Abstract
Working from a social relationship and life course perspective, we provide generalizable population-based evidence on partnered sexuality linked to cardiovascular risk in later life using national longitudinal data from the NSHAP (N=2204). We consider characteristics of partnered sexuality of older men and women, particularly sexual activity and sexual quality, as they affect cardiovascular risk. Cardiovascular risk is defined as hypertension, rapid heart rate, elevated CRP, and general cardiovascular events. We find that older men are more likely to report being sexually active, report having sex more often and more enjoyably than are older women. Results from cross-lagged models suggest that high frequency of sex is positively related to later risk of cardiovascular events for men but not women, whereas good sexual quality seems to protect women but not men from cardiovascular risk in later life. We find no evidence that poor cardiovascular health interferes with later sexuality for either gender.
Involvement in social relationships has long been demonstrated to promote health (Umberson and Montez 2010). The sexual relationship, which we define here as either a long- or short-term connection with a partner that includes sex, particularly sexual activity and sexual intimacy, is one of the most fundamental types of social relationships, and it has long been recognized as an essential part of human life (Masters and Johnson 1966; Satcher 2001; Schnarch 1991). Yet, our scientific understanding of sexual relationships, especially the consequences of partnered sexuality for health, is in its nascent stage both theoretically and empirically. We focus on sexuality with a partner since, especially in the current cohorts of older adults, the vast majority of sex takes place with another person in a relationship (Galinsky, McClintock & Waite 2014). We work from a social relationship and life course perspective to consider how partnered sexuality modifies individuals’ life context at older ages and thus shapes cardiovascular risk. Cardiovascular risk, defined as “the presence of any physiological or functional state that is a step on the way to cardiovascular disease” (Liu and Waite 2014:404), is the leading cause of death in the U.S. (Mozzafarian et al. 2015). A large body of work points to the important role of social relationships in the development and progression of this disease (Liu and Waite 2014; Zhang and Hayward 2006).
There are several reasons to expect partnered sexuality to affect cardiovascular health. First, sexual activity is a form of exercise. During sexual intercourse as well as foreplay, both men and women experience stretching of muscles and tendons, flexion of joints, and hormone fluctuation (Frappier et al. 2013), which may promote cardiovascular fitness (Levin 2007). Yet, there are also clinical concerns that sexual activity may precipitate acute cardiac events for patients with a prior history of cardiovascular disease (Cheitlin 2003; Dahabreh and Paulus 2011; Muller et al. 1996; Stein 2000). Second, the intimacy built into a sexual relationship is a source of emotional and social support, which is a key component that defines life context and in turn shapes health (Schnarch 1991). Third, partnered sexuality and satisfaction with it may reduce exposure to stress, modify response to stress and promote recovery from stress (Ein-Dor and Hirschberger 2012), thereby reducing the risk of cardiovascular disease (Schwartz et al. 2003).
The present study provides the first generalizable, population-based evidence of the longitudinal links between partnered sexuality and cardiovascular risk in later life. Using a nationally representative longitudinal dataset from the National Social Life, Health and Aging Project (NSHAP), we assess how partnered sexual activity and sexual quality are related to cardiovascular risk for older men and women over time. The findings speak to health policy and practice as well as to our understanding of sexuality in later life.
PARTNERED SEXUALITY OF OLDER ADULTS: A SOCIAL RELATIONSHIP AND LIFE COURSE PERSPECTIVE
Increasingly, scholars build on a life course perspective to view the status and transitions of social relationships as one ages (Elder and O’Rand 1995). According to the life course perspective, the developmental tasks and challenges of life change from childhood through young adulthood, middle and older ages; men and women differ in their pathways and relationship transitions across life course stages. While much research has studied various social relationships over the life course, the sexual relationship has been largely ignored, perhaps because sex is often considered to be a private or individual behavior (Harvey, Wenzel, and Sprecher 2004). We work from the life course perspective to conceptualize partnered sexuality as a unique type of social relationship that defines the life context over the life course. As a consequence, the sexual relationship may shape individuals’ health.
Sexuality varies dynamically through the socially and biologically defined stages of life (Carpenter and DeLamater 2012; Waite and Charme 2015). Previous studies on sex and sexuality often focus on adolescence and young and middle adulthood, which are usually considered to be the most sexually active stages of life (DeLamater and Sill 2005). Scientific understanding of sexual relationships in later life is limited. A common conception is that older people do not have sex as often as their younger counterparts, and that the quality of sexual life tends to decline at older ages due to biological challenges that accompany aging (DeLamater 2012; Kinsey, Pomeroy and Martin 1998). However, recent studies show that sexuality remains important to the quality of life of many older adults (Iveniuk, Cagney, and O’Muircheartaigh 2015; Lindau et al. 2007; Stroope, McFarland and Uecker 2015). A sizeable share of both older men and older women agree that sex is a key part of their relationship and well-being (DeLamater 2012; DeLamater and Sill 2005). Indeed, some scholars argue that despite a decrease in sexual frequency, the quality of sexual life sometimes improves with age because men may gain greater voluntary control over ejaculation (DeLamater and Karraker 2009).
Sexuality at older ages, especially among the cohorts now in these ages, is almost exclusively experienced within long-established couples, virtually all of them married. Data from the National Social Life, Health, and Aging Project show that 95% of sex is within a partnered relationship for older adults. Thus, we focus here on sexual activity with a partner, mostly the spouse, and satisfaction with that experience. Although we look at partnered sex from the perspective of the individuals involved, we speak of sexual relationships, as these are the context for sex. Note that especially at older ages, not all those with partners are sexually active; among partnered men and women aged 75 and older fewer than half had any sex with their partner in the past year (Karraker and Delamater 2014; Lindau and Gavrilova 2010).
SEXUALITY AND CARDIOVASCULAR HEALTH: LIMITED CLINICAL AND COMMUNITY EVIDENCE
Cardiovascular disease (CVD) is the leading cause of death and disability for both men and women in the U.S. (Mozzafarian et al. 2015). According to the U.S. Centers for Disease Control (CDC), about 600,000 Americans die of CVD every year; this is about one in every four deaths. This problem becomes increasingly prevalent with advancing age (Go et al. 2014; Lakatta and Levy 2003). Researchers from a wide range of fields are devoted to identifying the key risk factors for CVD. However, we know little about whether and how involvement in a sexual relationship shapes cardiovascular risk.
Both empirical and theoretical research on the effects of sexuality on cardiovascular health is still rare (Dahabreh and Paulus 2011; Levine et al. 2012), and almost all focuses on the effect of sexual activity on risks of cardiovascular events (Brody 2010; Dahabreh and Paulus 2011; Levine et al. 2012). Moreover, the current limited empirical evidence on this topic is restricted to small, non-representative clinical or community samples (Dahabreh and Paulus 2011; Levine et al. 2012). For example, a Welsh longitudinal study of 914 men aged 45–59 recruited between 1979 and 1983 finds that men with more frequent sexual intercourse tend to have lower risks of experiencing ischemic stroke and coronary heart disease events during the twenty-year follow up (Ebrahim et al. 2002). Another study based on the same Welsh dataset finds that men who experience more orgasms have lower risks of dying from coronary heart disease (Smith, Frankel, and Yarnell 1997). Other clinical-based studies also find evidence of health benefits from sexual activity and suggest that increased frequency of vaginal intercourse is associated with better mental health outcomes as well as healthier heart rate variability and lower risk of mortality (see a review in Brody 2010). At the same time, there are also some clinical concerns that sexual activity may trigger acute cardiac events especially for patients with a prior history of CVD (Cheitlin 2003; Dahabreh and Paulus 2011; Muller et al. 1996; Stein 2000). Nevertheless, most clinical studies conclude that the triggering effect of sexual activities on acute cardiac events is minimal and can be alleviated through regular physical exercise (Cheitlin 2003; Dahabreh and Paulus 2011; Muller et al. 1996; Stein 2000).
Clinical studies usually consider sex as a form of physical activity, suggesting that sexual activity is equivalent to mild to moderate physical activity such as “climbing 2 flights of stairs or walking briskly” (Levine et al. 2012:1058). The premise is that sexual foreplay, stimulation and intercourse require both men and women to engage in stretching and physical movement. Regular physical activities enhance endothelial nitric-oxide synthase (eNOS) expression and function leading to increased nitric-oxide (NO) production and thereby vasodilation (Dimmeler and Zeiher 2003). This process improves the efficiency of the delivery of oxygen and nutrients to body cells and tissues, thus keeping the tissues healthy and strong (Butt 1990).
Although clinical studies represent a step forward in this line of investigation, both the quantity and quality of the research is limited. Studies to date have failed to demonstrate basic patterns for known populations. The fundamental weaknesses of these studies, which include small, unrepresentative samples, a focus only on younger adults, cross-sectional designs, and lack of control covariates (Brody 2010), make causal inference difficult. More importantly, these clinical studies mainly utilize a medical perspective that emphasizes the physical and behavioral traits of sex in the disease development processes, and tend to overlook the social and psychological context in which partnered sex occurs. Therefore, this line of literature suffers from its intellectual fragmentation and does not provide a theoretical frame to guide empirical analysis and integrate research findings (Hammack 2005).
TOWARD AN INTEGRATED MODEL: A SOCIAL RELATIONSHIP AND LIFE COURSE PERSPECTIVE ON PARTNERED SEXUALITY LINKED TO CARDIOVASCULAR HEALTH
The life course perspective on social relationships lays a broad theoretical foundation to expect that partnered sexuality holds significant meaning for individuals and functions to shape life context which, in turn, affects health. This perspective directs attention to both the resources and support that flow from relationships as well as the strain and demands that they carry, all of which constitute key components of the life course (Umberson and Montez 2010).
Resources and Support
Involvement in partnered sexuality increases access to social, psychological and behavioral resources. In terms of behavioral resources, sex is the central activity in a sexual relationship. However, in most cases, especially among older adults, involvement in partnered sexuality goes beyond the physical act of sex to include emotional closeness, availability of a confidant, and the benefits of physical touch (Iveniuk et al. 2015). Similar to other types of social relationships like marriage and parenthood, partnered sexuality may promote health via increasing social integration and social and emotional support (Burman and Margolin 1992; Cohen 2004), which are all important resources that promote health (Waite and Joyner 2001). Intimate relationships, whether sexually active or no longer so, are more likely to provide emotional support to men than to women (Erickson 2005; Kalmijn 2003) but women seem to be more sensitive to the quality of the relationship than are men (Kiecolt-Glaser and Newton 2001).
Stress Relief
Stress triggers the sympathetic nervous system to metabolize glucose and induces the release of stress hormones, specifically catecholamines and cortisol, which, in turn, results in increased blood pressure and heart rate, accelerated breathing, and constriction of blood vessels. This “fight or flight” process characterizes the general human response to stress which may increase allostatic load and foster wear and tear on the regulatory mechanisms, leading to chronic conditions, such as CVD and hypertension (Everson-Rose and Lewis 2005; McEwen and Stellar 1993; Taylor et al. 2000). Clinical scientists contend that physical exercise, including sexual activity, helps to reduce both women’s and men’s stress hormone levels (e.g., adrenaline, cortisol) and to stimulate the production of endorphins, a natural mood elevator. Sexual activity, especially orgasm, also triggers the release of oxytocin, which promotes bonding (Magon and Kalra 2011) and may help to relieve stress, thus enhancing cardiovascular health. Not only is stress relieved during intercourse and the moment of orgasm, but elevated mood may persist for some time, and have a positive impact on health (Exton et al. 1999; Kashdan et al. 2014; Kruger et al. 1998). The physical act of sex may alleviate stress directly in the same way as does any exercise (Salmon 2001). Sex may also work indirectly through the increased access to coping resources such as emotional support from a sexual relationship, which may alleviate the negative effect of stress. The efficacy of sexual activity for relieving stress may depend on the quality of the experience, with only satisfying sex reducing stress, in much the same way as only marriages of high quality improve physical health (Liu and Waite 2014).
Strain and Demands
While partnered sexuality may provide health-promoting resources, it may also constitute a source of emotional and physical strain and demands (Walen and Lachman 2000). The demands may come from the expectations and social norms related to gender and sexuality. For example, cultural scripts of masculinity may encourage men to enact their masculinity through sexual activities such as high frequency of sex and high expectation for their sexual performance (Carpenter 2015). This is consistent with the observations that men tend to report having sex more often than do women, and that men are more likely than women to suffer sexual performance anxiety and to take performance enhancing drugs (Laumann, Das & Waite 2008; Lindau et al. 2007). Given that a large proportion of older adults, especially men, suffer some problems of sexual dysfunction and/or sexual performance anxiety (Lindau et al. 2007), the social norms of masculinity may increase older men’s exposure to both emotional stress and physical demands as they try to adhere to the norms of frequent sex in the face of health challenges or sexual problems (Lindau et al. 2007). Yet, a sexual relationship that produces high physical pleasure and emotional satisfaction may promote relationship quality and minimize the consequences of strain and demands, thus promoting cardiovascular health.
THE PRESENT STUDY AND RESEARCH HYPOTHESES
We move beyond the medical perspective by integrating a social relationship and life course perspective to view partnered sexuality that constitutes the life context of individuals and in turn shapes cardiovascular health. Given the long standing observation that involvement in social relationships promotes health and that men receive more health benefits from an intimate relationship than do women (Liu and Umberson 2008), our general hypothesis is that: people who are sexually active with a partner will have lower cardiovascular risk than people who are sexually inactive, with stronger effects for men than for women (Hypothesis 1).
Social relationship scholars further distinguish quantitative (e.g., sexual frequency) and qualitative (e.g., sexual quality) dimensions of a relationship, and argue that both dimensions have significant implications for health (Umberson and Montez 2010).
Sexual Frequency
Frequency of partnered sex is a key mechanism through which sexual relationships may produce health outcomes. Medical researchers have reinforced scientific evidence linking regular physical exercise to various measures of cardiovascular health and emphasize frequency of exercise as a key component to developing cardiovascular fitness of older adults (Myers 2003). Similar to other forms of physical exercise, having sex frequently may enhance the capacity of the blood vessels to dilate, improve vascular wall function, more efficiently provide oxygen to the muscles and in turn promote cardiovascular health (Myers 2003). Moreover, moderate frequency of sex may promote intimacy in the relationship and thus overall relationship quality (Galinsky and Waite 2014), which has positive effects on health. However, a high frequency of sex may indicate potential problems of sexual obsessions or unmet sexual need of either partner, or may signal the presence of an extramarital sexual relationship. These may lead to stress and physical exhaustion and thus be detrimental to cardiovascular health (Safi et al. 2002). In addition, sexual intercourse per se is physically and biologically demanding and entails moderate stress on the cardiovascular system (Safi et al. 2002), perhaps more so for men’s bodies than for women’s due to biologically-based sex differences of genetic and hormonal origins (Fisher 2012). Taken together, we hypothesize that both men and women who have moderately frequent sex will have lower cardiovascular risk than those who are sexually inactive (Hypothesis 2a), but high frequency of sex will be related to increased cardiovascular risk especially for men (Hypothesis 2b).
Sexual Quality
Compared with objective measures of sexual frequency, clinical studies have paid less attention to subjective feelings of sexual well-being in linkages to health (Brody 2010). In contrast, social relationship scholars have consistently highlighted the importance of relationship quality in shaping health (Umberson and Montez 2010). Sexual quality broadly refers to individuals’ subjective appraisal of their sexual relationships, with physical dimensions differentiated from emotional (Lawrance and Byers 1992; Laumann et al., 2006). Both dimensions of sexual quality are seen as components of relationship satisfaction and stability (Galinsky and Waite 2014; Sprecher 2002), and thus modify the social support and stress processes and shape cardiovascular health. Greater satisfaction with one’s sexual relationship, both physically and emotionally, may improve relationship quality, promote access to social support, and enhance life satisfaction and happiness (Dogan, Tugut and Golbasi 2013; Galinsky and Waite 2014)—all factors that promote cardiovascular health. Because women are more sensitive to the quality of a relationship than are men, they may experience stronger effects of relationship quality on their cardiovascular health than do men (Kiecolt-Glaser and Newton 2001; Liu and Waite 2014; Zhang and Hayward 2006). This view is supported by clinical studies suggesting that multiple domains of relationship quality have stronger effects on women’s health—including immune system and cardiovascular function—than on men’s (Kiecolt-Glaser and Newton 2001; Liu and Waite 2014). Recent studies also find that sexual quality is more important for women’s happiness and life satisfaction than for men’s (Dogan et al. 2013). Taken together, we expect that better sexual quality will be related to lower cardiovascular risk, and this relationship will be stronger for women than for men (Hypothesis 3).
Potential Reversal Causality
Although our primary research question is about how partnered sexuality affects cardiovascular risk, it is also possible that poor cardiovascular health interferes with individuals’ sexual life. Despite limited empirical evidence, especially population-based, several clinical studies have examined how sexuality is affected by heart disease and suggested that the onset of cardiovascular disease is associated with a decline in sexual desire and frequency (Jaarsma et al. 1996; Schwarz and Rodriguez 2005). For example, Jaarsma and collegaues (1996) studied 62 patients with advanced heart failure and found that most patients reported a marked decrease in sexual interest and sexual frequency as well as decreases in the feeling of pleasure or satisfaction they normally experienced from sex after the event of heart failure. Given this literature, we expect that higher cardiovascular risk at one point will be related to both lower frequency and lower quality of sex at a later point for both men and women (Hypothesis 4).
DATA
We use the first two waves of nationally representative longitudinal data, which lie at the foundation of a life course perspective, from the National Social Life, Health and Aging Project (NSHAP). The NSHAP, one of the first national-scale population-based studies of health and intimate relationships at older ages, was conducted by NORC at the University of Chicago. A nationally representative probability sample of community-dwelling individuals ages 57–85 was selected from households across the U.S. and screened in 2004. African Americans, Latinos, men, and those 75–84 years old were over-sampled. All analyses are weighted and further adjusted for clustering and stratification of the complex sampling design using the complex analysis commands in MPLUS software (Muthén and Muthén 2007).
The first wave of the NSHAP (Wave 1) included a sample of 3,005 adults ages 57–85 who were interviewed during 2005–2006 (Waite, Laumann, et al. 2014). Both in-home interviews and lab tests and assays were conducted. Wave 2 consisted of 2,261 Wave 1 respondents who were re-interviewed during 2010–2011 (Waite, Cagney, et al. 2014). Because our study focuses on partnered sexuality, we exclude 57 respondents who reported having had sex in the past year but were not in a partnered relationship including marriage, cohabitation, and other intimate or sexual relationships at Wave 1. Thus, our final sample includes 1,046 men and 1,158 women who were interviewed in both waves.
MEASURES
Partnered Sexual Activity
We start with a basic measure of whether a respondent is sexually active with a partner. This is based on the question asking whether the respondent had sex with the partner in the last year (1 = Yes, 0 = No). Sex is defined as any “mutually voluntary activity with another person that involves sexual contact, whether or not intercourse or orgasm occurs” (Lindau et al. 2007:763). Then, we measure sexual frequency based on the question asking respondents how often they had sex with the partner during the last 12 months. The response includes: none (reference), about once a month, 2–3 times a month, and once a week or more.
Sexual Quality
Sexuality scholars distinguish two dimensions of sexual quality: physical pleasure and emotional satisfaction (Laumann et al. 2006; Waite and Joyner 2001). Respondents were asked how physically pleasurable they found their sexual relationship to be. They were also asked in a separate question how emotionally satisfying they found their sexual relationship to be. If the respondent was not sexually active last year, the questions referred to their most recent partnered sexual relationship. Because these two measures are left-skewed, we collapse the lower end categories and recode the variables into three categories: not very pleasurable/satisfying (including none, slightly and moderately), very pleasurable/satisfying, and extremely pleasurable/satisfying. We analyze these two variables as separate measures for the physical and emotional dimensions of sexual quality, respectively.
Cardiovascular Health Outcomes
We include four measures of cardiovascular risk: hypertension, rapid heart rate, elevated C-reactive protein (CRP), and general CVD events.
Hypertension is a key risk factor for CVD. Elevated blood pressure is associated with an increased risk of hypertensive heart disease, stroke, heart attack, and heart failure (Izzo and Black 2003). Hypertension increases the pressure on blood vessels and the heart, and can lead to inflammation of arteries, atherosclerosis and clogging, narrowing, and damaging of the blood vessels, all of which create multiple risks for CVD (Izzo and Black 2003). To measure hypertension, we combine both the biological and self-reported measures collected by the NSHAP (Cornwell and Waite 2012). The NSHAP measured the blood pressure of each respondent twice, using a LifeSource digital blood pressure monitor (model UA-767PVL). Hypertension is identified when the mean of the two readings is greater than 140 mm Hg systolic or 90 mm Hg diastolic. For respondents who have been diagnosed with diabetes, we use the recommended lower cutoff of either 130 mm Hg systolic or 80 mm Hg diastolic (National Heart, Lung, and Blood Institute 2003). In addition, respondents were asked whether they had ever been told by a medical doctor that they had high blood pressure or hypertension. Based on responses to this question, along with the measures of blood pressure, we categorize respondents into four groups: (1) normal blood pressure reading and no diagnosis of hypertension (referred to as the “normal” blood pressure group), (2) normal blood pressure reading but diagnosed with hypertension (referred to as “controlled” hypertensive group), (3) high blood pressure reading but no diagnosis of hypertension (referred to as “undiagnosed” hypertensive group), and (4) high blood pressure reading and diagnosed hypertension (referred to as “uncontrolled” hypertensive group). The normal blood pressure group is the reference group.
The second measure of cardiovascular risk is rapid heart rate. Heart rate is measured as the number of times the heart beats per minute. When the heart cannot effectively deliver blood and oxygen to meet the needs of the body it will beat abnormally fast. A long-term resting heart rate greater than 80 beats per minute is linked to a significant risk of hypertension, heart disease, and mortality (Izzo and Black 2003). Heart rate was measured twice for the NSHAP respondents. Rapid heart rate (coded as 1) is identified if the mean reading is greater than 80 beats per minute, and all others are identified as normal heart rate (coded as 0).
The third measure of cardiovascular risk is C-reactive protein (CRP). Elevated CRP is often used as a marker for systemic inflammation, and it has emerged as an important predictor of CVD (Nallanathan et al. 2008; Ridker 2003). Ridker (2003) suggests that CRP is a stronger predictor of cardiovascular events than are other traditional markers, such as low-density-lipoprotein cholesterol. During the home interviews, blood was obtained via a single finger-stick using a retractable-tip, single-use disposable lancet and then applied to filter paper. The filter paper was allowed to dry for the remainder of the interview before being placed in a plastic bag with desiccant for transport and storage. High-sensitivity CRP (mg/L) was derived from the dried blood. Details about the procedures of NSHAP dried blood spot CRP measurement are described by Nallanathan et al. (2008). We follow the recommendations of the CDC with respect to classification of cardiovascular risk when interpreting CRP values: low and normal risks exist when CRP <= 3 mg/L, high risk exists when CRP > 3 mg/L but <= 10 mg/L, and presence of acute infection when CRP > 10 mg/L (Pearson et al. 2003). CRP is analyzed as an ordinal categorical variable with higher values indicating higher levels of CRP.
Finally, we include a measure of self-reported general CVD events. During the home interviews, all NSHAP respondents were asked whether they had ever been told by a medical doctor that they had had a heart attack, heart failure, or stroke. These events are the most common forms of CVD among older adults. Respondents who reported any of these CVD events are coded as 1, and others are coded as 0.
Other Covariates
We include two types of covariates (all measured at Wave 1) that are related to both sexuality and cardiovascular risk: socio-demographic covariates and health-related covariates.
Socio-Demographic Covariates
We stratify all analyses by gender. Age is measured as a continuous variable in years. Marital status includes the married (coded as 0) and unmarried (coded as 1). Race-ethnicity includes non-Hispanic white (reference), non-Hispanic black, Hispanic, and other. Education is grouped into four categories: less than high school (reference), high school graduate, some college, and college graduate. Family income is derived from the question that asked respondents to compare their family income levels with other American families. Responses range from below average (reference), average, to above average.
Health-Related Covariates
We control for general measures of both mental and physical health. Physical health is measured based on self-reported physical health, ranging from 1 poor/fair to 5 excellent. Mental health is measured by psychological distress using an 11-question subset of the Center for Epidemiological Studies Depression Scale (CES-D) (Radloff 1977). Respondents were asked how often in the past week they experienced any of the following: (1) I did not feel like eating; (2) I felt depressed; (3) I felt that everything I did was an effort; (4) My sleep was restless; (5) I was happy; (6) I felt lonely; (7) People were unfriendly; (8) I enjoyed life; (9) I felt sad; (10) I felt that people disliked me; and (11) I could not get “going”. Response categories range from (0), rarely or none of the time, to (3), most of the time. The items are recoded such that higher values indicate higher levels of depression (i.e., poorer mental health). The final scale is the sum of the 11 scores.
We also control for a number of health behaviors. Because respondents may take medications for hypertension or sexual hormones, we include an indicator for taking any antihypertensive medicine (1 = Yes, 0 = No) and another separate indicator for taking sex hormones (e.g., estrogen, progestin, and testosterone, 1 = Yes, 0 = No). We also include body mass index (BMI), a significant predictor of CVD, as an indicator of obesity (Izzo and Black 2003). BMI is calculated from measured height and weight, grouped into four categories: normal or underweight (BMI < 25), overweight (25 <= BMI < 30), obese (30 <= BMI < 40), and morbidly obese (BMI >= 40) (World Health Organization 1995). In addition, we include indicators for currently smoke (1 = Yes, 0 = No), currently drink alcohol (1 = Yes, 0 = No), and physical exercise (1= vigorous physical activity or exercise three times or more per week, 0 = others).
ANALYTIC APPROACH
We apply cross-lagged models (illustrated in Figure 1), widely used in the analysis of longitudinal data, to account for the possibility of reversal causality (Finkel 2004). Specifically, we use Wave 1 sexuality to predict Wave 2 cardiovascular risk outcomes, and use Wave 1 cardiovascular risks to predict Wave 2 sexuality. In each prediction equation, we control for Wave 1 cardiovascular risks, Wave 1 sexuality and all other covariates. We run four separate cross-lagged models to assess the status of being sexually active (i.e., had sex last year) (Model A), sexual frequency (Model B), physical (Model C) and emotional (Model D) dimensions of sexual quality, respectively, in relation to all cardiovascular risks. The specific prediction equation varies by the measurement of the endogenous variables. Specifically, we estimate multinomial logistic regression models to predict hypertension, binary logistic regression models to predict rapid heart rate, general CVD events and being sexually active, and ordinal logistic regression models to predict CRP, sexual frequency, physical pleasure and emotional satisfaction. Because women and men play different roles in a sexual relationship and their CVD risks also differ, we stratify all analyses by gender and assess statistical significance of gender differences in the regression coefficients using Z-tests (Agresti and Finley 2009). Results from the Z-tests (not shown but available upon request) suggested that gender differences in all key findings were statistically significant. All models are estimated using MPLUS (Muthén and Muthén 2007).
Figure 1.
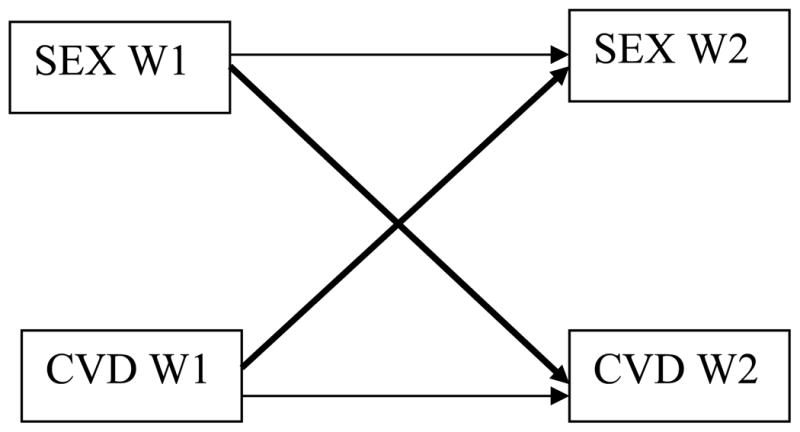
Structural Path Diagram of Cross-lagged Model for Sexuality and Cardiovascular Risks.
Note: Bolded paths are the focus of this study with results reported in tables.
We use the Full Information Maximum Likelihood (FIML) methods provided by MPLUS to handle missing values of all endogenous variables such as CVD risks and sexuality factors. The FIML approach maximizes a casewise likelihood function using only those observed variables with the assumption of missing at random (Muthén and Muthén 2007). Missing values for categorical exogenous covariates are flagged as separate missing categories. Cases with missing values (about 1%) on continuous exogenous covariates are replaced with the mean.
Correction for Sample Attrition Due to Mortality
Our analysis sample includes only respondents who were interviewed in both waves of NSHAP. Sample attrition between waves, especially due to mortality, is not random. Therefore, we apply the approach, developed by Heckman (1979), to adjust the sample selection biases that are due to selection through mortality. See Liu and Waite (2014) for similar applications. This approach consists of modeling the probability that a respondent would die between Waves 1 and 2 using logistic regression models, conditional on a set of predictors measured at Wave 1. Then, for individuals who did not die, cardiovascular risk outcomes are modeled as a function of a set of independent variables, including the estimated probabilities of dying. Following this Heckman-type correction, estimates of cardiovascular risk should be interpreted as being adjusted for factors that may affect that risk as well as the tendency to die.
RESULTS
We start our discussion with descriptive results, shown in Tables 1–2 for men and women separately. Clearly, we can see that men are more likely to report having had partnered sex last year (70% at Wave 1 and 49% at Wave 2) than are women (39% at Wave 1 and 23% at Wave 2). Men also report a higher frequency of sex than do women. Specifically, 25% and 20% of men in contrast to 11% and 11% of women report that they had sex once a week or more in the past year at Wave 1 and Wave 2 respectively. Moreover, men are more likely than women to report their sexual relationship as extremely physically pleasurable (36% vs. 23% at Wave 1, 33% vs. 17% at Wave 2) and extremely emotionally satisfying (37% vs. 25% at Wave 1, 34% vs. 15% at Wave 2). Tables 1 and 2 also show moderate gender differences in cardiovascular risks, but the differences are much smaller than the gender differences in the sexuality variables.
Table 1.
Weighted Descriptive Statistics for Men (N=1,046)
| %/mean(SD) | %/mean(SD) | ||
|---|---|---|---|
| Sexuality Variables at Wave 1 | Sexuality Variables at Wave 2 | ||
| Respondent had sex last year | Respondent had sex last year | ||
| No (ref) | 30.5 | No (ref) | 51.3 |
| Yes | 69.5 | Yes | 48.7 |
| Sex frequency in past year | Sex frequency in past year | ||
| Never (ref) | 30.5 | Never (ref) | 40.0 |
| Once a month | 22.0 | Once a month | 19.5 |
| 2–3 times a month | 20.0 | 2–3 times a month | 18.3 |
| Once a week or more | 24.9 | Once a week or more | 19.8 |
| Missing | 2.6 | Missing | 2.4 |
| Physical pleasure of relationship | Physical pleasure of relationship | ||
| None/slightly/moderately pleasurable (ref) | 19.2 | None/slightly/moderately pleasurable (ref) | 17.3 |
| Very pleasurable | 41.3 | Very pleasurable | 34.6 |
| Extremely pleasurable | 35.7 | Extremely pleasurable | 33.4 |
| Missing | 3.8 | Missing | 14.7 |
| Emotional satisfaction of relationship | Emotional satisfaction of relationship | ||
| None/slightly/moderately satisfying (ref) | 18.6 | None/slightly/moderately satisfying (ref) | 16.4 |
| Very satisfied | 42.7 | Very satisfied | 36.2 |
| Extremely satisfied | 36.7 | Extremely satisfied | 34.1 |
| Missing | 2.0 | Missing | 13.3 |
|
| |||
| Cardiovascular Risk Outcomes at Wave 1 | Cardiovascular Risk Outcomes at Wave 2 | ||
| Hypertension | Hypertension | ||
| Normal (ref) | 30.0 | Normal (ref) | 23.9 |
| Controlled hypertension | 20.3 | Controlled hypertension | 22.5 |
| Undiagnosed hypertension | 16.6 | Undiagnosed hypertension | 16.1 |
| Uncontrolled hypertension | 31.6 | Uncontrolled hypertension | 32.9 |
| Missing | 1.5 | Missing | 4.6 |
| Rapid heart rate | Rapid heart rate | ||
| No (ref) | 80.4 | No (ref) | 75.8 |
| Yes | 17.8 | Yes | 19.0 |
| Missing | 1.8 | Missing | 5.2 |
| CRP level | CRP level | ||
| ≤3 (ref) | 52.6 | ≤3 (ref) | 60.7 |
| >3 and ≤10 | 12.9 | >3 and ≤10 | 22.8 |
| >10 | 1.8 | >10 | 7.1 |
| Missing | 32.7 | Missing | 9.4 |
| CVD events | CVD events | ||
| No (ref) | 79.3 | No (ref) | 77.9 |
| Yes | 20.3 | Yes | 21.4 |
| Missing | 0.4 | Missing | 0.7 |
|
| |||
| Covariates at Wave 1 | |||
| Race-ethnicity | BMI | ||
| Non-Hispanic white (ref) | 80.8 | Normal or underweight (ref) | 19.4 |
| Non-Hispanic black | 8.6 | Overweight | 38.6 |
| Hispanic | 7.1 | Obesity | 33.3 |
| Others | 3.5 | Morbidly obese | 3.3 |
| Education | Missing | 5.4 | |
| Less than high school (ref) | 15.4 | Smoke | |
| High school | 22.7 | No (ref) | 84.0 |
| Some college | 27.3 | Yes | 16.0 |
| College graduate | 34.6 | Drink | |
| Relative family income | No (ref) | 31.8 | |
| Below average (ref) | 20.9 | Yes | 68.2 |
| Average | 31.9 | Sexual hormones use | |
| Above average | 30.1 | No (ref) | 97.7 |
| Missing | 17.1 | Yes | 2.3 |
| Marital status | Antihypertensive medication use | ||
| Not married (ref) | 19.5 | No (ref) | 4.4 |
| Married | 80.5 | Yes | 55.6 |
| Physical activity | Self-rated health | 2.4(1.0) | |
| < 3 times per week (ref) | 28.7 | Psychological distress | 4.5(4.5) |
| >= 3 times per week | 71.3 | Age | 66.7(7.5) |
| Probability of death at Wave 2 | 0.1(0.1) | ||
ref indicates the reference category.
Table 2.
Weighted Descriptive Statistics for Women (N=1,158)
| %/mean(SD) | %/mean(SD) | ||
|---|---|---|---|
| Sexual Variables at Wave 1 | Sexual Variables at Wave 2 | ||
| Respondent had sex last year | Respondent had sex last year | ||
| No (ref) | 60.5 | No (ref) | 77.0 |
| Yes | 39.3 | Yes | 22.9 |
| Missing | 0.2 | Missing | 0.1 |
| Sex frequency in past year | Sex frequency in past year | ||
| Never (ref) | 60.5 | Never (ref) | 67.2 |
| Once a month | 13.6 | Once a month | 9.7 |
| 2–3 times a month | 11.7 | 2–3 times a month | 11.2 |
| Once a week or more | 11.4 | Once a week or more | 10.8 |
| Missing | 2.8 | Missing | 1.1 |
| Physical pleasure of relationship | Physical pleasure of relationship | ||
| None/slightly/moderately pleasurable (ref) | 36.6 | None/slightly/moderately pleasurable (ref) | 19.4 |
| Very pleasurable | 35.1 | Very pleasurable | 17.7 |
| Extremely pleasurable | 22.5 | Extremely pleasurable | 16.5 |
| Missing | 5.8 | Missing | 46.4 |
| Emotional satisfaction of relationship | Emotional satisfaction of relationship | ||
| None/slightly/moderately satisfying (ref) | 36.3 | None/slightly/moderately satisfying (ref) | 18.4 |
| Very satisfied | 33.8 | Very satisfied | 21.1 |
| Extremely satisfied | 24.8 | Extremely satisfied | 14.9 |
| Missing | 5.1 | Missing | 45.6 |
|
| |||
| Cardiovascular Risk Outcomes at Wave 1 | Cardiovascular Risk Outcomes at Wave 2 | ||
| Hypertension | Hypertension | ||
| Normal (ref) | 27.6 | Normal (ref) | 23.1 |
| Controlled hypertension | 21.8 | Controlled hypertension | 24.4 |
| Undiagnosed hypertension | 16.9 | Undiagnosed hypertension | 16.5 |
| Uncontrolled hypertension | 31.8 | Uncontrolled hypertension | 32.6 |
| Missing | 1.9 | Missing | 3.4 |
| Rapid heart rate | Rapid heart rate | ||
| No (ref) | 76.7 | No (ref) | 74.2 |
| Yes | 21.4 | Yes | 21.6 |
| Missing | 1.9 | Missing | 4.2 |
| CRP level | CRP level | ||
| ≤3 (ref) | 44.9 | ≤3 (ref) | 51.1 |
| >3 and ≤10 | 17.1 | >3 and ≤10 | 31.3 |
| >10 | 3.3 | >10 | 8.9 |
| Missing | 34.7 | Missing | 8.7 |
| CVD events | CVD events | ||
| No (ref) | 86.5 | No (ref) | 84.7 |
| Yes | 13.1 | Yes | 14.6 |
| Missing | 0.4 | Missing | 0.7 |
|
| |||
| Covariates at Wave 1 | |||
| Race-ethnicity | BMI | ||
| Non-Hispanic white (ref) | 80.8 | Normal or underweight (ref) | 24.7 |
| Non-Hispanic black | 10.4 | Overweight | 33.3 |
| Hispanic | 6.5 | Obesity | 30.2 |
| Others | 2.3 | Morbidly obese | 6.2 |
| Education | Missing | 5.6 | |
| Less than high school (ref) | 17.8 | Smoke | |
| High school | 27.8 | No (ref) | 87.2 |
| Some college | 35.0 | Yes | 12.8 |
| College graduate | 19.4 | Drink | |
| Relative family income | No (ref) | 47.5 | |
| Below average (ref) | 29.5 | Yes | 52.5 |
| Average | 35.7 | Sexual hormones use | |
| Above average | 19.1 | No (ref) | 87.5 |
| Missing | 15.7 | Yes | 12.5 |
| Marital status | Antihypertensive medication use | ||
| Not married (ref) | 47.1 | No (ref) | 41.4 |
| Married | 52.9 | Yes | 58.6 |
| Physical activity | Self-rated health | 2.4(1.0) | |
| < 3 times per week (ref) | 38.6 | Psychological distress | 5.4(5.1) |
| >= 3 times per week | 61.4 | Age | 68.0(7.5) |
| Probability of death at Wave 2 | 0.1(0.1) | ||
ref indicates the reference category.
Results from Cross-Lagged Models for Men
Next, we move to the results from the cross-lagged models for men. We first discuss the results for sexuality predicting later cardiovascular risks (shown in Table 3) followed by the results for cardiovascular risks predicting later sexuality (shown in Table 4).
Table 3.
Estimated Odds Ratios of Wave 1 Sexuality Predicting Wave 2 Cardiovascular Risks from Cross-Lagged Models for Men (N=1,046)
| Hypertension (multinomial logit) | Rapid heart rate (binary logit) | High CRP (ordinal logit) | CVD events (binary logit) | |||
|---|---|---|---|---|---|---|
| Controlled v.s. normal | Undiagnosed v.s. normal | Uncontrolled v.s. normal | ||||
|
|
|
|
|
|||
| Model A: Sexually Active (ref: no) | ||||||
| Had sex last year | 1.04 | 1.29 | 0.96 | 1.19 | 0.61* | 1.18 |
|
| ||||||
| Model B: Sex frequency (ref: none) | ||||||
| Once a month | 1.48 | 1.80 | 1.66 | 0.62 | 0.43** | 1.11 |
| 2–3 times a month | 0.91 | 1.57 | 0.85 | 1.00 | 0.73 | 1.37 |
| Once a week or more | 1.11 | 1.02 | 0.83 | 1.42 | 0.66 | 1.90* |
|
| ||||||
| Model C: Physical pleasure (ref: not very pleasurable) | ||||||
| Very pleasurable | 1.44 | 1.65 | 1.46 | 1.07 | 0.85 | 1.32 |
| Extremely pleasurable | 1.09 | 1.11 | 1.39 | 1.23 | 0.72 | 1.65* |
|
| ||||||
| Model D: Emotional satisfaction (ref: not very satisfying) | ||||||
| Very satisfying | 0.64 | 0.69 | 0.78 | 0.78 | 0.83 | 1.33 |
| Extremely satisfying | 0.59 | 0.67 | 0.68 | 0.97 | 0.73 | 2.04* |
Two-tailed tests:
p<0.001,
p<0.01,
p<0.05. In all models, we control for age, race-ethnicity, marital status, education, relative family income, self-rated physical health, psychological distress, smoking, drinking, BMI, physical activity, antihypertensive medication use, and sexual hormones use (all measured at Wave 1) as well as probability of death at W2. Cardiovascular risks and sexuality at W1 are also controlled.
Table 4.
Estimated Odds Ratios of Wave 1 Cardiovascular Risks Predicting Wave 2 Sexuality from Cross-Lagged Models for Men (N=1,046)
| Model A Sexually Active (binary logit)
|
Model B Sex frequency (ordinal logit)
|
Model C Physical pleasure (ordinal logit)
|
Model D Emotional satisfaction (ordinal logit)
|
|
|---|---|---|---|---|
| Hypertension (ref: normal) | ||||
| Controlled | 0.91 | 1.04 | 0.80 | 0.72 |
| Undiagnosed | 0.68 | 1.94* | 1.43 | 1.09 |
| Uncontrolled | 1.20 | 0.92 | 0.81 | 0.86 |
| Rapid heart rate (ref: no) | ||||
| Yes | 0.68 | 1.27 | 1.51 | 1.20 |
| CRP (ref: <3) | ||||
| >3 and ≤10 | 0.94 | 0.98 | 0.92 | 0.69 |
| >10 | 1.61 | 0.95 | 0.76 | 0.83 |
| CVD events (ref: no) | ||||
| Yes | 1.00 | 1.13 | 1.34 | 0.96 |
Two-tailed tests:
p<0.001,
p<0.01,
p<0.05. In all models, we control for age, race-ethnicity, marital status, education, relative family income, self-rated physical health, psychological distress, smoking, drinking, BMI, physical activity, antihypertensive medication use, and sexual hormones use (all measured at Wave 1) as well as probability of death at W2. Cardiovascular risks and sexuality at W1 are also controlled.
Sexuality Predicting Cardiovascular Risks
From Model A of Table 3 we can see that men who were sexually active with a partner at Wave 1 are less likely to be in a higher CRP category five years later than men who were sexually inactive (OR = 0.61, p < 0.05), although sexually active men are not significantly different from sexually inactive men in other cardiovascular outcomes.
Results in Model B of Table 3 further suggest that only sexually active men who had sex once a month at Wave 1 have significantly lower odds of being in a higher CRP category than men who had no sex last year at Wave 1 (OR = 0.43, p < 0.01). Yet, higher frequency of sex (i.e., 2–3 times a month or once a week or more) is not related to CRP for men. Moreover, as shown in Model B of Table 3, the odds of experiencing CVD events by Wave 2 for men who had sex once a week or more at Wave 1 are nearly double (OR = 1.90, p < 0.05) the odds for men who were sexually inactive, although lower frequency of sex (i.e., 2–3 times a month or once a month) at Wave 1 is not significantly related to CVD events at Wave 2 for men.
Furthermore, results in Table 3 also suggest that reporting a sexual relationship extremely pleasurable (Model C) and extremely satisfying (Model D) at Wave 1 are both related to higher odds of experiencing CVD events by Wave 2 for men. Specifically, men who reported that that their sexual relationship was extremely pleasurable have 65% higher odds of experiencing CVD events five years later than men who reported it not very physically pleasurable; men who reported their sexual relationship extremely satisfying face about twice of the odds of experiencing CVD events within the next five years compared to men who were not very emotionally satisfied (OR = 2.04, p < 0.05).
Cardiovascular Risks Predicting Sexuality
Table 4 shows the results for the reverse causal pathway in which cardiovascular risks predict later sexuality for men. This table shows only one significant effect: men who had undiagnosed hypertension at Wave 1 tend to report higher sex frequency five years later than men with normal blood pressure initially (OR = 1.94, p < 0.05), but other CVD risks at Wave 1 are unrelated to later sexual activity at Wave 2 for men.
Results from Cross-Lagged Models for Women
Results from the cross-lagged models for women are shown in Table 5 for sexuality predicting cardiovascular risks and in Table 6 for cardiovascular risks predicting sexuality.
Table 5.
Estimated Odds Ratios of Wave 1 Sexuality Predicting Wave 2 Cardiovascular Risks from Cross-Lagged Models for Women (N=1,158)
| Hypertension (multinomial logit) | Rapid heart rate (binary logit) | High CRP (ordinal logit) | CVD events (binary logit) | |||
|---|---|---|---|---|---|---|
| Controlled v.s. normal | Undiagnosed v.s. normal | Uncontrolled v.s. normal | ||||
|
|
|
|
|
|||
| Model A: Sexually Active (ref: no) | ||||||
| Had sex last year | 1.20 | 1.28 | 1.22 | 0.86 | 0.91 | 1.60 |
|
| ||||||
| Model B: Sex frequency (ref: none) | ||||||
| Once a month | 0.98 | 0.86 | 0.74 | 0.63 | 0.90 | 1.91 |
| 2–3 times a month | 2.01 | 1.17 | 1.78 | 1.51 | 1.18 | 1.23 |
| Once a week or more | 2.02 | 1.82 | 1.58 | 0.93 | 1.48 | 1.16 |
|
| ||||||
| Model C: Physical pleasure (ref: not very pleasurable) | ||||||
| Very pleasurable | 1.70 | 1.00 | 1.13 | 0.68 | 1.07 | 1.17 |
| Extremely pleasurable | 0.86 | 0.53* | 0.42* | 1.08 | 0.88 | 0.71 |
|
| ||||||
| Model D: Emotional satisfaction (ref: not very satisfying) | ||||||
| Very satisfying | 1.09 | 0.97 | 0.77 | 1.14 | 0.84 | 1.34 |
| Extremely satisfying | 0.79 | 0.71 | 0.44** | 1.24 | 0.70 | 1.14 |
Two-tailed tests:
p<0.001,
p<0.01,
p<0.05. In all models, we control for age, race-ethnicity, marital status, education, relative family income, self-rated physical health, psychological distress, smoking, drinking, BMI, physical activity, antihypertensive medication use, and sexual hormones use (all measured at Wave 1) as well as probability of death at W2. Cardiovascular risks and sexuality at W1 are also controlled.
Table 6.
Estimated Odds Ratios of Wave 1 Cardiovascular Risks Predicting Wave 2 Sexuality from Cross-Lagged Models for Women (N=1,158)
| Model A Sexually Active (binary logit)
|
Model B Sex frequency (ordinal logit)
|
Model C Physical pleasure (ordinal logit)
|
Model D Emotional satisfaction (ordinal logit)
|
|
|---|---|---|---|---|
| Hypertension (ref: normal) | ||||
| Controlled | 0.54 | 1.24 | 1.65 | 1.30 |
| Undiagnosed | 0.98 | 0.89 | 0.95 | 1.40 |
| Uncontrolled | 0.53 | 2.01* | 1.73 | 1.92* |
| Rapid heart rate (ref: no) | ||||
| Yes | 0.98 | 0.83 | 1.06 | 1.21 |
| CRP (ref: <3) | ||||
| >3 and ≤10 | 1.07 | 0.86 | 0.83 | 0.91 |
| >10 | 0.69 | 1.98 | 1.06 | 1.51 |
| CVD events (ref: no) | ||||
| Yes | 0.93 | 0.78 | 0.90 | 0.79 |
Two-tailed tests:
p<0.001,
p<0.01,
p<0.05. In all models, we control for age, race-ethnicity, marital status, education, relative family income, self-rated physical health, psychological distress, smoking, drinking, BMI, physical activity, antihypertensive medication use, and sexual hormones use (all measured at Wave 1) as well as probability of death at W2. Cardiovascular risks and sexuality at W1 are also controlled.
Sexuality Predicting Cardiovascular Risks
Results from Table 5 suggest that neither the status of having partnered sex (Model A) nor the frequency of sex (Model B) at Wave 1 is a significant predictor of women’s cardiovascular risks at Wave 2. However, both higher levels of physical pleasure (Model C) and emotional satisfaction (Model D) seem to protect women from developing cardiovascular risks, particularly hypertension. Specifically, results from Model C of Table 5 suggest that women who assessed their sexual relationship as extremely physically pleasurable at Wave 1 have significantly lower odds of both undiagnosed (OR = 0.53, p < 0.05) and uncontrolled (OR = 0.42, p < 0.05) hypertension at Wave 2 than women who reported not very physically pleasurable. Results from Model D of Table 5 suggest that women who reported that they felt extremely satisfied with their sexual relationship at Wave 1 have significantly lower odds of uncontrolled hypertension (OR = 0.44, p < 0.05) at Wave 2 than women who did not feel very emotionally satisfied.
Cardiovascular Risks Predicting Sexuality
Table 6 shows the estimated odds ratios of Wave 1 cardiovascular risks predicting Wave 2 sexuality for women. These results suggest that women who had uncontrolled hypertension at Wave 1 tend to report both higher frequency of sex (Model B) and higher levels of emotional satisfaction (Model D) in their sexual relationship at Wave 2 than women whose blood pressure were normal at Wave 1. Other cardiovascular risks at Wave 1 are unrelated to sexuality at Wave 2 for women.
DISCUSSION
Although sex is generally viewed as good for one’s health (Brody 2010), the health consequences of sex for older adults are less scientifically understood. We conceptualize partnered sex within a social relationship framework and argue that partnered sex shapes individuals’ life context over time and in turn evokes cardiovascular response. We make a further contribution by providing the first population-based evidence of the longitudinal association between partnered sexuality and cardiovascular health in later life using a nationally representative longitudinal data set. Below, we outline our major findings and implications.
His and Her Sex in Later Life
Consistent with previous studies (e.g., Lindau et al. 2007; Lindau and Gavrilova 2010), our results suggest that a fairly large proportion of older adults are sexually active, but the patterns vary significantly by gender. We find, as have others, that older men are more likely to report being sexually active than are older women. But in addition, older men report a higher frequency of partnered sex than do older women, and more men than women say that they enjoy their sexual relationship, both physically and emotionally. It is likely that gender differences in sexual enjoyment lead to gender differences in sexual frequency. Because we use self-reported measures of sexuality, it is also possible that men tend to over-report while women tend to under-report their sexual activities (Fisher 2012). This may be related to the social and cultural pressures of expression of masculinity through sexual activities for men, as well as our social conventions that usually suppress women’s openness to discussion of sex (Milhausen and Herold 1999). Despite such potential biases due to misreporting by gender, the observed gender difference in sexuality in later life is consistent with the long-observed cultural norms of a “sexual double standard” that encourages men’s sexual activities but suppresses women’s (Milhausen and Herold 1999). More importantly, our results suggest important gender differences in the linkages between partnered sexuality and cardiovascular risk, as we will discuss shortly.
Partnered Sexuality and Cardiovascular Risk in Later Life
Working from a social relationship and life course perspective, we hypothesized that people, especially men, who were sexually active with a partner would have lower cardiovascular risk than those who were sexually inactive (Hypothesis 1). Consistent with this hypothesis, we find that sexually active men have lower levels of CRP five years later than sexually inactive men. Yet, we did not find evidence for differences between the sexually active and the inactive in other cardiovascular risks for either men or women. More importantly, our results suggest that the benefits and costs of partnered sexuality highly depend on the nature of the sexual relationship, with substantial variation by gender.
Does Sexual Frequency Matter?
We find that men who had sex once a week or more are more likely to experience CVD events (e.g., heart attack, heart failure and stroke) in the following five years than men who did not have sex in the past year (consistent with Hypothesis 2b), although infrequent sex (e.g., once or 2–3 times a month) is not related to CVD risks but instead, even lower risks in some measures (e.g., CRP) (consistent with Hypothesis 2a). This suggests that while infrequent sex may bring some health benefits, having sex too frequently may be detrimental to health, especially for older men. This result is in contrast with the general notion, mostly based on clinical or community-based research, that higher frequency of sex as a form of physical exercise may uniformly promote health on various dimensions (Brody 2010; Ebrahim et al. 2002).
Several factors may explain the difference between our findings and ideas posed by others. First, our study sample is nationally representative of a relatively older population in the U.S., while most previous studies focus on relatively younger age groups without a nationally representative population-based sample (e.g., Ebrahim et al. 2002). It is likely that the risks related to high sexual frequency tend to increase at older ages due to physiological changes over the aging process. Indeed, some clinical studies suggest that sexual activity may trigger sudden cardiovascular events such as myocardial infarction especially among people who have a sedentary lifestyle (Cheitlin 2003; Dahabreh and Paulus 2011; Mittleman et al. 1993; Muller et al. 1996; Stein 2000), which is more prevalent among older than younger adults. At the same time, we want to note that the amount of physical exercise from sex may not be enough to affect the cardiovascular system significantly. Future studies should test the possibility of lifestyle and age variation using other datasets that include a sample with a wider age range. Moreover, our analysis controls for a number of important social and health-related covariates often overlooked in previous studies. Indeed, our additional analysis without controlling for any covariates (not shown but available upon request) reveals a similar finding to previous studies suggesting a negative relationship between sexual frequency and risks of CVD for men. However, once we control for all covariates, we find that a higher sexual frequency is related to a higher risk of CVD events for older men. This suggests that the covariates may have confounded the true relationship between sexual frequency and cardiovascular health. For example, men in better health tend to have sex more frequently than men in poorer health and they also experience lower CVD risks. Without controlling health status as well as other related covariates, estimation of the relationship between sexuality and cardiovascular risk may be biased. Interestingly, we did not find similar patterns among women. Neither being sexually active nor frequency of sex is significantly related to women’s later cardiovascular risks.
A social relationship and life course perspective directs attention to both benefits and costs of a sexual relationship for health (Umberson and Montez 2010), and suggests that the processes differ for men and women (Fuhrera and Stansfeld 2002). On the one hand, men are more likely than women to receive the benefits of the social and psychological resources provided by an intimate relationship (Erickson 2005; Kalmijn 2003), which may promote men’s cardiovascular health more so than women’s. On the other hand, the social norms of gender and masculinity may indicate greater demands for men in a sexual relationship, which may lead to greater physical and emotional stress and thus poorer health. Our results suggest that for men, especially at older ages, the “demands” from a sexual relationship, particularly with a high frequency of sex, overweigh the “resources” it provides for health.
The strain and demands from a sexual relationship may be more relevant for men as they get older, become increasingly frail and suffer more sexual problems. Because older men have more difficulties reaching an orgasm for medical or emotional reasons than do their younger counterparts (Levine et al. 2012; Lindau et al. 2007), they may exert themselves to a greater degree of exhaustion and create relatively more stress on their cardiovascular system in order to achieve a climax (Levine et al. 2012). Moreover, periodically stimulated sympathetic nervous system and testosterone may play a synergetic role leading to adverse cardiovascular health for men (Curtis and O’Keefe 2002; Xu et al. 2013). Another possibility is that due to the gendered social expectations in a sexual relationship and/or sex differences in human biology, men are more likely to use medication or supplements to improve sexual function (Lindau et al. 2007). Although scientific evidence is still rare, it is likely that such sexual medication or supplements may have negative effects on their cardiovascular health. Moreover, having quite a high frequency of sex may indicate problems of sexual addiction, sexual compulsivity or sexual impulsivity, related to psychological states such as anxiety or depression (Bancroft and Vukadinovic 2004), which may lead to negative cardiovascular health.
Does Sexual Quality Matter?
A growing body of literature on social relationships points to the importance of relationship quality in shaping health outcomes over one’s life, which might be more important than whether one is involved in a relationship per se (Liu and Waite 2014; Robles and Kiecolt-Glaser 2003). Consistent with this view as well as Hypothesis 3, we find that women who reported that their sexual relationship was extremely physically pleasurable and/or extremely emotionally satisfying tend to have lower risks of hypertension in the following five years than women who were not physically or emotionally satisfied. A good quality sexual relationship may enhance emotional closeness and intimacy between partners. Previous studies suggest that a strong, deep and close relationship is an important source of social and emotional support (Wellman and Worley 1990), which may reduce stress and promote psychological well-being and, in turn, cardiovascular health. This may be more relevant to women than to men because men in all relationships, regardless of the quality, are more likely to receive support from their partner than are women (Erickson 2005; Kalmijn 2003); while only women in good quality relationships may acquire such benefits from their partner (Gallo et al. 2003). Moreover, the female sexual hormone released during orgasm, which is more likely to happen when they feel pleasure and satisfaction in the process of sex, may also promote women’s health. Future studies should examine the specific social, psychological, behavioral and biological mechanisms under which sexual quality affects women’s cardiovascular health.
Surprisingly, better sexual quality seems not to protect men’s cardiovascular health. Indeed, our results suggest that men who felt extremely pleasured and extremely satisfied in their sexual relationship even have higher risk of experiencing CVD events five years later than men who did not feel very pleasured or satisfied in their relationship. These results are consistent with our suspicion that older men who reported that they had sex frequently and those who reported very high levels of physical and/or emotional satisfaction with sex may also use sexual medication or supplements, or have some type of sexual addiction, sexual compulsivity or sexual impulsivity. These may damage cardiovascular health directly or lead to behaviors that do so.
Reverse Causation
Although we develop a causal framework from which we draw hypotheses on how partnered sexuality affects cardiovascular risk, it is also likely that poor cardiovascular health disrupts later sexual life (Hypothesis 4). Surprisingly, we find no evidence for this reverse causation. Indeed, the only significant reverse effects we find indicate an opposite direction. We find that men who had undiagnosed hypertension and women who had uncontrolled hypertension tend to report higher frequency of sex and/or higher levels of emotional satisfaction in their sexual relationship five years later in comparison to those with normal blood pressure initially. Although not well understood yet, one possibility is that reproductive steroids, especially testosterone, may increase both sexual behavior/motivation and arterial hypertension by stimulating the renin-angiotensin-aldosterone system (dos Santos, Silva, Ribeiro and Stefanon 2014). In addition, recent clinical studies suggest that hypertension per se does not predispose men to erection problems (Korhonen et al. 2015). This is especially true for undiagnosed or uncontrolled hypertension that is often at an early stage of the disease, in which the blood vessels are functionally but not structurally (or permanently) constricted (i.e. the vessels are dilatable). Moreover, given that our measures of sexual frequency and sexual quality are based on self-reported measures, it is likely that hypertensive people have relatively lower expectations for their sex life than others and therefore are more likely to overestimate their activity and look on that activity more positively than would others. Given the relatively sparse evidence we found, future research is clearly warranted to confirm these findings.
Limitations
Several study limitations should be considered. First, although we attempt to tease out the possibility of the reciprocal relationships between sexuality and cardiovascular health by applying one of the most widely used statistical methods, cross-lagged models, to analyze longitudinal panel data, this approach is limited in fully determining causality (Finkel 2004). Second, our analyses are based on two waves of panel data with a five-year interval. To better understand the causal processes linking partnered sexuality and cardiovascular risk, future studies should employ longitudinal data with shorter intervals as well as more waves of follow-up. The NSHAP is currently collecting the third wave of data, which will provide opportunities to further untangle causality. Third, our study focuses on later life. We want to caution readers not to extend the interpretation of the findings to a broader age range. Some of the patterns may be different among younger adults. Future studies should examine a broader range of ages to understand whether the association between sexual relationships and cardiovascular risk varies across age. Fourth, due to data limitations, our measures for CVD risk lack important markers such as low-density lipoprotein (LDL) and high-density lipoprotein (HDL). Future research should examine a broader range of measures for CVD risk. Fifth, sexual quality is one dimension of overall relationship quality. The enjoyment of sex may interact with other dimensions of relationship quality, such as conflict or support, to determine overall quality. Future research should examine the role of sexuality in relationship quality more generally. Sixth, the relatively small number of significant effects identified in this study may indicate Type 1 error by chance. Future studies are clearly warranted to further investigate health links with sexuality among older adults. Finally, various social, biological, psychological, and behavioral mechanisms underlie the link between sexuality and cardiovascular risk. Future studies should seek to identify the precise mechanisms and processes through which sexuality affects men and women’s cardiovascular health.
CONCLUSION
Despite a large body of evidence pointing to a strong linkage between social relationships and health (Umberson and Montez 2010), partnered sexuality, as a fundamental type of social relationship, has been relatively ignored. Our understanding of this unique relationship is even less advanced among older adults. This is important given that adults aged 65 and over account for 13 percent of the U.S. population, with this share projected to grow substantially over the next several decades (U.S. Census 2010). In this study, we provide some of the first generalizable population-based evidence of linkages between partnered sexuality and cardiovascular health in later life using nationally representative longitudinal data. We find that for women, partnered sex of good quality seems to promote cardiovascular health, specifically reducing the risks of hypertension. Although growing evidence suggests that women are especially vulnerable to cardiovascular problems from poor relationship quality or marital loss (Liu and Waite 2014; Zhang and Hayward 2006), our results show the positive side, with benefits to women’s cardiovascular health from a rewarding sexual relationship. Unfortunately, good sexual quality does not protect men’s cardiovascular risk. Indeed, for men especially at older ages, although moderate frequency of sex may also bring some health benefits, having sex too frequently or extremely high levels of physical and/or emotional enjoyment from sex might be a risk factor for experiencing CVD events over time. Strikingly, we find that having sex once a week or more puts older men at a risk for experiencing CVD events that is almost two times greater than older men who are sexually inactive. These findings challenge the assumption that sex brings uniform health benefits to everyone (Brody 2010).
Acknowledgments
This research was supported by the National Institute on Aging K01 Award K01AG043417 to Hui Liu, the MERIT Award R37AG030481 to Linda Waite, and by Grants R01 AG043538, R01 AG033903, and P30 AG012857 from the National Institute on Aging, Grant R03 HD078754 from the Eunice Kennedy Shriver National Institute of Child Health and Human Development and the Office of Behavioral and Social Sciences Research, and Grant R01 HL073287 from the National Heart, Lung, and Blood Institute.
Contributor Information
Hui Liu, Department of Sociology, Michigan State University.
Linda Waite, Department of Sociology & NORC, University of Chicago.
Shannon Shen, Department of Sociology, Michigan State University.
Donna Wang, Department of Medicine, Michigan State University.
References
- Agresti Alan, Finley Barbara. Statistical Methods for the Social Sciences. 4. Prentice Hall; 2009. [Google Scholar]
- Bancroft John, Vukadinovic Zoran. Sexual Addition, Sexual Compulsivity, Sexual Impulsivity, or What? Toward a Theoretical Model. Journal of Sex Research. 2004;41(3):225–34. doi: 10.1080/00224490409552230. [DOI] [PubMed] [Google Scholar]
- Brody Stuart. The Relative Health Benefits of Different Sexual Activities. Journal of Sexual Medicine. 2010;7(4pt1):1336–61. doi: 10.1111/j.1743-6109.2009.01677.x. [DOI] [PubMed] [Google Scholar]
- Burman B, Margolin G. Analysis of the Association between Marital Relationships and Health Problems: An Interactional Perspective. Psychological Bulletin. 1992;112(1):39–63. doi: 10.1037/0033-2909.112.1.39. [DOI] [PubMed] [Google Scholar]
- Butt Dorcas Susan. The Sexual Response as Exercise. Sports Medicine. 1990;9(6):330–43. doi: 10.2165/00007256-199009060-00002. [DOI] [PubMed] [Google Scholar]
- Carpenter Laura M. Studying Sexualities from a Life Course Perspective. In: DeLamater John, Plante Rebecca F., editors. Handbook of the Sociology of Sexualities. New York: Springer; 2015. [Google Scholar]
- Carpenter Laura M, DeLamater John., editors. Sex for Life: From Virginity to Viagra, How Sexuality Changes Throughout our Lives. New York: New York University Press; 2012. [Google Scholar]
- Cheitlin Melvin D. Sexual Activity and Cardiovascular Disease. American Journal of Cardiology. 2003;92(9):3–8. doi: 10.1016/s0002-9149(02)03367-2. [DOI] [PubMed] [Google Scholar]
- Cohen S. Social Relationships and Health. American Psychologist. 2004;59(8):676–84. doi: 10.1037/0003-066X.59.8.676. [DOI] [PubMed] [Google Scholar]
- Cornwell Erin York, Waite Linda J. Social Network Resources and Management of Hypertension. Journal of Health and Social Behavior. 2012;53(2):215–231. doi: 10.1177/0022146512446832. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Curtis Brian M, O’Keefe James H., Jr Autonomic Tone as a Cardiovascular Risk Factor: The Dangers of Chronic Fight or Flight. Mayo Clinic Proceedings. 2002;77(1):45–54. doi: 10.4065/77.1.45. [DOI] [PubMed] [Google Scholar]
- Dahabreh Issa J, Paulus Jessica K. Association of Episodic Physical and Sexual Activity with Triggering of Acute Cardiac Events Systematic Review and Meta-analysis. JAMA. 2011;305(12):1225–33. doi: 10.1001/jama.2011.336. [DOI] [PMC free article] [PubMed] [Google Scholar]
- DeLamater John. Sexual Expression in Later Life: A Review and Synthesis. The Journal of Sex Research. 2012;49(2–3):125–41. doi: 10.1080/00224499.2011.603168. [DOI] [PubMed] [Google Scholar]
- John DeLamater, Karraker Amelia. Sexual Functioning in Older Ddults. Current Psychiatry Reports. 2009;11(1):6–11. doi: 10.1007/s11920-009-0002-4. [DOI] [PubMed] [Google Scholar]
- DeLamater John, Sill Morgan. Sexual Desire in Later Life. The Journal of Sex Research. 2005;42(2):138–49. doi: 10.1080/00224490509552267. [DOI] [PubMed] [Google Scholar]
- DeLamater John, Moorman Sara M. Sexual Behavior in Later Life. Journal of Aging and Health. 2007;19(6): 921–46. doi: 10.1177/0898264307308342. [DOI] [PubMed] [Google Scholar]
- DeLamater John, Friedrich William N. Human Sexual Development. The Journal of Sex Research. 2002;39(1):10–4. doi: 10.1080/00224490209552113. [DOI] [PubMed] [Google Scholar]
- Dimmeler Stefanie, Zeiher Andreas M. Exercise and Cardiovascular Health Get Active to “AKTivate” Your Endothelial Nitric Oxide Synthase. Circulation. 2003;107(25):3118–20. doi: 10.1161/01.CIR.0000074244.82874.A0. [DOI] [PubMed] [Google Scholar]
- Dogan Tayfun, Tugut Nilufer, Golbasi Zehra. The Relationship between Sexual Quality of Life, Happiness, and Satisfaction with Life in Married Turkish Women. Sex Disability. 2013;31(3):239–47. [Google Scholar]
- dos Santos Roger Lyrio, da Silva Fabrício Bragança, Ribeiro Rogério Faustino, Stefanon Ivanita. Sex Hormones in the Cardiovascular System. Hormone Molecular Biology and Clinical Investigation. 2014;18(2):89–103. doi: 10.1515/hmbci-2013-0048. [DOI] [PubMed] [Google Scholar]
- Ebrahim Shah, May Margaret, Ben Shlomo Y, McCarron P, Frankel S, Yarnell J, Davey Smith G. Sexual Intercourse and Risk of Ischaemic Stroke and Coronary Heart Disease: The Caerphilly Study. Journal of Epidemiology and Community Health. 2002;56(2): 99–102. doi: 10.1136/jech.56.2.99. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Ein-Dor Tsachi, Hirschberger Gilad. Sexual Healing: Daily Diary Evidence That Sex Relieves Stress for Men and Women in Satisfying Relationships. Journal of Social and Personal Relationships. 2012;29(1): 126–139. [Google Scholar]
- Elder Glen H, Jr, O’Rand Angela M. Adult Lives in a Changing Society. In: Cook KS, Fine GA, House JS, editors. Sociological Perspectives on Social Psychology. Needham Heights, MA: Allyn and Bacon; 1995. pp. 452–75. [Google Scholar]
- Erickson Rebecca J. Why Emotion Work Matters: Sex, Gender, and the Division of Household Labor. Journal of Marriage and Family. 2005;67:337–351. [Google Scholar]
- Everson-Rose Susan A, Lewis Tené T. Psychosocial Factors and Cardiovascular Diseases. Annual Review of Public Health. 2005;26:469–500. doi: 10.1146/annurev.publhealth.26.021304.144542. [DOI] [PubMed] [Google Scholar]
- Exton Michael S, Bindert Anne, Kruger Tillmann, Scheller Friedmann, Hartmann Uwe, Schedlowski Manfred. Cardiovascular and Endocrine Alterations after Masturbation-Induced Orgasm in Women. Psychosomatic Medicine. 1999;61(3):280–9. doi: 10.1097/00006842-199905000-00005. [DOI] [PubMed] [Google Scholar]
- Finkel Steven E. Cross-Lagged. In: Lewis-Beck Michael S, Bryman Alan, Liao Tim Futing., editors. The SAGE Encyclopedia of Social Science Research Methods. SAGE Publications, Inc; 2004. [Google Scholar]
- Fisher Terri D. Publication of The Society for the Scientific Study of Sexuality. 2012. What Sexual Scientists Know About Gender Differences and Similarities in Sexuality. [Google Scholar]
- Frappier Julie, Toupin Isabelle, Levy Joseph J, Aubertin-Leheudre Mylene, Karelis Antony D. Energy Expenditure during Sexual Activity in Young Healthy Couples. PLoS one. 2013;8(10):e79342. doi: 10.1371/journal.pone.0079342. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Fuhrera Rebecca, Stansfeld Stephen A. How Gender affects Patterns of Social Relations and the Impact on Health: A comparison of One or Multiple Souces of Support from ‘Close Persons.’. Social Science & Medicine. 2002;54(5):811–25. doi: 10.1016/s0277-9536(01)00111-3. [DOI] [PubMed] [Google Scholar]
- Galinsky Adena M, Waite Linda J. Sexual Activity and Psychological Health as Mediators of the Relationship Between Physical Health and Marital Quality. Journals of Gerontology: Social Sciences. 2014;69:482–92. doi: 10.1093/geronb/gbt165. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Galinsky Adena M, McClintock Martha K, Waite Linda J. Sexuality and Physical Contact in National Social Life, Health, and Aging Project Wave 2. The Journals of Gerontology Series B: Psychological Sciences and Social Sciences. 2014;69(2):S83–S98. doi: 10.1093/geronb/gbu072. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Gallo Linda C, Troxel Wendy M, Matthews Karen A, Kuller Lewis H. Marital Status and Quality in Middle-aged Women: Associations with Levels and Trajectories of Cardiovascular Risk Factors. Health Psychology. 2003;22(5):453–63. doi: 10.1037/0278-6133.22.5.453. [DOI] [PubMed] [Google Scholar]
- Go Alan S, et al. on behalf of the American Heart Association Statistics Committee and Stroke Statistics. Heart Disease and Stroke Statistics—2014 Update: A Report from the American Heart Association. Circulation. 2014;129:e28–292. doi: 10.1161/01.cir.0000441139.02102.80. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Hammack Phillip L. The Life Course Development of Human Sexual Orientation: An Integrative Paradigm. Human Development. 2005;48:267–90. [Google Scholar]
- Harvey John, Wenzel Amy, Sprecher Susan. Introduction. In: Harvey John, Wenzel Amy, Sprecher Susan., editors. The Handbook of Sexuality in Close Relationships. Hillsdale, NJ: Erlbaum; 2004. pp. 3–6. [Google Scholar]
- Heckman James J. Sample Selection Bias as a Specification Error. Econometrica. 1979;47(1):153–61. [Google Scholar]
- Iveniuk James, Cagney Kathleen A, O’Muircheartaigh Colm. Religious Influence on Older American’s Sexual Lives: A Nationally Representative Profile. Archives of Sexual Behavior. 2015 doi: 10.1007/s10508-015-0534-0. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Izzo Joseph L, Jr, Black Henry R., editors. Hypertension Primer: The Essentials of High Blood Pressure. 3. Baltimore: Lippincott Williams & Wilkins; 2003. [Google Scholar]
- Jaarsma Tiny, Dracup Kathleen, Walden Julie, Stevenson Lynne Warner. Sexual Function in Patients with Advanced Heart Failure. Heart & Lung: The Journal of Acute and Critical Care. 1996;25(4):262–70. doi: 10.1016/s0147-9563(96)80061-6. [DOI] [PubMed] [Google Scholar]
- Kalmijn Matthijs. Shared Friendship Networks and the Life Course: An Analysis of Survey Data on Married and Cohabiting Couples. Social Networks. 2003;25:231–249. [Google Scholar]
- Kashdan Todd B, Adams Leah M, Farmer Antonina S, Ferssizidis Patty, McKnight Patrick E, Nezlek John B. Sexual Healing: Daily Diary Investigation of the Benefits of Intimate and Pleasurable Sexual Activity in Socially Anxious Adults. Archives of Sexual Behavior. 2014;43(7):1417–1429. doi: 10.1007/s10508-013-0171-4. [DOI] [PubMed] [Google Scholar]
- Kiecolt-Glaser Janice K, Newton Tamara L. Marriage and Health: His and Hers. Psychological Bulletin. 2001;127(4): 472–503. doi: 10.1037/0033-2909.127.4.472. [DOI] [PubMed] [Google Scholar]
- Kinsey Alfred Charles, Pomeroy Wardell Baxter, Martin Clyde Eugene. Sexual Behavior in the Human Male. Bloomington, IL: Indiana University Press; 1998. [Google Scholar]
- Korhonen PE, Ettala O, Kautiainen H, Kantola I. Factors Modifying the Effect of Blood Pressure on Erectile Function. Journal of Hypertension. 2015;33(5):975–980. doi: 10.1097/HJH.0000000000000519. [DOI] [PubMed] [Google Scholar]
- Kruger Tillmann, Exton Michael S, Pawlak Cornelius, von zur Muhlen Alexander, Hartmann Uwe, Schedlowski Manfred. Neuroendocrine and Cardiovascular Response to Sexual Arousal and Orgasm in Men. Psychoneuroendocrinology. 1998;23(4):401–411. doi: 10.1016/s0306-4530(98)00007-9. [DOI] [PubMed] [Google Scholar]
- Lakatta Edward G, Levy Daniel. Arterial and Cardiac Aging: Major Shareholders in Cardiovascular Disease Enterprises Part I: Aging Arteries: A “Set Up” for Vascular Disease. Circulation. 2003;107(1):139–46. doi: 10.1161/01.cir.0000048892.83521.58. [DOI] [PubMed] [Google Scholar]
- Laumann Edward O, Paik Anthony, Glasser Dale B, Kang Joeng-Han, Wang Tianfu, Levinson Bernard, Moreira Edwon D, Nicolosi Alfredo, Gingell Clive. A Cross-National Study pf Subjective Sexual Well-Being Among Older Women and Men: Findings from the Global Study of Sexual Attitudes and Behaviors. Archives of Sexual Behavior. 2006;35(2):145–61. doi: 10.1007/s10508-005-9005-3. [DOI] [PubMed] [Google Scholar]
- Laumann Edward O, Das Aniruddha, Waite Linda J. Sexual Dysfunction among Older Adults: Prevalence and Risk Factors from a Nationally Representative U.S. Probability Sample of Men and Women 57 to 85 Years of Age. Journal of Sexual Medicine. 2008;5:2300–2311. doi: 10.1111/j.1743-6109.2008.00974.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Lawrance Kelli-an, Sandra Byers E. Development of the Interpersonal Exchange Model of Sexual Satisfaction in Long Term Relationships. Canadian Journal of Human Sexuality. 1992;1(3):123–8. [Google Scholar]
- Levin Roy J. Sexual Activity, Health and Well-Being – The Beneficial Roles of Coitus and Masturbation. Sexual and Relationship Therapy. 2007;22(1):135–48. [Google Scholar]
- Levine Glenn N, et al. on behalf of the American Heart Association Council on Clinical Cardiology Council on Cardiovascular Nursing Council on Cardiovascular Surgery and Anesthesia, and Council on Quality of Care and Outcomes Research. Sexual Activity and Cardiovascular Disease: A Scientific Statement from the American Heart Association. Circulation. 2012;125:1058–72. doi: 10.1161/CIR.0b013e3182447787. [DOI] [PubMed] [Google Scholar]
- Lindau Stacy Tessler, Gavrilova Natalia. Sex, Health, and Years of Sexually Active Life Gained Due to Good Health: Evidence from Two US Population Based Cross Sectional Surveys of Ageing. British Medical Journal. 2010;340:c810. doi: 10.1136/bmj.c810. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Lindau Stacy Tessler, Philip Schumm L, Laumann Edward O, Levinson Wendy, O’Muircheartaigh Colm A, Waite Linda J. A Study of Sexuality and Health among Older Adults in the United States. The New England Journal of Medicine. 2007;357(8):762–74. doi: 10.1056/NEJMoa067423. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Liu Hui, Umberson Debra. The Times They Are A Changin’: Marital Status and Health Differentials From 1972 to 2003. Journal of Health and Social Behavior. 2008;49(3):239–53. doi: 10.1177/002214650804900301. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Liu Hui, Waite Linda. Bad Marriage, Broken Heart? Age and Gender Differences in the Link between Marital Quality and Cardiovascular Risks among Older Adults. Journal of Health and Social Behavior. 2014;55(4):403–423. doi: 10.1177/0022146514556893. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Magon Navneet, Kalra Sanjay. The Orgasmic History of Oxytocin: Love, Lust, and Labor. Indian Journal of Endocrinology & Metabolism. 2011;15(Suppl 3):S156–S161. doi: 10.4103/2230-8210.84851. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Masters William H, Johnson Virginia E. Human Sexual Response. Toronto; New York: Bantam Books; 1966. [Google Scholar]
- McEwen Bruce S, Stellar Eliot. Stress and the Individual: Mechanisms Leading to Disease. Archives of Internal Medicine. 1993;153(18):2093–101. [PubMed] [Google Scholar]
- Milhausen Robin R, Herold Edward S. Does the Sexual Double Standard Still Exist? Perceptions of University Women. The Journal of Sex Research. 1999;36(4): 361–368. [Google Scholar]
- Mittleman Murray A, Maclure Malcolm, Tofler Geoffrey H, Sherwood Jane B, Goldberg Robert J, Muller James E for the Determinants of Myocardial Infarction Onset Study Investigators. Triggering of Acute Myocardial Infarction by Heavy Physical Exertion -- Protection against Triggering by Regular Exertion. New England Journal of Medicine. 1993;329(23):1677–83. doi: 10.1056/NEJM199312023292301. [DOI] [PubMed] [Google Scholar]
- Mozzafarian Dariush, Benjamin Emelia J, Go Alan S, et al. Heart Disease and Stroke Statistics-2015 Update: A Report From the American Heart Association. Circulation. 2015;131: e29–322. doi: 10.1161/CIR.0000000000000152. [DOI] [PubMed] [Google Scholar]
- Muller James E, Mittleman Murray A, Maclure Malcolm, Sherwood Jane B, Tofler Geoffrey H. Triggering Myocardial Infarction by Sexual Activity: Low Absolute Risk and Prevention by Regular Physical Exertion. The Journal of the American Medical Association. 1996;275(18):1405–9. doi: 10.1001/jama.275.18.1405. [DOI] [PubMed] [Google Scholar]
- Muthén L, Muthén B. Mplus User’s Guide. 3. Los Angeles: Authors; 2007. [Google Scholar]
- Myers Jonathan. Exercise and Cardiovascular Health. Circulation. 2003;107(1):e2–e5. doi: 10.1161/01.cir.0000048890.59383.8d. [DOI] [PubMed] [Google Scholar]
- Nallanathan Bhairavi, McDade Thomas, Williams Sharon, Lindau Stacy Tessler. NORC and the University of Chicago. 2008. Dried Blood Spot Measurement of C-reactive Protein in Wave I of the National Social Life, Health & Aging Project (NSHAP) [Google Scholar]
- National Heart, Lung, and Blood Institute. The Seventh Report of the Joint National Committee on Prevention, Detection, Evaluation, and Treatment of High Blood Pressure. Bethesda, MD: U.S. Department of Health and Human Services; 2003. [PubMed] [Google Scholar]
- Pearson Thomas A, Mensah George A, Wayne Alexander R, Anderson Jeffrey L, Cannon Richard O, III, Criqui Michael, Fadl Yazid Y, Fortmann Stephen P, Hong Yuling, Myers Gary L, Rifai Nader, Smith Sidney C, Jr, Taubert Kathryn, Tracy Russell P, Vinicor Frank. Markers of Inflammation and Cardiovascular Disease: Application to Clinical and Public Health Practice: A Statement for Healthcare Professionals from the Centers for Disease Control and Prevention and the American Heart Association. Circulation. 2003;107(3):499–511. doi: 10.1161/01.cir.0000052939.59093.45. [DOI] [PubMed] [Google Scholar]
- Radloff Lenore Sawyer. The CES-D Scale: A Self-Report Depression Scale for Research in the General Population. Applied Psychological Measurement. 1977;1(3):385–401. [Google Scholar]
- Ridker Paul M. Clinical Application of C-reactive Protein for Cardiovascular Disease Detection and Prevention. Circulation. 2003;107(3):363–69. doi: 10.1161/01.cir.0000053730.47739.3c. [DOI] [PubMed] [Google Scholar]
- Safi Arshad M, Rachko Maurice, Yeshou Dima, Stein Rishard A. Sexual Activity as a Trigger for a Ventriclar Tachycardia in a Patient with Implantable Cardioverter Defibrillator. Archives of Sexual Behavior. 2002;31(3):295–9. doi: 10.1023/a:1015209121678. [DOI] [PubMed] [Google Scholar]
- Salmon Peter. Effects of Physical Exercise on Anxiety, Depression, and Sensitivity to Stress: A Unifying Theory. Clinical Psychology Review. 2001;21(1):33–61. doi: 10.1016/s0272-7358(99)00032-x. [DOI] [PubMed] [Google Scholar]
- Satcher David. The Surgeon General’s Call to Action to Promote Sexual Health and Responsible Sexual Behavior. American Journal of Health Education. 2001;32(6):356–368. [Google Scholar]
- Schnarch David M. Constructing the Sexual Crucible: An Integration of Sexual and Marital Therapy. New York: Norton; 1991. [Google Scholar]
- Schwartz Amy R, Gerin William, Davidson Karina W, Pickering Thomas G, Brosschot Jos F, Thayer Julian F, Christenfeld Nicholas, Linden Wolfgang. Toward a Causal Model of Cardiovascular Responses to Stress and the Development of Cardiovascular Disease. Psychosomatic Medicine. 2003;65(1): 22–35. doi: 10.1097/01.psy.0000046075.79922.61. [DOI] [PubMed] [Google Scholar]
- Schwarz ER, Rodriguez J. Sex and the Heart. International Journal of Impotence Research. 2005;17:S4–S6. doi: 10.1038/sj.ijir.3901422. [DOI] [PubMed] [Google Scholar]
- Smith George Davey, Frankel Stephen, Yarnell John. Sex and Death: Are they Related? Findings from the Caerphilly Cohort Study. BMJ. 1997;315(7123):1641–4. doi: 10.1136/bmj.315.7123.1641. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Susan Sprecher. Sexual Satisfaction in Premarital Relationships: Associations with Satisfaction, Love, Commitment, and Stability. Journal of Sex Research. 2002;39(3):190–6. doi: 10.1080/00224490209552141. [DOI] [PubMed] [Google Scholar]
- Stein Richard A. Cardiovascular Response to Sexual Activity. The American Journal of Cardiology. 2000;86(2):27–9. doi: 10.1016/s0002-9149(00)00888-2. [DOI] [PubMed] [Google Scholar]
- Stroope Samuel, McFarland Michael J, Uecker Jeremy E. Marital Characteristics and the Sexual Relationships of U.S. Older Adults: An Analysis of National Social Life, Health, and Aging Project Data. Archives of Sexual Behavior. 2015;44(1): 233–247. doi: 10.1007/s10508-014-0379-y. [DOI] [PubMed] [Google Scholar]
- Taylor Shelley E, Klein Laura Cousino, Lewis Brian P, Gruenewald Tara L, Gurung Regan AR, Updegraff John A. Biobehavioral Responses to Stress in Females: Tend-and-Befriend, not Fight-or-Flight. Psychological Review. 2000;107(3):411–29. doi: 10.1037/0033-295x.107.3.411. [DOI] [PubMed] [Google Scholar]
- Umberson Debra, Montez Jennifer Karas. Social Relationships and Health: A Flashpoint for Health Policy. Journal of Health and Social Behavior. 2010;51(1 suppl):S54–S66. doi: 10.1177/0022146510383501. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Waite Linda J, Charme Cameron. Sexuality over the Lifecourse. In: Wright J, editor. Heterosexuality. International Encyclopedia for the Behavioral and Social Sciences. 2. Vol. 21. Elsevier Ltd; 2015. pp. 840–5. [DOI] [Google Scholar]
- Waite Linda J, Laumann Edward O, Levinson Wendy, Lindau Stacy Tessler, O’Muircheartaigh Colm A. National Social Life, Health, and Aging Project (NSHAP): Wave 1. Ann Arbor, MI: Inter-university Consortium for Political and Social Research [distributor]; 2014. ICPSR20541-v6. [Google Scholar]
- Waite Linda J, Joyner Kara. Emotional Satisfaction and Physical Pleasure in Sexual Unions: Time Horizon, Sexual Behavior and Sexual Exclusivity. Journal of Marriage and the Family. 2001;63(1):247–64. [Google Scholar]
- Waite Linda J, Cagney Kathleen, Dale William, Huang Elbert, Laumann Edward O, McClintock Martha, O’Muircheartaigh Colm A, Phillip Schumm L, Cornwell Benjamin. National Social Life, Health, and Aging Project (NSHAP): Wave 2 and Partner Data Collection. Ann Arbor, MI: Inter-university Consortium for Political and Social Research [distributor]; 2014. ICPSR34921-v1. [Google Scholar]
- Walen Heather R, Lachman Margie E. Social Support and Strain from Partner, Family, and Friends: Costs and Benefits for Men and Women in Adulthood. Journal of Social and Personal Relationships. 2000;17(1):5–30. [Google Scholar]
- Wellman Barry, Wortley Scot. Different Strokes from Different Folks: Community Ties and Social Support. American Journal of Sociology. 1990;96(3):558–88. [Google Scholar]
- World Health Organization. Physical Status: The Use and Interpretation of Anthropometry. Geneva: World Health Organization; 1995. WHO Technical Report Series 854. [Google Scholar]
- Xu Lin, Freeman Guy, Cowling Benjamin J, Mary Schooling C. Testosterone Therapy and Cardiovascular Events among Men: A Systematic Review and Meta-analysis of Placebo-controlled Randomized Trials. BMC Medicine. 2013;11(1):108. doi: 10.1186/1741-7015-11-108. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Zhang Zhenmei, Hayward Mark D. Gender, the Marital Life Course, and Cardiovascular Health in Late Midlife. Journal of Marriage and Family. 2006;68(3):639–657. [Google Scholar]


