Abstract
Prior research examining links between neighborhood violence and mental health has not been able to establish whether it is perceived levels of neighborhood violence, or actual levels of violent crime, that matter most for adolescents’ psychological well-being. In this study, we ascertained both perceived neighborhood safety and objectively-measured neighborhood-level violent crime (using a novel geospatial index of police-reported crime incidents) for 4464 adolescent respondents from the California Health Interview Survey (CHIS 2011–2014). We used propensity score-matched regression models to examine associations between these measures and CHIS adolescents’ symptoms of psychological distress. We found that adolescents who perceived their neighborhood to be unsafe were two times more likely than those who perceived their neighborhood to be safe to report serious psychological distress (OR = 2.4, 95 % CI = 1.20, 4.96). Adolescents who lived in areas objectively characterized by high levels of violent crime, however, were no more likely than their peers in safer areas to be distressed (OR = 1.41; 95 % CI = 0.60, 3.32). Our results suggest that, at the population level, adolescents’ perceptions of neighborhood violence, rather than objective levels of neighborhood crime, are most salient for their mental health.
Electronic supplementary material
The online version of this article (doi:10.1007/s11524-016-0079-0) contains supplementary material, which is available to authorized users.
Keywords: Adolescent, Mental health, Neighborhood, Violence
More than a third of all adolescents in the USA report being exposed to violence (e.g., assault, gang intimidation, or robbery) in their neighborhood. 1 Much research finds that adolescents who report such neighborhood violence exposure are, in comparison to non-exposed peers, significantly more likely to exhibit symptoms of depression, anxiety, and other mental health problems. 2 – 5 These findings have been interpreted as suggesting that residence in a violent neighborhood may have a potentially large impact on adolescent mental health 6 and have helped motivate neighborhood-level interventions aimed at reducing emotional problems. 7 It remains unclear, however, whether it is adolescents’ perceptions of the levels of violence and crime in their neighborhood, or the actual levels of violence, that are most salient for their mental health.
The majority of studies in this literature limit their focus to adolescents’ perceptions of their exposure to neighborhood violence. The estimated associations between perceived violence exposure and depression/anxiety symptoms are fairly robust (e.g., Cohen’s d = 0.45) 2, but the validity of this approach has been questioned. 2 , 8 Residents’ perceptions of their neighborhood’s safety may be more strongly influenced by neighborhood sociodemographic characteristics than by true levels of violence. 9 – 12 Furthermore, self-reported measures are vulnerable to common method bias, in which personality or affective traits influence not only individuals’ evaluations of their neighborhoods but also their risk of mental health problems. 13 – 15
It has historically been difficult to obtain neighborhood-level crime data, especially across multiple areas. As a result, only a few studies (none on adolescents) have assessed how objective levels of neighborhood violent crime are related to residents’ mental health. The associations of these studies report are generally weak or null. In a small sample of Baltimore children (n = 97), Hill and colleagues found that census tract-level crime was unrelated to anxiety symptoms. 16 In a separate Baltimore sample of adult former drug users (n = 786), Curry and colleagues found that census block-group violent crime rates did not directly affect depression symptoms, although there was a weak association between the two that was mediated by participants’ perceptions of neighborhood disorder and personal experiences of violence. 17 Lastly, in two large representative samples (n > 10,000) of English adults, Dustmann and Fasani found that while overall area crime rates were positively related to psychological distress the effect of violent crime was weak. 18
These findings suggest that it may be adolescents’ perceptions of their neighborhood that matter most for their mental health. No research, however, has explicitly compared how perceived vs. objectively-measured levels of neighborhood violence are related to adolescents’ symptoms of depression and anxiety. Answering this question is crucial for understanding the mechanisms that connect violence exposure to psychological problems and for directing mental health treatment resources to the adolescents at highest risk.
In the current study, we used a large population-representative sample of California youths for whom we had measures of perceived neighborhood safety, objective levels of neighborhood violent crime, and psychological distress. Our objective neighborhood measure was a commercially-developed index of census tract-level violent crime, derived from Uniform Crime Reports data from the Federal Bureau of Investigation (FBI). 19 These data allowed us to test the hypothesis that it is adolescents’ perceptions of their exposure to neighborhood violence, rather than their residence in a neighborhood characterized by high levels of violent crime, that most strongly influences their likelihood of psychological distress.
Methods
Sample
We used data from the adolescent portions of the 2011/2012, 2013, and 2014 California Health Interview Survey (CHIS), which has been described in detail elsewhere. 20 – 24 Briefly, the CHIS is a large, repeated, statewide cross-sectional telephone survey that collects health, social, and demographic information on a representative sample of the non-institutionalized civilian population of California. The CHIS uses a two-stage design that combines a landline sample, supplemental surname-listed samples, and a statewide cell phone sample. One adult per household is randomly selected for interview, and if that adult is the parent/guardian of an adolescent (aged 12–17 years), the adolescent is also interviewed. Household response rates ranged from 51.4 to 53.9 %, and adolescent response rates from 41.0 to 42.7 %, during the period 2011 to 2014. This is comparable to other random-digit dialing (RDD) surveys. Post-stratification and other nonresponse adjustments correct for selective nonresponse on the basis of demographic and geographic factors. Participating CHIS households’ addresses are geocoded to the census tract level. Following established practice, we used adolescents’ census tracts (defined using 2010 boundaries) as approximations of their local neighborhoods. 25 , 26
The CHIS includes data on 4616 adolescents during the study period. Our final analytic sample included adolescents whose addresses were accurately geocoded, who had lived at their address for ≥6 months, and whose parent or legal guardian completed the adult interview, for a total of 4,462 youths (96.7 % of the original sample) living in 1969 unique census tracts. Of this analytic sample, 54.8, 24.2, and 21.0 % were from the 2011/2012, 2013, and 2014 CHIS surveys, respectively. This analysis was approved by the Institutional Review Board of the University of California, Merced.
Outcome Measure
The outcome of interest, incidence of past-month serious psychological distress (SPD), was assessed using the Kessler-6. 27 The K-6 is a widely used, six-item measure of depression and anxiety symptoms designed to identify cases of diagnosable mental illness in population surveys. Adolescents who received a K-6 score of ≥13 were considered to have SPD.
Exposure Measures
Perceived Neighborhood Safety
Adolescents’ neighborhood safety perceptions were measured using a single query: “Do you feel safe in your neighborhood all of the time, most of the time, some of the time, or none of the time?” This question was identical in each CHIS survey cycle. For regression and propensity score analyses, responses were dichotomized, with adolescents who responded that they felt safe in their neighborhood “some” or “none” of the time coded as living in a neighborhood perceived to be unsafe. Adolescents who responded that they felt safe “all” or “most” of the time were coded as living in a neighborhood perceived to be safe.
Objectively-Measured Neighborhood Violence
Adolescents’ exposure to objectively-measured neighborhood violence was assessed using a geospatial index of violent crime victimization risk developed by Location Inc. This index is based on Uniform Crime Reports (UCR) statistics reported annually to the FBI by local law enforcement agencies. UCR data include all known crime incidents that occur in each agency’s jurisdiction and are considered a valid measure of the incidence of criminal behavior. 28 , 29 Location Inc.’s violent crime victimization risk index incorporates information on incidents of assault, robbery, rape, and homicide.
To create the annual crime-risk index for a given area, Location Inc. takes the violent crime incident reports aggregated from all law enforcement agencies with jurisdiction in that area, normalizes that number to the area’s population, and combines those data with local indicators of social and economic segmentation to generate smoothed, high-resolution geospatial models of violent crime risk. Initial models are further validated against the large subset of crime incidents that contain geocoded (i.e., address-specific) data. Finally, the geospatial model for the area is partitioned at the census tract level and translated into a numeric index, with scores representing each tract’s local violent-crime risk relative to the national average. The index is constructed on a 0–5000 scale: 100 indicates that the census tract is at the national average for violent crime-risk, 50 represents half the national average, and 5000 represents 50 times the national average. In tests against insurance claims, Location Inc.’s risk models have proven highly reliable and valid. 30
We used a categorical version (range: 1 to 5) of the continuous scale, where 1 indicates a low-risk community (crime-risk score of 0 to 49) and 5 indicates a very high-risk community (crime-risk score of 300 to 5000). For regression and propensity score analyses, based on the developers’ recommendation, neighborhoods scoring 4 or 5 on the crime-risk scale were defined as highly violent. All other neighborhoods were defined as non-violent. Violent crime-risk data from 2013, corresponding approximately to the midpoint of our CHIS survey data, were used for this analysis.
Covariates
Individual-, family-, and community-level covariates were selected for inclusion in analyses based on their established associations with the exposure and outcome variables. Adolescents’ age, gender, and racial/ethnic status were assessed during the CHIS interview and based on self-report. Race was categorized as white, black, Hispanic, Asian, or other/multiple races. Adolescents’ family socioeconomic status was assessed using both parental self-reported education (less than high school, high school, some college, or college degree) and household income as a percent of the federal poverty level (0–99 %, 100–199 %, 200–299 %, and ≥300 %). Urbanicity of the adolescent’s household was coded as urban, second city, suburban, or town/rural, based on population density of the household’s zip code and surrounding areas. Adolescents’ parents’ marital status was coded as married/living with partner or other. Finally, adolescents whose parent received a past-month K-6 score ≥ 13 or reported a lifetime suicide attempt were coded as having a family history of mental disorder.
Data on census tract-level sociodemographic and housing characteristics were drawn from the U.S. Census Bureau’s American Community Survey (ACS). We used 5-year ACS estimates for the years 2009–2013, the most recent dataset available. Following established practice in epidemiology, we measured adolescents’ neighborhood-level socioeconomic disadvantage using a standardized index that combines information on census tract median household income, median value of housing units, percent of households with interest income, percent of persons with a high school degree, percent of persons with a college degree, and percent of persons employed in high-status jobs. 31 Higher index scores correspond to increasing socioeconomic advantage.
Statistical Analyses
We linked each CHIS adolescent’s interview data to the violent crime-risk index and ACS data for his or her residential census tract. Means of the CHIS outcome variables and other sample characteristics were similar across survey cycle years, supporting concatenation of the datasets. Clustering of adolescents within census tracts was negligible.
We used chi-square and t tests to examine the distribution of adolescent psychological distress and covariates in the CHIS sample overall and by perceived and objectively-measured neighborhood violence (accounting for the complex survey design and sampling weights). We used chi-square tests and logistic regression models to examine the association between perceived and objective neighborhood violence.
To assess how perceived and objectively-measured neighborhood violence was each related to adolescent psychological distress, we first estimated design-based, survey-weighted bivariate logistic regression models. Next, we used a propensity score matching approach to account for non-random selection of adolescents into neighborhoods. 32 Two propensity scores were estimated for each adolescent. The first reflected his or her predicted probability of living in a neighborhood perceived to be unsafe; the second reflected his or her predicted probability of living in a neighborhood objectively high in violence. Because the individual- and neighborhood-level characteristics that predict perceived and objective levels of violence are likely similar, each of our propensity scores was estimated as a function of the covariates specified above. For each propensity score, we used kernel matching to match “treated” adolescents to a weighted composite of “non-treated” adolescents. In this approach—recommended when using weighted complex survey data—non-treated individuals are weighted by their distance in propensity score from treated individuals within a bandwidth (0.06) of the propensity score. 33 – 35 After matching, covariate balance (as indicated by standardized mean differences of <10 %) was achieved (Supplementary Figures 1 and 2). Finally, we ran a survey-weighted, design-based logistic regression model within each matched sample to estimate adolescents’ log odds of psychological distress as a function of their perceived or objectively-measured neighborhood violence and associated propensity score, to account for residual confounding. All analyses were performed using Stata 14 (StataCorp LP, College Station, TX). Propensity score matching was implemented using the psmatch2 command. 33 Use of survey weights allowed to extrapolate our results to the adolescent population of California.
Results
One in every nine California adolescents (11.1 %) perceived their neighborhood to be unsafe. A slightly larger proportion (11.8 %) lived in a neighborhood identified by the crime-risk index as objectively high in violent crime. Survey-weighted characteristics of the study sample overall, and by perceived and objectively-measured neighborhood violence exposure, are shown in Table 1. Compared to those in safer neighborhoods, the adolescents who lived in subjectively unsafe or objectively violent neighborhoods were more likely to be of minority race/ethnicity, to have a household income less than 300 % FPL, and to have parents who were unmarried, who had a history of mental illness, and who had less than a college degree. The perceived- and objectively-unsafe neighborhoods were also more socioeconomically disadvantaged and more likely to be urban.
TABLE 1.
Individual, family, and neighborhood characteristics of 2011–2014 California Health Interview Survey (CHIS) adolescents residing in neighborhoods characterized according to perceived safety and objective levels of violent crime
| Adolescents residing in neighborhoods perceived to be: | Adolescents residing in neighborhoods objectively measured as: | ||||
|---|---|---|---|---|---|
| Full sample (n = 4462) | Safe (n = 4000) | Unsafe (n = 462) | Non-violent (n = 4027) | Highly violent (n = 435) | |
| Individual characteristicsa | |||||
| Gender (% female) | 49.2 % | 48.6 % | 54.3 % | 49.4 % | 47.7 % |
| Age (mean (SE)) | 14.6 (0.22) | 14.6 (0.27) | 14.7 (0.14) | 14.6 (0.23) | 14.7 (0.18) |
| Race/ethnicity (%) | |||||
| Hispanic | 31.6 % | 30.5 % | 39.8 % | 29.4 % | 47.9 % |
| White | 35.0 % | 36.6 % | 22.7 % | 38.0 % | 12.9 % |
| Black | 5.6 % | 5.2 % | 8.4 % | 4.1 % | 16.2 % |
| Asian | 11.4 % | 11.4 % | 12.1 % | 11.8 % | 8.8 % |
| Other/multiple | 16.4 % | 16.3 % | 17.1 % | 16.7 % | 14.2 % |
| Serious psychological distress (%) | 4.4 % | 3.8 % | 9.8 % | 4.1 % | 6.8 % |
| Family characteristicsa | |||||
| Household income as percentage of the FPL (%) | |||||
| Below 100 % FPL | 19.7 % | 18.2 % | 31.2 % | 17.3 % | 37.6 % |
| 100–199 % FPL | 24.2 % | 22.9 % | 34.5 % | 22.8 % | 34.6 % |
| 200–299 % FPL | 13.0 % | 13.5 % | 9.0 % | 13.2 % | 11.3 % |
| 300 % FPL and above | 43.2 % | 45.4 % | 25.3 % | 46.7 % | 16.5 % |
| Parental educational attainment (%) | |||||
| Less than high school | 21.1 % | 19.4 % | 34.5 % | 18.5 % | 40.3 % |
| High school graduate | 16.9 % | 16.3 % | 22.3 % | 16.8 % | 18.2 % |
| Some college | 23.2 % | 23.5 % | 20.4 % | 23.4 % | 21.2 % |
| College graduate | 38.8 % | 40.8 % | 22.8 % | 41.3 % | 20.3 % |
| Parental marital status (%) | |||||
| Married or living with partner | 67.6 % | 74.8 % | 63.2 % | 76.0 % | 55.1 % |
| Other | 32.4 % | 25.2 % | 36.8 % | 24.0 % | 45.0 % |
| Parental history of mental disorder (%) | 11.0 % | 10.1 % | 17.9 % | 10.4 % | 15.3 % |
| Neighborhood characteristicsa | |||||
| Urbanicity | |||||
| Urban | 47.8 % | 45.6 % | 65.5 % | 44.1 % | 75.5 % |
| Second city | 22.3 % | 22.5 % | 20.6 % | 23.2 % | 15.3 % |
| Suburban | 20.0 % | 21.6 % | 7.2 % | 22.2 % | 4.1 % |
| Town and rural | 9.9 % | 10.3 % | 6.7 % | 10.5 % | 5.1 % |
| Neighborhood socioeconomic disadvantage (mean (SE)) | −0.1 (0.06) | 0.2 (0.09) | −2.3 (0.21) | 0.4 (0.15) | −3.8 (0.26) |
FPL Federal Poverty Limit
aEstimates are weighted to be representative of the California population and are adjusted for complex survey design effects
Measures of perceived and objective neighborhood violence were strongly associated, but not entirely concordant. Adolescents who lived in objectively violent areas were three times more likely than those in non-violent areas to perceive their neighborhood as unsafe (24.0 vs. 9.4 %), and adolescents who perceived their neighborhood to be unsafe were three times more likely than those who saw their neighborhood as safe to live in an objectively violent area (25.5 vs. 10.1 %) (OR = 3.04, 95 % CI = 2.05, 4.52; see Table 2). Correspondingly, 76.0 % of adolescents who lived in an objectively violent area thought their neighborhood was safe, and 74.5 % of those who thought their neighborhood was unsafe lived in a non-violent area.
TABLE 2.
Concordance between perceived and objectively-measured levels of neighborhood violence among CHIS Adolescents, 2011–2014
| Adolescents residing in neighborhoods perceived to be: | Adolescents residing in neighborhoods objectively characterized as: | ||||
|---|---|---|---|---|---|
| Full sample (n = 4463) | Safea (n = 4000) | Unsafea (n = 462) | Non-violenta (n = 4027) | Highly violenta (n = 435) | |
| Perceived neighborhood violence: | |||||
| Adolescent feels neighborhood is safe most/all of time | 88.9 % | 90.6 % | 76.0 % | ||
| Adolescent feels neighborhood is safe some/none of time | 11.1 % | 9.4 % | 24.0 % | ||
| Objective neighborhood violence: | |||||
| Neighborhood is non-violent | 88.2 % | 89.9 % | 74.5 % | ||
| Neighborhood is highly violent | 11.8 % | 10.1 % | 25.5 % | ||
aPercentages reflect column percents.
bEstimates are weighted to be representative of the California population and are adjusted for complex survey design effects.
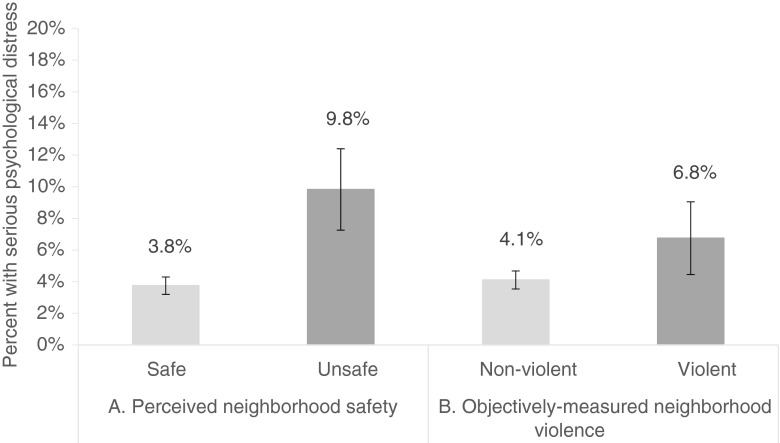
An estimated 4.4 % of all surveyed adolescents reported past-month serious psychological distress. We first examined the associations between neighborhood violence and odds of SPD by running unadjusted logistic regression models, accounting for the survey design and weights (Table 3). Prevalence estimates for SPD were 9.8 and 3.8 % among adolescents who perceived their neighborhood to be unsafe and safe, respectively (ORunadj = 2.80, 95 % CI = 1.47, 5.32). By contrast, living in an objectively violent neighborhood was not significantly associated with adolescents’ odds of distress. Prevalence of SPD was 6.8 vs. 4.1 % for adolescents in highly violent vs. non-violent neighborhoods, respectively (ORunadj = 1.69; 95 % CI = 0.26, 11.17). Figure 1 depicts the survey-weighted SPD prevalence estimates across levels of both perceived and objectively-measured neighborhood violence.
TABLE 3.
Unadjusted and propensity score-matched odds ratios between perceived neighborhood safety, objectively-measured neighborhood violence, and adolescent serious psychological distress (SPD), CHIS, 2011–2014
| OR (95 % CI) for SPD: Unadjusted analysesa | OR (95 % CI) for SPD: Propensity score-matched analysesb | |
|---|---|---|
| Living in a neighborhood perceived to be unsafe | 2.80 (1.47, 5.32) | 2.44 (1.20, 4.96) |
| Living in a neighborhood objectively characterized as highly violent | 1.69 (0.26, 11.17) | 1.41 (0.60, 3.32) |
aAnalytic sample included all CHIS 2011–2014 adolescent subjects whose addresses were accurately geocoded, who had lived at their address for ≥6 months, and whose parent or legal guardian completed the adult interview (n = 4462)
bAnalytic sample was identical to that for unadjusted models, but models used kernel-matched propensity scores to match “treated” adolescents to a weighted composite of “non-treated” adolescents
FIGURE 1.
Proportion of CHIS 2011–2014 adolescents reporting past-month serious psychological distress, according to their residence in neighborhoods a perceived to be safe vs. unsafe and b objectively measured as non-violent vs. highly violent.
We then ran survey-weighted propensity score-matched models. In these models, the estimated effect sizes were slightly reduced but inference remained the same. Adolescents who perceived their neighborhood to be unsafe had more than twice the odds of recent SPD compared to those who saw their neighborhood as safe (OR = 2.44, 95 % CI = 1.20, 4.96). The association between objective levels of violence and SPD was estimated with greater precision, but adolescents who lived in an objectively violent area remained no more likely than their peers in safer areas to report serious distress (OR = 1.41, 95 % CI = 0.60, 3.32). Lastly, to assess whether there was any residual confounding of the relationship between adolescents’ perceived safety and SPD by objective levels of violent crime, we re-estimated the perceived safety model with objective violence as a covariate. Results were unchanged (OR = 2.42, 95 % CI = 1.22, 4.79).
Discussion
Results from our large, population-based study in California show that adolescents who perceived their neighborhood to be unsafe had nearly 2.5-fold greater odds of recent serious psychological distress compared to those who believed their neighborhood to be safe. Adolescents who lived in areas objectively characterized by high levels of violent crime, however, were no more likely to be distressed than their peers in safer areas. These patterns were evident in both unadjusted analyses and in propensity score-matched models that accounted for a wide range of individual-, family-, and neighborhood-level confounders. Our results also confirm earlier evidence that while perceived and objective levels of neighborhood violence are strongly associated, they are not interchangeable. 9 , 12 , 14
Our findings are broadly consistent with two separate bodies of research showing, on the one hand, that perceived exposure to neighborhood violence is significantly associated with youths’ mental health problems, 2 – 5 and, on the other hand, that residing in an area with high rates of violent crime appears to have little impact on risk of depression and anxiety 16 – 18 (with a possible exception for older adults 36). None of these studies examined the relative impacts of both subjectively- and objectively-measured neighborhood violence on adolescents’ mental health, and many used high-risk participant samples from urban areas, so they could not rule out the possibility that inadequate variation in levels of neighborhood violence had biased their results. 37 , 38 In contrast, we examined the psychological impact of both subjective and objective neighborhood violence on an epidemiologic sample of >4400 adolescents from a wide spectrum of social and geographic contexts. Our study thus provides rigorous new support for the idea that it is adolescents’ perceptions of their neighborhood that matter most for their mental health.
There are several potential explanations for why adolescents’ perceptions of their neighborhood may be more strongly linked to their mental health than are objective levels of local violence. First, as noted earlier, common method bias may explain the strong association we observed between self-reported neighborhood safety and psychological distress. 13 – 15 Second, it is possible that only youths who are personally victimized by assault, robbery, rape, or other violence (and thus particularly likely to see their environs as dangerous) develop symptoms of distress. 17 Rates of such victimization tend to be higher in communities characterized by crime and disorder, but even in safer communities >30 % of adolescents report some type of victimization. 1 Third, our findings may be due to reverse causation: adolescents with poor mental health may be more vulnerable to being victimized and engaging in violence 39 , 40 and experience their neighborhoods as more threatening than would a psychologically healthy teen 14—regardless of true levels of crime. Fourth, adolescents who grow up surrounded by violence may become psychologically desensitized to its occurrence, 41 reducing both their perceived exposure to neighborhood violence and their likelihood of reporting mental health problems (however, there are conflicting findings 42). Lastly, exposure to neighborhood-level violence may be more strongly tied to delinquent and aggressive behaviors than to the depression/anxiety symptoms we could assess in this study. 2 Our study design did not allow us to test these explanations’ relative importance, and more research will be needed to disentangle their effects.
Methodological advantages of our study include our use of a population-based epidemiologic sample of adolescents from a large and diverse state, propensity score matching techniques that accounted for confounding and selection of vulnerable youths into violent neighborhoods, and a unique combination of both perceived and objective indicators of exposure to neighborhood safety and violence. In particular, by capitalizing on a commercially-developed measure of area-level violent crime risk based on UCR crime data, we were able to specifically examine residents’ exposure to neighborhood violence (as distinct from neighborhood socioeconomic disadvantage); to our knowledge, no prior work has been able to do this across multiple cities.43 – 45
There are several limitations to this study. First, due to the cross-sectional nature of the data, no causal or temporal relationship between the study risk factors and outcome can be inferred. Second, our measure of adolescent mental health was limited to a brief (although well-validated 27) screening instrument assessing non-specific distress symptoms, and our measure of perceived neighborhood safety was also limited to a single query. 46 Future work should re-examine these questions using more nuanced measures. Third, our research relies on the assumption that the CHIS survey weights adequately correct for sample selection and non-response. We also assumed that our propensity score was correctly specified, although the fact that both unadjusted and adjusted models resulted in the same inference provides some reassurance about our findings’ robustness.
It is also important to highlight that our objective indicator of neighborhood violence has never before been used in health research. However, the crime-risk index is similar to other measures of area-level crime used in health research 36 , 47 , 48 and is widely employed for commercial purposes (e.g., insurance rate-setting) that demand a high degree of accuracy. Our confidence in the index’s validity was also bolstered by its strong—though not perfect—correlations with neighborhood-level socioeconomic disadvantage, adolescents’ demographic characteristics, and adolescents’ subjective ratings of neighborhood safety. Notably, we used a version of the index that classifies neighborhoods according to their crime rates relative to the national average, which we believe to be the most conservative and appropriate approach given our statewide population-based sample. However, Location, Inc. also constructs crime-risk indices relative to state and county averages, and future research should investigate whether the choice of this comparison influences observed associations between neighborhood violent crime and health. Lastly, we note that—as in most epidemiologic research in this area—the crime-risk index defines neighborhood boundaries on the basis of census tracts, which may not reflect the relevant area of exposure and may not correspond with adolescents’ own definitions of their “neighborhood.” 49 , 50
This study employed population-based data to investigate the respective associations between perceived and objective levels of neighborhood violence and adolescent mental health. Our results suggest that perceptions of neighborhood violence, irrespective of actual levels of violence in neighborhoods, influence adolescent psychological distress. Adolescents who perceive their neighborhoods as unsafe may be a potentially vulnerable subgroup in need of mental health services. Research that explores the mechanisms underlying this association, and public health strategies that target these youths for better mental health care, may be important for reducing the public health burden of psychological disorder among adolescents in the U.S.
Electronic supplementary material
(DOCX 171 kb)
References
- 1.Turner HA, Shattuck A, Hamby S, Finkelhor D. Community disorder, victimization exposure, and mental health in a national sample of youth. J Health Soc Behav. 2013;54(2):258–75. doi: 10.1177/0022146513479384. [DOI] [PubMed] [Google Scholar]
- 2.Fowler PJ, Tompsett CJ, Braciszewski JM, et al. Community violence: a meta-analysis on the effect of exposure and mental health outcomes of children and adolescents. Dev Psychopathol. 2009;21(1):227–59. doi: 10.1017/S0954579409000145. [DOI] [PubMed] [Google Scholar]
- 3.Mrug S, Windle M. Prospective effects of violence exposure across multiple contexts on early adolescents’ internalizing and externalizing problems. J Child Psychol Psychiatry. 2010;51(8):953–61. doi: 10.1111/j.1469-7610.2010.02222.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Slopen N, Fitzmaurice GM, Williams DR, Gilman SE. Common patterns of violence experiences and depression and anxiety among adolescents. Soc Psychiatry Psychiatr Epidemiol. 2012;47(10):1591–605. doi: 10.1007/s00127-011-0466-5. [DOI] [PubMed] [Google Scholar]
- 5.Newbury J, Arseneault L, Caspi A, et al. Why are children in urban neighborhoods at increased risk for psychotic symptoms? findings from a UK longitudinal cohort study. Schizophr Bull. 2016; 1–12. [DOI] [PMC free article] [PubMed]
- 6.Cooley-Strickland M, Quille TJ, Griffin RS, et al. Community violence and youth: affect, behavior, substance use, and academics. Clin Child Fam Psychol Rev. 2009;12(2):127–56. doi: 10.1007/s10567-009-0051-6. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Kessler RC, Duncan GJ, Gennetian LA, et al. Associations of housing mobility interventions for children in high-poverty neighborhoods with subsequent mental disorders during adolescence. JAMA. 2014;311(9):937–48. doi: 10.1001/jama.2014.607. [DOI] [PMC free article] [PubMed] [Google Scholar] [Retracted]
- 8.Diez Roux AV, Mair C. Neighborhoods and health. Ann N Y Acad Sci. 2010;1186(1):125–45. doi: 10.1111/j.1749-6632.2009.05333.x. [DOI] [PubMed] [Google Scholar]
- 9.Selner-O’Hagan MB, Kindlon DJ, Buka SL, et al. Assessing exposure to violence in urban youth. J Child Psychol Psychiatry. 1998;39(2):215–24. doi: 10.1111/1469-7610.00315. [DOI] [PubMed] [Google Scholar]
- 10.Sampson RJ, Raudenbush SW. Seeing disorder: neighborhood stigma and the social construction of “broken windows.”. Soc Psychol Q. 2004;67(4):319–42. doi: 10.1177/019027250406700401. [DOI] [Google Scholar]
- 11.Hill HM, Madhere S. Exposure to community violence and African American children: a multidimensional model of risks and resources. J Community Psychol. 1996;24(1):26–43. doi: 10.1002/(SICI)1520-6629(199601)24:1<26::AID-JCOP3>3.0.CO;2-1. [DOI] [Google Scholar]
- 12.Kneeshaw-Price SH, Saelens BE, Sallis JF, et al. Neighborhood crime-related safety and its relation to children’s physical activity. J Urban Heal. 2015;92(3):472–89. doi: 10.1007/s11524-015-9949-0. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Meltzer H, Vostanis P, Goodman R, Ford T. Children’s perceptions of neighbourhood trustworthiness and safety and their mental health. J Child Psychol Psychiatry. 2007;48(12):1208–13. doi: 10.1111/j.1469-7610.2007.01800.x. [DOI] [PubMed] [Google Scholar]
- 14.Chung HL, Slocum C, Proverbs T. Objective and perceived community factors: exploring responses to context. Am J Health Behav. 2013;37(6):763–8. doi: 10.5993/AJHB.37.6.5. [DOI] [PubMed] [Google Scholar]
- 15.Fujiwara T, Kawachi I. A prospective study of individual-level social capital and major depression in the United States. J Epidemiol Community Health. 2008;62(7):627–33. doi: 10.1136/jech.2007.064261. [DOI] [PubMed] [Google Scholar]
- 16.Hill HM, Levermore M, Twaite J, Jones LP. Exposure to community violence and social support as predictors of anxiety and social and emotional behavior among African American children. J Child Fam Stud. 1996;5(4):399–414. doi: 10.1007/BF02233862. [DOI] [Google Scholar]
- 17.Curry A, Latkin C, Davey-Rothwell M. Pathways to depression: the impact of neighborhood violent crime on inner-city residents in Baltimore, Maryland. USA Soc Sci Med. 2008;67(1):23–30. doi: 10.1016/j.socscimed.2008.03.007. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.Dustmann C, Fasani F. The effect of local area crime on mental health. Econ J. 2014; 1–40.
- 19.United States Department of Justice Federal Bureau of Investigation. Crime in the United States, 2013. Washington, DC: Federal Bureau of Investigation; 2014.
- 20.Survey CHI. CHIS 2011–2012 methodology series: report 1—sample design. Los Angeles, CA: UCLA Center for Health Policy Research; 2014.
- 21.California Health Interview Survey. CHIS 2011–2012 methodology series: report 2—data collection methods. California Health Interview Survey. Los Angeles, CA: UCLA Center for Health Policy Research; 2014.
- 22.California Health Interview Survey. CHIS 2011–2012 methodology series: report 3—data processing procedures. California Health Interview Survey. Los Angeles, CA: UCLA Center for Health Policy Research; 2014.
- 23.California Health Interview Survey. CHIS 2011–2012 methodology series: report 4—response rates. California Health Interview Survey. Los Angeles, CA: UCLA Center for Health Policy Research; 2014.
- 24.California Health Interview. CHIS 2011–2012 methodology series: report 5—weighting and variance estimation. California Health Interview Survey. Los Angeles, CA: UCLA Center for Health Policy Research; 2014.
- 25.Diez Roux AV. Investigating neighborhood and area effects on health. Am J Public Health. 2001;91(11):1783–9. doi: 10.2105/AJPH.91.11.1783. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 26.Krieger N, Chen JT, Waterman PD, et al. Geocoding and monitoring of US socioeconomic inequalities in mortality and cancer incidence: does the choice of area-based measure and geographic level matter?: the public health disparities geocoding project. Am J Epidemiol. 2002;156(5):471–82. doi: 10.1093/aje/kwf068. [DOI] [PubMed] [Google Scholar]
- 27.Kessler RC, Andrews G, Colpe LJ, et al. Short screening scales to monitor population prevalences and trends in non-specific psychological distress. Psychol Med. 2002;32(6):959–76. doi: 10.1017/S0033291702006074. [DOI] [PubMed] [Google Scholar]
- 28.Blau JR, Blau PM. The cost of inequality: metropolitan structure and violent crime. Am Sociol Rev. 1982;47(1):114. doi: 10.2307/2095046. [DOI] [Google Scholar]
- 29.Gove WR, Huges M, Geerken M. Are uniform crime reports a valid indicator of the index crimes? an affirmative answer with minor qualifications. Criminology. 1985;23(3):451–502. doi: 10.1111/j.1745-9125.1985.tb00350.x. [DOI] [Google Scholar]
- 30.Location I. SecurityGauge commercial property crime risk index: white paper. 2013.
- 31.Diez Roux AV, Kiefe CI, Jacobs DR, et al. Area characteristics and individual-level socioeconomic position indicators in three population-based epidemiologic studies. Ann Epidemiol. 2001;11(6):395–405. doi: 10.1016/S1047-2797(01)00221-6. [DOI] [PubMed] [Google Scholar]
- 32.Rosenbaum PR, Rubin DB. The central role of the propensity score in observational studies for causal effects. Biometrika. 1983;70(1):41–55. doi: 10.1093/biomet/70.1.41. [DOI] [Google Scholar]
- 33.Garrido MM, Kelley AS, Paris J, et al. Methods for constructing and assessing propensity scores. Health Serv Res. 2014; 49(5): 1–20. [DOI] [PMC free article] [PubMed]
- 34.Dugoff EH, Schuler M, Stuart E. Generalizing observational study results: applying propensity score methods to complex surveys. Health Serv Res. 2014;49(1):284–303. doi: 10.1111/1475-6773.12090. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 35.Heckman JJ, Ichimura H, Todd PE. Matching as an econometric evaluation estimator: evidence from evaluating a job training programme. Rev Econ Stud. 1997;64(4):605–54. doi: 10.2307/2971733. [DOI] [Google Scholar]
- 36.Wilson-Genderson M, Pruchno R. Effects of neighborhood violence and perceptions of neighborhood safety on depressive symptoms of older adults. Soc Sci Med. 2013;85:43–9. doi: 10.1016/j.socscimed.2013.02.028. [DOI] [PubMed] [Google Scholar]
- 37.Duncan GJ, Raudenbush SW. Assessing the effects of context in studies of child and youth development. Educ Psychol. 1999;34(1):29–41. doi: 10.1207/s15326985ep3401_3. [DOI] [Google Scholar]
- 38.Duncan GJ, Connell JP, Klebanov PK. Conceptual and methodological issues in estimating causal effects of neighborhoods and family conditions on individual development. In: Brooks-Gunn J, Duncan GJ, Aber JL, editors. Neighborhood poverty: Vol. 1. Context and consequences for children. New York, NY: Russell Sage; 1997. pp. 219–50. [Google Scholar]
- 39.Arseneault L, Bowes L, Shakoor S. Bullying victimization in youths and mental health problems: “Much ado about nothing”? Psychol Med. 2010;40:717–29. doi: 10.1017/S0033291709991383. [DOI] [PubMed] [Google Scholar]
- 40.Fisher HL, Moffitt TE, Houts RM, et al. Bullying victimisation and risk of self harm in early adolescence: longitudinal cohort study. BMJ. 2012;344:e2683. doi: 10.1136/bmj.e2683. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 41.Gaylord-Harden NK, Cunningham JA, Zelencik B. Effects of exposure to community violence on internalizing symptoms: does desensitization to violence occur in African American youth? J Abnorm Child Psychol. 2011;39(5):711–9. doi: 10.1007/s10802-011-9510-x. [DOI] [PubMed] [Google Scholar]
- 42.Mccart MR, Smith DW, Saunders BE, et al. Do urban adolescents become desensitized to community violence? data from a national survey. Am J Orthopsychiatry. 2007;77(3):434–42. doi: 10.1037/0002-9432.77.3.434. [DOI] [PubMed] [Google Scholar]
- 43.Gary TL, Stark SA, Laveist TA. Neighborhood characteristics and mental health among African Americans and whites living in a racially integrated urban community. Heal Place. 2007;13(2):569–75. doi: 10.1016/j.healthplace.2006.06.001. [DOI] [PubMed] [Google Scholar]
- 44.Mair C, Diez Roux AV, Galea S. Are neighborhood characteristics associated with depressive symptoms? a critical review. J Epidemiol Community Heal. 2008;62(11):940–6. doi: 10.1136/jech.2007.066605. [DOI] [PubMed] [Google Scholar]
- 45.Morenoff JD. Neighborhood mechanisms and the spatial dynamics of birth weight. Am J Sociol. 2003;108(5):976–1017. doi: 10.1086/374405. [DOI] [PubMed] [Google Scholar]
- 46.Earls FJ, Brooks-Gunn J, Raudenbush SW, Sampson RJ. Project on human development in Chicago neighborhoods: community survey, 1994–1995. Ann Arbor, MI: Interuniversity Consortium for Political and Social Research (ICPSR), University of Michigan; 1997.
- 47.Gupta RS, Zhang X, Springston EE, et al. The association between community crime and childhood asthma prevalence in Chicago. Ann Allergy Asthma Immunol. 2010;104(4):299–306. doi: 10.1016/j.anai.2009.11.047. [DOI] [PubMed] [Google Scholar]
- 48.Kennedy BP, Kawachi I, Prothrow-Stith D, et al. Social capital, income inequality, and firearm violent crime. Soc Sci Med. 1998;47(1):7–17. doi: 10.1016/S0277-9536(98)00097-5. [DOI] [PubMed] [Google Scholar]
- 49.Sampson RJ, Morenoff JD, Gannon-Rowley T. Assessing “neighborhood effects”: social processes and new directions in research. Annu Rev Sociol. 2002;28(1):443–78. doi: 10.1146/annurev.soc.28.110601.141114. [DOI] [Google Scholar]
- 50.Coulton CJ, Korbin J, Chan T, Su M. Mapping residents’ perceptions of neighborhood boundaries: a methodological note. Am J Community Psychol. 2001;29(2):371–83. doi: 10.1023/A:1010303419034. [DOI] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Supplementary Materials
(DOCX 171 kb)