Abstract
Background
Photographing injuries in the acute setting allows for improved documentation as well as assessment by clinicians and others who have not personally examined a patient. This tool is important, particularly for telemedicine, tracking of wound healing, the evaluation of potential abuse, and injury research. Despite this, protocols to ensure standardization of photography in clinical practice, forensics, or research have not been published. In preparation for a study of injury patterns in elder abuse and geriatric falls, our goal was to develop and evaluate a protocol for standardized photography of injuries that may be broadly applied.
Methods
We conducted a literature review for techniques and standards in medical, forensic, and legal photography. We developed a novel protocol describing types of photographs and body positioning for eight body regions, including instructional diagrams. We revised it iteratively in consultation with experts in medical photography; forensics; and elder, child, and domestic abuse. The resulting protocol requires a minimum of four photos of each injury at multiple distances with and without a ruler/color guide. To evaluate the protocol’s efficacy, multiple research assistants without previous photography experience photographed injuries from a convenience sample of elderly patients presenting to a single large, urban, academic emergency department. A selection of these patients’ images were then evaluated in a blinded fashion by four nontreating emergency medicine physicians and the inter-rater reliability between these physicians was calculated.
Results
Among the 131 injuries, from 53 patients, photographed by 18 photographers using this protocol, photographs of 25 injuries (10 bruises, seven lacerations, and eight abrasions) were used to assess characterization of the injury. Physicians’ characterizations of the injuries were reliable for the size of the injury (κ = 0.91, 95% confidence interval [CI] = 0.77 to 1.00), side of the body (κ = 0.97, 95% CI = 0.88 to 1.00), precise location of the injury (κ = 0.74, 95% CI = 0.63 = 0.81), and type of abrasion (κ = 0.76, 95% CI = 0.45 to 1.00). The exact shape of the injury (κ = 0.44, 95% CI = 0.17 to 0.51), and the primary color of bruises (κ = 0.37, 95% CI = 0.25 to 0.48) were not as reliably characterized.
Conclusions
Standardizing the documentation of injuries with photographs for clinical and research assessment can be conducted by nonprofessional photographers. A photography protocol will ensure that this important mechanism for documentation is optimized.
Photographs provide a reliable, highly detailed record of an injury, including its precise location, size, and color, among other characteristics. Written documentation often lacks this detail and precision due to clinicians’ time limitations, the difficulty of accurately describing injuries in the electronic medical record, and the perceived importance of minor injuries. As electronic medical records begin to allow for the inclusion of photographs, it is likely that digital photography will significantly increase in the acute care setting.
Photographing injuries in the acute care setting is clinically important and also allows for the collection of information that can be later utilized by future clinicians to improve care, including return visit reassessment by different providers. This has particular utility for telemedicine,1 tracking of wound healing,2 medicolegal assessment of assault,3,4 and provider education.
Photographs are particularly important for researchers investigating injury patterns, as they provide a reliable record of every injury a subject has which can be comprehensively evaluated by multiple members of a research team who have not examined the subject. Using photographs may also facilitate the analysis of small, superficial injuries that may be omitted from clinical documentation but contribute significantly to identifying injury patterns and mechanisms of injury. Additionally, the ability to store photographs over time may allow for the development of photographic data-banks that can be used for future investigation.
As photography has an important role in current clinical1,5 and legal practice,4,6 and the potential to benefit other practice areas,2,7,8 there exist many instructional guidebooks and articles of “tips” for untrained photographers to take legally defensible photographs.9,10 These include recommendations for photography in sexual assault examinations from the United States Department of Justice11 and the American College of Emergency Physicians.12 However, we were unable to identify any existing published protocols that 1) described techniques for optimizing photographs of all major parts of the body, 2) included recommendations for appropriate positioning to photograph each body part, and 3) systematically evaluated the effectiveness of the protocol to generate photographs for clinical practice or research that were interpretable by others who had not seen the patient. In preparation for a study of injury patterns in elder abuse and accidental falls, our goal was to develop and evaluate a novel protocol to standardize the photography of injury types in all major body regions.
METHODS
Study Design, Setting, and Population
We used a multiphase process to design, implement, and evaluate the effectiveness of a comprehensive protocol describing techniques for photographing injuries in an acute care setting. We conducted this study in the emergency department (ED) of a large, urban, academic medical center. This protocol was designed to facilitate the prospective evaluation of injuries in geriatric (≥60 years) ED patients presenting after an accidental fall as part of a larger investigation into injury patterns indicative of elder abuse. These subjects were enrolled from September 2014 to June 2015. Recruitment was conducted from 7:30 am to 11:30 pm by the research team, who approached a convenience sample of potential subjects who presented to the ED after an accidental fall. Potential subjects were excluded if they had critical illness requiring emergent resuscitation, they did not speak English, or they or a proxy were unable to provide informed consent. Each enrollee was screened to ensure that they were not a victim of elder abuse. This project was reviewed and approved by the Weill Cornell Institutional Review Board.
Literature Review (Phase 1)
We conducted a nonsystematic literature review to identify existing descriptions of techniques and standards in medical, forensic, and legal photography. We searched the Medline and Scopus databases, using terms “photograph”/“photographs”/“photography” and “protocol”/“guidelines”/“methods”/“manual.” Further searches within these databases were conducted to identify instructions specific to photographing injury types or body regions. We also conducted general internet searches using Google and Google Scholar for protocols from sexual assault and domestic violence organizations using the search terms described above in combination with: “medical,” “forensic,” and “legal.” We reviewed existing textbooks and consulted experts in medical photography, forensics, child abuse, domestic violence, elder abuse, and injury research for additional guidance and to ensure that a comprehensive protocol instructing lay people on photography was not available. We focused our searches on descriptions of photography technique and how to optimize body positioning. Given our future research goals, we also focused on photographic documentation of violence-related injuries for legal purposes. We excluded photography of intraoral and genital injuries from our protocol. Many protocols provide detailed instructions and techniques for photographing injuries in these challenging and sensitive areas,11,12 typically for victims of sexual assault. In many clinical settings, photographs of these areas are taken by specialists, such as sexual assault nurse examiners, who often have additional training in photographic techniques. The availability of these professionals is expanding, reducing the need for emergency physicians to take these photos. In circumstances where trained professionals are not available, we would recommend that physicians consult the available specialized protocols and guidance. We also excluded descriptions of the use of ultraviolet light and other advanced imaging modalities to photograph injuries not visible to the naked eye as they are less feasible in the busy ED setting.6,13,14
Synthesis/Development (Phase 2)
We synthesized information from this literature review and the preliminary advice from experts to collaboratively develop a comprehensive protocol to standardize photography of injuries by untrained photographers. This protocol describes general principles to optimize the quality and interpretability of photographs, procedures to ensure that an injury is completely visualized, specific instructions for photographing different body regions, and consideration of the subject’s comfort and dignity.
General Principles to Optimize Quality and Interpretability
To optimize the quality and interpretability of the images produced, our protocol incorporates several principles from existing literature. To produce an image that is not distorted the camera should be held at a 90° angle to the plane of the injury area to be photographed.15 A ruler placed in the image next to the injury and held 1–2 inches from the skin16 by an assistant, or the subject, should be used to allow for assessment of injury size.16 Although holding the ruler at different distances from the injury may cause some variation, placing the ruler directly on the subject’s skin and therefore bending the ruler to follow the curvature of the body part may lead to significant distortion.15 A standard color guide should also be included in the image to allow for calibration across photos and lighting environments.16 This is particularly useful in an ED setting where changing the light around a patient may not be possible. Forensic literature emphasizes the importance of having identifying information in all photos, such as the subject’s face or hospital identification band, to remove doubt about the identity of subject in the photos.4,17 Given that our protocol has been initially designed for use in research, and we prioritized limiting the risk of a loss of confidentiality, we recommended that images should only include the patient’s face, or other identifiable features, if the injury is located in that particular area.
For use with this protocol, we designed a ruler with a color guide and area to label the subject’s study identification number and/or medical record number (Figure 1). We chose to use a ruler rather than an existing standardized forensic scale (e.g., American Board of Forensic Odontology Number 2 Standard Reference Scale18) with the goal of developing a simple process that could be easily replicated without specialized tools. Notably, forensic scales are often L-shaped allowing for simultaneous measurement in two directions, particularly to facilitate the characterization of bites, and are typically small, optimized to photograph genital injuries after assault. In current forensic photography practice, the reference scale is typically saved as a piece of evidence associated with the patient and is not reused, limiting the ready availability of these scales. We envision that photography of injuries may become a practice that occurs commonly, potentially in triage, for all injured patients, and this approach would improve feasibility. We chose to use a large, straight ruler, as we anticipated needing to photograph larger injuries on other parts of the body which may be occluded by an L-arm and poorly characterized with a small scale. Similarly, standard color scales are available for forensic photography.19 We chose to design our own color scale on a ruler rather than using a standard one to further our goal of developing a simple process that could be easily replicated without specialized tools.
Figure 1.
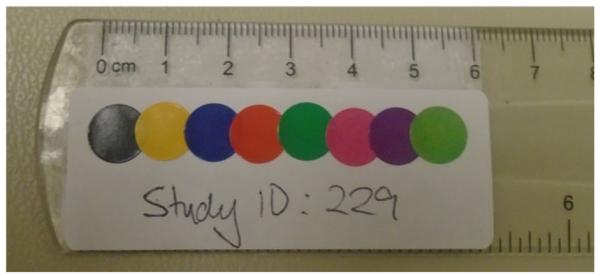
Ruler, color guide, and identifier label.
Procedures to Ensure Complete Visualization
To ensure that an injury may be completely visualized, the protocol recommends taking photographs from two distances, a medium distance (~3 feet from injury) that ensures that an entire body part can be visualized (i.e., the entire arm) and close up (~1 foot from injury), which gives a better visualization of the injury.15,17 Although measurement of these distances between the injury and the camera would have added precision, we decided to allow photographers to estimate distances. While this may have caused some inconsistency in the results, we thought that measurement would be impractical and difficult to accomplish in a busy ED. Photographs should be taken at each distance with and without the ruler/color guide,3 to ensure that the ruler is not covering any part of an injury. Each injury is therefore photographed at least four times (Figure 2). For smaller injuries (approximately less than 3 cm in length), we recommend taking at least two additional super closeup images (one with and one without the ruler/color guide) using the zoom function to capture the injury in detail. As the digital zoom function may distort an image, photographers should only use the optical zoom. Furthermore, we would recommend the macro setting for acquisition of super close-up images.
Figure 2.
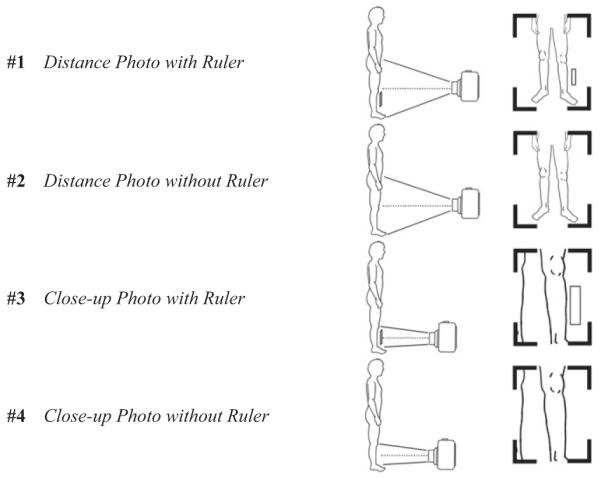
Diagram depicting the four pictures to be taken of every injury at two distances.
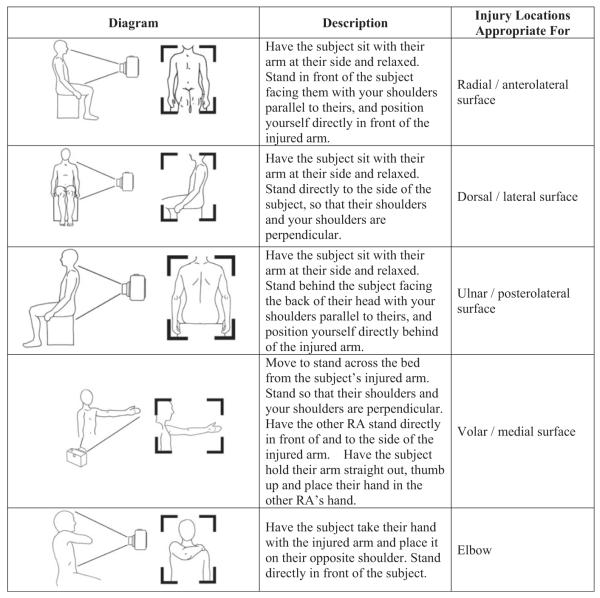
Specific Instructions for Photographing Different Body Regions
The developed protocol includes instructions for appropriate body positioning to photograph injuries in 33 locations on eight body regions (Table 1). Body positioning is important for image standardization as it will affect how the image is captured, particularly if lighting creates glare.5,16 These positions were based on existing literature when available5,16 and modified when possible to limit movement in subjects who may have acute pain or unstable injuries (e.g., fractures, dislocations). Diagrams depicting appropriate body and camera positioning for each location were created by one of the authors (JC) and are accompanied by written instructions. Figure 3 provides a sample from the protocol describing appropriate body positioning for five locations on a subject’s arm.
Table 1.
Body Regions and Specific Locations for Photography
| Body Region | Specific Locations |
|---|---|
| Skull | Back of head* Side of head Top of head |
| Face and neck | Face Center of neck Side of neck |
| Arms | Radial/anterolateral surface Dorsal/lateral surface Ulnar/posterolateral surface Volar/medial surface Elbow |
| Hand | Palmar hand Dorsal hand Lateral/medial finger |
| Leg | Anterior leg–able to stand Anterior leg–unable to stand Posterior leg–able to stand Posterior leg–unable to stand Medial leg Lateral leg Knee–able to sit Knee–unable to sit |
| Foot | Dorsal foot–able to place foot on floor Dorsal foot–unable to place foot on floor Plantar foot Lateral/ medial foot |
| Back | Back–able to sit Back–unable to sit |
| Chest, abdomen, pelvis, and buttocks |
Chest and abdomen–front view Chest and abdomen–side view Pelvis Buttocks |
This view can also be used to photograph the back of the neck.
Figure 3.
Example protocol: positioning for the arm.
Consideration of Comfort and Dignity
Our protocol also emphasizes consideration for the comfort and dignity of the subject, who may be an ED patient in acute pain. All planned procedures should be explained clearly and completely to the subject, and informed consent should be obtained.20 Any uninjured area of the body should be covered with a sheet or blanket.4 If sensitive parts of the body need to be photographed, a chaperone of the same sex and gender as the subject should be present.
Implementation/Training (Phase 3)
Our initial protocol was reviewed by experts and revised based on their recommendations. The protocol was then pilot tested by three of the authors (EMB, TR, MRM), who photographed injuries from 20 patients and made additional modifications to improve ease of use. The complete finalized protocol is available as an online supplement to this article and at http://nyceac.com/wpcontent/uploads/2012/02/Photography-Protocol.pdf.
Photography using the finalized protocol was conducted by research associates (RAs), who recruit and enroll subjects into prospective research studies within our ED. These RAs, typically undergraduate students interested in medical careers, receive research education and training. The use of RAs is common in emergency medicine research and is well described.21–23 None of the RAs participating in this study had previous formal photography training. RAs worked in teams of two, with one taking the photographs and the other assisting with body positioning and holding the ruler. We chose to have photography conducted in teams of two as we anticipated that acutely injured older adults might have difficulty moving and maintaining body positions and to allow the photographer to focus on taking photographs. All photographs were taken with a Sony Cyber-shot DSC-W800 point-and-shoot digital camera. The photographs used in this evaluation were taken as part of a study evaluating injuries in ED patients aged ≥60 years presenting after a fall. Each subject provided consent for his or her injuries to be photographed and for the photographs to be used for research. The photographs were not added to the patient’s electronic medical record.
RAs were initially trained on the photography protocol with a 10-minute lecture. At that time, each RA also received a written copy of the protocol and was asked to review it before enrolling patients. Before independently photographing subjects, each RA observed a member of the research team photograph one subject’s injuries and was then observed by a member of the research team photographing another subject’s injuries. Using the protocol to photograph an injury typically took a team of two RAs less than 2 minutes and photographing multiple injuries on a patient took less than 5 minutes. The time required to take photographs may be longer with a single photographer not working in a team or for patients with many injuries.
Evaluation (Phase 4)
To evaluate the efficacy of the protocol, we examined the ability of experienced emergency physicians, who had not evaluated a subject in person, to accurately characterize in detail injuries based on the photographs produced. This was done after the protocol had been in use for 6 months and had been used by 18 RA photographers to photograph 131 injuries in 53 subjects for the parent study.
To evaluate the reliability of the protocol, the lead author (EMB) selected 25 injuries as a representative sample. Injuries were selected to ensure representation of all major body regions (face, skull, arms, hands, and legs) and multiple injury types (bruises, lacerations, and abrasions). As the large majority of subjects were white, all injuries from nonwhite participants were included. Injuries were excluded from consideration for inclusion if the photographer was judged to have not followed the protocol, typically due to an insufficient number of photos taken. All of the injury photographs and the selections for evaluation were subsequently reviewed by another author (SC) to reduce bias.
The injuries selected included 10 bruises, eight abrasions, and seven lacerations on subjects’ faces, heads, arms, hands, and legs. Subjects with injury photographs included in this evaluation were 48% female and 95% white and had a mean age of 80 (SD, 9) years.
For each injury, four emergency physicians were asked to describe characteristics of an injury including precise location, shape, length, and side of body (if appropriate). For abrasions, we also asked physicians to characterize the type of abrasion and, for bruises, we asked them to characterize the predominant color. We compared the injury descriptions from these physicians to assess the inter-rater reliability of photographs taken using this protocol to characterize an injury. Physicians evaluating the injury photographs were members of the research team (TR, MRM, MES, RM) with a mean of 4 years of experience as an emergency medicine attending physician.
For precise location, physicians were given a list of body regions for the injury and asked to check all that applied. For shape, physicians were given an injury type–specific list of options and asked to select the most appropriate. An “other” option was included. For length, the physician was given a blank and asked to write the length in centimeters. For side of body, physicians were asked to select “left” or “right.” For abrasion type, the physicians were given a list, including scuff/brush, linear/ scratch, point/gouge, crush, and other. For predominant color of bruise, physicians were given a list, including purple, blue, black, red, green, and yellow.
RESULTS
The level of agreement of the physicians’ characterizations of the injuries is described in Table 1. Physicians reliably characterized the size of the injury (κ = 0.91, 95% confidence interval [CI] = 0.77 to 1.00), the side of the body (κ = 0.97, 95% CI = 0.88 to 1.00), the precise location of the injury (κ = 0.74, 95% CI = 0.63 to 0.81), and the type of abrasion (κ = 0.76, 95% CI = 0.45 to 1.00). The exact shape of the injury (κ = 0.44, 95% CI = 0.17 to 0.51) and the predominant color of bruises (κ = 0.37, 95% CI = 0.25 to 0.48) were not as reliably characterized.
DISCUSSION
To our knowledge, this represents the first comprehensive protocol published describing techniques for nonprofessional photographers to photographically document injuries in the acute care setting. We used a multiphase development process to incorporate existing literature, recommendations of experts, and experience from pilot testing. We evaluated the efficacy of the protocol and have preliminarily shown that photographs taken using it may be used by physicians to accurately and reliably describe acute injuries in detail. Most areas of characterization had good reliability between providers. The shape of an injury and primary color of a bruise had poor reliability, as would be expected due to the more subjective nature of these characterizations (i.e., an oval versus a circle shape or a bruise being primarily blue rather than purple).
This protocol may have broad utility for clinical practice, forensics, and research. For practicing emergency physicians, the most immediately relevant application of this protocol is likely in the forensic evaluation of child abuse, intimate partner violence, and elder abuse. Emergency physicians are responsible for documenting injuries in these vulnerable patients, yet they typically receive very little training in the acquisition of a photo image, forensic evaluation, and documentation24,25 and may feel uncomfortable performing these tasks without tools and protocols to help guide this process. Additionally, standardizing this process through a protocol will improve the quality of photos and their utility in any future legal process.
With many electronic medical records now allowing inclusion of digital photographs, emergency physicians may in the future become responsible for photographing acute injuries and other physical findings. Using this protocol will assist providers in producing images that are most useful for future clinicians or other applicable parties. Before initiating ED-based photography of injuries for clinical purposes, we would recommend that physicians consult their hospital’s legal department regarding issues surrounding patient consent and privacy, which may vary according to hospital policy or by jurisdiction.
LIMITATIONS
This protocol has been implemented and evaluated using older adult research subjects in an acute care setting and may require modifications for other uses, populations, and settings. Our preliminary validation of the protocol has only been conducted in a single, large, academic, urban ED and may not be generalizable to other settings. While we attempted to select representative injuries for evaluation, the selection process may have introduced bias that affected our results. Also, we excluded injuries where the photographs were judged to have not been taken according to the protocol. Doing so may have increased the inter-rater reliability we found. Notably, the majority of the subjects were white, which may impact the generalizability of the techniques to other racial and ethnic groups as characterizing injuries and dermatologic conditions among other skin tones is known to be challenging and often requires different techniques.26,27 Given that our protocol recommended taking photographs at estimated distances of ~3 feet and ~1 foot from the injury without confirmatory measurement, variability may have been introduced into our findings for which we did not account. Also, photographs included in this evaluation did not include heavy tattoos, significant previous scarring, or injuries located under heavily haired areas or within natural skin folds, which have been shown to increase difficulty in interpreting photographic images.28–30 The physicians who evaluated the photos were not screened for color blindness or other vision issues, which may have impacted these results. Future research objectives include additional validation of this protocol in other clinical settings and for other patient populations and modifying the protocol for other uses.
CONCLUSION
Photographing injuries for clinical and research assessment can be standardized and conducted by nonprofessional photographers. Use of a comprehensive photography protocol will ensure that this potentially invaluable tool is optimized.
Supplementary Material
Acknowledgments
The authors thank Dr. Veronica LoFaso for her tremendous support of our work as well as all of the volunteer research associates who assisted with this project.
Our work was supported by a GEMSSTAR (Grants for Early Medical and Surgical Subspecialists’ Transition to Aging Research) grant from the National Institute on Aging (R03 AG048109). Tony Rosen is also the recipient of a Jahnigen Career Development Award, supported by the John A. Hartford Foundation, the American Geriatrics Society, the Emergency Medicine Foundation, and the Society of Academic Emergency Medicine. Mark Lachs is the recipient of a mentoring award in patient-oriented research from the National Institute on Aging (K24 AG022399).
Footnotes
Preliminary versions of this work were presented at the Society of Academic Emergency Medicine Annual Meeting, San Diego, CA, May 12–15, 2015; and the American Geriatrics Society Annual Scientific Meeting, National Harbor, MD, May 14–17, 2015.
The authors have no relevant financial information or potential conflicts to disclose.
Supervising Editor: Kabir Yadav, MDCM, MS, MSHS.
References
- 1.Chanussot-Deprez C, Contreras-Ruiz J. Telemedicine in wound care: a review. Adv Skin Wound Care. 2013;26:78–82. doi: 10.1097/01.ASW.0000426717.59326.5f. [DOI] [PubMed] [Google Scholar]
- 2.Gabison S, McGillivray C, Hitzig SL, Nussbaum E. A study of the utility and equivalency of 2 methods of wound measurement: digitized tracing versus digital photography. Adv Wound Care. 2015;28:252–8. doi: 10.1097/01.ASW.0000465301.37313.57. [DOI] [PubMed] [Google Scholar]
- 3.Pasqualone GA. Forensic RNs as photographers. Documentation in the ED. J Psychosoc Nurs Ment Health Serv. 1996;34:47–51. doi: 10.3928/0279-3695-19961001-12. [DOI] [PubMed] [Google Scholar]
- 4.Kodner C, Wetherton A. Diagnosis and management of physical abuse in children. Am Fam Physician. 2013;88:669–75. [PubMed] [Google Scholar]
- 5.Smoot EC, Higgs J. Photographing the patient with burns for medical documentation. J Burn Care Res. 1994;15:434–7. doi: 10.1097/00004630-199409000-00011. [DOI] [PubMed] [Google Scholar]
- 6.Barsley RE, West MH, Fair JA. Forensic photography. Ultraviolet imaging of wounds on skin. Am J Forensic Med Pathol. 1990;11:300–8. [PubMed] [Google Scholar]
- 7.Stockton KA, McMillan CM, Storey KJ, David MC, Kimble RM. 3D photography is as accurate as digital planimetry tracing in determining burn wound area. Burns. 2015;41:80–4. doi: 10.1016/j.burns.2014.04.022. [DOI] [PubMed] [Google Scholar]
- 8.Perednia DA, Gaines JA, Butruille TW. Comparison of the clinical informativeness of photographs and digital imaging media with multiple-choice receiver operating characteristic analysis. Arch Dermatol. 1995;131:292–7. [PubMed] [Google Scholar]
- 9.Verhoff MA, Kettner M, Laszik A, Ramsthaler F. Digital photo documentation of forensically relevant injuries as part of the clinical first response protocol. Dtsch Arztebl Int. 2012;109:638–42. doi: 10.3238/arztebl.2012.0638. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Ozkalipci O, Volpellier M. Photographic documentation, a practical guide for non professional forensic photography. Torture. 2010;20:45–52. [PubMed] [Google Scholar]
- 11.Office on Violence Against Women. U.S. Department of Justice [Accessed Nov 27, 2015];A National Protocol for Sexual Assault Medical Forensic Examinations: Adults/Adolescents. Available at: https://www.ncjrs.gov/pdffiles1/ovw/241903.pdf.
- 12.American College of Emergency Physicians [Accessed Nov 27, 2015];Evaluation and Management of the Sexually Assaulted or Sexually Abused Patient. Available at: http://www.acep.org/workarea/downloadasset.aspx?id=8984.
- 13.Lynnerup N, Hjalgrim H, Eriksen B. Routine use of ultraviolet light in medicolegal examinations to evaluate stains and skin trauma. Med Sci Law. 1995;35:165–8. doi: 10.1177/002580249503500211. [DOI] [PubMed] [Google Scholar]
- 14.Vogeley E, Pierce MC, Bertocci G. Experience with wood lamp illumination and digital photography in the documentation of bruises on human skin. Arch Pediatr Adolesc Med. 2002;156:265–8. doi: 10.1001/archpedi.156.3.265. [DOI] [PubMed] [Google Scholar]
- 15.Evans S, Baylis S, Carabott R, et al. Focussing on the future: survey results on the image capture of patterned cutaneous injuries. J Forensic Leg Med. 2014;24:7–11. doi: 10.1016/j.jflm.2014.02.007. [DOI] [PubMed] [Google Scholar]
- 16.Evans S, Baylis S, Carabott R, et al. Guidelines for photography of cutaneous marks and injuries: a multi-professional perspective. J Vis Commun Med. 2014;37:3–12. doi: 10.3109/17453054.2014.911152. [DOI] [PubMed] [Google Scholar]
- 17.Recommended Guidelines [Accessed Nov 27, 2015];Washington State. Sexual Assault Emergency Medical Evaluation Adult and Adolescent. 2010 Available at: https://depts.washington.edu/hcsats/PDF/guidelines/Adult%20Adolescent%20Recommended%20Guidelines%202010.pdf.
- 18.Ferrucci M, Doiron TD, Thompson RM, Jones JP, Ballou SM, Neiman JA, National Institute of Standards and Technology [Accessed Nov 27, 2015];Dimensional Review of Scales for Forensic Photography. 2010 Available at: http://www.nist.gov/forensics/research/upload/Dimensional-Review-of-Scales-for-Forensic-Photography.pdf.
- 19.Nuzzolese E, Di Vella G. The development of a colorimetric scale as a visual aid for the bruise age determination of bite marks and blunt trauma. J Forensic Odontostomatol. 2012;30:1–6. [PMC free article] [PubMed] [Google Scholar]
- 20.Dysmorphology Subcommittee of the Clinical Practice Committee. American College of Medical Genetics Informed consent for medical photographs. Genet Med. 2000;2:353–5. doi: 10.1097/00125817-200011000-00010. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21.Sparano DM, Shofer FS, Hollander JE. Participation in the academic associate program: effect on medical school admission rate. Acad Emerg Med. 2004;11:695–8. [PubMed] [Google Scholar]
- 22.Hollander JE, Singer AJ. An innovative strategy for conducting clinical research: the academic associate program. Acad Emerg Med. 2002;9:134–7. doi: 10.1111/j.1553-2712.2002.tb00230.x. [DOI] [PubMed] [Google Scholar]
- 23.Hollander JE, Valentine SM, Brogan GX., Jr. Academic associate program: integrating clinical emergency medicine research with undergraduate education. Acad Emerg Med. 1997;4:225–30. doi: 10.1111/j.1553-2712.1997.tb03747.x. [DOI] [PubMed] [Google Scholar]
- 24.Smock WS. Development of a clinical forensic medicine curriculum for emergency physicians in the USA. J Clin Forensic Med. 1994;1:27–30. doi: 10.1016/1353-1131(94)90057-4. [DOI] [PubMed] [Google Scholar]
- 25.Auten JD, Ross EM, French MA, et al. Low-fidelity hybrid sexual assault simulation training’s effect on the comfort and competency of resident physicians. J Emerg Med. 2015;48:344–50. doi: 10.1016/j.jemermed.2014.09.032. [DOI] [PubMed] [Google Scholar]
- 26.Scheinfeld N. Film photography’s limitations in imaging skin of color underlies racial imaging disparities; new digital photography features facilitate the imaging of skin of color. J Am Acad Dermatol. 2008;59:351–2. doi: 10.1016/j.jaad.2008.02.018. [DOI] [PubMed] [Google Scholar]
- 27.Ebede T, Papier A. Disparities in dermatology educational resources. J Am Acad Dermatol. 2006;55:687–90. doi: 10.1016/j.jaad.2005.10.068. [DOI] [PubMed] [Google Scholar]
- 28.Anthony EP, Godbolt A, Tang F, McMeniman EK. Malignant melanoma disguised in a tattoo. Australas J Dermatol. 2015;56:232–3. doi: 10.1111/ajd.12219. [DOI] [PubMed] [Google Scholar]
- 29.Brooks J, Behrens E, Prickett K. Painful and pruritic papules in the gray shading of a tattoo. JAMA Dermatol. 2015:1–2. doi: 10.1001/jamadermatol.2015.3448. [DOI] [PubMed] [Google Scholar]
- 30.Taylor SC. Skin of color: biology, structure, function, and implications for dermatologic disease. J Am Acad Dermatol. 2002;46:S41–62. doi: 10.1067/mjd.2002.120790. [DOI] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.