Abstract
Objective
Tube thoracostomy (TT) is a commonly performed intensive care procedure. Simulator training may be a good alternative method for TT training, compared with conventional methods such as apprenticeship and animal skills laboratory. However, there is insufficient evidence supporting use of a simulator. The aim of this study is to determine whether training with medical simulator is associated with faster TT process, compared to conventional training without simulator.
Methods
This is a simulation study. Eligible participants were emergency medicine residents with very few (≤3 times) TT experience. Participants were randomized to two groups: the conventional training group, and the simulator training group. While the simulator training group used the simulator to train TT, the conventional training group watched the instructor performing TT on a cadaver. After training, all participants performed a TT on a cadaver. The performance quality was measured as correct placement and time delay. Subjects were graded if they had difficulty on process.
Results
Estimated median procedure time was 228 seconds in the conventional training group and 75 seconds in the simulator training group, with statistical significance (P=0.040). The difficulty grading did not show any significant difference among groups (overall performance scale, 2 vs. 3; P=0.094).
Conclusion
Tube thoracostomy training with a medical simulator, when compared to no simulator training, is associated with a significantly faster procedure, when performed on a human cadaver.
Keywords: Education, Chest tubes, Simulation training, Cadaver
INTRODUCTION
Chest tube insertion is an invasive procedure commonly performed during the management of critically ill or injured patients [1]. The traditional method for teaching surgical procedures is apprenticeship, which allows novices to directly perform procedures on real patients for skill acquisition [2]. More advanced skills laboratories use animals such as dogs, cats, and pigs [3]. However, the use of live animals is prohibited in many countries due to strict regulations, and the use of a medical simulator has been suggested as an alternative [4]. Furthermore, medical simulation can provide the opportunity to learn and refresh skills for physicians at any level without risk to patients [5].
A few studies evaluated the efficacy of a medical simulator for chest tube insertion training, but these studies failed to show an advantage that could be transferred to actual performance [4,6,7]. All studies compared the efficacy of training on a simulator to animal models, with the limitation of not representing real patients. We performed this study to assess the actual efficacy of a medical simulator for training chest tube insertion using a human cadaver model, which is thought to provide the closest simulation of a living patient.
METHODS
The ethics review board of study site approved this study. Participants were recruited from a cadaver procedure workshop held in one medical school. The workshop is a yearly operative procedure skill course run by the department of emergency medicine. The curriculum includes surgical airways, intraosseous insertion, pericardiocentesis, central line insertion, and tube thoracostomy. The study was performed at the tube thoracostomy skill station using lightly-embalmed cadavers. A lightly-embalmed cadaver was used due to its soft and realistic texture. These cadavers were donated for educational and research purposes to the department of anatomy. Five cadavers with similar body status (male, weight 70 to 75 kg, height 170 to 175 cm, body mass index 20 to 25) with no anatomical anomalies or distortion were selected for this study. Two points in the third to sixth intercostal spaces were targeted for procedure. Emergency medicine residents with very few tube thoracostomy experience (≤3 times) were recruited for the study. After giving written consent participants were randomly divided into a conventional training group (CTG) and a simulator training group (STG). Randomization was performed using numbers generated by Microsoft Office Excel 2010 (Microsoft, Redmond, WA, USA). First, all participants watched a 20-minute didactic lecture including a video showing the entire process. Then, the CTG watched a demonstration by an instructor performing tube thoracostomy on a cadaver, while the STG directly performed tube thoracostomy on a simulator, the TraumaMan (Simulab, Seattle, WA, USA) with the guidance of an instructor. Standard chest tube insertion technique as described in the advanced trauma life support student course manual was used for the entire lecture and training process [8]. After the end of the lecture and training session, all participants performed tube thoracostomy on the cadavers in random sequence, regardless of assigned group. Incision to tube placement (ITP) time was measured and recorded for each performance and whether a performance succeeded was verified by dissecting the cadavers after the entire session was finished. Any type of malposition including intraparenchymal, fissural, chest wall, and mediastinal tube placement was considered a failed performance. Each participant was graded for difficulty in dissecting skin and muscles, pleural opening, and overall performance using a 10-point digital numerical scale, just after the end of procedure performance on a cadaver.
Mean and standard deviation values were used to report data with a normal distribution, and a median with interquartile range was used for nonparametric variables. Kaplan-Meier survival analysis using the log rank method was used to compare ITP time according to the group and a failed performance was treated as a censored case. The Mann-Whitney U-test and Fisher’s exact test were used to compare other measurable and non-measurable variables. A P-value <0.05 was defined as statistically significant. Microsoft Office Excel 2010 was used to record and analyze the data, and IBM SPSS Statistics ver. 21.0 (IBM Corp., Armonk, NY, USA) was used for statistical calculations.
RESULTS
A total of 29 participants were enrolled for the analysis (Fig. 1). There was no significant difference in general characteristics between the CTG and STG. Although the STG had a better success rate than the CTG, this was not statistically significant (Table 1). There was no significant difference in difficulty in dissecting skin and muscles, pleural opening, and overall performance between the groups (Table 2).
Fig. 1.
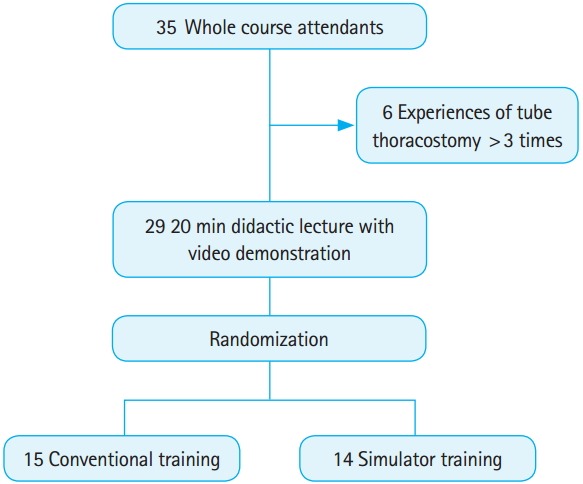
Selection and randomization of study participants.
Table 1.
General characteristics and performance data of the participants
| Training modality |
Overall | P-value | ||
|---|---|---|---|---|
| Conventional | Simulator | |||
| Age (yr) | 29 (28–34) | 29 (27–34) | 29 (28–34) | 0.861 |
| Training grade (yr) | 1 (1–2) | 1 (1–2) | 1 (1–2) | 0.880 |
| Male gender (%) | 73.3 | 85.7 | 79.3 | 0.651 |
| Prior experience (%) | 40.0 | 57.1 | 48.3 | 0.466 |
| Successful performance (%) | 66.7 | 78.6 | 72.4 | 0.682 |
Numerical values are expressed as median (interquartile range) for age and training grade. P-values were calculated using the Mann-Whitney U-test for age and training grade, and Fisher’s exact test for other variables.
Table 2.
Procedure difficulty during performance in a cadaver model (using a 10-point digital numerical scale)
| Difficulty in | Training modality |
Overall | P-value | |
|---|---|---|---|---|
| Conventional | Simulator | |||
| Dissection of skin/muscles | 3 (2–4) | 2 (2–3) | 3 (2–4) | 0.201 |
| Pleural opening | 4 (2–6) | 3.5 (2–5) | 4 (2–5) | 0.508 |
| Overall performance | 3 (2–5) | 2 (1.75–3.25) | 3 (2–4) | 0.094 |
Numerical values are expressed as median (interquartile range). P-values were calculated using the Mann-Whitney U-test.
Estimated median ITP time calculated from Kaplan-Meier survival analysis was 228.0 seconds (standard error, 92.3) in the CTG, and 75.0 seconds (standard error, 26.7) in the STG, which was significantly different (P=0.040) (Fig. 2).
Fig. 2.
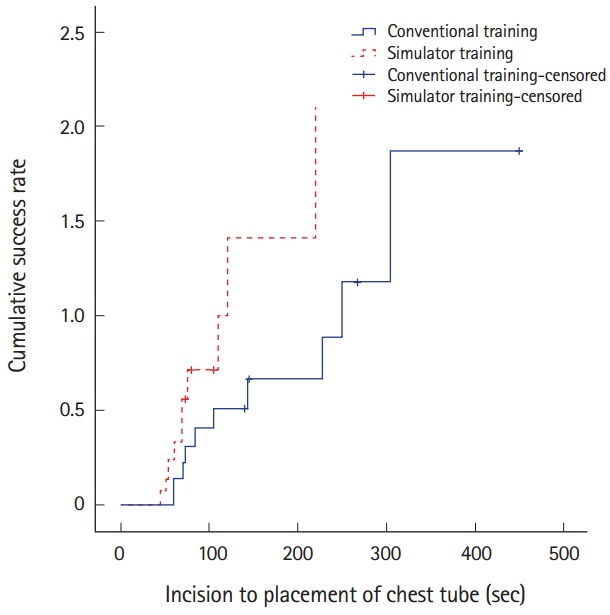
Cumulative success rate of tube thoracostomy in each group.
DISCUSSION
This is the first report to show the effect of simulator training on actual tube thoracostomy performance using a human cadaver model. Current use of a simulator for tube thoracostomy training has not been supported by sufficient positive evidence.
The classical concept of “see one, do one, teach one” in learning clinical skills has changed. Skill learners in all positions must have the opportunity to compare their level of performance against a standard and to practice until it meets an acceptable level of proficiency, which can be fulfilled by a sophisticated simulation model [2]. This is especially important for an emergency physician who is required to perform a wide range of procedures covering a broad spectrum of expertise [9]. However, there remains the possibility of inferior emergency procedure education using a simulation model compared to that using a live tissue model for skill acquisition [10]. Most prior studies providing supportive results for the use of a medical simulator in training of tube thoracostomy were limited to data showing subjective preference of the participants for simulation training, rather than measurable improvement in skill performance [4,6].
Our results failed to show any statistically significant difference in procedure success rates between CTG and STG, which might discourage the use of a simulation model in tube thoracostomy training, and was consistent with a previous study [7]. However, our study showed significant shortening of performance time in STG, even without any difference in subjective difficulty in performing tube thoracostomy, unlike a previous study. This might be due to the difference in study design, characteristics of the participants, or the statistical method used. Specifically, the statistical method we used to compare the procedure time, Kaplan-Meier survival analysis, is one of the most significant differences compared with other similar studies. Considering that most skill training sessions might include significant numbers of novices, there must have been a significant failure rate in performing the skill, not just a delay in performance time. Hence, we treated the failure cases using a special method, survival analysis, to correctly calculate and compare the performance time for skill assessment. Our result using survival analysis with log-rank comparison indicates that simulator training may be superior to the conventional method in performing more skillful tube thoracostomy, which was indicated by a marked difference in estimated procedure times between CTG and STG. This superiority of skill observed in our results indicates that simulator training may help novice physicians to achieve a certain level of tube thoracostomy technique more quickly than the conventional method of training, which may help them perform a safer procedure before they become fully experienced in tube thoracostomy. Based on the results of this and another study, a simulator model for tube thoracostomy training could be a good substitute for animal training models [10].
Our study had a few limitations. First, a short time interval after training to performance may be a major limitation of our study. This could discourage interpreting our data as the pure result of the educational effect of the intervention. Statistical comparison of general characteristics including training background was performed to overcome this. Second, the next or a later operator on each cadaver might be influenced by the incision or other marks left by the previous operator due to the limitation of the number of cadavers. We carefully performed randomization to avoid this. Third, our study was not statistically powered because only a limited number of participants were eligible for the analysis. Hence, any negative result in the study could not be generalized. Fourth, the criterion for selecting the participants with minimum tube thoracostomy experience was defined without any published evidence.
Tube thoracostomy training with a medical simulator, when compared to no simulator training, is associated with a significantly faster procedure, when performed on a human cadaver.
Capsule Summary
What is already known
A medical simulator has been suggested as a good alternative method for training of invasive procedure such as tube thoracostomy.
What is new in the current study
This study demonstrates that simulation training is associated with faster placement of tube thoracostomy, compared to the conventional training method.
Footnotes
No potential conflict of interest relevant to this article was reported.
REFERENCES
- 1.Mongardon N, Tremey B, Marty J. Thoracentesis and chest tube management in critical care medicine: a multicenter survey of current practices. Chest. 2010;138:1524–5. doi: 10.1378/chest.10-1193. [DOI] [PubMed] [Google Scholar]
- 2.Bass BL. Fundamental changes in general surgery residency training. Am Surg. 2007;73:109–13. [PubMed] [Google Scholar]
- 3.Proano L, Jagminas L, Homan CS, Reinert S. Evaluation of a teaching laboratory using a cadaver model for tube thoracostomy. J Emerg Med. 2002;23:89–95. doi: 10.1016/s0736-4679(02)00468-7. [DOI] [PubMed] [Google Scholar]
- 4.Berkenstadt H, Munz Y, Trodler G, Blumenfeld A, Rubin O, Ziv A. Evaluation of the trauma-man simulator for training in chest drain insertion. Eur J Trauma. 2006;32:523–6. [Google Scholar]
- 5.Cooke M, Irby DM, Sullivan W, Ludmerer KM. American medical education 100 years after the Flexner report. N Engl J Med. 2006;355:1339–44. doi: 10.1056/NEJMra055445. [DOI] [PubMed] [Google Scholar]
- 6.Block EF, Lottenberg L, Flint L, Jakobsen J, Liebnitzky D. Use of a human patient simulator for the advanced trauma life support course. Am Surg. 2002;68:648–51. [PubMed] [Google Scholar]
- 7.Hishikawa S, Kawano M, Tanaka H, et al. Mannequin simulation improves the confidence of medical students performing tube thoracostomy: a prospective, controlled trial. Am Surg. 2010;76:73–8. [PubMed] [Google Scholar]
- 8.American College of Surgeons Committee on Trauma . ATLS student course manual. Chicago, IL: American College of Surgeons; 2012. [Google Scholar]
- 9.Wang EE, Quinones J, Fitch MT, et al. Developing technical expertise in emergency medicine: the role of simulation in procedural skill acquisition. Acad Emerg Med. 2008;15:1046–57. doi: 10.1111/j.1553-2712.2008.00218.x. [DOI] [PubMed] [Google Scholar]
- 10.Hall AB. Randomized objective comparison of live tissue training versus simulators for emergency procedures. Am Surg. 2011;77:561–5. doi: 10.1177/000313481107700514. [DOI] [PubMed] [Google Scholar]


