Abstract
Background:
The functional benefits of double-row (DR) versus single-row (SR) rotator cuff repair are not clearly established.
Purpose:
To examine the effect of DR versus SR rotator cuff repair on functional outcomes and strength recovery in patients with full-thickness tears.
Study Design:
Randomized controlled trial; Level of evidence, 2.
Methods:
Forty-nine patients were randomized to DR or SR repairs; 36 patients (13 women, 23 men; mean age, 62 ± 7 years; 20 SR, 16 DR) were assessed at a mean 2.2 ± 1.6 years after surgery (range, 1-7 years; tear size: 17 medium, 13 large, 9 massive). The following data were recorded prior to surgery and at follow-up: Penn shoulder score, American Shoulder and Elbow Surgeons (ASES), and Simple Shoulder Test (SST) results; range of motion (ROM) for shoulder flexion, external rotation (ER) at 0° and 90° of abduction, and internal rotation (IR) at 90° of abduction; and shoulder strength (Lafayette manual muscle tester) in empty- and full-can tests, abduction, and ER at 0° of abduction. Treatment (SR vs DR) × time (pre- vs postoperative) mixed-model analysis of variance was used to assess the effect of rotator cuff repair.
Results:
Rotator cuff repair markedly improved Penn, ASES, and SST scores (P < .001), with similar improvement between SR and DR repairs (treatment × time, P = .38-.10) and excellent scores at follow-up (DR vs SR: Penn, 91 ± 11 vs 92 ± 11 [P = .73]; ASES, 87 ± 12 vs 92 ± 12 [P = .21]; SST, 11.4 ± 1.0 vs 11.3 ± 1.0 [P = .76]). Patients with DR repairs lost ER ROM at 0° of abduction (preoperative to final follow-up, 7° ± 10° loss [P = .013]). ER ROM did not significantly change with SR repair (5° ± 14° gain, P = .16; treatment by time, P = .008). This effect was not apparent for ER ROM at 90° of abduction (treatment × time, P = .26). IR ROM improved from preoperative to final follow-up (P < .01; SR, 17° ± 27°; DR, 7° ± 21°; treatment × time, P = .23). Rotator cuff repair markedly improved strength in empty-can (54%), full-can (66%), abduction (47%), and ER (54%) strength (all P < .001), with no difference between SR and DR repairs (P = .23-.75). All clinical tests with the exception of the lift-off test were normalized at follow-up (P < .05).
Conclusion:
Outcomes were not different between SR or DR repair, with generally excellent outcomes for both groups. Rotator cuff repair and subsequent rehabilitation markedly improved shoulder strength.
Keywords: full-thickness tear, shoulder strength, handheld dynamometer, empty-can test
Biomechanical superiority of double-row (DR) versus single-row (SR) arthroscopic rotator cuff repair has been consistently demonstrated in cadaveric models.11,12,17,19 Consistent with these biomechanical findings, multiple systematic reviews and meta-analyses have reported that retear rates are lower for DR versus SR repair.4,6,14,15,20,21 However, the clinical superiority of DR versus SR is still debated.5 Several meta-analyses have reported no difference in functional outcomes between SR and DR repairs.4,14–16 Two more recent meta-analyses indicated potentially better functional outcomes with DR repairs in patients with tear sizes greater than 3 cm.20,21
Most randomized controlled trials (RCTs) comparing DR with SR rotator cuff repairs have used standardized questionnaires as the primary measure of functional outcome.1–3,7–9,13 Some of these RCTs have examined shoulder strength,2,3,8,9,13 but in only 18,9 or 2 muscle groups.2,13 The only RCT to look at multiple muscle groups3 reported results relative to the contralateral arm. However, bilateral pathology is common in this patient population, and in long-term follow-up, the contralateral side does not represent a stable control. Thus, a comprehensive assessment of strength recovery after DR compared with SR rotator cuff repair is lacking. Additionally, RCTs have not examined outcomes in terms of the signs and symptoms commonly assessed in this patient population. The effectiveness of DR versus SR repair in resolving impingement signs or normalizing tests of rotator cuff integrity has not typically been examined in RCTs.
Therefore, the purpose of this RCT was to compare functional outcome between DR and SR in terms of standardized outcome scores, comprehensive shoulder strength recovery, and standardized clinical tests of rotator cuff integrity and symptomatology.
Methods
Patients presenting or referred to the authors (S.J.N. and S.J.L.) with complaints of shoulder pain or loss of function underwent evaluation and treatment of their involved shoulder. Diagnosis of rotator cuff tear was made based on history and clinical examination and confirmed by magnetic resonance imaging (MRI). The study was approved by an institutional review board, and patients provided written informed consent.
Patient Selection
Inclusion criteria included the following: a full-thickness rotator cuff tear >1 cm as seen on MRI, ability to comply with the standardized rotator cuff physical therapy program, willingness to be randomized to an SR or DR repair, and a tear pattern that was amenable to repair with either SR or DR fixation when evaluated at the time of surgery (eg, some complex tears or long-standing, retracted tears with poor tissue quality could not be repaired). During the surgical procedure, satisfaction of inclusion criteria was confirmed based on the operative findings. Exclusion criteria were revision rotator cuff repair, any neurological involvement, and presentation of trophic changes of the involved tendon.
Clinical Evaluation
Preoperative and postoperative clinical evaluations were performed by independent physical therapists with at least 7 years of orthopaedic clinical experience. These evaluators were blinded to the surgical repair technique performed. Evaluations were performed 1 to 2 weeks prior to surgery and more than 1 year postoperatively. Outcome measures used included the American Shoulder and Elbow Surgeons (ASES) shoulder score,18 Penn shoulder score,10 and Simple Shoulder Test (SST).18 Physical examination included the following shoulder special tests: Neer impingement sign, the lift-off test, abduction drop-arm test, O’Brien active compression test, Hawkins-Kennedy test, and lag sign at 0° and 90° of abduction.
Strength and Range of Motion Testing
Passive range of motion (ROM) was tested in the following planes using a standard goniometer: flexion, internal rotation (IR) and external rotation (ER) at 90° of shoulder abduction, and ER with arm at side. Strength measurements were performed using a handheld dynamometer (Lafayette Instruments) for shoulder flexion in the scapular plane with maximum humeral internal rotation (empty can), shoulder flexion with humeral external rotation (full can), shoulder abduction at 10° of abduction, and ER at 0° of abduction. The patient was instructed to resist with maximal force, and the tester performed a break test. Two trials were performed in each motion, and the mean of the results was used.
Surgical Technique
The surgical procedures were performed with the patient in the beach-chair position under regional anesthesia. The shoulder was prepared and draped in the usual sterile fashion. A diagnostic arthroscopy via standard anterior and posterior portals was performed. The rotator cuff tendon was debrided, and the greater tuberosity was gently abraded using a bur to allow bleeding from the greater tuberosity footprint. SR repairs were performed with double-loaded 5-mm Bio-Corkscrew anchors (Arthrex). The No. 2 FiberWire (Arthrex) sutures were passed through the cuff using a Scorpion Needle (Arthrex) in a horizontal mattress configuration and arthroscopically tied using a Duncan loop knot. The sutures were placed approximately 10 mm from the tendon edge and approximately 10 mm apart.
DR repairs were performed using the modified DR suture bridge technique. For the medial row, two 5-mm anchors were used (Bio-Corkscrew FT; Arthrex), double loaded with suture (FiberWire). Anchor placement was in the medial footprint at the articular margin. The anchors were placed as far anteriorly and posteriorly as possible within the margins of the tear to maximize the pressurized contact area. Both limbs from each of the 2 sutures were passed through the tendon (Scorpion Needle) at least 5 mm distal to the musculotendinous junction in a double mattress fashion, resulting in 4 mattress stitches medially. After the medial row was tied, the suture limbs were crossed to create suture bridges across the tendon. To complete the lateral row, two 4.57-mm SwiveLock anchors (Arthrex) were fully inserted at an angle perpendicular to the cortical surface at the lateral aspect of the greater tuberosity.
Rehabilitation
Postoperative rehabilitation was identical for both groups. For the first 4 weeks, the affected upper extremity was placed in an abduction sling (Ultrasling II; DJO Global) that was removed 3 times daily for pendulum exercises. Passive ROM up to 90° of forward flexion and 90° of abduction was allowed. Passive ER and IR ROM was restricted to 30° for the first 6 weeks. Scapular mobility and stability exercises were initiated at this time. From the fourth week, passive ROM was extended up to 120° of forward flexion and 120° of abduction. After 6 weeks, passive motion was increased as tolerated. Active motion was encouraged as well as specific training of the rotator cuff in the scapular plane before progressing to the frontal and sagittal planes. Abduction strengthening was initiated between 10 and 12 weeks postoperatively. ER strengthening at 0° of abduction was initiated 10 to 12 weeks postoperatively and progressed to 45° at approximately 16 weeks and 90° at approximately 20 weeks. Patients were in physical therapy 2 to 3 times per week for 3 to 4 months.
Statistical Analysis
Time (preoperative vs follow-up) by treatment (SR vs DR) mixed-model analysis of variance was used to assess the effect of SR versus DR repair on outcome scores, ROM, and strength. Comparison of clinical shoulder tests between SR and DR groups were assessed using chi-square analyses. Improvements in clinical shoulder tests with surgery were assessed using Wilcoxon signed-rank tests. Other between-group comparisons were made using independent t tests or chi-square analyses where appropriate. Based on the normal variability in treatment improvements in ASES scores,17 it was estimated that with 20 patients per group, an 11-point difference in improvement in ASES scores between SR and DR treatments could be detected at an alpha level of 0.05 with 80% power. A similar estimate was not possible for strength measures because previous studies have not reported strength improvements (and the SD of those improvements). Therefore, unpublished data from repeated strength tests on rotator cuff patients were used. Based on the variability in repeated strength tests for the 4 tests used, it was estimated that with 20 patients per group, an 11-N difference in improvement in strength between SR and DR could be detected at an alpha level of 0.05 with 80% power.
Results
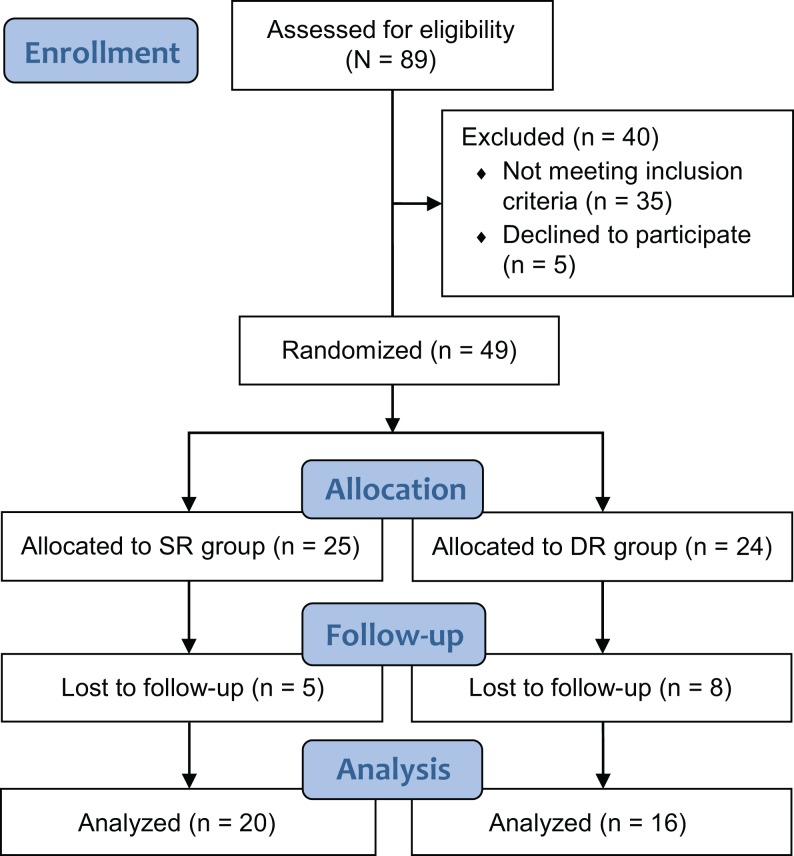
The initial study sample consisted of 49 patients who met the preoperative inclusion criteria and had intraoperative findings of a full-thickness rotator cuff repair that was greater than 1 cm (Figure 1). Surgeries were performed between 2007 and 2012. Thirty-six of these patients were available for follow-up at 1 year or more after surgery (20 SR, 16 DR). Of the 13 patients lost to follow-up, 6 had relocated to another part of the country, 4 were unwilling to come for the long-term follow-up examination, and 3 could not be reached by phone or other means. The remaining 36 patients were followed up with at a mean 26 ± 18 months after surgery (range, 23-84 months). Patients with DR repairs (4 women, 12 men) were older (65 ± 5 vs 61 ± 6 years, P < .05) and weighed more (89.7 ± 18.9 vs 76.9 ± 12.8 kg, P < .05) than SR patients (9 women, 11 men) but did not differ regarding height (1.76 ± 0.79 vs 1.68 ± 1.19 m, P = .08) nor proportions of men and women (P = .30). Tear size and concomitant pathology did not differ between SR and DR groups (Table 1).
Figure 1.
CONSORT (Consolidated Standards of Reporting Trials) flow diagram. DR, double-row; SR, single-row.
TABLE 1.
Operative Findingsa
| Single-Row Repair (n = 20) | Double-Row Repair (n = 16) | P Value | |
|---|---|---|---|
| Tear size | .89 | ||
| Medium (≥1 and <3 cm) | 8 | 7 | |
| Large (3-5 cm) | 7 | 5 | |
| Massive (>5 cm) | 5 | 4 | |
| Labral tear | 4 | 3 | .99 |
| SLAP tear | 2 | 2 | .99 |
| Biceps tear | 6 | 2 | .26 |
| AC DJD | 3 | 6 | .15 |
| GH DJD | 2 | 1 | .99 |
aAC, acromioclavicular; DJD, degenerative joint disease; GH, glenohumeral; SLAP, superior labral anterior-posterior.
One anterior labral repair was performed, and debridement was performed on the 6 other tears. A debridement was performed on all 4 superior labral anterior-posterior (SLAP) and all 8 biceps tears. Subacromial decompression was performed with 15 of 20 SR repairs and 9 of 16 DR repairs (P = .29). Resection of the distal clavicle was performed with 3 SR repairs and 6 DR repairs (P = .16). SR repairs were performed using a mean 1.8 ± 0.7 anchors (range, 1-4) compared with 3.9 ± 0.7 (range, 3-4) for DR repairs (P < .001).
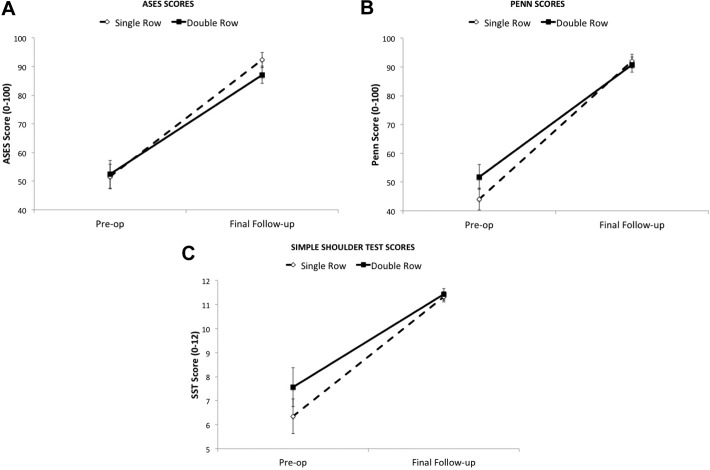
Functional Outcome Scores
ASES (P = .91), Penn (P = .19), and SST (P = .27) scores did not differ between SR and DR groups prior to surgery. All 3 outcome scores had improved substantially at final follow-up (P < .001), with similar improvements in SR and DR groups (Figure 2, A-C). At final follow-up, there was no difference in ASES (P = .21), Penn (P = .73), or SST (P = .76) scores between SR and DR groups.
Figure 2.
Functional outcome scores prior to and after surgery. (A) ASES scores: treatment × time, P = .38; time effect, P < .001. (B) Penn scores: treatment × time, P = .10; time effect, P < .001. (C) SST scores: treatment × time, P = .32; time effect, P < .001. ASES, American Shoulder and Elbow Surgeons; SST, simple shoulder test.
Clinical Tests
The results for the clinical shoulder tests are provided in Table 2. With the exception of the lift-off test, all clinical tests were significantly improved at final follow-up (P < .05). For the lift-off test, 53% of SR and 38% of DR patients had positive tests prior to surgery. Despite the high number of positive lift-off tests, only 4 of these patients were found to have a subscapularis test during surgery (all SR). At final follow-up, only 10% (n = 2) of patients with SR repairs (P < .01) but 44% (n = 7) of patients with DR repairs had positive lift-off tests (P < .05). The patients with positive lift-off tests at final follow-up had less passive ROM than the rest of the patients (12° less flexion, 9° less ER at 90° of abduction, and 10° less IR at 90° of abduction; all P < .05). ER ROM at 0° of abduction was not different (4° difference between groups). The drop-arm test, Hawkins-Kennedy test, and lag sign at 0° were negative in all patients at follow-up. Only 1 patient had a positive lag sign at 90°, and only 1 patient had a positive Neer impingement sign. The O’Brien test remained positive in 4 patients (2 SR, 2 DR).
TABLE 2.
Special Shoulder Tests Prior to Surgery and at Final Follow-upa
| Preoperative | Final Follow-up | P Value for Improvement | ||||||
|---|---|---|---|---|---|---|---|---|
| SR | DR | P Value | SR | DR | P Value | SR | DR | |
| Neer sign | 12/18b | 12/16 | .72 | 1/20 | 0/16 | .99 | <.001 | <.001 |
| Lift-off test | 10/19b | 6/16 | .50 | 2/20 | 7/16 | .049 | <.01 | .71 |
| Drop-arm test | 5/20 | 2/16 | .43 | 0/20 | 0/16 | n/a | <.05 | .16 |
| O’Brien test | 14/18b | 8/16 | .15 | 2/20 | 2/16 | .99 | <.001 | .06 |
| Hawkins-Kennedy test | 14/18b | 13/16 | .99 | 0/20 | 0/16 | n/a | <.001 | <.001 |
| Lag sign, 0° | 3/20 | 2/16 | .99 | 0/20 | 0/16 | n/a | .08 | .16 |
| Lag sign, 90° | 6/17b | 4/13c | .92 | 1/20 | 0/16 | .99 | <.05 | <.05 |
aDR, double-row repair; n/a, not applicable; SR, single-row repair.
bTests prior to surgery were not performed on patients who did not have sufficient range of motion or strength to place their arms in the test positions: Neer sign, n = 2; lift-off test, n = 1; O’Brien test, n = 2; Hawkins-Kennedy test, n = 2; Lag sign 90°, n = 3.
cThree patients were not tested.
Shoulder ROM
Prior to surgery, passive shoulder ROM was not different between the SR and DR groups (Table 3). IR ROM significantly improved from preoperative to final follow-up (P < .01), with no difference between SR and DR groups (P = .16). Patients with DR repairs had a 7° loss of ER ROM at 0° of abduction from preoperative to final follow-up (P < .05). At follow-up, patients with DR repairs had 10° less ER ROM at 0° of abduction than patients with SR repairs (P < .01). This effect was not apparent for ER ROM at 90° (5° difference, P = .18).
TABLE 3.
Shoulder Passive ROM Testsa
| Preoperative | Final Follow-up | P Value, ANOVA | ||||||
|---|---|---|---|---|---|---|---|---|
| ROM, deg | SR | DR | P Value | SR | DR | P Value | Time | Time × Treatment |
| Flexion | 148 ± 8 | 162 ± 10 | .31 | 170 ± 3 | 162 ± 3 | .09 | .08 | .09 |
| ER at 0° | 62 ± 12 | 65 ± 8 | .36 | 67 ± 10 | 59 ± 10 | .02 | .49 | .008 |
| ER at 90° b | 80 ± 26 | 84 ± 14 | .61 | 90 ± 8 | 85 ± 13 | .18 | .09 | .22 |
| IR at 90° b | 39 ± 21 | 45 ± 14 | .39 | 57 ± 15 | 50 ± 11 | .17 | .018 | .16 |
aData are reported as mean ± SD. ANOVA, analysis of variance; DR, double-row repair; ER, external rotation; IR, internal rotation; ROM, range of motion; SR, single-row repair.
bER and IR ROM measurements at 90° were not made on 4 patients who could not comfortably reach 90° of shoulder abduction prior to surgery (2 SR, 2 DR).
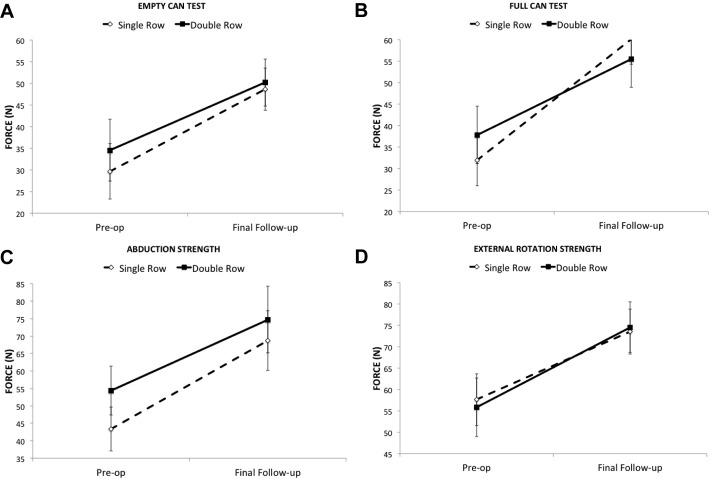
Shoulder Strength
Strength improved dramatically for all 4 tests from preoperative to final follow-up (Figure 3, A-D). Strength improvements were not different between SR and DR groups (P = .23-.75). For all patients, strength improved by 54% in the empty-can test, 66% in the full-can test, 47% in abduction, and 54% in external rotation.
Figure 3.
Clinical outcome scores prior to and after surgery. (A) Empty-can strength: effect of time, P < .001; treatment × time, P = .69. (B) Full-can strength: effect of time, P < .001; treatment × time, P = .23. (C) Abduction strength: effect of time, P < .001; treatment × time, P = .55. (D) External rotation strength: effect of time, P < .001; treatment × time, P = .75.
Factors Associated With Outcome
Greater passive shoulder flexion ROM at final follow-up was associated with better ASES (r = 0.37, P < .05) and Penn scores (r = 0.40, P < .05) and similar SST scores (r = 0.32, P = .06). Passive ER ROM at 0° of abduction at final follow-up was correlated with Penn scores (r = 0.36, P < .05), but this association did not reach statistical significance for the ASES (r = 0.32, P = .06) or SST scores (r = 0.21, P = .22). Other ROM tests at final follow-up were unrelated to outcome scores. No preoperative ROM measure was related to final functional outcome scores. Strength measures were unrelated to functional outcome scores. The 4 patients with SLAP tears had worse outcome scores compared with the rest of the patients (ASES, 73 ± 12 vs 92 ± 11 [P = .002]; Penn, 79 ± 15 vs 93 ± 9 [P = .008]; SST, 10.7 ± 1.5 vs 11.5 ± 0.9 [P = .14]). Prior to surgery, 4 patients had grade 4 fatty infiltration (based on the Goutallier classification), 1 patient had grade 3, 1 patient had grade 1, and the remaining patients had no fatty infiltration. Outcome scores were not different between patients with grade 3 or 4 fatty infiltration and the rest of the patients (P = .65-.93).
Discussion
The purpose of this RCT was to compare functional outcome between DR and SR in terms of standardized outcome scores, comprehensive shoulder strength recovery, and standardized clinical tests of rotator cuff integrity and symptomatology. There was no difference between DR and SR groups for outcome scores and strength recovery. Patients with DR repairs had less ER ROM at 0° of abduction than patients with SR repairs and had more positive lift-off tests.
The most notable finding with respect to the outcome scores was the overall excellent outcome regardless of type of rotator cuff repair. ASES scores averaged 87 and 92 out of 100 for DR and SR repairs, with Penn scores averaging 91 and 92 out of 100, and SST scores averaging 11.4 and 11.3 out of 12, respectively. These ASES scores are comparable to ASES scores reported in previous RCTs.2,3,9,12 A 12- to 17-point improvement in ASES scores is thought to represent a clinically important improvement.18 In the SR group, 19 of 20 patients had a ≥12-point improvement in ASES scores compared with 13 of 16 patients in the DR group. Thus, 89% of patients had clinically significant improvements in ASES scores.
Previous RCTs comparing DR and SR rotator cuff repairs have not reported the effect of surgery on clinical shoulder tests that are routinely used in the evaluation of patients with rotator cuff pathology. In the present study, 71% of patients had a positive Neer impingement sign prior to surgery and 79% had a positive Hawkins-Kennedy impingement test. At follow-up, only 1 patient (3%) had a positive Neer impingement sign, and no patients had a positive Hawkins-Kennedy test. Thus, both treatments successfully eliminated impingement signs (eg, pain) in most patients. Seven patients with DR repairs and 2 patients with SR repairs had positive lift-off tests at follow-up, but only 1 of these patients had subscapularis involvement at the time of surgery. These patients had less passive shoulder ROM than the patients with negative lift-off tests so this finding might be due to shoulder stiffness. Overall, the 9 patients tended to have lower ASES scores than patients with negative lift-off tests (84 ± 11 vs 92 ± 12, P = .10), but this was not apparent for Penn (90 ± 7 vs 92 ± 11, P = .61) or SST (11.3 ± 1.1 vs 11.3 ± 0.9, P = .90) scores. Four patients had subscapularis tears; all 4 were in the SR group, and the subscapularis tears were contiguous with supraspinatus and infraspinatus tears. These 4 patients had good outcomes (ASES, 96 ± 5; Penn, 94 ± 3; SST, 11 ± 1). Only 1 of these patients still had a positive lift-off test at follow-up. The O’Brien active compression test, drop-arm test, and lag sign at 90° showed significant improvements with treatment while the lag sign at 0° was only positive in 5 patients prior to surgery and negative in all patients at follow-up. Prior to surgery, there were a high number of positive O’Brien tests despite there being few SLAP tears. The resolution of the positive O’Brien tests after rotator cuff repair is likely due to the overall symptom resolution and strength improvement.
It is notable that at follow-up, patients with DR repairs had less ER ROM at 0° of abduction than patients with SR repairs. Patients with a DR repair had a loss of ER ROM from preoperative to follow-up. It is possible that increased coverage area in DR repair may have pulled the cuff too far laterally and constrained the anterior aspect of the glenohumeral joint, resulting in loss of ER ROM. This effect was not apparent with DR repairs in previous RCTs.1–3,7–9,13 Other ROM measures were not different between SR and DR repairs.
Decreased ER ROM at follow-up was associated with lower Penn scores (r = 0.36, P < .05), with a tendency toward lower ASES scores (r = 0.32, P = .06). Therefore, the loss of ER ROM in the DR patients may have some clinical significance. Flexion ROM at follow-up was also related to outcome scores (ASES: r = 0.37, P < .05; Penn: r = 0.40, P < .05). The combination of flexion ROM and ER ROM at 0° of abduction at follow-up dramatically impacted outcome scores. For the 20 patients with flexion ROM >164° and ER ROM >59°, ASES and Penn scores were 95 ± 7 and 96 ± 5, respectively. By contrast, ASES and Penn scores were markedly lower (P < .01) for the 7 patients with flexion ROM <165° and ER ROM <60° (ASES, 81 ± 17; Penn, 83 ± 16). Therefore, an emphasis on flexion ROM and ER ROM exercises in rehabilitation may improve outcomes after rotator cuff repair.
In the present study, restoration of strength in the empty- and full-can tests, ER, and abduction were shown to be similar between SR and DR repairs (see Figure 2, A-D). In previous RCTs, Burks et al2 demonstrated an 85% improvement in ER strength and a 69% improvement in IR strength, Grasso et al8 demonstrated a 40% improvement in full-can strength, Lapner et al9 demonstrated a 73% improvement in flexion strength, and Ma et al13 demonstrated a 53% improvement in abduction strength and a 71% improvement in ER strength. Strength improvements in the present study were 54% in the empty-can test, 66% in the full-can test, 47% in abduction, and 54% in ER. IR strength was not assessed in this study because in strong subjects it is not possible to perform a break test with the shoulder in 0° of abduction and it is not safe to test patients at 90° of abduction. With respect to the concomitant pathologies, the poor outcome scores for the 4 patients with SLAP tears (and debridement) are notable despite the small number of patients, as the outcome scores were very low (ASES, 73; Penn, 79; SST, 10.7).
While the present results are consistent with several other RCTs with respect to finding no differences in functional outcomes between DR and SR repairs, this study has some limitations. It was estimated that 20 patients per group would provide 80% power to detect an 11-point difference in ASES improvement between groups. Forty-nine patients were recruited to allow for anticipated loss to follow-up. At final follow-up, the intended sample size was achieved for the SR group but fell short by 4 patients for the DR group. Thus it is important to assess whether there was insufficient power to detect a meaningful difference in ASES scores between the DR and SR groups at follow-up. Post hoc power analysis indicated that there was 80% power to detect a 12-point difference in ASES scores between SR and DR groups. A 12- to 17-point difference in ASES scores is thought to be clinically significant.18 The actual difference in ASES scores was very small (SR, 92 ± 12; DR, 87 ± 12); therefore, it is unlikely that this negative finding is subject to type 2 error. Between-group differences in Penn scores (SR, 92 ± 11; DR, 91 ± 11) and SST scores (SR, 11.3 ± 1.0; DR, 11.4 ± 1.0) were similarly small. Thus, the lack of a significant difference in outcome scores is unlikely to be due to a lack of statistical power.
The lack of any postoperative imaging of the rotator cuff repairs is also a limitation in the present study. The present study sought to focus on functional recovery, specifically a comprehensive assessment of strength recovery and symptomatology with clinical shoulder tests. Other RCTs have not addressed the effect of DR versus SR on the normalization of clinical shoulder tests nor have they examined strength recovery in multiple muscle groups.
The mean follow-up was 22 ± 18 months with a wide range (12-84 months). Thus, it is important to understand the extent to which differences in outcomes between patients were due to differences in the length of time to follow-up. It was apparent that length of follow-up was unrelated to outcome scores (P = .36-.96), ROM results (P = .19-.90), or strength results (P = .11-.46).
Conclusion
This RCT found no advantage of DR repair compared with SR repair for medium, large, and massive rotator cuff tears in terms of outcome scores, clinical tests of shoulder function, shoulder ROM, or shoulder strength. Overall results were very good regardless of surgical technique. DR had some loss of ER ROM and a great number of patients with a positive lift-off test at follow-up. Poorer outcomes were associated with a preoperative SLAP tear and limited flexion and ER ROM at follow-up.
Footnotes
One or more of the authors has declared the following potential conflict of interest or source of funding: S.J.N. receives royalties from Arthrex Inc. S.J.L. is a paid consultant for Arthrex Inc.
References
- 1. Aydin N, Kocaoglu B, Guven O. Single-row versus double-row arthroscopic rotator cuff repair in small- to medium-sized tears. J Shoulder Elbow Surg. 2010;19:722–725. [DOI] [PubMed] [Google Scholar]
- 2. Burks RT, Crim J, Brown N, Fink B, Greis PE. A prospective randomized clinical trial comparing arthroscopic single- and double-row rotator cuff repair: magnetic resonance imaging and early clinical evaluation. Am J Sports Med. 2009;37:674–682. [DOI] [PubMed] [Google Scholar]
- 3. Carbonel I, Martinez AA, Calvo A, Ripalda J, Herrera A. Single-row versus double-row arthroscopic repair in the treatment of rotator cuff tears: a prospective randomized clinical study. Int Orthop. 2012;36:1877–1883. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4. Chen M, Xu W, Dong Q, Huang Q, Xie Z, Mao Y. Outcomes of single-row versus double-row arthroscopic rotator cuff repair: a systematic review and meta-analysis of current evidence. Arthroscopy. 2013;29:1437–1449. [DOI] [PubMed] [Google Scholar]
- 5. Dahm DL. Controversy remains regarding the optimal technique for arthroscopic rotator cuff repair. J Bone Joint Surg Am. 2012;94:106. [DOI] [PubMed] [Google Scholar]
- 6. Duquin TR, Buyea C, Bisson LJ. Which method of rotator cuff repair leads to the highest rate of structural healing? A systematic review. Am J Sports Med. 2010;38:835–841. [DOI] [PubMed] [Google Scholar]
- 7. Franceschi F, Ruzzini L, Longo UG, et al. Equivalent clinical results of arthroscopic single-row and double-row suture anchor repair for rotator cuff tears: a randomized controlled trial. Am J Sports Med. 2007;35:1254–1260. [DOI] [PubMed] [Google Scholar]
- 8. Grasso A, Milano G, Salvatore M, Falcone G, Deriu L, Fabbriciani C. Single-row versus double-row arthroscopic rotator cuff repair: a prospective randomized clinical study. Arthroscopy. 2009;25:4–12. [DOI] [PubMed] [Google Scholar]
- 9. Lapner PL, Sabri E, Rakhra K, et al. A multicenter randomized controlled trial comparing single-row with double-row fixation in arthroscopic rotator cuff repair. J Bone Joint Surg Am. 2012;94:1249–1257. [DOI] [PubMed] [Google Scholar]
- 10. Leggin BG, Michener LA, Shaffer MA, Brenneman SK, Iannotti JP, Williams GR., Jr The Penn shoulder score: reliability and validity. J Orthop Sports Phys Ther. 2006;36:138–151. [DOI] [PubMed] [Google Scholar]
- 11. Lorbach O, Bachelier F, Vees J, Kohn D, Pape D. Cyclic loading of rotator cuff reconstructions: single-row repair with modified suture configurations versus double-row repair. Am J Sports Med. 2008;36:1504–1510. [DOI] [PubMed] [Google Scholar]
- 12. Ma CB, Comerford L, Wilson J, Puttlitz CM. Biomechanical evaluation of arthroscopic rotator cuff repairs: double-row compared with single-row fixation. J Bone Joint Surg Am. 2006;88:403–410. [DOI] [PubMed] [Google Scholar]
- 13. Ma HL, Chiang ER, Wu HT, et al. Clinical outcome and imaging of arthroscopic single-row and double-row rotator cuff repair: a prospective randomized trial. Arthroscopy. 2012;28:16–24. [DOI] [PubMed] [Google Scholar]
- 14. Millett PJ, Warth RJ, Dornan GJ, Lee JT, Spiegl UJ. Clinical and structural outcomes after arthroscopic single-row versus double-row rotator cuff repair: a systematic review and meta-analysis of level I randomized clinical trials. J Shoulder Elbow Surg. 2014;23:586–597. [DOI] [PubMed] [Google Scholar]
- 15. Prasathaporn N, Kuptniratsaikul S, Kongrukgreatiyos K. Single-row repair versus double-row repair of full-thickness rotator cuff tears. Arthroscopy. 2011;27:978–985. [DOI] [PubMed] [Google Scholar]
- 16. Sheibani-Rad S, Giveans MR, Arnoczky SP, Bedi A. Arthroscopic single-row versus double-row rotator cuff repair: a meta-analysis of the randomized clinical trials. Arthroscopy. 2013;29:343–348. [DOI] [PubMed] [Google Scholar]
- 17. Smith CD, Alexander S, Hill AM, et al. A biomechanical comparison of single and double-row fixation in arthroscopic rotator cuff repair. J Bone Joint Surg Am. 2006;88:2425–2431. [DOI] [PubMed] [Google Scholar]
- 18. Tashjian RZ, Deloach J, Green A, Porucznik CA, Powell AP. Minimal clinically important differences in ASES and simple shoulder test scores after nonoperative treatment of rotator cuff disease. J Bone Joint Surg Am. 2010;92:296–303. [DOI] [PubMed] [Google Scholar]
- 19. Tuoheti Y, Itoi E, Yamamoto N, et al. Contact area, contact pressure, and pressure patterns of the tendon-bone interface after rotator cuff repair. Am J Sports Med. 2005;33:1869–1874. [DOI] [PubMed] [Google Scholar]
- 20. Xu C, Zhao J, Li D. Meta-analysis comparing single-row and double-row repair techniques in the arthroscopic treatment of rotator cuff tears. J Shoulder Elbow Surg. 2014;23:182–188. [DOI] [PubMed] [Google Scholar]
- 21. Ying ZM, Lin T, Yan SG. Arthroscopic single-row versus double-row technique for repairing rotator cuff tears: a systematic review and meta-analysis. Orthop Surg. 2014;6:300–312. [DOI] [PMC free article] [PubMed] [Google Scholar]