Abstract
Background
With a growing focus on the importance of men’s reproductive health--including preconception health--the ways in which young men’s knowledge, attitudes, and beliefs (KAB) predict their reproductive paths are understudied.
Objective
To determine if reproductive KAB predicts fatherhood status, timing and residency (living with child or not).
Methods
Reproductive KAB and fatherhood outcomes were analyzed from the National Longitudinal Study of Adolescent Health, a 20-year, nationally representative study of individuals from adolescence into adulthood. Four measures of reproductive KAB were assessed during adolescence in Waves I and II. A generalized linear latent and mixed model predicted future fatherhood status (non-father, resident/nonresident father, adolescent father) and timing while controlling for other socio-demographic variables.
Results
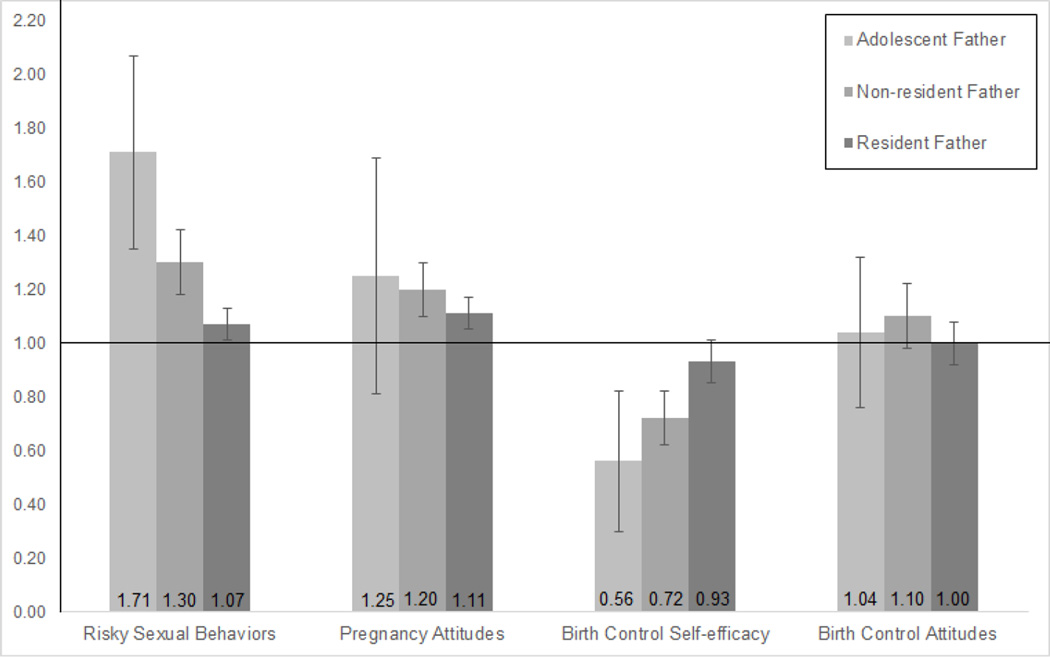
Of the 10,253 males, 3425 were fathers (686 non-resident/2739 resident) by wave IV. Higher risky sexual behavior scores significantly increased the odds of becoming nonresident father (OR=1.30, p < 0.0001), resident father (OR=1.07, p = 0.007), and adolescent father (OR=1.71, p < 0.0001); higher pregnancy attitudes scores significantly increased the odds of becoming a nonresident father (OR=1.20, p < 0.0001) and resident father (O =1.11, p < 0.0001); higher birth control self-efficacy scores significantly decreased the odds of becoming a nonresident father (O =0.72, p < 0.0001), and adolescent father (OR=0.56, p = 0.01).
Conclusion
Young men’s KAB in adolescence predicts their future fatherhood and residency status. Strategies that address adolescent males' reproductive KAB are needed in the prevention of unintended reproductive consequences such as early and nonresident fatherhood.
Introduction
The field of reproductive health is turning attention toward understanding young men’s reproductive needs and outcomes. [1] Despite the growing recognition of the importance of young men in reproductive health programs and policies, [2, 3] knowledge is lacking regarding men’s reproductive health [4] including such factors as fatherhood status and timing. While many studies explore women’s knowledge, attitudes, and beliefs (KAB) and their reproductive outcomes, [5–7] little is known about such associations in men. Recent research has examined adolescent male’s reproductive KAB and their sexual behavior, including abstinence, and condom and contraception use;[8–10] however, due to data limitations these studies could not account for a central outcome--entrance into fatherhood. Measuring KAB during adolescence, a period when such knowledge about sexual and reproductive behavior is developed [11] has the potential to inform future outcomes such as fatherhood status, timing and residency.
Studying adolescent reproductive KAB and later fatherhood may lead to earlier identification of young men at-risk for becoming adolescent or nonresident fathers, and improve sexual education programs to address the needs of these young men thereby helping them take control of their reproductive outcomes. Adolescent and nonresident fathers are known to be younger, have less education, lower SES, and to be unemployed[12, 13] with nonresident fathers having less contact, involvement and quality interactions with their children than do resident fathers. [14–16] Though many unmarried couples are cohabitating at the time of the child’s birth, 63% of unmarried fathers are nonresident with their child after five years [14]. One compelling perspective for understanding young, nonresident fathers and their well-being suggests including reproductive cultural values and norms along with reproductive attitudes, aspirations, and resources as part of a conceptual framework of fatherhood. [17] The National Campaign to End Teenage and Unwanted Pregnancy lists 17 characteristics of effective sexual education programs; paramount among them is to address “sexual psychosocial risk and protective factors that affect sexual behavior (e.g., knowledge, perceived risks, values, attitudes, perceived norms, and self-efficacy) and change them.”[18] Thus, education programs that focus on KAB during the formative adolescent years may be particular useful in preventing future unintended transitions to fatherhood.
The primary goal of this study is to determine if certain adolescent reproductive KAB predict fatherhood status, timing and residency. Data come from the National Longitudinal Study of Adolescent Health (Add Health), which followed a nationally representative sample of American youth from adolescence through early adulthood. This large, longitudinal, and nationally-representative data set allows better understanding of the reproductive paths young men take, fostering associations between adolescent KAB and later fatherhood outcomes. Understanding these connections may help identify at-risk young men earlier, allowing preventive interventions that address these men’s reproductive KAB.
Methods
Study Design and Sample
The National Longitudinal Study of Adolescent Health (Add Health) is a longitudinal study of a nationally representative sample of youth focusing on social, behavioral, and biomedical health as they progress from adolescence into adulthood. Wave I (n=10,253 males, ages=12–21; Response rate (RR):79%) was conducted in 1994–95; Wave II (n=7192, ages=13–21; RR:88.6%) in 1996; Wave III (n=7192, ages=18–28; RR:77.4%) six years later in 2001–02, and Wave IV (n=7347, ages=25–34; RR:80.3%) in 2007–08. Procedures for data access and analysis were implemented per our Institutional Review Board and in agreement with the Add Health data security plan.
Variables
Fatherhood status
Fatherhood status was the outcome of interest in this study. It was coded into three categories: non-fathers (referent), nonresident fathers, and resident fathers. At each wave, men reported in the household roster whether they had a biological child living with them; beginning in wave 3, men reported in the live child data set whether they fathered a biological child at all. If the same child is listed in the live child data set and the household roster, the father was categorized as a resident father. If a child was listed only in the live child data set, the father was categorized as a non-resident father. If no child was listed in either, the man was categorized as a non-father. If a biological child was listed only in the household roster (as may have occurred prior to wave 3), then the father was categorized as a resident father. Resident and non-resident fatherhood status was established at the earliest wave a biological child was listed and held constant through all future waves.
Reproductive knowledge, attitudes, and beliefs
Reproductive KAB was measured using four scales from data in both Waves I and II. Add Health contained no intact surveys or scales from pre-existing literature, building instead on a number of successful past surveys of adolescents and adults. [19] Three of the four measures used—1) risky sexual behavior scales, 2) pregnancy attitudes, and 3) birth control self-efficacy -- were administered in the student’s home by an interviewer. The fourth measure, 4) birth control attitudes, was administered via audio-CASI technology due to sensitivity. Each item was answered on a 5-point scale from “strongly agree” to “strongly disagree” except where otherwise noted. The KAB scales from both Waves I and II were used as individual variables in all analyses.
The risky sexual behavior scale (RSB) is a 10-item scale assessing reasons for engaging in or not engaging in sexual intercourse. This scale has been used in numerous studies investigating sexual and contraceptive behaviors, unintended pregnancies and sexually transmitted infections[20–23] Participants were presented with statements such as “If you had sexual intercourse your friends would respect you more’’ and “If you had sexual intercourse, you would feel less lonely. “ Higher scores indicated a greater motivation to engage in risky sexual behaviors.
The pregnancy attitude scale (PA) is a 2-item scale assessing the perceived impact of a pregnancy on the respondent’s life. [6, 24] Participants were presented with the statements “Getting someone pregnant at this time in your life is one of the worst things that could happen to you” and “It wouldn’t be all that bad if you got someone pregnant at this time in your life.” Higher scores indicate a more positive attitude towards getting someone pregnant.
The birth control self-efficacy scale (BCSE) is a 3-item scale assessing the perceived ability to ensure the use of birth control during sexual intercourse, used previously in studies of adolescent contraceptive usage [23–25] Each item was answered on a 6-point scale from “very sure” to “very unsure”, with the additional option of “I never want to use birth control”. Higher scores indicated a greater sense of self-efficacy to use birth control.
The birth control attitudes scale (BCA) is a 7-item scale assessing reasons for using or not using birth control.[23] Participants were presented with statements such as “In general, birth control is too much of a hassle to use” and “Using birth control interferes with sexual enjoyment.” Higher scores indicated a greater motivation to use birth control.
All four KAB scales were standardized to a continuous, standard normal distribution for both Waves I and II.
Socio-demographic variables
Socio-demographic variables were included in the analyses to control for confounding effects. Mother’s education, family income and participant’s self-reported race measured at wave I were included in the analyses. Participant’s education, personal income (if family income not used), age, and general health (an ordinal self-reported measure assessing health on a scale from “poor” to “excellent”) measured at Waves I through IV were included in the analyses. Age and marital status were removed from the analysis of adolescent fatherhood status due to their both being perfectly predictive of the outcome.
Statistical Analysis
In order to diagnose measures of validity, reliability, and unidimensionality (i.e. whether the scales measured a single construct) of the four latent constructs for both waves, classical item analyses were run including Cronbach’s alphas to measure internal consistency, item-rest correlations to measure homogeneity, and the ratio of the first two eigenvalues to assess dimensionality.
A logistic regressions was used to predict the odds of becoming an adolescent father given the KAB scales and key demographic variables (excepting age and marital status). A multinomial logistic regression was then used to predict the odds of becoming either a nonresident or resident father (compared to a non-father) given the above scales and independent variables. These regressions were modeled using a generalized linear latent and mixed model (GLLAMM), resulting in four repeated measures for each participant, and allowing each wave to act as a level-1 cluster. [26] Sample participants were classified within the GLLAMM into one of three fatherhood categories: non-fathers (referent), nonresident fathers, and resident fathers. When modeling the odds of becoming an adolescent father, the participants were classified into one of two categories: adolescent father (<18-years-old) and adult father (≥18-years-old; referent). To account for certain ethnicities being oversampled in Add Health (e.g. Blacks from higher educated families, Chinese, Cuban, and Puerto Rican participants), Add Health longitudinal weights were used in all analyses. Further, to account for this oversampling a level-2 random intercept was determined for race. All analyses were conducted in Stata 12.1 with multiple imputations of five cycles calculated to account for missing data. [27]
Results
Sample demographics
Of the 10,253 men in the sample, 3425 (33.5%) were fathers and 6828 (66.5%) were non-fathers by Wave 4. Of the fathers, 686 (20.0%) were nonresident and 2739 (80.0%) were resident (Table 1). Most resident fathers were married (72%), compared with nonresident fathers (8%) and non-fathers (13%). Equal numbers of nonresident fathers were white and African American. Resident fathers and non-fathers had more education than nonresident fathers. Additional demographic characteristics can be found in Table 1.
Table 1.
Characteristics of Fathers and Non-fathers
| Non-Fathers (N = 6828) |
Nonresident Fathers (N = 686) |
Resident Fathers (N = 2739) |
p-valuea | ||
|---|---|---|---|---|---|
| Age at Fatherhood Entranceb | N/A | 21.91 (3.98) | 25.60 (3.91) | 0.355 | |
| Racec | <0.001 | ||||
| White | 3434 (50.6) | 274 (39.3) | 1460 (53.3) | ||
| African-American | 1331 (19.6) | 274 (39.3) | 520 (19.0) | ||
| Hispanic | 1115 (16.4) | 97 (14.1) | 502 (18.3) | ||
| Asian | 609 (9.0) | 15 (2.2) | 143 (5.2) | ||
| Other | 302 (4.5) | 26 (3.8) | 113 (4.1) | ||
| Own Educationc,d | <0.001 | ||||
| Less than HS | 439 (6.4) | 127 (18.5) | 291 (10.6) | ||
| HS Graduate, Vocational School, or Technical School |
1357 (19.9) | 244 (35.6) | 927 (33.8) | ||
| Some college to college graduate | 2734 (40.0) | 251 (36.6) | 1227 (44.8) | ||
| Some graduate school to professional degree |
588 (8.6) | 15 (2.2) | 140 (5.1) | ||
| Personal Income (Wave IV)c | <0.001 | ||||
| < $30,000 | 698 (18.5) | 137 (36.3) | 294 (15.8) | ||
| $30,000 – $49,999 | 833 (22.1) | 86 (22.8) | 438 (23.6) | ||
| $50,000 – $74,999 | 852 (22.6) | 79 (20.9) | 503 (27.1) | ||
| > $75,000 | 1391 (36.9) | 75 (19.9) | 621 (33.5) | ||
| General Healthb | 0.236 | ||||
| 3.09 (0.848) | 3.04 (0.871) | 3.11 (0.824) | |||
| Marital Statusc | <0.001 | ||||
| Married | 857 (12.6) | 54 (7.9) | 1975 (72.1) | ||
| Unmarried | 5971 (87.4) | 632 (92.1) | 764 (27.9) | ||
| Mother's Educationc | <0.001 | ||||
| Less than HS | 868 (16.2) | 115 (20.6) | 419 (19.2) | ||
| HS Graduate, Vocational School, or Technical School |
2017 (37.7) | 256 (45.9) | 967 (44.2) | ||
| Some college to college graduate | 1919 (35.9) | 162 (29.0) | 674 (30.8) | ||
| Some graduate school to professional degree |
545 (10.2) | 25 (4.5) | 127 (5.8) | ||
| Parent's Income (Wave I)c | <0.001 | ||||
| < $30,000 | 1696 (29.7) | 262 (38.9) | 784 (29.2) | ||
| $30,000 – $49,999 | 1355 (23.7) | 137 (20.4) | 596 (22.2) | ||
| $50,000 – $74,999 | 1214 (21.3) | 84 (12.5) | 447 (16.6) | ||
| > $75,000 | 1442 (25.3) | 189 (28.1) | 862 (32.1) | ||
= p-values derived from F-test (continuous) and X2 (categorical variables);
= Mean (SD);
= N (%)
KAB scale diagnostics
Table A1 (online appendix) provides descriptive statistics of each KAB scale at Waves I and II. Psychometric properties were assessed by the totality of the information at both waves. By Wave II, all of the scales had a coefficient alpha of at least 0.70 with the two shortest scales each being slightly under 0.7 in Wave I. The item-rest correlations for all items were above 0.2 and the mean item-rest correlations for each scale were above 0.4 at each Wave.[28] The eigenvalue ratio, which determines whether the cumulative variance of the items in a scale can be explained by a single factor, exceeded the recommended value of 4.0 for all scales except the two-item Perceived Pregnancy Attitude scale.
Fatherhood status and adolescent KAB
Three of the four adolescent reproductive KAB scales collected during adolescence predicted future fatherhood status controlling for key socio-demographic variables for all of the analyses: risky sexual behaviors, pregnancy attitudes, and birth control self-efficacy (Table 2 and Table 3). The birth control attitudes scale was not statistically significant for either analysis.
Table 2.
Logistic Regression Model Predicting Adolescent Fatherhood Status
| Adolescent Fatherhood Status2 (N = 362) |
||||
|---|---|---|---|---|
| OR (SE) | p-value | 95% CI | ||
| Risky Sexual Behaviors1 | 1.71 (0.18) | < 0.0001 | (1.39, 2.12) | |
| Pregnancy Attitudes1 | 1.25 (0.22) | 0.205 | (0.89, 1.76) | |
| Birth Control Self-efficacy1 | 0.56 (0.13) | 0.010 | (0.36, 0.87) | |
| Birth Control Attitudes1 | 1.04 (0.14) | 0.752 | (0.80, 1.35) | |
| Mother's Education | 0.82 (0.08) | 0.046 | (0.68, 1.00) | |
| Own Education | 0.62 (0.04) | < 0.0001 | (0.54, 0.71) | |
| Income | 0.97 (0.14) | 0.834 | (0.73, 1.29) | |
| Employed | 0.91 (0.12) | 0.473 | (0.70, 1.18) | |
| General Health | 0.96 (0.05) | 0.360 | (0.87, 1.05) | |
| Intercept | 0.02 (0.01) | < 0.0001 | (0.01, 0.03) | |
| Random Effects | Estimate | SE | ||
| Race | ||||
| var(γ) | 0.223 | 0.0241 | ||
= Knowledge, Attitudes, and Belief scores were standardized over all men in the study
= Adult fathers (≥ 18-years-old) were referent group
Table 3.
Multinomial Logistic Regression Model Predicting Fatherhood and Residence Status
| Fatherhood & Residence Status | |||||||
|---|---|---|---|---|---|---|---|
| Non-resident Father2 (N = 686) |
Resident Father2 (N = 2739) |
||||||
| OR (SE) | p-value | 95% CI | OR (SE) | p-value | 95% CI | ||
| Risky Sexual Behaviors1 | 1.30 (0.06) | < 0.0001 | (1.18, 1.43) | 1.07 (0.03) | 0.007 | (1.02, 1.12) | |
| Pregnancy Attitudes1 | 1.20 (0.05) | < 0.0001 | (1.10, 1.30) | 1.11 (0.03) | < 0.0001 | (1.06, 1.17) | |
| Birth Control Self-efficacy1 | 0.72 (0.05) | < 0.0001 | (0.63, 0.81) | 0.93 (0.04) | 0.075 | (0.86, 1.01) | |
| Birth Control Attitudes1 | 1.10 (0.06) | 0.061 | (1.00, 1.22) | 1.00 (0.04) | 0.904 | (0.94, 1.08) | |
| Mother's Education | 0.89 (0.10) | 0.281 | (0.72, 1.10) | 0.79 (0.01) | < 0.0001 | (0.77, 0.82) | |
| Own Education | 0.66 (0.02) | < 0.0001 | (0.61, 0.70) | 0.88 (0.06) | 0.069 | (0.77, 1.01) | |
| Income Level | 1.05 (0.08) | 0.523 | (0.90, 1.22) | 1.16 (0.06) | 0.003 | (1.05, 1.29) | |
| Employed | 1.09 (0.07) | 0.212 | (0.95, 1.24) | 1.30 (0.04) | < 0.0001 | (1.22, 1.39) | |
| Married | 5.18 (4.50) | 0.058 | (0.94, 28.41) | 5.65 (1.49) | < 0.0001 | (3.37, 9.48) | |
| Age | 1.09 (0.03) | 0.001 | (1.03, 1.14) | 1.18 (0.02) | < 0.0001 | (1.15, 1.22) | |
| General Health | 0.99 (0.05) | 0.905 | (0.90, 1.10) | 1.02 (0.02) | 0.337 | (0.98, 1.06) | |
| Intercept | 0.05 (0.02) | < 0.0001 | (0.03, 0.09) | 0.03 (0.01) | < 0.0001 | (0.02, 0.05) | |
| Random Effects | Estimate | SE | |||||
| Race | |||||||
| var(γ) | 0.028 | 0.0068 | |||||
= Knowledge, Attitude and Belief scores were standardized over all men in the study
= Non-fathers were referent group
Table 2 provides results of the logistic regression comparing the odds of becoming an adolescent father compared to an adult father. Risky sexual behaviors were positively associated with the odds of becoming an adolescent father compared to an adult father with an increase in the odds ratio by 71% (OR=1.71, p<0.0001) for every one SD increase in risky sexual behaviors score. A single SD increase in the birth control self-efficacy score was associated with a 44% decrease in the odds ratio of becoming an adolescent father (OR=0.56, p=0.01).
Table 3 provides results of the multinomial logistic regression comparing the odds of becoming either a non-resident father or resident father compared to a non-father. A one SD higher risky sexual behavior score increased the odds ratio of becoming a nonresident father by 30% (OR=1.30, p-value<0.0001) and increased the odds ratio of becoming a resident father by 7% (OR=1.07, p-value=0.007). A single SD higher pregnancy attitudes score was related to an increase of 20% in the odds ratio of becoming a nonresident father (OR=1.20, p-value<0.0001) and an 11% increase in the odds ratio of becoming a resident father (OR=1.11, p-value<0.0001). A one unit SD higher birth control self-efficacy score was related to a decrease in the odds ratio of becoming a nonresident father by 28% (OR=0.72, p-value<0.0001), as might be expected, but it was not statistically significantly related with the odds of becoming a resident father (OR=0.93, p-value=0.75). The birth control attitudes scale was not statistically significant in predicting the odds of becoming either a nonresident father or resident father. Figure 1 provides bar plots of the estimates of becoming an adolescent father (comparison is to adult father), of becoming a non-resident father, and of becoming a resident father (comparison is to non-fathers.).
Figure 1.
Predicted Odds Ratios of Becoming an Adolescent Father, Non-resident Father, or Resident Father based on Knowledge, Attitudes and Beliefs Measured in Early Adolescence
Tables 2 and 3 also list the odds ratios of fatherhood status for the control variables. Mother’s education and own education decreased the odds of becoming an adolescent father (Table 2). When estimating the odds of becoming either a non-resident or resident father compared to a non-father, income level, employment status, marital status, and age were all positively related to the odds of becoming a resident father. However, only age was statistically significant among these variables when predicting the odds of becoming a nonresident father. Higher mother’s education decreased the odds of becoming a resident father but a higher personal education decreased the odds of becoming a nonresident father.
Discussion
In this study of associations between reproductive KAB and future fatherhood outcomes in a nationally representative sample, we find that several attitudes and beliefs identified during adolescence can predict both fatherhood and residency status in our sample of young adults up to age 34, after controlling for key variables such as age, income, race, maternal education, health, employment and marriage. Young men scoring higher on a risky sexual behavior scale during adolescence were more likely to become fathers of any type with a greater increase in odds for nonresident than resident father status and adolescent father status (<18 years) compared to adult father status. Similarly, men who had more positive attitudes towards pregnancy during adolescence were more likely to be fathers, with a greater increase in odds for nonresident father status. Greater birth control self-efficacy predicted lower odds of becoming a father overall but, if a father, more likely to be a resident father and more likely to be an adult father.
Adolescence is a key developmental period for reproductive KAB, and many health KAB and behaviors established during adolescence persist into adulthood. While past studies have identified how adolescent reproductive KAB affects initiation of sexual intercourse, contraceptive use, and pregnancy during adolescence, [5–8, 10, 20, 23, 24] these studies were unable to address how these KAB formed during adolescence impact pregnancy outcomes later in life for men. As many of these prior studies focus exclusively on women, [5–7] it is particularly important to investigate this relationship for men in order to better understand the paths leading to various fatherhood states. This study establishes that many of the KAB that are associated with adolescents’ sexual and contraceptive behavior during adolescence continue to be associated with their reproductive outcomes into young adulthood.
Examining certain KAB responses more closely, endorsement of risky sexual behavior and pregnancy attitudes had the strongest associations with becoming a father, and among fathers, a greater odds of being a nonresident father, while greater birth control self-efficacy decreased the odds of becoming a father at all, or if a father, it significantly decreased the odds of being a nonresident father. The first two associations are likely due to the fact that risky sexual behavior and ambivalent attitudes toward pregnancy may contribute to a higher risk of unplanned pregnancy. In turn, unplanned pregnancy puts men at higher risk for nonresident fatherhood, with its potential detrimental effects on father involvement, child academic performance, and child behavioral development. [29, 30] A similar explanation may be applicable to birth control self-efficacy, which was only statistically significant among nonresident fathers. Lower birth control self-efficacy may lead to greater unprotected sex, which is likely to result in an unplanned pregnancy and a nonresident father. Therefore, for men who become resident fathers, it may be that the pregnancy is more likely to be planned, and thus men who have the self-efficacy and confidence [10] to avoid unprotected sex may be choosing to become fathers with more intention. The lack of significance around the birth control attitudes score may reflect the deficit in knowledge among adolescents from certain regions in the US regarding birth control and the reproductive system in general [23, 39]. While birth control self-efficacy presupposes a confidence about the knowledge of using birth control successfully, attitudes towards birth control do not. Thus birth control attitudes may not be as useful an instrument for predicting fatherhood outcomes as self-efficacy.
The ability to identify young men during adolescence who have reproductive KAB that are predictive of non-optimal fatherhood paths has the potential to pave the way for more effective interventions. If those most at risk can be identified during adolescence, before they have entered fatherhood, educational programming and support can be provided that may change their reproductive trajectories, as has been shown in adolescent women.[31, 32] Programming and interventions for adolescent male reproductive health is an understudied and underdeveloped area and therefore the ideal form of such support is not evident.
As young men are historically the least likely to be engaged in the healthcare system, the first challenge may be finding and connecting with young males. One possibility is school-based teen clinics, which have successfully provided interventions for adolescent females, although no such positive results have been found thus far for adolescent men. [33] Clinics outside of a school setting specifically designed to target young men, such as the Young Men’s Clinic at New York-Presbyterian, [34] may also serve as a base from which to provide interventions. Community-based programming has proven effective in addressing HIV risk reduction, [35] and may be a useful approach for addressing men’s’ reproductive KAB.
Developmentally appropriate programs designed to engage young men as they are forming their reproductive KAB are essential. [18, 36, 37] One promising approach is preconception health care for men. [36, 38] Education surrounding reproductive KAB can be part of such care, and begin as early as adolescence. Although ideally these young men will not be entering fatherhood until later in the life-course, providing support during adolescence, especially to men at risk for entering fatherhood early or becoming nonresident fathers, may have a positive effect if and when these men do become fathers. Intervening early, especially before the entrance into fatherhood, can help identify risks to young men’s physical and mental health, resulting in a potentially healthier male, partner and fathers. [39]
Our study has limitations. First, although Add Health is a longitudinal study, the reproductive KAB survey was only administered at waves I and II and therefore changes in participants later KAB are unknown. Additionally, as a longitudinal study with 4 data collection time points, our data cannot begin to pinpoint the exact relationship between KAB, sexual behaviors, and timing of fatherhood. However, identifying associations between adolescent KAB endorsement and time to fatherhood is contingent upon first identifying associations between the two as we have shown. Second, fatherhood residency is constrained to one entry per participant so we cannot account for changes some fathers may have had between non-resident and resident fatherhood. Finally, due to study design and timing, our sample consists of younger fathers. However, resident fathers’ age of fatherhood entry, 25, is the same as the National Survey of Family Growth’s age at first birth for men.
CONCLUSION
Growing attention is being paid to the importance of including young men in sexual and reproductive health research across the life course and how KAB in adolescence lays a foundation for future outcomes. In this longitudinal, nationally-representative sample of young men followed from adolescences through young adulthood, we find that their adolescent reproductive KAB predict future fatherhood and residency status. Knowing which young men may be at-risk for early or nonresident fatherhood allows for innovative educational programs and public health interventions that focus on prevention for young men in adolescence.
Supplementary Material
Implications and Contributions.
Young men’s reproductive knowledge, attitudes, and beliefs during adolescence predict their future fatherhood status, timing, and residency. Earlier public health and educational interventions to identify at-risk young men may optimize fatherhood outcomes.
Acknowledgments
C.F.G acknowledges the support of grant K23HD060664 from the Eunice Kennedy Shriver National Institute of Child Health and Human Development in conducting this study.
The study sponsor had no role in study design; collection, analysis, and interpretation of data; writing the report; and the decision to submit the report for publication.
Abbreviations
- KAB
Knowledge, Attitudes, and Beliefs
- OR
odds ratio
- Add Health
National Longitudinal Study of Adolescent Health
- RR
response rate
- RSB
risky sexual behavior scale
- PA
pregnancy attitude scale
- BCSE
birth control self-efficacy scale
- BCA
birth control attitudes scale
- GLLAMM
generalized linear latent and mixed model
Footnotes
Publisher's Disclaimer: This is a PDF file of an unedited manuscript that has been accepted for publication. As a service to our customers we are providing this early version of the manuscript. The manuscript will undergo copyediting, typesetting, and review of the resulting proof before it is published in its final citable form. Please note that during the production process errors may be discovered which could affect the content, and all legal disclaimers that apply to the journal pertain.
Conflict of Interest (grants, institutional and corporate affiliations)
None of the authors have any real or perceived conflicts of interest to report.
Greg Duncan has no financial disclosures.
Sarah Peters has no financial disclosures.
Joshua Rutsohn has no financial disclosures.
Thomas W. McDade has no financial disclosures.
Emma K. Adam has no financial disclosures.
Rebekah Levine Coley has no financial disclosures.
P. Lindsay Chase-Lansdale has no financial disclosures.
References
- 1.Greene ME, Biddlecom AE. Absent and problematic men: Demographic accounts of male reproductive roles. Population and development review. 2000;26:81–115. [Google Scholar]
- 2.Gavin L, Moskosky S, Carter M, et al. Providing quality family planning services. MMWR. 2014;63:1–54. [PubMed] [Google Scholar]
- 3.Casey FE, Sonenstein FL, Astone NM, et al. Family Planning and Preconception Health Among Men in Their Mid-30s Developing Indicators and Describing Need. American Journal of Men's Health. 2014 doi: 10.1177/1557988314556670. Epub ahead of print. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Saewyc EM. What about the boys? The importance of including boys and young men in sexual and reproductive health research. J Adolesc Health. 2012;51:1–2. doi: 10.1016/j.jadohealth.2012.05.002. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Brückner H, Martin A, Bearman PS. Ambivalence and pregnancy: adolescents' attitudes, contraceptive use and pregnancy. Perspect Sex Reprod Health. 2004:248–257. doi: 10.1363/psrh.36.248.04. [DOI] [PubMed] [Google Scholar]
- 6.Jaccard J, Dodge T, Dittus P. Do adolescents want to avoid pregnancy? Attitudes toward pregnancy as predictors of pregnancy. J Adolesc Health. 2003;33:79–83. doi: 10.1016/s1054-139x(03)00134-4. [DOI] [PubMed] [Google Scholar]
- 7.Rocca CH, Harper CC, Raine-Bennett TR. Young women's perceptions of the benefits of childbearing: associations with contraceptive use and pregnancy. Perspect Sex Reprod Health. 2013;45:23–31. doi: 10.1363/4502313. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Cummings T, Auerswald CL, Ott MA. Factors Influencing Abstinence, Anticipation, and Delay of Sex Among Adolescent Boys in High–Sexually Transmitted Infection Prevalence Communities. J Adolesc Health. 2014;54:593–598. doi: 10.1016/j.jadohealth.2013.10.011. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Frost JJ, Lindberg LD, Finer LB. Young adults' contraceptive knowledge, norms and attitudes: associations with risk of unintended pregnancy. Perspect Sex Reprod Health. 2012;44:107–116. doi: 10.1363/4410712. [DOI] [PubMed] [Google Scholar]
- 10.Gloppen KM, David-Ferdon C, Bates J. Confidence as a predictor of sexual and reproductive health outcomes for youth. J Adolesc Health. 2010;46:S42–S58. doi: 10.1016/j.jadohealth.2009.11.216. [DOI] [PubMed] [Google Scholar]
- 11.Brooks-Gunn J, Furstenberg FF., Jr Adolescent sexual behavior. Am Psychol. 1989;44:249–257. [PubMed] [Google Scholar]
- 12.Castillo J, Welch G, Sarver C. Fathering: The Relationship Between Fathers’ Residence, Fathers’ Sociodemographic Characteristics, and Father Involvement. Matern Child Health J. 2011;15:1342–1349. doi: 10.1007/s10995-010-0684-6. [DOI] [PubMed] [Google Scholar]
- 13.Sorensen E, Zibman C. Getting to know poor fathers who do not pay child support. Soc Serv Rev. 2001;75:420–434. [Google Scholar]
- 14.Carlson MJ, McLanahan SS, Brooks-Gunn J. Coparenting and nonresident fathers' involvement with young children after a nonmarital birth. Demography. 2008;45:461–488. doi: 10.1353/dem.0.0007. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Cheadle JE, Amato PR, King V. Patterns of nonresident father contact. Demography. 2010;47:205–225. doi: 10.1353/dem.0.0084. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Adamsons K, Johnson SK. An updated and expanded meta-analysis of nonresident fathering and child well-being. J Fam Psychol. 2013;27:589. doi: 10.1037/a0033786. [DOI] [PubMed] [Google Scholar]
- 17.Marsiglio W. Young nonresident biological fathers. Marriage Fam Rev. 1994;20:325–348. [Google Scholar]
- 18.Kirby D, Answers E. Research findings on programs to reduce teen pregnancy and sexually transmitted diseases. Washington, DC: National Campaign to Prevent Teen and Unplanned Pregnancy; 2007. [Google Scholar]
- 19.Udry JR. National Longitudinal Study of Adolescent Health. [Accessed September 10 2015];References, instruments, and questionnaires consulted in the development of the Add Health in-home adolescent interview. Available at: http://www.cpc.unc.edu/projects/addhealth/data/guides/refer.pdf. [Google Scholar]
- 20.Henry DB, Deptula DP, Schoeny ME. Sexually transmitted infections and unintended pregnancy: A longitudinal analysis of risk transmission through friends and attitudes. Soc Dev. 2012;21:195–214. doi: 10.1111/j.1467-9507.2011.00626.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21.Henry DB, Schoeny ME, Deptula DP, et al. Peer selection and socialization effects on adolescent intercourse without a condom and attitudes about the costs of sex. Child Dev. 2007;78:825–838. doi: 10.1111/j.1467-8624.2007.01035.x. [DOI] [PubMed] [Google Scholar]
- 22.Rostosky SS, Regnerus MD, Wright MLC. Coital debut: The role of religiosity and sex attitudes in the Add Health Survey. J Sex Res. 2003;40:358–367. doi: 10.1080/00224490209552202. [DOI] [PubMed] [Google Scholar]
- 23.Ryan S, Franzetta K, Manlove J. Knowledge, perceptions, and motivations for contraception: influence on teens' contraceptive consistency. Youth Soc. 2007 [Google Scholar]
- 24.Shneyderman Y, Schwartz SJ. Contextual and intrapersonal predictors of adolescent risky sexual behavior and outcomes. Health Educ Behav. 2013;40:400–414. doi: 10.1177/1090198112447800. [DOI] [PubMed] [Google Scholar]
- 25.Kao T-SA, Manczak M. Family influences on adolescents’ birth control and condom use, likelihood of sexually transmitted infections. J Sch Nurs. 2013;29:61–70. doi: 10.1177/1059840512444134. [DOI] [PubMed] [Google Scholar]
- 26.Skrondal A, Rabe-Hesketh S. Generalized latent variable modeling: Multilevel, longitudinal, and structural equation models. Boca Raton, GL: Chapman and Hall/CRC Press; 2004. [Google Scholar]
- 27.White IR, Royston P, Wood AM. Multiple imputation using chained equations: issues and guidance for practice. Stat Med. 2011;30:377–399. doi: 10.1002/sim.4067. [DOI] [PubMed] [Google Scholar]
- 28.Kline P. A handbook of test construction: Introduction to psychometric design: Methuen. 1986 [Google Scholar]
- 29.Choi J-K. Nonresident fathers’ parenting, family processes, and children’s development in urban, poor, single-mother families. Soc Serv Rev. 2010;84:655–677. doi: 10.1086/657422. [DOI] [PubMed] [Google Scholar]
- 30.Magnuson K, Berger LM. Family structure states and transitions: associations with children's well-being during middle childhood. J Marriage Fam. 2009;71:575–591. doi: 10.1111/j.1741-3737.2009.00620.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 31.Guse K, Levine D, Martins S, et al. Interventions using new digital media to improve adolescent sexual health: a systematic review. J Adolesc Health. 2012;51:535–543. doi: 10.1016/j.jadohealth.2012.03.014. [DOI] [PubMed] [Google Scholar]
- 32.Morrison-Beedy D, Jones SH, Xia Y, et al. Reducing sexual risk behavior in adolescent girls: results from a randomized controlled trial. J Adolesc Health. 2013;52:314–321. doi: 10.1016/j.jadohealth.2012.07.005. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 33.Dittus PJ, De Rosa CJ, Jeffries RA, et al. The Project Connect Health Systems Intervention: Linking Sexually Experienced Youth to Sexual and Reproductive Health Care. J Adolesc Health. 2014;55:528–534. doi: 10.1016/j.jadohealth.2014.04.005. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 34.Young Men's Health Initiative (YMHI) Young Men's Clinic. [Accessed September 1 2015]; Available at: http://www.youngmensclinic.org/ [Google Scholar]
- 35.Wilson TE, Fraser-White M, Williams KM, et al. Barbershop Talk With Brothers: Using Community-Based Participatory Research to Develop and Pilot Test a Program to Reduce HIV Risk Among Black Heterosexual Men. AIDS Educ Prev. 2014;26:383. doi: 10.1521/aeap.2014.26.5.383. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 36.Frey KA, Navarro SM, Kotelchuck M, et al. The clinical content of preconception care: preconception care for men. Am J Obstet Gynecol. 2008;199:S389–S395. doi: 10.1016/j.ajog.2008.10.024. [DOI] [PubMed] [Google Scholar]
- 37.Ott MA. Examining the development and sexual behavior of adolescent males. J Adolesc Health. 2010;46:S3–S11. doi: 10.1016/j.jadohealth.2010.01.017. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 38.Centers for Disease Control and Prevention. Preconception Health and Health Care: Information for Men. [Accessed September 1 2015]; Available at: http://www.cdc.gov/preconception/men.html.
- 39.Kohler PK, Manhart LE, Lafferty WE. Abstinence-only and comprehensive sex education and the initiation of sexual activity and teen pregnancy. Journal of Adolescent Health. 2008 Apr 30;42(4):344–351. doi: 10.1016/j.jadohealth.2007.08.026. [DOI] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.