Abstract
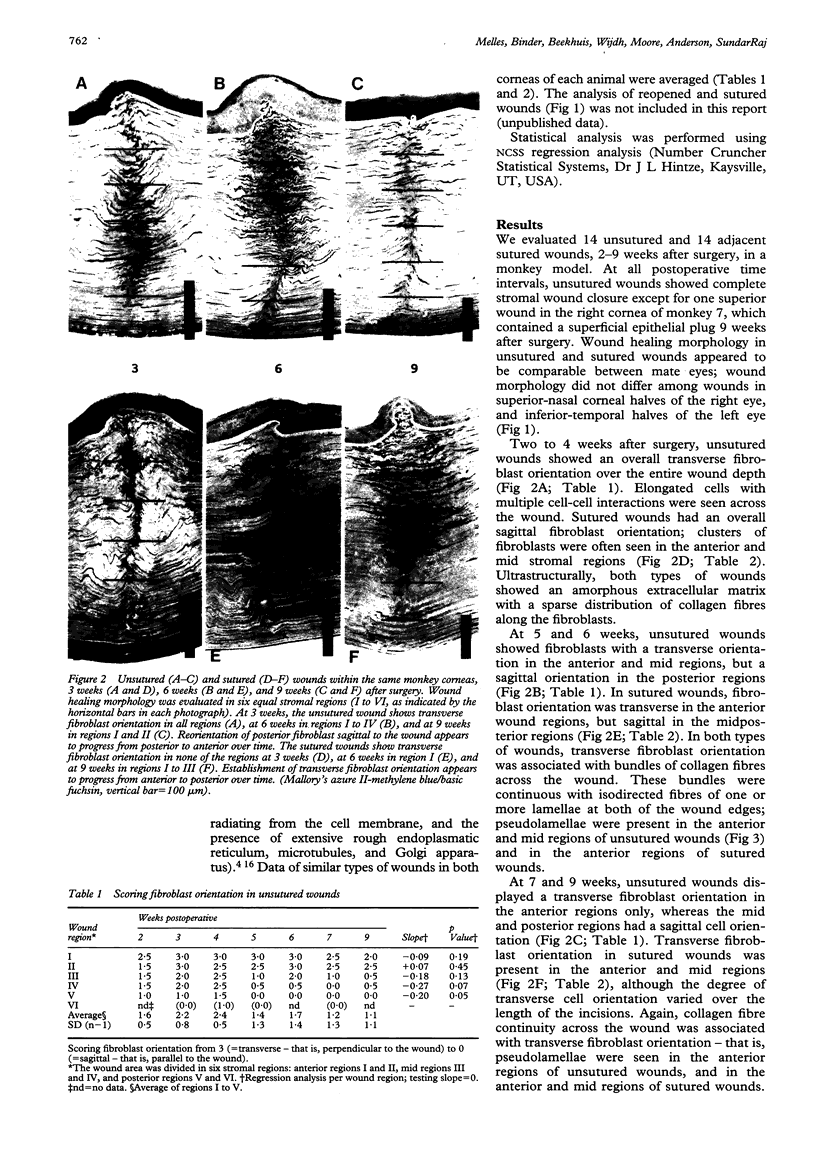
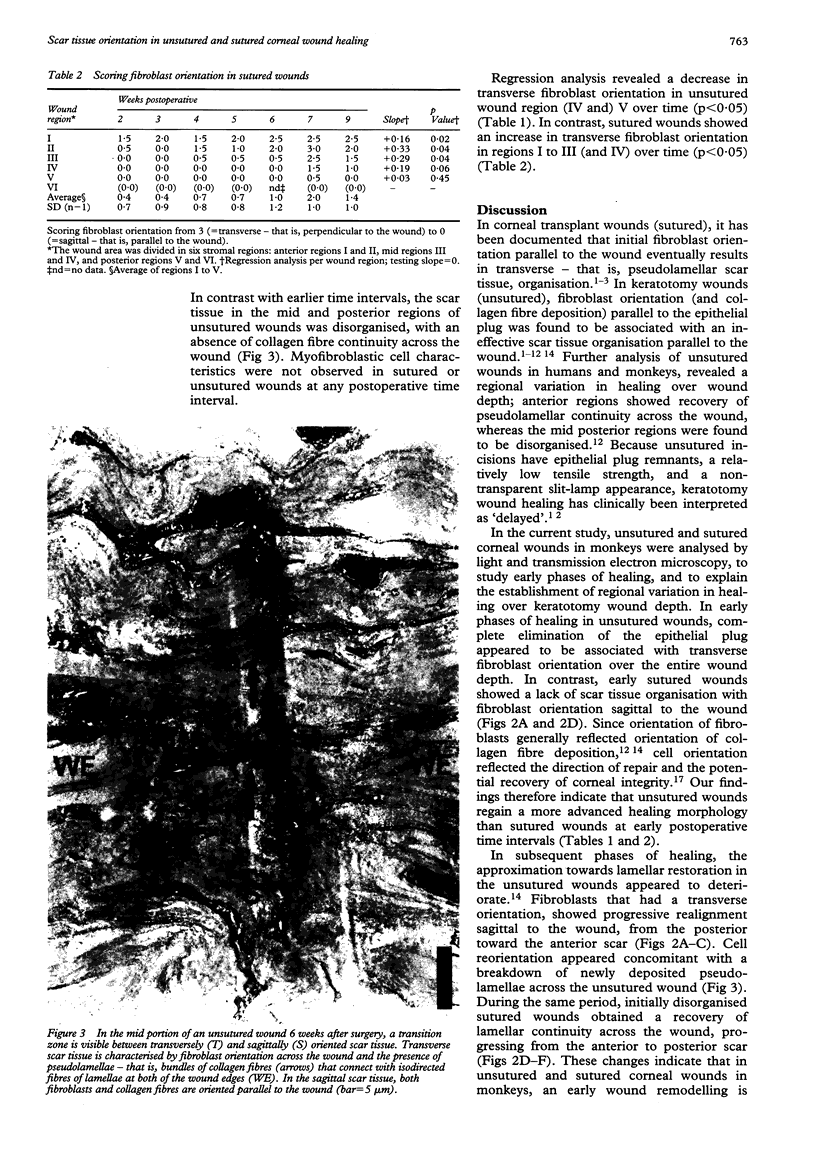
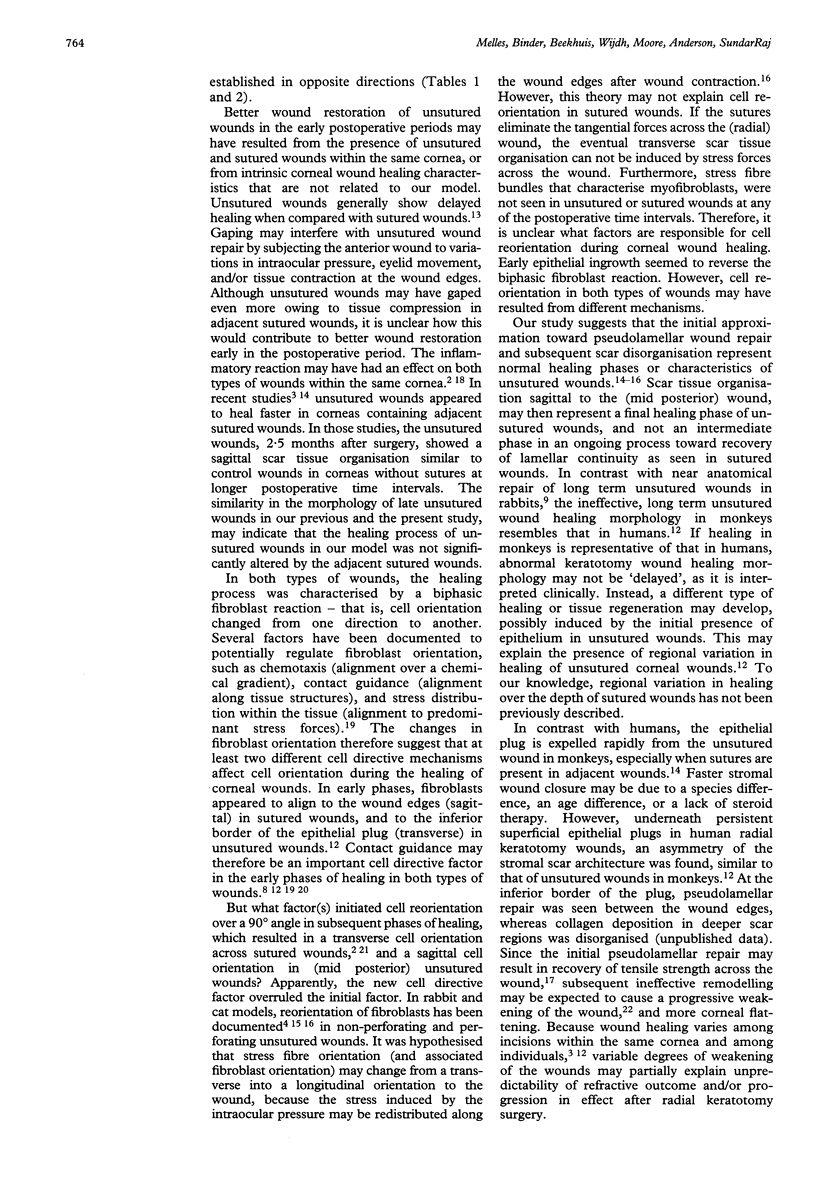
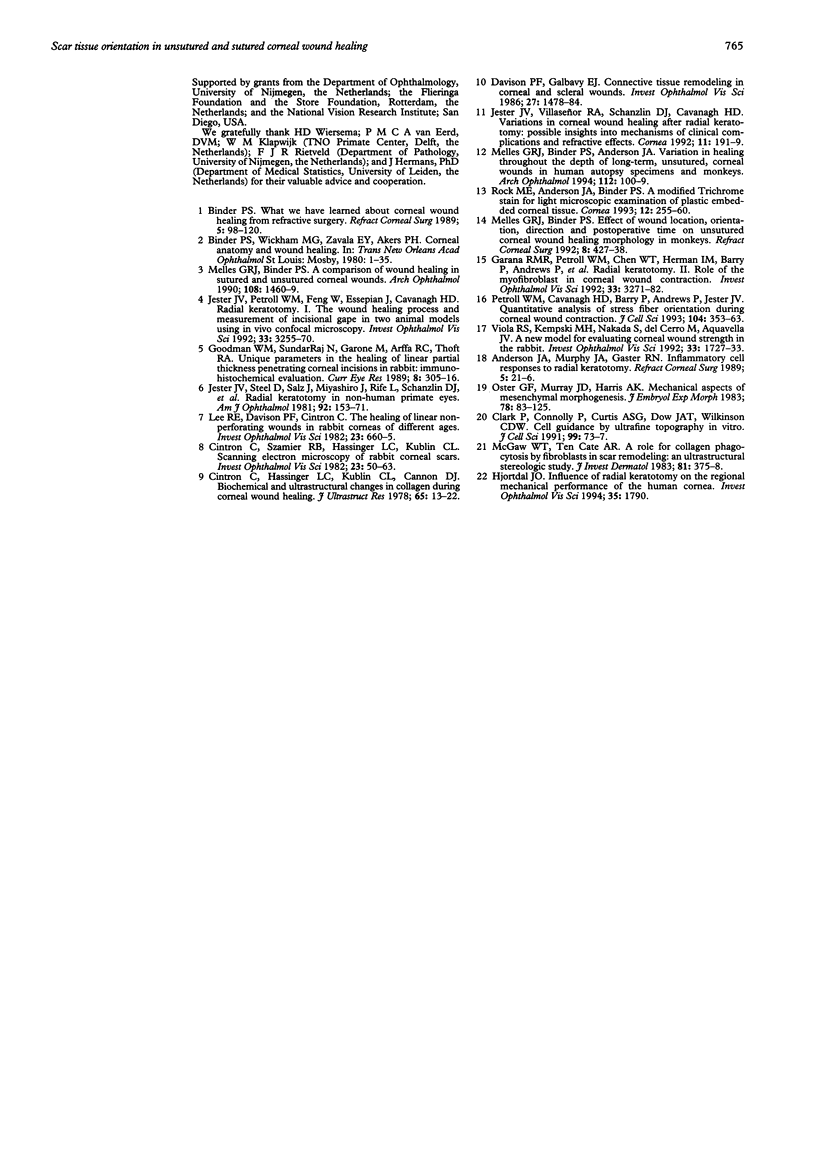
AIMS--This study aimed to evaluate stromal wound healing morphology in short term unsutured compared with sutured corneal wounds, to define regional variation in healing within radial keratotomy wounds. METHODS--Stromal scar tissue orientation (fibroblast and collagen fibre orientation) was analysed in unsutured and adjacent sutured keratotomy wounds in monkeys, 2 to 9 weeks after surgery, using light and transmission electron microscopy. RESULTS--At 2 to 4 weeks, scar tissue orientation was transverse to the wound edge in unsutured wounds, but sagittal in sutured wounds. At 5 to 9 weeks, a reorientation of scar tissue sagittal to the wound was seen in the unsutured wounds, proceeding from the posterior to anterior wound regions. In sutured wounds, a scar tissue reorientation transverse to the wound was seen, proceeding from the anterior wound region in a posterior direction. CONCLUSIONS--Within the same cornea, sutured and unsutured wounds showed opposite patterns of healing. Sutured wounds initially healed more slowly, but obtained pseudolamellar continuity over time. In contrast, healing of unsutured wounds was characterised by an early approximation towards lamellar repair that was followed by an ineffective reorganisation of the scar. This latter pattern of healing, that may be associated with a variable weakening of the wound, may relate to the clinical findings of unpredictability and/or progression of refractive effect following radial keratotomy.
Full text
PDF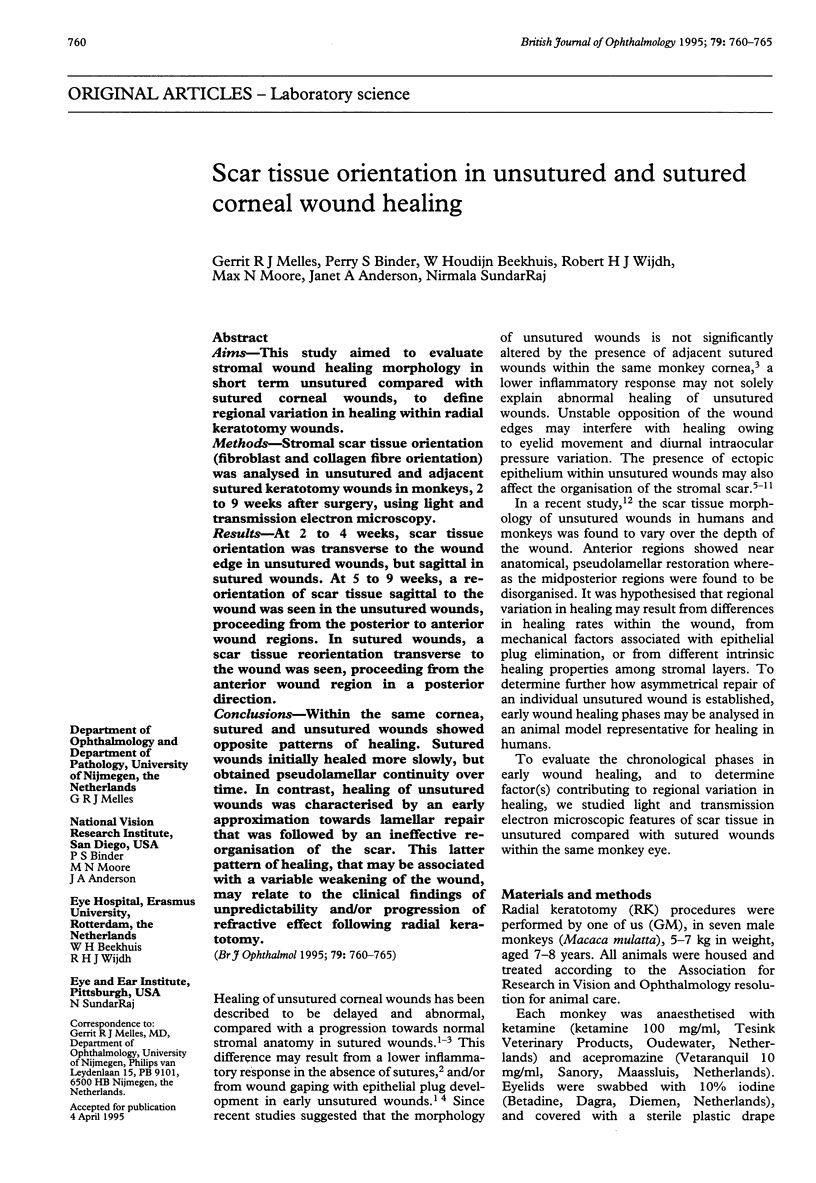
Images in this article
Selected References
These references are in PubMed. This may not be the complete list of references from this article.
- Anderson J. A., Murphy J. A., Gaster R. N. Inflammatory cell responses to radial keratotomy. Refract Corneal Surg. 1989 Jan-Feb;5(1):21–26. [PubMed] [Google Scholar]
- Binder P. S. Barraquer lecture. What we have learned about corneal wound healing from refractive surgery. Refract Corneal Surg. 1989 Mar-Apr;5(2):98–120. [PubMed] [Google Scholar]
- Cintron C., Hassinger L. C., Kublin C. L., Cannon D. J. Biochemical and ultrastructural changes in collagen during corneal wound healing. J Ultrastruct Res. 1978 Oct;65(1):13–22. doi: 10.1016/s0022-5320(78)90017-5. [DOI] [PubMed] [Google Scholar]
- Cintron C., Szamier R. B., Hassinger L. C., Kublin C. L. Scanning electron microscopy of rabbit corneal scars. Invest Ophthalmol Vis Sci. 1982 Jul;23(1):50–63. [PubMed] [Google Scholar]
- Clark P., Connolly P., Curtis A. S., Dow J. A., Wilkinson C. D. Cell guidance by ultrafine topography in vitro. J Cell Sci. 1991 May;99(Pt 1):73–77. doi: 10.1242/jcs.99.1.73. [DOI] [PubMed] [Google Scholar]
- Davison P. F., Galbavy E. J. Connective tissue remodeling in corneal and scleral wounds. Invest Ophthalmol Vis Sci. 1986 Oct;27(10):1478–1484. [PubMed] [Google Scholar]
- Garana R. M., Petroll W. M., Chen W. T., Herman I. M., Barry P., Andrews P., Cavanagh H. D., Jester J. V. Radial keratotomy. II. Role of the myofibroblast in corneal wound contraction. Invest Ophthalmol Vis Sci. 1992 Nov;33(12):3271–3282. [PubMed] [Google Scholar]
- Goodman W. M., SundarRaj N., Garone M., Arffa R. C., Thoft R. A. Unique parameters in the healing of linear partial thickness penetrating corneal incisions in rabbit: immunohistochemical evaluation. Curr Eye Res. 1989 Mar;8(3):305–316. doi: 10.3109/02713688908997573. [DOI] [PubMed] [Google Scholar]
- Jester J. V., Petroll W. M., Feng W., Essepian J., Cavanagh H. D. Radial keratotomy. 1. The wound healing process and measurement of incisional gape in two animal models using in vivo confocal microscopy. Invest Ophthalmol Vis Sci. 1992 Nov;33(12):3255–3270. [PubMed] [Google Scholar]
- Jester J. V., Steel D., Salz J., Miyashiro J., Rife L., Schanzlin D. J., Smith R. E. Radial keratotomy in non-human primate eyes. Am J Ophthalmol. 1981 Aug;92(2):153–171. doi: 10.1016/0002-9394(81)90764-9. [DOI] [PubMed] [Google Scholar]
- Jester J. V., Villaseñor R. A., Schanzlin D. J., Cavanagh H. D. Variations in corneal wound healing after radial keratotomy: possible insights into mechanisms of clinical complications and refractive effects. Cornea. 1992 May;11(3):191–199. [PubMed] [Google Scholar]
- Lee R. E., Davison P. F., Cintron C. The healing of linear nonperforating wounds in rabbit corneas of different ages. Invest Ophthalmol Vis Sci. 1982 Nov;23(5):660–665. [PubMed] [Google Scholar]
- McGaw W. T., Ten Cate A. R. A role for collagen phagocytosis by fibroblasts in scar remodeling: an ultrastructural stereologic study. J Invest Dermatol. 1983 Oct;81(4):375–378. doi: 10.1111/1523-1747.ep12519983. [DOI] [PubMed] [Google Scholar]
- Melles G. R., Binder P. S. A comparison of wound healing in sutured and unsutured corneal wounds. Arch Ophthalmol. 1990 Oct;108(10):1460–1469. doi: 10.1001/archopht.1990.01070120108039. [DOI] [PubMed] [Google Scholar]
- Melles G. R., Binder P. S., Anderson J. A. Variation in healing throughout the depth of long-term, unsutured, corneal wounds in human autopsy specimens and monkeys. Arch Ophthalmol. 1994 Jan;112(1):100–109. doi: 10.1001/archopht.1994.01090130110027. [DOI] [PubMed] [Google Scholar]
- Melles G. R., Binder P. S. Effect of wound location, orientation, direction, and postoperative time on unsutured corneal wound healing morphology in monkeys. Refract Corneal Surg. 1992 Nov-Dec;8(6):427–438. [PubMed] [Google Scholar]
- Oster G. F., Murray J. D., Harris A. K. Mechanical aspects of mesenchymal morphogenesis. J Embryol Exp Morphol. 1983 Dec;78:83–125. [PubMed] [Google Scholar]
- Petroll W. M., Cavanagh H. D., Barry P., Andrews P., Jester J. V. Quantitative analysis of stress fiber orientation during corneal wound contraction. J Cell Sci. 1993 Feb;104(Pt 2):353–363. doi: 10.1242/jcs.104.2.353. [DOI] [PubMed] [Google Scholar]
- Rock M. E., Anderson J. A., Binder P. S. A modified trichrome stain for light microscopic examination of plastic-embedded corneal tissue. Cornea. 1993 May;12(3):255–260. doi: 10.1097/00003226-199305000-00012. [DOI] [PubMed] [Google Scholar]
- Viola R. S., Kempski M. H., Nakada S., del Cerro M., Aquavella J. V. A new model for evaluating corneal wound strength in the rabbit. Invest Ophthalmol Vis Sci. 1992 Apr;33(5):1727–1733. [PubMed] [Google Scholar]