Abstract
Inflammatory bowel disease is a risk factor for colorectal cancer (CRC) initiation and development. In this study the effects of American ginseng on chemically-induced colitis and colon carcinogenesis were evaluated using an azoxymethane (AOM)/dextran sulfate sodium (DSS) mouse model. During the acute phase on day 15, the oral administration of ginseng (15 and 30 mg/kg/day) significantly suppressed AOM/DSS-induced colitis, as demonstrated by the disease activity index and colon tissue histology. During the chronic phase in week 13, AOM/DSS-induced tumor multiplicity was significantly suppressed by ginseng. Ginseng significantly attenuated the increase of inflammatory cytokines such as IL-1α, IL-1β, IL-6, G-CSF and GM-CSF. Serum metabolomics data in the PCA plots showed good separation between the AOM/DSS model and ginseng-treated mice, and the most important endogenous metabolite changes were identified. The 16S rRNA data showed that after AOM/DSS, the microbiome community in the model group was obviously changed, and ginseng inhibited these changes. Fecal metabolomics analysis supported these findings. In conclusion, oral ginseng significantly decreased AOM/DSS-induced colitis and colon carcinogenesis by inhibiting inflammatory cytokines, and restoring the metabolomic and microbiota profiles accordingly. Selective endogenous small molecules could be used as biomarkers to elucidate the effects of ginseng treatment.
Keywords: Inflammatory bowel disease, colitis, cancer, American ginseng, Panax quinquefolius, metabolites, intestinal microbiome, metabolomics, AOM/DSS model
Introduction
Colorectal cancer (CRC) is one of the most common malignancies in the world (1, 2). Ulcerative colitis is a risk factor for CRC initiation and development (3, 4). Previous studies have provided evidence that anti-inflammatory phytochemicals possess unique modes of action against CRC (5, 6). In this regard, identifying botanical sources as an alternative strategy to develop better prevention and treatment options could be an effective step in advancing the management of CRC.
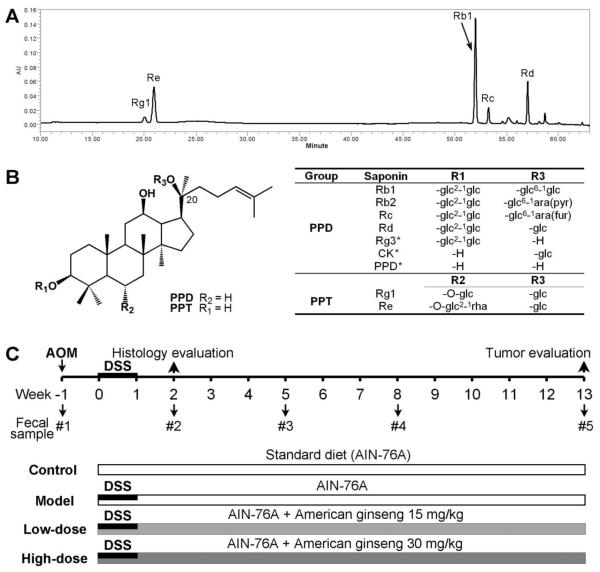
American ginseng (Panax quinquefolius L.) is a very commonly used herbal medicine in the U.S., and ginsenosides are considered to be its bioactive constituents (Fig. 1A and B) (7-9). As an anti-inflammatory botanical, ginseng plays a therapeutic role in reducing inflammation and suppressing colitis (10, 11). Interestingly, epidemiological and experimental studies have suggested that ginseng can prevent or treat cancer in humans, including CRC (6, 12, 13). Thus, the anti-inflammatory activity of ginseng may play a critical role in CRC chemoprevention (10, 11).
Figure 1.
Phytochemical analysis and experimental protocol. (A) HPLC chromatogram of American ginseng extract recorded at 202 nm. Five major ginsenoside peaks are shown. (B) Chemical structures of ginsenosides fall into two groups: protopanaxatriols (PPT) and protopanaxadiols (PPD). *, Ginsenoside metabolites, Rg3, CK (compound K), and PPD (protopanaxadiol). (C) Experimental scheme for the mice with AOM/DSS-induced colitis and colon carcinogenesis. All the A/J mice received a standard diet (AIN-76A) and were assigned to four groups: Control, normal control; Model, AOM/DSS only; Low-dose, AOM/DSS plus low-dose oral American ginseng (15 mg/kg/day); High-dose, AOM/DSS plus high-dose oral American ginseng (30 mg/kg/day).
Ginseng’s bioavailability after its oral ingestion is low, due to the incomplete absorption of the parent compound and conversion to metabolites (14, 15). The ingested parent ginseng compounds can be biotransformed to metabolites by the enteric microbiome (16, 17). Although host-microbial interactions in the mammalian colon are complex and incompletely understood, they play an important role in maintaining intestinal homeostasis and protecting colorectal carcinogenesis (18). Therefore, the study of the shift of gut microbiota community induced by ginseng may provide new information on CRC management. However, the effects of ginseng compounds on gut microbial species have yet to be investigated in an in vivo CRC model.
In this study, an azoxymethane (AOM)/dextran sulfate sodium (DSS) mouse model was used to evaluate the effects of American ginseng on attenuating colitis and colon carcinogenesis. A metabolomic analysis (19, 20) was conducted to detect endogenous metabolite changes for potential biomarkers. In addition, the enteric microbiota population changes induced by ginseng in the context of its treatment were also characterized using a 16S rRNA gene-based analysis.
Materials and Methods
Plant materials, extraction and analysis
The root of P. quinquefolius L. was collected from Roland Ginseng Limited Liability Company (Wausau, WI). The voucher specimen was authenticated and deposited at the Tang Center for Herbal Medicine Research at the University of Chicago. Ginseng extraction and HPLC analysis were conducted (21, 22).
Animals and experimental protocols
The experimental protocols were approved by the Institutional Animal Care and Use Committee of the University of Chicago. Approximately 6-week old male A/J mice, weighing between 18 and 22 g, were obtained from Jackson Laboratories (Bar Harbor, ME).
As shown in Fig. 1C, animals were separated into 4 groups (n = 10 per group): the normal control or control group, the AOM/DSS model or model group, the American ginseng low dose (15 mg/kg/day) or AG 15 group, and the high dose (30 mg/kg/day) or AG 30 group. Except for animals in the control group, all animals initially received a single intraperitoneal injection of AOM (7.5 mg/kg), and one week after the AOM injection (set as Day 1), the animals began receiving 2.5% DSS in drinking water for 8 consecutive days. Animals in the model group received only AOM/DSS without any ginseng. The ginseng group animals received American ginseng extract at 110 or 220 ppm in standard AIN-76A chow from Day 1 to Week 13. We calculated that the daily dose of ginseng was approximately 15 and 30 mg/kg/day, respectively. In addition, for the acute phase observation, five animals per group were sacrificed on Day 15. The remaining five animals were kept in the chronic phase and were sacrificed at the end of Week 13. The serum and gut tissue samples of all animals were collected. The stool samples were collected during Weeks -1, 2, 5, 8 and 13.
Disease activity index and histological assessment
AOM/DSS induced colitis was scored on the disease activity index (DAI) in the acute phase, as described previously (23). Paraffin-embedded gut tissue samples were serially sectioned, and some sections were stained with hematoxylin and eosin (H&E). The stained sections were subsequently examined for histopathological changes by a gastrointestinal pathologist.
RNA extraction and quantitative real-time PCR
Total RNA was isolated from the mouse colonic tissue using the miRNeasy kit (Qiagen, Valencia, CA). First strand cDNA was synthesized using a Maxima™ First Strand cDNA Synthesis Kit (Thermo Scientific, Waltham, MA). Quantitative real-time PCR was performed on a 7900HT RT-qPCR system (Applied Biosystems, Foster City, CA). The primers used for real-time PCR were described previously (24, 25). β-actin was used as an endogenous control.
Enzyme-linked immunosorbent analysis (ELISA)
Proteins of the mouse colonic tissue were extracted with RIPA lysis buffer (Thermo Scientific, Waltham, MA). The levels of cytokines IL-1β and IL-6 were quantified by ELISA (Life Technologies, Grand Island, NY) (24).
Metabolomic analysis using GC/TOF-MS
Serum and stool samples were pretreated with different solvents and derivatization reagents (24, 26). GC/MS analyses were performed on an Agilent 7890N gas chromatograph coupled with a Pegasus HT time-of-flight mass spectrometer (Leco Corporation, St Joseph, MI) (24). Metabolomic data were analyzed using principle component analysis (PCA). The differential metabolites were selected when they met the requirements of variable importance in the projection (VIP) > 1 in the OPLS model. Compared to the control, the corresponding fold change was calculated and the most changed small molecules were identified (24).
Fecal microbiota terminal-restriction fragment length polymorphism (T-RFLP) analysis
Fecal samples were mixed and homogenized in 1 ml extraction buffer. Standard DNA extraction with phenol:chloroform:isoamyl alcohol and precipitation with ethanol was performed (27). 16S rRNA gene sequences were amplified from DNA templates using broad-range primers 8F (5′-AGAGTT TGATCCTGGCTCAG-3′) labeled with 6′ carboxyfluorescein (6-FAM) and 1492R (5′-GGTTACCTTGTTACGACTT-3′) for the bacterial domain. Aliquots of purified PCR products were digested by Msp I (New England Biolabs, Ipswich, MA) and subsequently were subjected to capillary electrophoresis using the DNA sequencer 3130 (Applied Biosystems, Foster City, CA) (26). PCA plots were generated using fluorescently labeled 5’-terminal restriction fragments (28).
Fecal 16S rRNA sequencing-based phylogenetic analysis
The 16S rRNA gene sequencing was performed by an Illumia MiSeq DNA sequencer at the Argonne National Laboratory (Lemont, IL) (28). Raw sequence data were processed with the QIIME toolkit. Using the QIIME wrappers, OTUs were picked at 97% sequence identity using cdhit and a representative sequence was then chosen for each OTU by selecting the most abundant sequence in that OTU. The RDP classifier analysis was used to assign 16S rRNA sequences to the taxonomical hierarchy at the phylum level (29).
Statistical analysis
All data were expressed as mean ± S.D. A student's t-test and a one-way ANOVA were used to test the significance of the differences between ginseng treatment and model groups. The statistical significance was set at P < 0.05.
Results
Phytochemical analysis of American ginseng
The HPLC chromatogram of American ginseng extract is shown in Fig. 1A. The chemical structures of the major ginsenosides are shown in Fig. 1B. The ginsenoside content ratio of the protopanaxatriol group to the protopanaxadiol group was 1:2.8. The contents of ginsenosides Rb1, Rc, Rd, Rg1 and Re were 28.1%, 4.5%, 8.6%, 1.7% and 13.1%, respectively. Compound K (CK), ginsenoside Rg3 and protopanaxadiol (PPD) are the major metabolites transformed by the intestinal microbiota (Figs. 1B and 6) (15, 17).
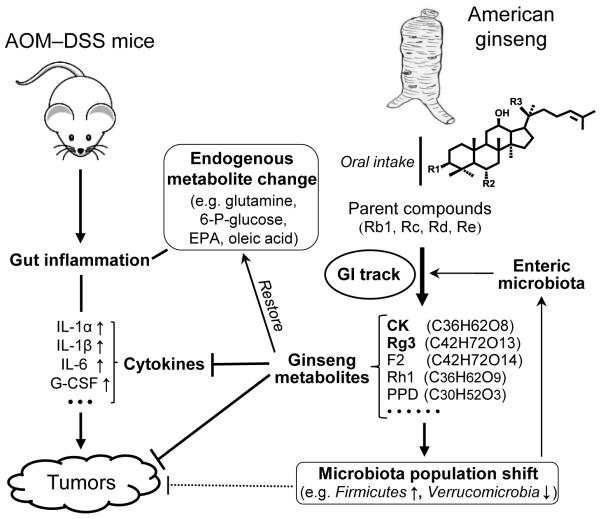
Figure 6.
Schematic diagram of American ginseng on AOM/DSS-induced colon cancer. The effects of ginseng metabolites can be measured by the decreased gut cytokine levels and tumor multiplicity, supported by the shift of the microbiota population and the restoration of endogenous metabolite levels.
Ginseng attenuated AOM/DSS-induced acute colitis
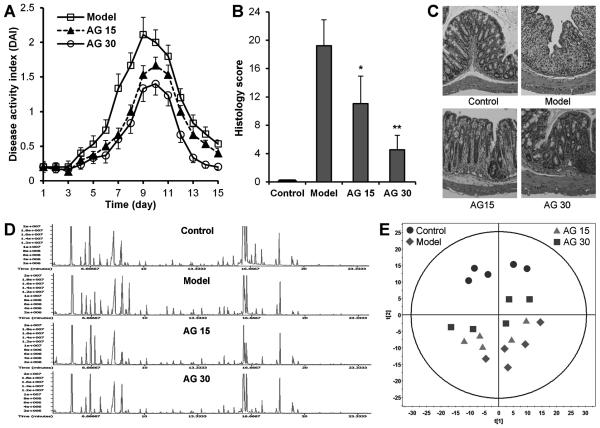
After AOM/DSS administration, animals in the model group showed apparent diarrhea and rectal bleeding starting on Day 4. As the treatment continued, the presence and development of inflammation was clearly demonstrated. The disease severity, scored by DAI, reached the highest level on Day 9. Fig. 2A shows the effects of American ginseng on the inflammation, which resulted in the reduction of the DAI score in a dose-related manner (P < 0.01).
Figure 2.
Effects of American ginseng on acute experimental colitis. (A) Ginseng attenuated AOM/DSS-induced colitis, expressed in disease activity index (DAI). Data from the control group were all set zeros from Day 1 to Day 15. (B-C) Effects of ginseng on the histological characterization in AOM/DSS-induced colitis. Colon samples were collected on Day 15. (B) Overall histology scores in different groups. *, P < 0.05; **, P < 0.01 compared to the model group. (C) Representative H&E staining histological sections in different groups. (D-E) Metabolomic analysis of animal serum samples on Day 15. (D) Representative total ion chromatograms (TIC) from GC/MS analysis. (E) Metabolic profiling of serum samples. Principal components analysis (PCA) score plot. Model, AOM+DSS; AG, American ginseng; AG 15, AOM+DSS+AG (15 mg/kg/day); AG 30, AOM+DSS+AG (30 mg/kg/day).
Histological H&E staining of the colon tissue from model animals showed severe inflammatory lesions, supported by the significant and complete loss of crypts, surface erosion with exuberant inflammatory exudate, patchy re-epithelization, lamina propria fibrosis with acute and chronic inflammatory infiltrate, and submucosa edema and mixed inflammatory cell infiltration. In the ginseng groups, there was a significant reduction in colon inflammation. This reduction was particularly evident in the high-dose group because the serosa colon tissue had mild inflammation, the mucosa had tightly packed glands with a normal amount of goblet cells, the lamina propria showed patchy neutrophilic infiltrate which extended into the submucosa, and the serosa was normal. The overall histology scores and representative H&E staining histological sections are shown in Fig. 2B and C.
Ginseng changed the serum endogenous metabolite profile in acute colitis mice
The typical GC/MS total ion current (TIC) chromatograms of serum samples from the control, model, and two ginseng groups on Day 15 are shown in Fig. 2D. Visual inspection of the GC/MS spectra revealed obvious differences between the four groups.
Multivariate analyses were performed to reduce the data to a low dimensional space where discrimination of metabolomic profiles between the groups was possible. A number of 228 metabolites were annotated in the Day 15 serum samples. All 20 samples from the four experimental groups were analyzed with an unsupervised PCA model. A clear separation tendency can be observed in the scores plot (2 components, R2X = 0.579) with no outliers (Fig. 2E). Using the second component, we were able to find the separation between these four groups, with the control group having the highest scores, the model group having the lowest scores, and ginseng-treated mice having scores in between these two groups in a dose-related manner.
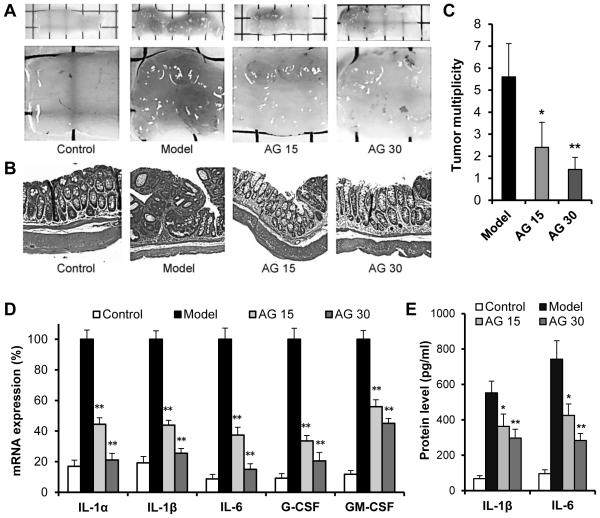
Ginseng decreased colon carcinogenesis and chronic colitis
AOM/DSS induced tumor multiplicity was evaluated on Week 13. No tumors were detected in the control group. Tumors or adenocarcinomas were detected in model and ginseng groups (incidence = 100%). The representative macroscopic morphology for the control, model and two ginseng groups are shown in Fig. 3A. Obvious carcinogenesis was observed in the model group. In contrast, the tumors were both fewer in number and smaller in size in both ginseng groups. The representative histological H&E staining sections of the four groups are shown in Fig. 3B. Tumor multiplicity data are shown in Fig. 3C. Compared to the model group, ginseng treatment significantly and dose dependently reduced tumor numbers (P < 0.05 and P < 0.01, respectively).
Figure 3.
Effects of American ginseng on AOM/DSS-induced colon carcinogenesis and chronic colitis. Colon tissue was collected at the end of week 13. (A) Representative macroscopic morphology of the whole colon (upper panel) and tumors (lower panel). (B) Representative microscopic H&E staining sections. (C) Colon tumor multiplicity was reduced significantly in the two ginseng groups in a dose-related manner. (D) Expression of inflammatory cytokine genes in colon tissues assayed by real-time PCR. (E) Expression of inflammatory cytokines assayed by ELISA. Model, AOM+DSS; AG, American ginseng; AG 15, AOM+DSS+AG (15 mg/kg/day); AG 30, AOM+DSS+AG (30 mg/kg/day). *, P < 0.05 and **, P < 0.01 compared to the model group.
The effects of American ginseng on the expression of inflammatory cytokines were examined in normal colon tissue on Week 13. Real-time PCR data showed that the expression of 5 inflammatory cytokines (IL-1α, IL-1β, IL-6, G-CSF and GM-CSF) in the model group was significantly higher than it was in the control group (all P < 0.001). Based on the differences between the control group and ginseng group, it can be concluded that ginseng treatment significantly decreased the expression of these inflammatory cytokines in a dose-dependent manner (all P < 0.01) (Fig. 3D). An ELISA assay showed that compared to the model group, the levels of IL-1β and IL-6 in the colonic tissue were downregulated (P < 0.05 and P < 0.01) (Fig. 3E), which is consistent with the real-time PCR data.
Serum endogenous metabolite profile changes
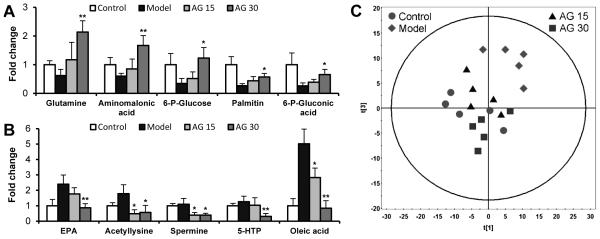
In the chronic phase, 208 metabolites were annotated in the serum samples, of which 103 metabolites were detected to be differentially expressed in the model group compared to the control group, including amino acids, lipids and carbohydrates. Compared to the model group, the most obvious differences in metabolites in the ginseng groups are shown in Fig. 4A and B. The PCA showed a clear separation between samples from the model and control group (PC1 and PC2, 2 components, R2X = 0.696, Fig. 4C). Good separations were also obtained in the PCA plot between model mice and ginseng treated mice, and the high-dose ginseng group was closer to that of the control group.
Figure 4.
Metabolomic analysis of serum samples in Week 13. (A-B) The top 10 metabolites responsible for the separation between the model and ginseng groups. (A) Top five upregulated metabolites. (B) Top five downregulated metabolites. EPA, 5,8,11,14,17-eicosapentaenoic acid; 5-HTP, 5-hydroxy-L-tryptophan; oleic acid, 9-octadecenoate. Ordinate values are peak area ratios, i.e., relative concentrations (peak area of each groups/peak area of control group) of each metabolite. (C) Metabolic profiling of serum samples. Principal components analysis (PCA) score plot showing data from different groups. Model, AOM+DSS; AG, American ginseng; AG 15, AOM+DSS+AG (15 mg/kg/day); AG 30, AOM+DSS+AG (30 mg/kg/day). *, P< 0.05 and ** P< 0.01 compared to the model group.
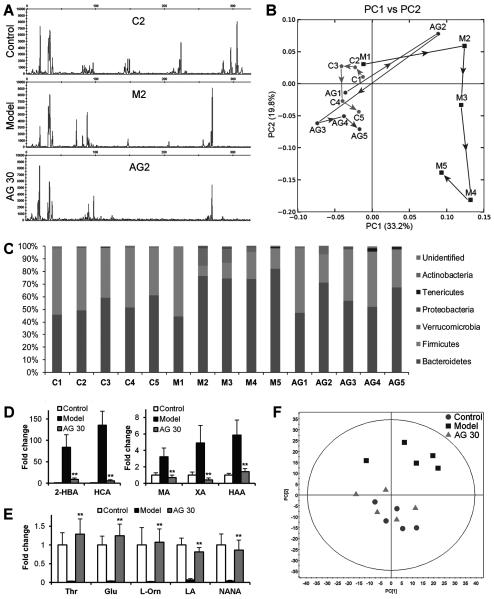
Effects of ginseng on intestinal microbiome populations
Fecal samples were examined by T-RFLP analysis. As shown in Fig. 5A, on Week 2, remarkable differences in T-RFLP profiles were observed between the control group and the other groups. The changes in the fecal microbiota profile over time (Week 1 through Week 13) were analyzed using PCA of T-RFLPs. As shown in Fig. 5B, the plots of the model group are far away from those of the control group after AOM/DSS. From Week 5 to Week 13, the plots of the ginseng group were very close to those of the control group.
Figure 5.
Microbiota and metabolomic analyses of stool samples. (A-C) Effects of American ginseng on the structure of intestinal microbiota. (A) Representative T-RFLP chromatograms from different-sized bacterioplankton populations. (B) T-RFLP-based PCA profiles showing differences in the microbiota profile. (C) Taxonomic composition of the microbiota at the phylum level identified by high-throughput 16S rRNA gene sequencing. C, control; M, model; and AG, American ginseng 30 mg/kg/day. Number 1, 2, 3, 4 and 5 in the x-axis indicate Weeks -1, 2, 5, 8 and 13, respectively. (D-F) Metabolomic analysis of samples in Week 13. (D-E) The top 10 metabolites responsible for the separation between the model and ginseng groups. (D) Five downregulated metabolites. 2-HBA, 2-hydroxybutanoic acid; HCA, hydrocinnamic acid; MA, malic acid; XA, xanthurenic acid; HAA, hydroxyacetic acid. (E) Five upregulated metabolites. Thr, threonine; Glu, glutamate; L-Orn, L-ornithine; LA, linolenic acid; NANA, N-acetylneuraminic acid. (F) Metabolic profiling of stool samples. Principal components analysis (PCA) score plot showing data from different groups. ** P < 0.01 compared to the model group.
To analyze specific bacterial phylotypes, 16S rRNA gene clone libraries were established and sequenced. The majority of sequences were classified into two phyla, Firmicutes and Bacteroidetes. Among the different groups, a relatively stable composition was observed in the normal control group. However, there was a clear difference in the model group after AOM/DSS, with significantly increased levels of Bacteroidetes and Verrucomicrobia, and decreased levels of Firmicutes. In contrast, after treatment, although the proportion of Firmicutes was somewhat reduced at Week 2, this level was quickly increased, while the levels of Bacteroidetes and Verrucomicrobia were decreased (Fig. 5C). This result supported our T-RLFP data, in which AOM/DSS significantly changed the intestinal microbiota populations. Ginseng treatment restored the gut microbiota communities to compositions resembling those of the healthy control group.
Fecal metabolite profile changes
To investigate whether the metabolic variations were associated with ginseng, fecal metabolites were analyzed. A total of 493 metabolites were annotated in the Week 13 fecal samples. The most obvious differences in metabolites between the model and ginseng groups are shown in Fig. 5D and E. Clear separations were obtained between samples collected from the model and ginseng groups in the PCA scores plot (2 components, R2X = 0.684), while plots of the ginseng group were close to those of the control group (Fig. 5F). These results are consistent with the above microbiota community data.
Discussion
As a commonly used herbal medicine, ginseng has many reported health benefits, including cancer prevention (30). We previously observed that after oral administration, parent ginseng compounds were biotransformed by the enteric microbiome to metabolites such as Rg3, Rh1, CK and PPD (16, 17). We have also shown that these ginseng metabolites have potential anticancer effects on CRC (31-33). In this study, we evaluated the effects of oral American ginseng on AOM/DSS-induced colitis and colorectal carcinogenesis, and the subsequent changes in metabolomics and gut microbiota profiles. The ginseng was added to the rodent chow for better dose titration.
In the acute phase, chemically-induced colitis was significantly reduced by ginseng in a dose-dependent manner, which was supported by histology evaluation. In the chronic phase, obvious colon carcinogenesis was observed in the model group. Ginseng treatment significantly reduced colon tumor multiplicity, consistent with pro-inflammatory cytokine level changes. Our results suggested that ginseng attenuated the colitis and colon carcinogenesis in part via the depression of pro-inflammation (Fig. 6).
Metabolomic fingerprinting is the systematic and unbiased study of small endogenous metabolites (34). In the acute colitis phase, serum metabolomic analysis showed that the plots of the model group were clearly separated from the normal control group, while ginseng treatment, especially in high-dose group, pushed the plots back towards the control group (Fig. 2E). In the chronic phase, our data suggested that in the model group, the levels of several key endogenous metabolites were significantly up- or downregulated. Compared to the model group, the levels of the most-regulated metabolites were close to those of the normal control group, indicating beneficial effects of this herbal medicine. As an amino acid source, glutamine played an important role in colonocyte nutrition and integrity (35). Glutamine could inhibit colonic inflammation through the downregulation of IL-8 and TNF-α expressions (36). The ginseng-mediated increase in the glutamine level was likely linked to the inhibition of AOM/DSS-induced acute and chronic inflammation. Further, glutamine synthetase played an essential role in the metabolism of nitrogen by catalyzing the condensation of glutamate and ammonia to form glutamine. Recently, a new mechanism of tumor growth regulation by glutamine synthetase has been reported, in which the overexpression of glutamine synthetase resulted in tumor cell growth arrest and motility suppression via activation of the expression of p21 and cyclin D1 (37). In the model group animals, since the integrity of the colon was damaged, the gut tissue glutamine level was significantly lower than that of the control. Ginseng-treated animals reversed this glutamine level reduction, suggesting ginseng’s effects on inflammation and carcinogenesis. In addition,an inflammation-associated increased energy consumption was observed, including reduced levels of 6-P-glucose and 6-P-gluconic acid, and increased levels of lipids, such as EPA and oleic acid. Ginseng appears to restore the levels of observed key endogenous metabolites.
Bacteria are an important component of the human body (38). We previously observed that intestinal microbiota are critical for the conversion of ginseng metabolites (16, 17), and these metabolites showed significant antitumor potential (8, 32). In this study, we observed that the intestinal microbiome community underwent obvious changes after ginseng administration, including increases in Firmicutes and decreases in Bacteroidales and Verrucomicrobia. It was reported that certain Gram-negative phyla (e.g., Bacteroidales and Verrucomicrobia) promote tumorigenesis while certain Gram-positive phyla (e.g., Firmicutes) have anti-inflammatory and anti-tumorigenic properties (18, 39). We observed that ginseng treatment effectively restored the enteric microbiome community to a healthy state, and protected against pathological processes (Fig. 6).
Fecal metabolomic analysis showed that the composition of fecal metabolites in the model group was different from that in the control. In ginseng group, the composition was very similar to that of the normal control. A recent report revealed that the content of several compounds, including malic acid and 3-hydroxybutanoic acid, was significantly higher in tumor tissue compared to normal tissue (40). In our study, very high concentrations of malic acid and 2-hydroxybutanoic acid were also observed in the stool samples of the model group, which may have enhanced carcinogenesis. As expected, the contents of these two compounds were decreased very significantly after ginseng administration. In addition, it was found that linolenic acid possess anti-tumorigenesis potential via gut mucosa protection and pro-inflammatory cytokine inhibition (41). In the stool samples, AOM/DSS very significantly decreased the level of linolenic acid, while its level was restored by ginseng. Fecal metabolomic results suggested that ginseng treatment may have an ability to maintain healthy communities and functions of intestinal microbiota.
In this study, we observed that American ginseng significantly attenuated AOM/DSS-induced colitis and colon carcinogenesis, which was linked to the inhibition of inflammatory cytokines. We used a platform combining metabolomic and microbiome data to interpret the efficacies of ginseng, and our data showed that along with anticancer effects, ginseng also changed the metabolomic and microbiota profiles accordingly. With further verification, selective endogenous small molecules could be used as biomarkers to elucidate the effects of ginseng on colitis-associated CRC. Data from this study suggest that American ginseng compounds may have potential value in CRC chemoprevention.
Acknowledgments
Financial Support: This work was supported in part by the NIH/NCCAM grants P01 AT 004418 (C.S. Yuan) and K01 AT005362 (C.Z. Wang).
Footnotes
Conflict of Interest: The authors declare no conflict of interest.
References
- 1.Siegel RL, Miller KD, Jemal A. Cancer statistics, 2016. CA Cancer J Clin. 2016;66:7–30. doi: 10.3322/caac.21332. [DOI] [PubMed] [Google Scholar]
- 2.Zhang L, Ren XY, Alt E, Bai XW, Huang SY, Xu ZM, et al. Chemoprevention of colorectal cancer by targeting APC-deficient cells for apoptosis. Nature. 2010;464:1058–61. doi: 10.1038/nature08871. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Aggarwal BB, Van Kuiken, Iyer LH, Harikumar KB, Sung B. Molecular targets of nutraceuticals derived from dietary spices: potential role in suppression of inflammation and tumorigenesis. Exp Biol Med. 2009;234:825–49. doi: 10.3181/0902-MR-78. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.McCarthy N. Tumorigenesis: All together now. Nat Rev Cancer. 2013;13:148–9. doi: 10.1038/nrc3469. [DOI] [PubMed] [Google Scholar]
- 5.Madka V, Rao CV. Anti-inflammatory phytochemicals for chemoprevention of colon cancer. Curr Cancer Drug Targets. 2013;13:542–57. doi: 10.2174/15680096113139990036. [DOI] [PubMed] [Google Scholar]
- 6.Yun TK. Panax ginseng--a non-organ-specific cancer preventive? Lancet Oncol. 2001;2:49–55. doi: 10.1016/S1470-2045(00)00196-0. [DOI] [PubMed] [Google Scholar]
- 7.Qi LW, Wang CZ, Yuan CS. Isolation and analysis of ginseng: advances and challenges. Nat Prod Rep. 2011;28:467–95. doi: 10.1039/c0np00057d. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Qi LW, Wang CZ, Yuan CS. Ginsenosides from American ginseng: chemical and pharmacological diversity. Phytochemistry. 2011;72:689–99. doi: 10.1016/j.phytochem.2011.02.012. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Park EY, Kim MH, Kim EH, Lee EK, Park IS, Yang DC, et al. Efficacy comparison of Korean ginseng and American ginseng on body temperature and metabolic parameters. Am J Chin Med. 2014;42:173–87. doi: 10.1142/S0192415X14500128. [DOI] [PubMed] [Google Scholar]
- 10.Hofseth LJ, Wargovich MJ. Inflammation, cancer, and targets of ginseng. J Nutr. 2007;137:183S–5S. doi: 10.1093/jn/137.1.183S. [DOI] [PubMed] [Google Scholar]
- 11.Jin Y, Hofseth AB, Cui X, Windust AJ, Poudyal D, Chumanevich AA, et al. American ginseng suppresses colitis through p53-mediated apoptosis of inflammatory cells. Cancer Prev Res. 2010;3:339–47. doi: 10.1158/1940-6207.CAPR-09-0116. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Yun TK, Choi SY. Preventive effect of ginseng intake against various human cancers: a case-control study on 1987 pairs. Cancer Epidemiol Biomarkers Prev. 1995;4:401–8. [PubMed] [Google Scholar]
- 13.Wang CZ, Zhang Z, Anderson S, Yuan CS. Natural products and chemotherapeutic agents on cancer: prevention vs. treatment. Am J Chin Med. 2014;42:1555–8. doi: 10.1142/S0192415X1420002X. [DOI] [PubMed] [Google Scholar]
- 14.Bae EA, Park SY, Kim DH. Constitutive beta-glucosidases hydrolyzing ginsenoside Rb1 and Rb2 from human intestinal bacteria. Biol Pharm Bull. 2000;23:1481–5. doi: 10.1248/bpb.23.1481. [DOI] [PubMed] [Google Scholar]
- 15.Tawab MA, Bahr U, Karas M, Wurglics M, Schubert-Zsilavecz M. Degradation of ginsenosides in humans after oral administration. Drug Metab Dispos. 2003;31:1065–71. doi: 10.1124/dmd.31.8.1065. [DOI] [PubMed] [Google Scholar]
- 16.Kang MJ, Kim HG, Kim JS, Oh do G, Um YJ, Seo CS, et al. The effect of gut microbiota on drug metabolism. Expert Opin Drug Metab Toxicol. 2013;9:1295–308. doi: 10.1517/17425255.2013.807798. [DOI] [PubMed] [Google Scholar]
- 17.Wan JY, Liu P, Wang HY, Qi LW, Wang CZ, Li P, et al. Biotransformation and metabolic profile of American ginseng saponins with human intestinal microflora by liquid chromatography quadrupole time-of-flight mass spectrometry. J Chromatogr A. 2013;1286:83–92. doi: 10.1016/j.chroma.2013.02.053. [DOI] [PubMed] [Google Scholar]
- 18.Baxter NT, Zackular JP, Chen GY, Schloss PD. Structure of the gut microbiome following colonization with human feces determines colonic tumor burden. Microbiome. 2014;2:20. doi: 10.1186/2049-2618-2-20. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.Corona G, Rizzolio F, Giordano A, Toffoli G. Pharmaco-metabolomics: an emerging "omics" tool for the personalization of anticancer treatments and identification of new valuable therapeutic targets. J Cell Physiol. 2012;227:2827–31. doi: 10.1002/jcp.24003. [DOI] [PubMed] [Google Scholar]
- 20.Ahlem CN, Page TM, Auci DL, Kennedy MR, Mangano K, Nicoletti F, et al. Novel components of the human metabolome: the identification, characterization and anti-inflammatory activity of two 5-androstene tetrols. Steroids. 2011;76:145–55. doi: 10.1016/j.steroids.2010.10.005. [DOI] [PubMed] [Google Scholar]
- 21.Wang CZ, Aung HH, Ni M, Wu JA, Tong R, Wicks S, et al. Red American ginseng: ginsenoside constituents and antiproliferative activities of heat-processed Panax quinquefolius roots. Planta Med. 2007;73:669–74. doi: 10.1055/s-2007-981524. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22.Wang CZ, Li XL, Wang QF, Mehendale SR, Fishbein AB, Han AH, et al. The mitochondrial pathway is involved in American ginseng-induced apoptosis of SW-480 colon cancer cells. Oncol Rep. 2009;21:577–84. doi: 10.3892/or_00000259. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23.Ghia JE, Blennerhassett P, Kumar-Ondiveeran H, Verdu EF, Collins SM. The vagus nerve: a tonic inhibitory influence associated with inflammatory bowel disease in a murine model. Gastroenterology. 2006;131:1122–30. doi: 10.1053/j.gastro.2006.08.016. [DOI] [PubMed] [Google Scholar]
- 24.Xie G, Wang CZ, Yu C, Qiu Y, Wen XD, Zhang CF, et al. Metabonomic profiling reveals cancer chemopreventive effects of American ginseng on colon carcinogenesis in Apc(Min/+) mice. J Proteome Res. 2015;14:3336–47. doi: 10.1021/acs.jproteome.5b00388. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25.Ydens E, Cauwels A, Asselbergh B, Goethals S, Peeraer L, Lornet G, et al. Acute injury in the peripheral nervous system triggers an alternative macrophage response. J Neuroinflammation. 2012;9:176. doi: 10.1186/1742-2094-9-176. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 26.Phua LC, Koh PK, Cheah PY, Ho HK, Chan EC. Global gas chromatography/time-of-flight mass spectrometry (GC/TOFMS)-based metabonomic profiling of lyophilized human feces. J Chromatogr B Analyt Technol Biomed Life Sci. 2013;937:103–13. doi: 10.1016/j.jchromb.2013.08.025. [DOI] [PubMed] [Google Scholar]
- 27.Wang Y, Hoenig JD, Malin KJ, Qamar S, Petrof EO, Sun J, et al. 16S rRNA gene-based analysis of fecal microbiota from preterm infants with and without necrotizing enterocolitis. ISME J. 2009;3:944–54. doi: 10.1038/ismej.2009.37. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 28.Huang EY, Leone VA, Devkota S, Wang Y, Brady MJ, Chang EB. Composition of dietary fat source shapes gut microbiota architecture and alters host inflammatory mediators in mouse adipose tissue. JPEN J Parenter Enteral Nutr. 2013;37:746–54. doi: 10.1177/0148607113486931. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 29.Evans CC, LePard KJ, Kwak JW, Stancukas MC, Laskowski S, Dougherty J, et al. Exercise prevents weight gain and alters the gut microbiota in a mouse model of high fat diet-induced obesity. PLoS One. 2014;9:e92193. doi: 10.1371/journal.pone.0092193. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 30.Attele AS, Wu JA, Yuan CS. Ginseng pharmacology: multiple constituents and multiple actions. Biochem Pharmacol. 1999;58:1685–93. doi: 10.1016/s0006-2952(99)00212-9. [DOI] [PubMed] [Google Scholar]
- 31.Wang CZ, Du GJ, Zhang Z, Wen XD, Calway T, Zhen Z, et al. Ginsenoside compound K, not Rb1, possesses potential chemopreventive activities in human colorectal cancer. Int J Oncol. 2012;40:1970–6. doi: 10.3892/ijo.2012.1399. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 32.Zhang Z, Du GJ, Wang CZ, Wen XD, Calway T, Li Z, et al. Compound K, a ginsenoside metabolite, inhibits colon cancer growth via multiple pathways including p53-p21 interactions. Int J Mol Sci. 2013;14:2980–95. doi: 10.3390/ijms14022980. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 33.Wang CZ, Zhang Z, Wan JY, Zhang CF, Anderson S, He X, et al. Protopanaxadiol, an active ginseng metabolite, significantly enhances the effects of Fluorouracil on colon cancer. Nutrients. 2015;7:799–814. doi: 10.3390/nu7020799. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 34.Sreekumar A, Poisson LM, Rajendiran TM, Khan AP, Cao Q, Yu J, et al. Metabolomic profiles delineate potential role for sarcosine in prostate cancer progression. Nature. 2009;457:910–4. doi: 10.1038/nature07762. [DOI] [PMC free article] [PubMed] [Google Scholar] [Research Misconduct Found]
- 35.Ardawi MS, Newsholme EA. Fuel utilization in colonocytes of the rat. Biochem J. 1985;231:713–9. doi: 10.1042/bj2310713. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 36.Ameho CK, Adjei AA, Harrison EK, Takeshita K, Morioka T, Arakaki Y, et al. Prophylactic effect of dietary glutamine supplementation on interleukin 8 and tumour necrosis factor alpha production in trinitrobenzene sulphonic acid induced colitis. Gut. 1997;41:487–93. doi: 10.1136/gut.41.4.487. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 37.Yin Y, Sun W, Xiang J, Deng L, Zhang B, Xie P, et al. Glutamine synthetase functions as a negative growth regulator in glioma. J Neurooncol. 2013;114:59–69. doi: 10.1007/s11060-013-1168-5. [DOI] [PubMed] [Google Scholar]
- 38.Compare D, Nardone G. Contribution of gut microbiota to colonic and extracolonic cancer development. Dig Dis. 2011;29:554–61. doi: 10.1159/000332967. [DOI] [PubMed] [Google Scholar]
- 39.Natividad JM, Pinto-Sanchez MI, Galipeau HJ, Jury J, Jordana M, Reinisch W, et al. Ecobiotherapy rich in Firmicutes decreases susceptibility to colitis in a humanized gnotobiotic mouse model. Inflamm Bowel Dis. 2015;21:1883–93. doi: 10.1097/MIB.0000000000000422. [DOI] [PubMed] [Google Scholar]
- 40.Hur H, Paik MJ, Xuan Y, Nguyen DT, Ham IH, Yun J, et al. Quantitative measurement of organic acids in tissues from gastric cancer patients indicates increased glucose metabolism in gastric cancer. PLoS One. 2014;9:e98581. doi: 10.1371/journal.pone.0098581. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 41.Thamphiwatana S, Gao W, Obonyo M, Zhang L. In vivo treatment of Helicobacter pylori infection with liposomal linolenic acid reduces colonization and ameliorates inflammation. Proc Natl Acad Sci U S A. 2014;111:17600–5. doi: 10.1073/pnas.1418230111. [DOI] [PMC free article] [PubMed] [Google Scholar]