a patient who cannot maintain facedown positioning. Case Rep Ophthalmol 2013;4:1–6. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Shin MK, Park KH, Park SW, et al. Perfluoro-n-octane-assisted single-layered inverted internal limiting membrane flap technique for macular hole surgery. Retina 2014;34:1905–1910. [DOI] [PubMed] [Google Scholar]
- 8.Sakurai H, Kinoshita F, Tano R, et al. Hemi-Inverted ILM flap technique for macular hole. Rinsho Ganka 2014;68:1449–1453. [Google Scholar]
- 9.Okubo A, Unoki K, Yamakiri K, et al. Early structural changes during spontaneous closure of idiopathic full-thickness macular hole determined by optical coherence tomography: a case report. BMC Res Notes 2013;6:396. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Sano M, Inoue M, Taniuchi S, et al. Ability to determine postoperative status of macular hole in gas-filled eyes by spectral-domain optical coherence tomography. Clin Experiment Ophthalmol 2011;39:885–892. [DOI] [PubMed] [Google Scholar]


